INTRODUCTION
In patients with paediatric hip disorders, such as hip dysplasia, septic arthritis, Legg-Calvé-Perthes, slipped capital femoral epiphysis, or post-traumatic conditions, total hip arthroplasty (THA) presents a significant challenge for orthopaedic surgeons[1]. These patients are generally younger than the typical population undergoing THA and have greater functional demands. Therefore, achieving optimal biomechanical conditions is of paramount importance. This includes positioning the acetabulum at the ideal centre of rotation and ensuring a stable femoral component with sufficient offset to preserve abductor muscle function and restore leg length because life expectancy and the need for longevity of THA is greater[2-4]. The altered anatomy resulting from these disorders, coupled with previous reconstructive procedures performed during childhood, complicates the THA procedure. As a result, thorough preoperative imaging and planning, alongside an individualised surgical approach, are essential to success in these cases[5,6]. In this paper, we present possible treatment options and outline our preferred techniques for THA in young patients with sequelae from paediatric hip diseases.
SPECIFIC OPERATIVE TECHNIQUES IN PATIENTS WITH PEDIATRIC HIP SEQUELAE
The primary consideration when performing THA in young patients with paediatric hip sequelae is to ensure best possible long-term outcome of the prosthesis, which is accomplished by restoring proper anatomical and biomechanical alignment. This can be challenging because of insufficient acetabular bone thickness, irregular femoral anatomy, altered femoral head shape, changes in femoral neck length, variations in neck-shaft angle and issues such as increased or decreased anteversion, muscle contracture, and leg-length discrepancy[7,8]. Additionally, leg-length discrepancy is a critical issue that must be addressed, and maintaining good soft tissue balance while retaining the continuity of the abductor muscles is essential for a favourable postoperative functional outcome[9,10].
Detailed preoperative imaging is crucial for effective surgical planning. Standard radiographs are often insufficient to gather all the necessary information. Computed tomography should be the gold standard in diagnostics, as it provides more comprehensive data on acetabular bone stock, orientation of the acetabulum, femoral head and neck alignment, and the shape of the femoral canal. Preoperative planning software offers precise information regarding the size and orientation of the acetabular and femoral components and, most importantly, helps determine the ideal centre of rotation[11].
Positioning the acetabular component can be challenging due to the loss of anatomical landmarks. Achieving the correct balance of cup size, inclination, anteversion, and coverage is essential for stability. But for longevity, most important is to place the acetabulum at the ideal centre of rotation. This is because for every 1 mm of lateral placement of the cup, hip load increases by 0.7%, while every millimetre of proximalization raises the load by 0.1%[12]. Often, in these patients, bone stock at the position of the true centre of rotation is insufficient and acetabular component must be additionally augmented superolateral with the bone graft or metal augments. Un-coverage of cementless acetabular cups for more than 30% must be covered[13,14]. In this cases grafts can be used (structural allografts, free or vascularized autografts)[15-19]. Insufficient acetabular bone stock can also be improved with trabecular metal augments or custom shaped acetabular components[20,21]. There are potential problems related to bone grafts like delayed healing or non-healing. The main issue with metal augments is deficit of bone stock for future revision or difficulties in removal of the component in case of infection[21].
The ideal technique involves medialising the acetabular component as much as possible to reduce the hip load while avoiding complications from superolateral segment coverage. Cotyloplasty is technique that allows us exactly that. It includes deliberate fracture of the medial side (bottom) of acetabulum and placing a cup more medially, beyond the Kohler’s ilioischial line. Although originally performed with cemented cups, uncemented porous acetabular cups have recently shown better outcomes[22-24]. This method includes controlled reaming of the bone from acetabulum until medial wall becomes paper-thin. Any hole in acetabulum, and medial side of acetabulum is jam-packed with cancellous bone, after which the press fit cup is inserted. In this way, acetabular component is medialized and cancellous bone between cup and paper-thin medial wall will allow preserving the bone stock for future revision surgeries, what is quite important for these young patients. Acetabular component is additionally stabilized with screws for better primary stability, and with time, bone ingrowth will provide the secondary stability of acetabular component (Figure 1). In such manner hip biomechanics and leg length are restored, reducing the risk for impingement and dislocation. Potential obstacle of cotyloplasty is the difficulty in controlling the extent of the medial wall fracture, which can lead to complications, for example dislocation of the cup into the pelvis[24]. In an in vitro study we published in 2023, using pig pelvises, we established guidelines for preserving the primary stability of the acetabular component. Our results indicate that, under a load of 700 N, the acetabular component remains stable if the medial wall defect is lower than 68% of its diameter or if the uncovered surface area is no greater than 27%. For higher loads of 1000 N, stability is maintained as long as the defect is less than 45% and uncoverage is less than 18%[25].
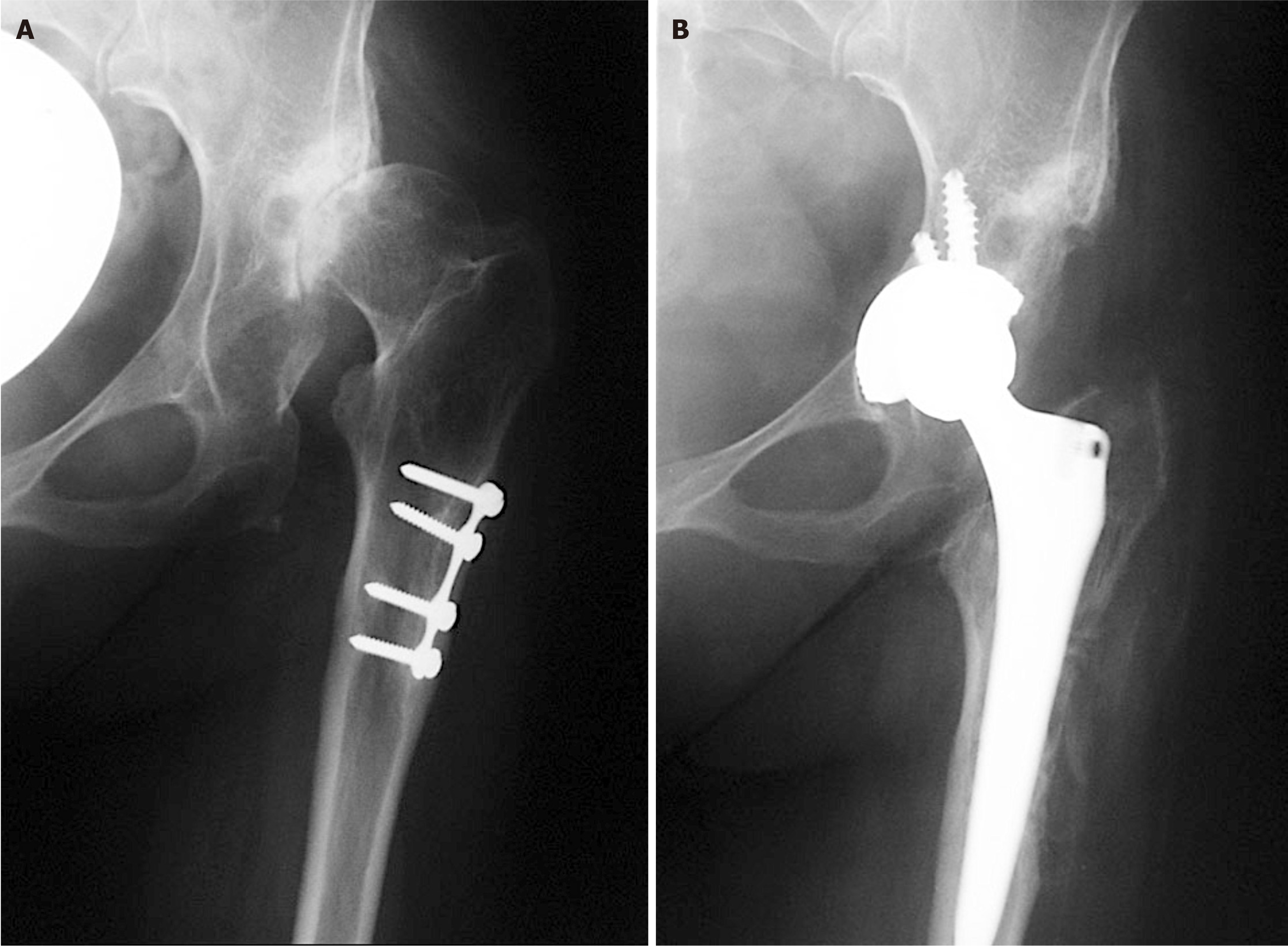
Figure 1 X-rays of left hip.
A: Preoperative X-ray of a patient with secondary osteoarthritis of the left hip due to dysplasia. Plate and screws in the proximal femur are left from the previous surgery performed in childhood; B: Postoperative X-ray with implanted uncemented acetabular cup and femoral stem. Acetabular cup is protruding beyond the Kohler’s line inside the pelvis and secured with 3 additional screws. Lesser trochanter is brought distally to the normal level so there is no leg length discrepancy postoperatively.
Femoral component placement in patients with paediatric hip sequelae is also complex due to altered anatomy, particularly after corrective osteotomies, osteoporotic or sclerotic bone, and narrow medullary canals. In some cases, a standard femoral stem cannot be used, requiring a modular stem instead[1]. Femur is often too long and must be shortened. Shortening is necessary for achieving position of endoprosthesis in ideal centre of rotation, correction of proximal femoral anteversion and to avoid sciatic nerve stretching. Additionally, the hip’s abductor mechanism is restored, resulting in same leg length[25]. Over time, various types of femoral shortening osteotomies have been developed. These can be classified based on the location of the osteotomy into proximal, distal and femoral shaft osteotomies[26-30].
Our preferred approach for THA in patients with paediatric hip sequalae is previously published, a variation of the direct lateral hip approach[9]. During approach, the front half is separated with a flake of bone from the greater trochanter, while remaining connected to the uninterrupted tendons of the gluteus medius and vastus lateralis. The same process is applied to the posterior portion, detaching it with the chisel, leaving a thicker bone flake. This technique strips the muscles from the greater trochanter without performing a trochanteric osteotomy. It preserves the continuity of the abductor muscles, allowing the femur to be shortened without impacting the muscles to much (it splits the continuous tendon only longitudinally) (Figure 2). This approach allows faster recovery and reduces complications related to trochanteric osteotomy[9]. We have used this technique for more than 10 years with good results in more than 65 patients. Initial results for first 12 patients were published with follow up of 2 years[9]. The average Harris hip score was 96.7 (range 92.2-100). The limb lengths were measured before and after the surgery, and after surgery the leg length difference was less than 5 mm in 11 of the 12 patients. Also, medialisation of the cup relative to the ideal centre of rotation according to method of Ranawat et al[31] was on average 8 mm. None of the patients limped or had positive trendelenburg sign, and no one had a peroneal nerve palsy. Additional results for 19 patients were analysed and presented previously. In this cohort some of the results were: Average medialization of the cup (protrusion of the cup bellow the ischio-ileal line) was 6.6 mm ± 2.9 mm (range 2.2-11.5 mm). Average protrusion of the acetabulum in the pelvis was 46% ± 20% (range 7%-77%). In 4 out of 19 cases acetabulum was partially uncovered. In those 4 cases average lateral cup placement was 6.5 mm ± 3.7 mm (range 3.3-10.2 mm). In one case where the cup was medialized 9.6 mm, postoperative instability happened and cup was revised. For revision we used bigger cementless cup and additional grafting of the bottom. Long term follow-up of the patients is underway which mostly focuses on possible long-term deterioration of functional outcome (if any) and Kaplan–Meier survivorship analysis with aseptic loosening and revision as endpoint which is beyond the scope of this paper.
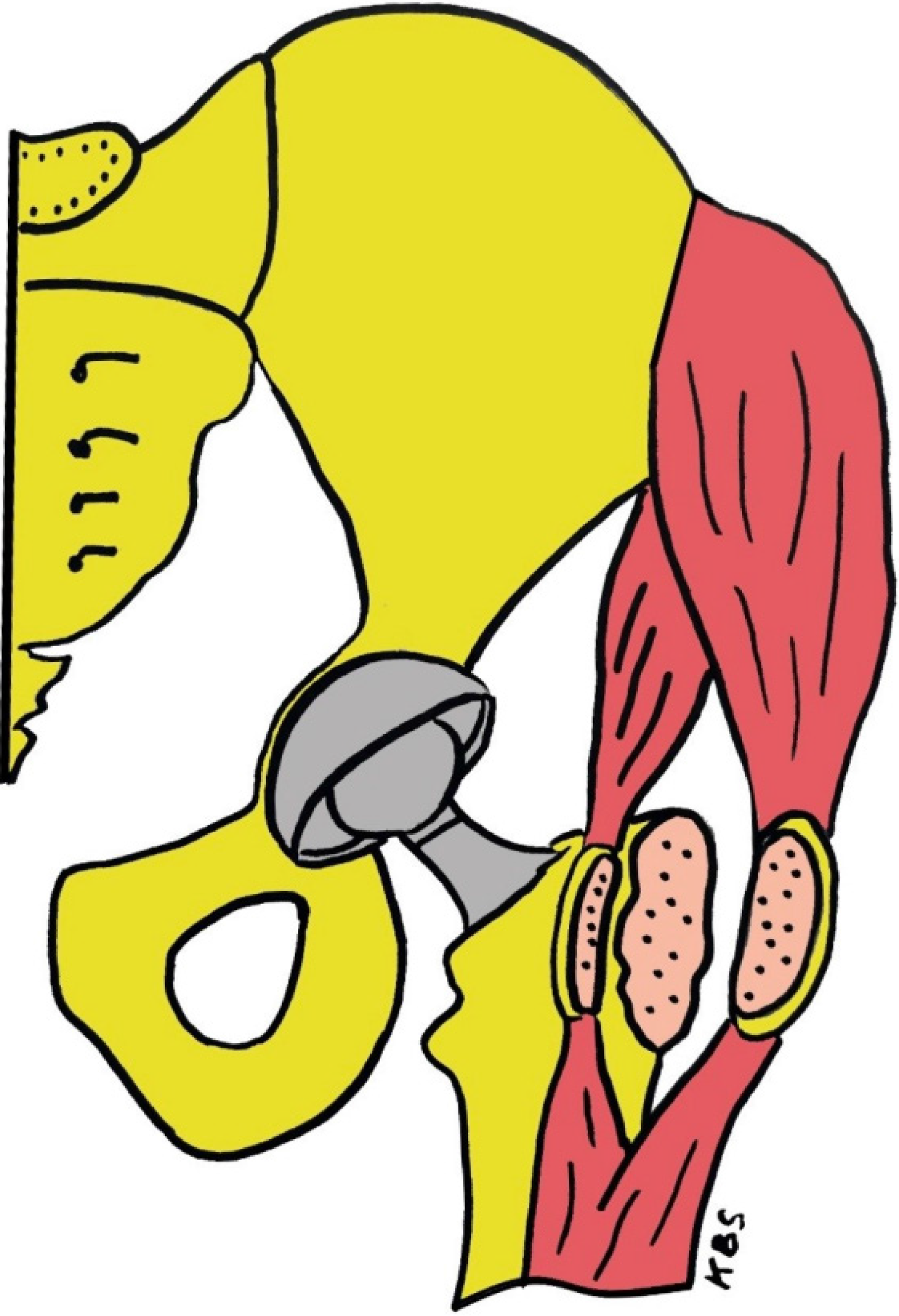
Figure 2 Drawing of our prefer method of treatment.
Acetabular cup is medialized (cotyloplasty) so that the dome of the cup is protruding beyond Kohler’s line inside the pelvis. On the femoral side anterior and posterior half of the continuous tendon is mobilized by a chisel. First the anterior part is divided with a thin layer of bone from the greater trochanter but remains attached to the continuous tendon of the gluteus medius and the vastus lateralis. And the same is done with the posterior half of the continuous tendon of the gluteus medius and the vastus lateralis which are detached with the chisel leaving a bone flake of at least 2 mm to 3 mm thickness attached to tendons. With that procedure continuity of abductor muscles is preserved and femur can be shortened without affecting the muscles. KBS: Critical region for definable segment defects.