Published online Dec 18, 2024. doi: 10.5312/wjo.v15.i12.1208
Revised: October 21, 2024
Accepted: November 8, 2024
Published online: December 18, 2024
Processing time: 179 Days and 23.8 Hours
Clavicle fractures are among the most common fractures seen in the emergency department. While acromioclavicular (AC) joint injuries are much less common. However, ipsilateral combinations of these injuries are quite rare with only a few cases reported in the literature.
A 29-year-old man who sustained a combination of ipsilateral AC joint dislocation and midshaft clavicle fracture. He underwent open reduction and plate fixation of the clavicle fracture, as well as semi-rigid surgical implants used to restore both the AC ligaments and the coracoclavicular joint. one year follow-up revealed that the patient had a complete range of motion and excellent shoulder scores. This case presents a rare presentation of such combination of injuries, contributing valuable insights to the literature on such rare injuries.
Combined midshaft clavicle fractures and AC joint dislocations are considered quite rare. Timely diagnosis of such injuries leads to great functional outcomes. AC joint dislocation should be suspected with midshaft clavicle fractures and should be investigated radiologically and clinically in an appropriate manner. Still, there is no consensus on the optimal management of such injuries.
Core Tip: The combination of ipsilateral acromioclavicular (AC) joint dislocation and midshaft clavicle fracture is uncommon. Only a few cases have been recorded in the literature. We report a case of a 29-year-old man who suffered this injury pattern. He underwent open reduction and plate fixation of the clavicle fracture, as well as semi-rigid surgical implants used to restore both the AC ligaments and the coracoclavicular joint. The patient's clinical findings, imaging results, and surgical procedure are presented, along with relevant images. This case is notable for the combined AC joint dislocation and midshaft clavicle fracture, a finding that contributes to the literature on such rare associated injuries.
- Citation: Korkoman AJ, Alhamodi A, Alrusayni S, Almalki MM. Ipsilateral Rockwood type V acromioclavicular joint dislocation and midshaft clavicle fracture: A case report. World J Orthop 2024; 15(12): 1208-1213
- URL: https://www.wjgnet.com/2218-5836/full/v15/i12/1208.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i12.1208
Clavicle fractures are among the most common fractures seen in the emergency department, accounting for 5% of all adult fractures and 35% of shoulder girdle fractures[1]. While acromioclavicular (AC) joint injuries account for about 9% of shoulder girdle injuries[2]. However, ipsilateral combinations of these injuries are quite rare with only a few cases reported in the literature[3]. Although the exact mechanism of injury is unknown these injuries almost always associated with high-energy trauma[3].
The clavicle is an S-shaped long bone connecting the axial to the appendicular skeleton in conjunction with the scapula. Medially, the clavicle articulates with the manubrium sterni, forming the sternoclavicular joint[4]. Laterally, the clavicle articulates with the acromion forming the AC joint which is a diarthrodial joint lined by fibrocartilage and contains an intra-articular disc. AC ligament, coracoclavicular (CC), and coracoacromial ligament constitute the three main ligaments supporting the AC joint[5].
Isolated clavicular fractures can be managed conservatively, surgically with open or close reduction and internal fixation using plate and screw osteosynthesis or an intramedullary nail[6]. Isolated AC joint dislocations can be managed conservatively, surgically with AC fixation and CC fixation in an acute setting or with CC reconstruction in chronic injuries[7].
In this article, we report a case of an adult male with a rare presentation of ipsilateral midshaft clavicle fracture and AC joint dislocation. We describe the clinical and radiographic presentation, surgical approaches, surgical management, and clinical and radiographic outcomes.
A fit and well 29-year-old, right-hand dominant male. Presented to the emergency department complaining of left shoulder pain after he fell from a motorcycle directly on his left shoulder.
The patient fell from a motorcycle directly on his left shoulder, resulting in left shoulder pain. The patient was transferred to our institution by emergency medical services.
There was no history of fracture or surgery.
The patient had no significant past medical, surgical, or family history.
Physical examination of the left shoulder showed intact skin with mild swelling, palpable midshaft tender deformity, and tenderness over the distal clavicle. The neurovascular examination was unremarkable.
No abnormalities were revealed in the laboratory examinations.
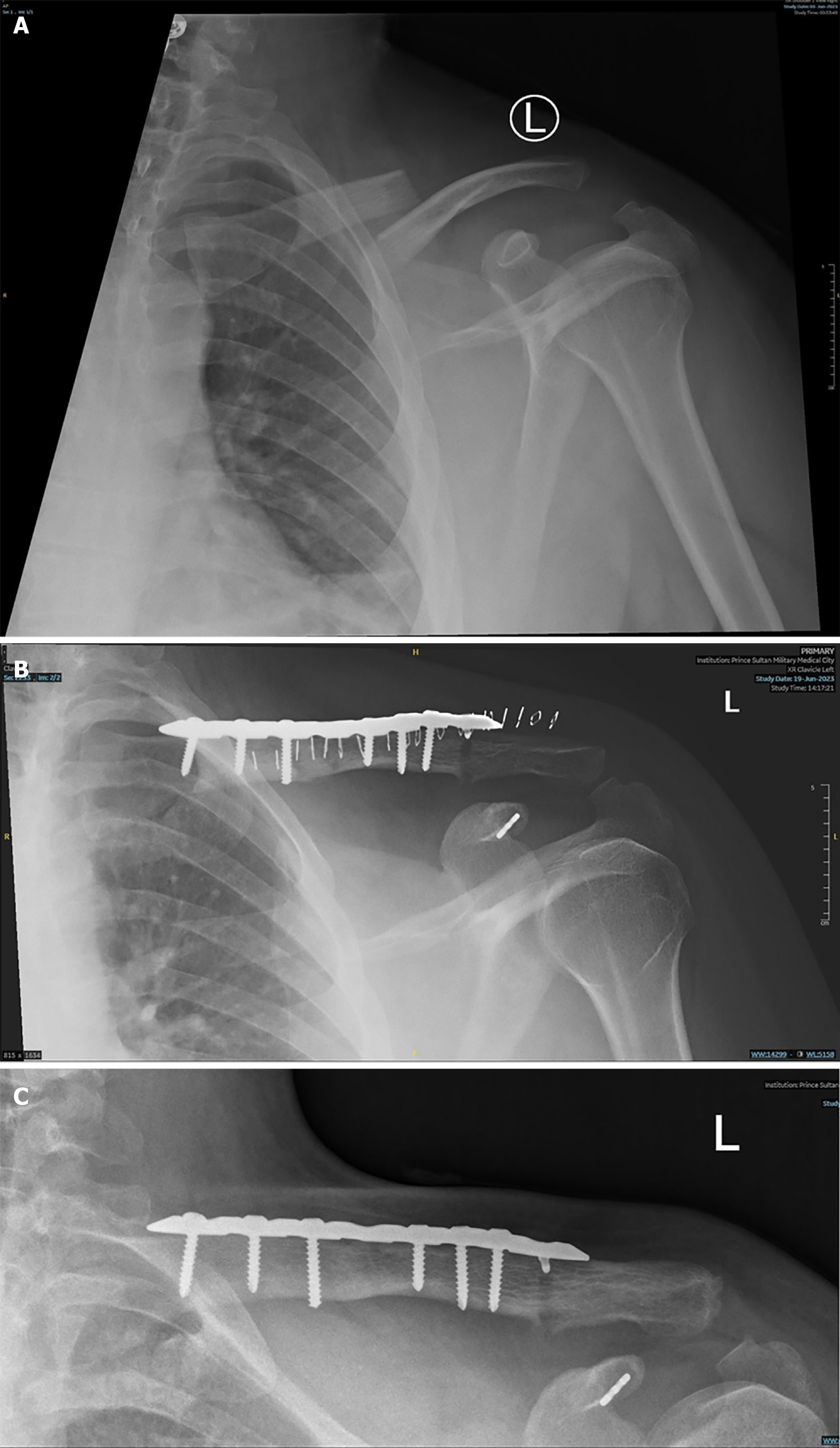
Anteroposterior and Zanca plain radiography of the left shoulder revealed a displaced midshaft clavicle fracture (Robinson type 2B1) and type 5 AC joint dislocation according to Rockwood classification (Figure 1A).
Based on the history, physical examination, and imaging, the patient was diagnosed with ipsilateral Rockwood type V acromioclavicular joint dislocation and midshaft clavicle fracture.
The patient underwent open reduction and internal fixation of the left clavicle two days after the trauma under general anesthesia in a beach chair position. A horizontal anterior approach to the clavicle was utilized and was extended laterally.
The fracture was visualized, the distal clavicle segment was superiorly displaced, and the CC and AC ligaments were completely disrupted. The fracture was reduced and fixed with a pre-contoured 8-hole 3.5 mm superior locking compression plate. The AC joint was reduced, the intra-articular disc removed, and CC fixation was done using a plate suture button on the most lateral plate hole just lateral to the coracoid (Figure 1B).
Post-operative plain radiography showed anatomical reduction and good plate osteosynthesis positioning but, the button looks more towards the tip of the coracoid. The patient was kept in an arm sling postoperatively for two weeks followed by passive range of motion, pendulum exercise of the left shoulder, and full active range of motion of the left elbow and wrist.
The patient was followed up for 1 year (Figure 1C), plain radiography demonstrated union of the fracture, normal CC distance, and increased AC joint distance. The functional outcomes were excellent with an Oxford shoulder score of 48; Quick-Dash: 0[8].
The AC joint is formed by the distal end of the clavicle and the acromion. It is a diarthroidal joint covered by fibrocartilage and contains an intra-articular disc. This joint is supported by surrounding capsular and extra-capsular ligaments that maintain its anterioposterior as well as its vertical stability. The AC joint is circumferentially surrounded by capsular ligaments which are important for horizontal stability that inserts on the lateral clavicle 3.5 mm from the articular surface[9]. The Vertical stability is maintained by the CC ligaments which compromise of the conoid and trapezoid ligaments that originated from the superior surface of the coracoid and insert on the undersurface of the clavicle on the conoid tubercle and trapezoid line, respectively. The conoid and trapezoid insert 2.5 cm and 3.5 cm from the lateral end of the clavicle, respectively[9].
The combination of ipsilateral midshaft clavicle fracture and AC joint injury is not well described with an incidence of 0.09%-6.8%[10,11]. The most common AC joint dislocations associated with midshaft clavicle fracture were Rockwood type 2 and type 3, respectively[10].
The mechanism of such injuries is not well understood, but it is thought to be a direct blow to the affected shoulder associated with a rotational force, with a fall from a motorized two-wheeler being the most common mechanism of injury[11].
AC joint dislocation should be thought of when evaluating a patient with a clavicle fracture. Conventional plain radiography can usually detect AC joint dislocations Rockwood types 3, 5, and 6. Additional axillary radiographs should be done to avoid missing, misclassification, and underestimation of Rockwood type 2 and 4 dislocations. Stress testing of AC joint stability should be done after operative fixation of clavicle fractures that undergoes surgical management to avoid pain, disfunction, and disability associated with such missed injuries[11].
There is no consensus on the optimal management of such injuries[11]. There is a preference in literature to manage such cases with associated bone and soft-tissue injuries surgically to expedite regaining range of motion and prevent stiffness, especially in Rockwood type 3 or higher AC joint dislocations[11]. The surgical treatment strategy and implant choice for such injuries are still controversial. The most common surgical strategy to manage such cases is open reduction and internal fixation of clavicle fractures, AC, and CC ligaments repair or reconstruction in different ways[11].
Missed AC joint dislocations in combination with mid-shaft clavicle fractures can lead to conservative treatment of “isolated” clavicle fractures. Continued pain, disability, and limitations of activities of daily living could result in such missed injuries[12].
AC joint primary osteoarthritis (OA) is more common than glenohumeral primary OA, Although AC joint post-traumatic OA is even more prevalent[13]. AC joint OA has been shown following Rockwood grade 1 and 2 in 8% and 42% of patients, respectively[14]. Absence and removal of AC joint intra-articular disc which is usually done to aid in the reduction of AC joint injuries are associated with accelerated AC joint OA[15].
In our case, reduced AC joint and complete fracture healing were achieved. Functional and radiographic outcomes were excellent.
Combined midshaft clavicle fractures and AC joint dislocations are considered quite rare. Timely diagnosis of such injuries leads to great functional outcomes. AC joint dislocation should be suspected with midshaft clavicle fractures and should be investigated radiologically and clinically in an appropriate manner. Still, there is no consensus on the optimal management of such injuries, with simultaneous surgical management of both injuries with Rockwood type 3 or higher being preferred.
| 1. | Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg Am. 2009;91:447-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 220] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 2. | Sirin E, Aydin N, Mert Topkar O. Acromioclavicular joint injuries: diagnosis, classification and ligamentoplasty procedures. EFORT Open Rev. 2018;3:426-433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 49] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Bakir MS, Carbon R, Ekkernkamp A, Schulz-Drost S. Monopolar and Bipolar Combination Injuries of the Clavicle: Retrospective Incidence Analysis and Proposal of a New Classification System. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 4. | Balcik BJ, Monseau AJ, Krantz W. Evaluation and treatment of sternoclavicular, clavicular, and acromioclavicular injuries. Prim Care. 2013;40:911-923, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Nakazawa M, Nimura A, Mochizuki T, Koizumi M, Sato T, Akita K. The Orientation and Variation of the Acromioclavicular Ligament: An Anatomic Study. Am J Sports Med. 2016;44:2690-2695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Song HS, Kim H. Current concepts in the treatment of midshaft clavicle fractures in adults. Clin Shoulder Elb. 2021;24:189-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 7. | Berthold DP, Muench LN, Dyrna F, Mazzocca AD, Garvin P, Voss A, Scheiderer B, Siebenlist S, Imhoff AB, Beitzel K. Current concepts in acromioclavicular joint (AC) instability - a proposed treatment algorithm for acute and chronic AC-joint surgery. BMC Musculoskelet Disord. 2022;23:1078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 35] [Reference Citation Analysis (0)] |
| 8. | Younis F, Sultan J, Dix S, Hughes PJ. The range of the Oxford Shoulder Score in the asymptomatic population: a marker for post-operative improvement. Ann R Coll Surg Engl. 2011;93:629-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Keener JD. Acromioclavicular Joint Anatomy and Biomechanics. Oper Tech Sports Med. 2014;22:210-213. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Ottomeyer C, Taylor BC, Isaacson M, Martinez L, Ebaugh P, French BG. Midshaft clavicle fractures with associated ipsilateral acromioclavicular joint dislocations: Incidence and risk factors. Injury. 2017;48:469-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | van de Voort JC, van Doesburg PG, Leijnen M. Ipsilateral Rockwood type IV acromioclavicular joint dislocation and midshaft clavicle fracture: a case report and review of the literature. JSES Rev Rep Tech. 2023;3:236-241. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Mohammed KD, Stachiw D, Malone AA. Type IV acromioclavicular joint dislocation associated with a mid-shaft clavicle malunion. Int J Shoulder Surg. 2016;10:37-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Shaffer BS. Painful conditions of the acromioclavicular joint. J Am Acad Orthop Surg. 1999;7:176-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 58] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Taft TN, Wilson FC, Oglesby JW. Dislocation of the acromioclavicular joint. An end-result study. J Bone Joint Surg Am. 1987;69:1045-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 205] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Buttaci CJ, Stitik TP, Yonclas PP, Foye PM. Osteoarthritis of the acromioclavicular joint: a review of anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil. 2004;83:791-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |