Published online Nov 18, 2024. doi: 10.5312/wjo.v15.i11.1101
Revised: October 3, 2024
Accepted: October 20, 2024
Published online: November 18, 2024
Processing time: 67 Days and 4.7 Hours
Chronic synovitis due to chronic knee gouty arthritis (KGA) resulting in synovial hyperplasia has not been documented in the current literature, and thus the optimal management for this condition remains unclear. This case report dis
A 34-year-old man presented to our outpatient clinic with a 5-year recurrent knee effusion and a history of chronic KGA. Symptoms persisted despite serial as
Arthroscopic synovectomy for synovial hyperplasia in chronic KGA sufficiently eradicates the symptoms of recurrent knee effusion.
Core Tip: Recurrent knee effusion in cases of chronic knee gouty arthritis (KGA) that are refractory to conservative treatment should alert surgeons to the possibility of synovial structural alteration, such as synovial hyperplasia. Diagnostic arthroscopy should be considered in these cases to allow a definitive diagnosis. In our case, tophi deposition and excessive synovial membrane thickening were observed intraoperatively. Therefore, partial synovectomy was performed to address the excessive synovial tissue. At six months, no further episode of recurrent knee effusion. These findings suggest that an arthroscopic synovectomy was effective in managing synovial hyperplasia in the case of chronic KGA.
- Citation: Utoyo GA, Calvin C. Arthroscopic synovectomy for synovial hyperplasia in chronic knee gouty arthritis: A case report. World J Orthop 2024; 15(11): 1101-1108
- URL: https://www.wjgnet.com/2218-5836/full/v15/i11/1101.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i11.1101
Knee gouty arthritis (KGA) is one of the most prevalent inflammatory arthritis among the adult population. This results from either an abnormally high purine production or an abnormal excretion of uric acid, leading to the deposition of monosodium urate crystals within the joint space[1,2]. The disease can progress to the form of chronic gouty arthritis, often manifesting as a case accompanied by chronic synovitis, bony erosions, cartilage damage, and tophi formation[3]. The chronic form of the disease is often debilitating, as it leads to significant pain, activity limitation, and reduced quality of life[4].
Although chronic synovitis has been found to be correlated with chronic KGA, its impact and consequences have not been thoroughly discussed in the literature[5,6]. This is mainly because most cases of chronic synovitis will resolve itself after being adequately managed with urate-lowering medication[7]. So far, the presentation of chronic synovitis resulting in synovial hyperplasia has never been documented in a case of chronic KGA. In this case report, we present an unusual case of a 34-year-old male with a 5-year history of recurrent knee effusion and chronic KGA. This patient was revealed to have synovial hyperplasia, which was related to chronic KGA, and successfully treated with arthroscopic synovectomy.
A 34-year-old man presented at our outpatient clinic with symptoms and a history of recurrent left knee effusion that occurred approximately five years ago.
The recurrent knee effusion was accompanied by pain and limitation of knee extension and flexion. The patient describes mild-to-moderate difficulty in performing daily activities. There was no history of recent or previous trauma.
The symptoms began approximately 5 years prior to consult at our department, during which the patient regularly visited the internal medicine outpatient clinic once a month for allopurinol therapy. However, despite treatment from the internal medicine physicians, the patient still experienced recurrent of knee effusion. A familial history of hyperuricemia was noted, but none of the patient's family member experienced the same symptoms.
No relevant family history has been identified.
Upon examination, left knee effusion was detected. Active and passive movement of the left knee was complete, but the patient experienced mild pain at full flexion. The Lachman test, anterior drawer test, posterior drawer test, varus stress test, valgus stress test, and McMurray test yielded negative results.
An initial laboratory examination at our outpatient clinic revealed a uric acid level of 684.08 μmol/L, and this had a hi
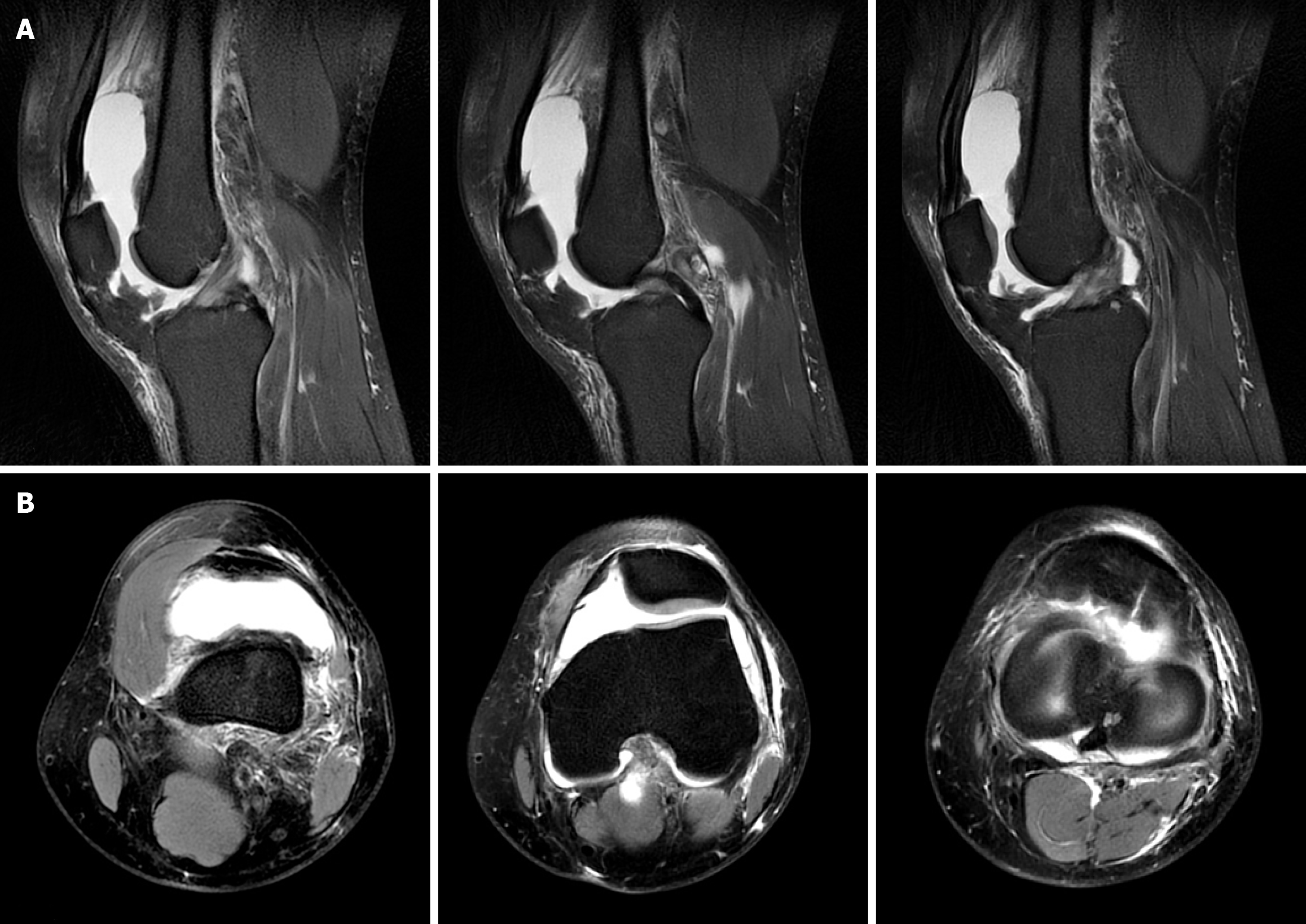
A plain left knee radiograph revealed no abnormalities (Figure 1). Magnetic resonance imaging revealed synovitis and supra- and infra-patellar recess effusion (Figure 2).
Several differential diagnoses for this unusual symptom other than gouty arthritis were considered, including septic arthritis, tuberculous synovitis, rheumatoid arthritis (RA), pigmented villonodular synovitis (PVNS), and synovial chondromatosis. Based on diagnostic arthroscopy and confirmation from synovial biopsy, the final diagnosis was synovial hyperplasia related to chronic KGA.
The patient was initially managed conservatively for 2 months with serial synovial aspiration (once every 2 weeks) and urate-lowering medication (febuxostat 80 mg once daily), but the recurrent knee effusion persisted. Due to the failure of conservative treatment, diagnostic arthroscopy was planned for this patient.
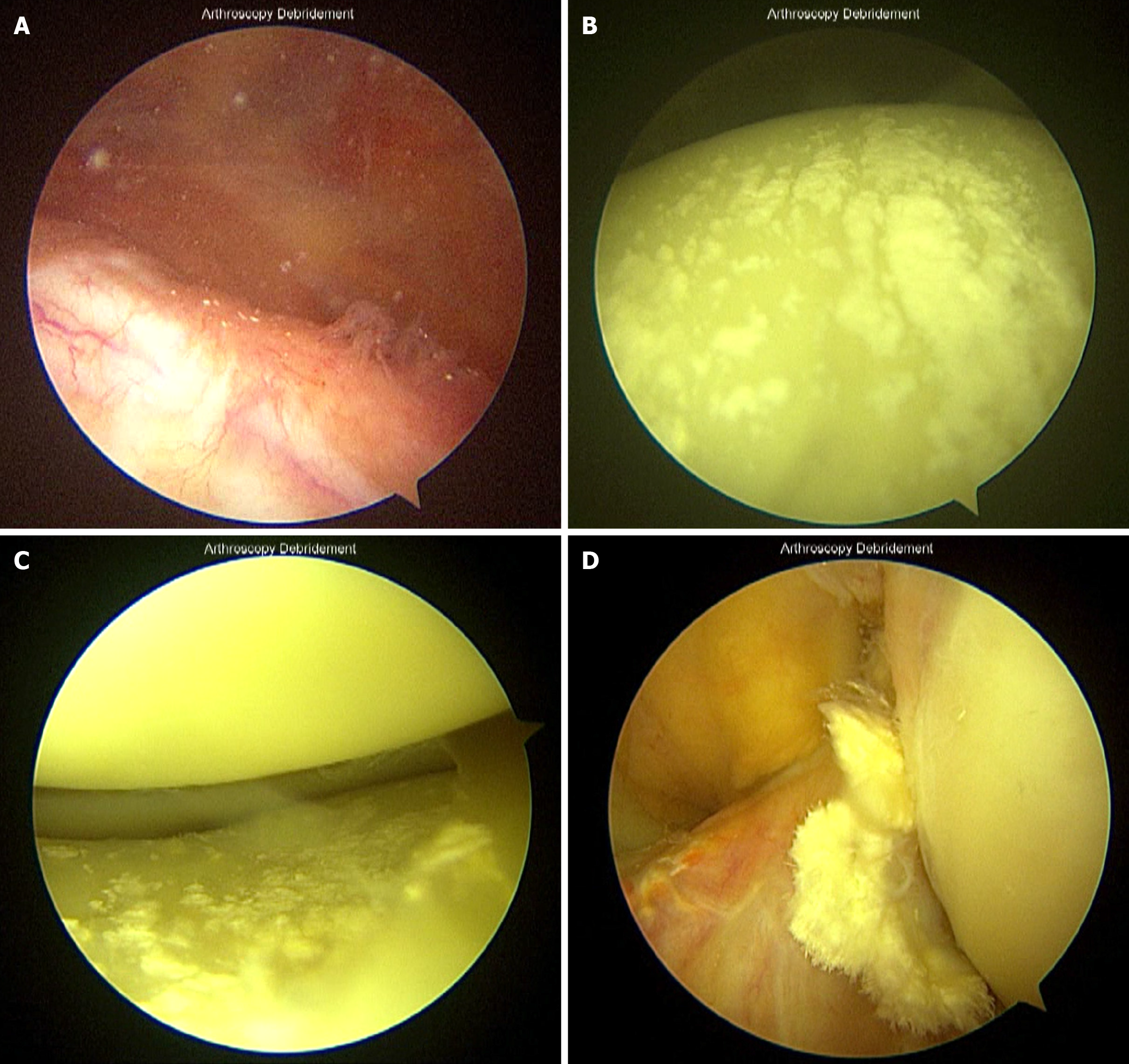
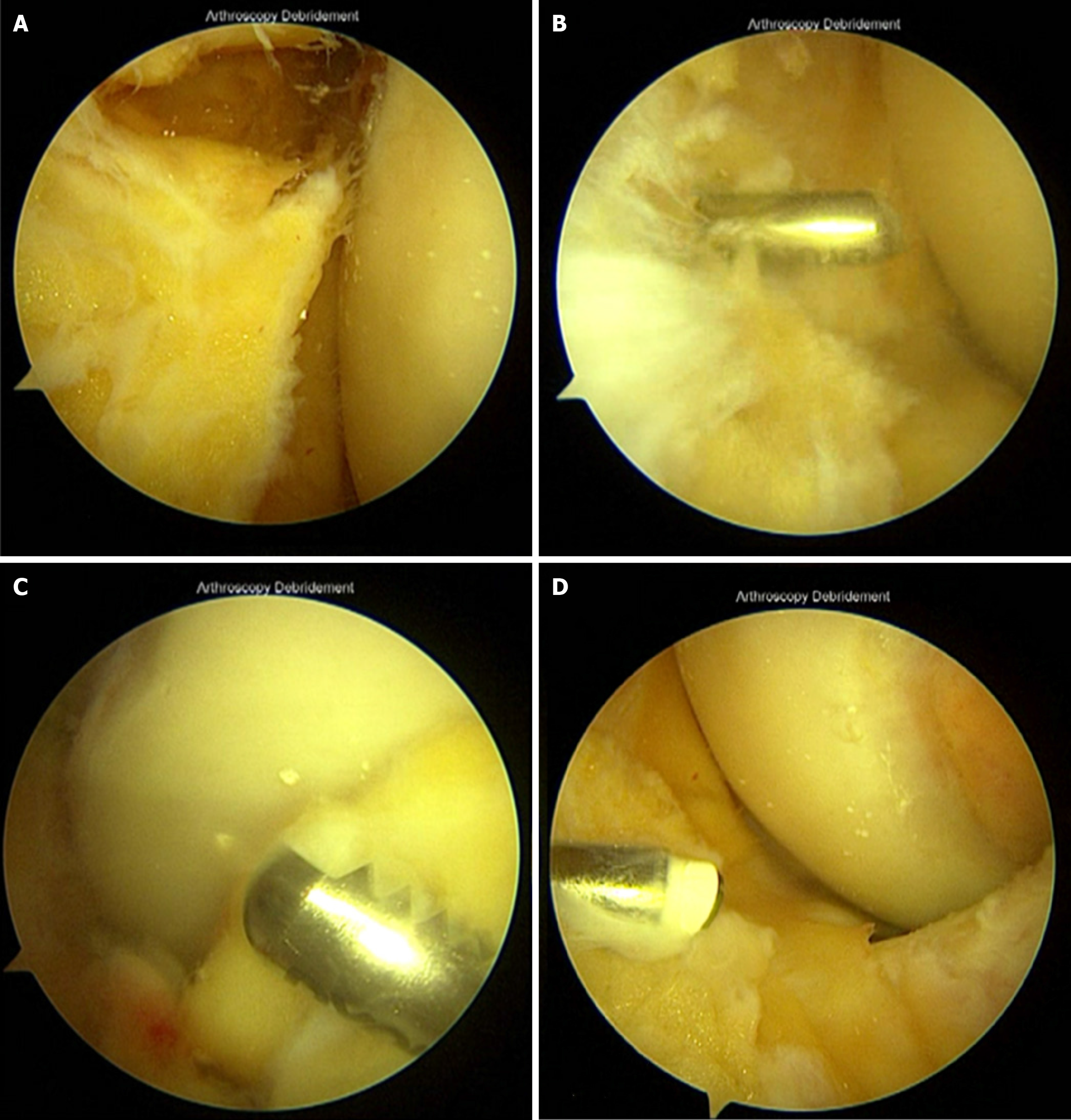
After draping the patient in a sterile fashion, an arthroscopic trochar was inserted to collect the synovial fluid for culture analysis, then, diagnostic arthroscopy was performed. After inserting the viewing portal, floating tophi, characterized as a white chalky substance was observed (Figure 3A). Deposition of this tophi was also observed over the femoral condyle (Figure 3B), tibial plateau, and meniscus (Figure 3C), as well as on the surface of the anterior cruciate ligament (ACL) (Figure 3D). Hook probes were used to carefully release the tophi from the cartilage surface. A shaver was used to debride tophi from the ACL surface. An extensive thickening synovium membrane was observed (Figure 4A). Afterward, partial synovectomy was performed through an anterolateral (Figure 4B) and anteromedial (Figure 4C) portal, then, a radiofrequency was applied to the synovium surface (Figure 4D). The synovium was sampled for biopsy using an arthroscopic punch. This procedure aimed to identify pathological change in the synovium and exclude any synovial malignancy resulting in productive synovial fluid.
Follow-up appointments were scheduled for 1 and 2 weeks, 1, 2, and 6 months postoperatively. Following the procedure, febuxostat was started at a dose of 80 mg daily for two months. A week after the initial procedure, the synovial biopsy results came out, revealing chronic synovitis with synovial hyperplasia. This feature was consistent with chronic KGA. No pathological change of cells within the synovium or granulomatous inflammation was observed. Hence, synovial tumor (PVNS and synovial chondromatosis) and tuberculous synovitis were ruled out. Two weeks postoperatively, knee effusion was observed, but synovial fluid aspiration was not performed. Knee flexion and extension were limited 30° and 10°, respectively, thus prompting referral to the rehabilitation unit for range of motion exercises. One month postoperatively, a slight knee effusion of approximately 12 mL was observed, but this is considered a normal occurrence post-arthroscopic surgery. Knee flexion improved to 90°, but knee extension was still limited to 10°. Two months postoperatively, the patient achieved knee flexion and extension of 130° and 0°, respectively. Laboratory tests revealed a uric acid level of 333.12 μmol/L. Subsequently, the patient reported no episodes of knee effusion. Six months postoperatively, the patient reported no further episodes of knee effusion, with only slight discomfort at the portal scar when squatting or kneeling. Outcomes were assessed using the International Knee Documentation Committee score, which improved from 72.41 preoperatively to 96.66 postoperatively at 6 months. Table 1 outlines the timeline of the patient's symptoms and treatment.
| Date | Event |
| 2018 to November, 2023 | History of recurrent left knee effusion and chronic knee gouty arthritis |
| History of allopurinol therapy from the internal medicine department for five years | |
| November 17, 2023 | Patient consulted at our outpatient clinic for recurrent left knee effusion |
| Plain left knee radiograph revealed no abnormalities | |
| Leukocyte count: 14.43 × 109/L, C-reactive protein: 14 mg/L, and uric acid: 684.08 µmol/L | |
| Synovial fluid aspiration was performed | |
| Conservative management: Serial synovial fluid aspiration and febuxostat 80 mg/day | |
| January 26, 2024 | The symptom of recurrent left knee effusion persisted |
| Uric acid: 553.21 µmol/L, and rheumatoid factor: Negative | |
| Synovial fluid culture: no growth of microorganisms | |
| MRI: Synovitis and large knee effusion | |
| Arthroscopic procedures were planned for diagnostic confirmation. Several differential diagnoses other than gouty arthritis, including: Septic arthritis, tuberculous synovitis, pigmented villonodular synovitis, and synovial chondromatosis | |
| Pre-operative IKDC score: 72.41 | |
| January 31, 2024 | Patient underwent an arthroscopic procedure |
| Sterile synovial fluid was obtained for culture analysis | |
| Intraoperative findings revealed synovial thickening and tophi deposition | |
| Synovial biopsy and synovectomy were performed | |
| February 7, 2024 (one weeks postoperatively) | Synovial biopsy: chronic synovitis with synovial hyperplasia that was consistent with chronic knee gouty arthritis |
| Culture of sterile synovial fluid: No growth of microorganisms | |
| August 23, 2024 (six months postoperatively) | Patient reported no further episodes of knee effusion |
| IKDC score: 96.66 |
Several unusual presentations of chronic KGA have been previously documented, including tophi mimicking a soft tissue mass[8], knee locking resembling meniscal tears[9], and tophi causing spontaneous ACL rupture[10,11]. In this case report, we present a rare occurrence of synovial hyperplasia in chronic KGA resulting in recurrent knee effusion for over five years, which has never been described in previous literature. Our case highlights the debilitating nature of chronic KGA and its significant impact on the patient's quality of life. This case also emphasizes the utility of arthroscopic procedures in managing the chronic form of KGA.
The arthroscopic management of KGA has been described in several reports, particularly the washout procedure. This procedure is mainly reserved for chronic cases, such as those with a symptomatic intra-articular tophaceous mass or KGA with concomitant septic arthritis. Gong et al[12] reported the uses of arthroscopic washout procedure in several conditions, including refractory gout, acute gouty arthritis not relieved by colchicine and non-steroidal anti-inflammatory drugs, and chronic gouty arthritis with severe joint pain. The combination of arthroscopic washout procedure and febuxostat was found effectively reduced uric acid levels and the number of acute flares.
Conversely, arthroscopic synovectomy alone has rarely been performed in the case of KGA. The use of this procedure is most well-known for recalcitrant chronic synovitis among RA patients[13,14]. In the study of Roch-Bras et al[15], approximately 70.7% of patients with RA had good clinical outcomes after being managed with arthroscopic synovectomy, with a mean follow-up of 8.9 years. This procedure resulted in decreased pain and recurrent effusion episodes, as well as improved knee range of motion. Based on those results, we hypothesized that the same principle also applies for the management of synovial hyperplasia among patients with chronic KGA.
Structural changes within the synovial membrane among patients with chronic articular inflammation might cause increased synovial fluid production within the joint cavity. Therefore, the presence of effusion can be a sensitive indicator for any synovial pathology[15]. In the present case, the excess synovial tissue seen on arthroscopy prompted us to perform a biopsy and partial synovectomy. Radical synovectomy was avoided, as the synovial hyperplasia was mostly less aggressive compared to cases of RA[16].
Although the form of synovitis in a case of chronic KGA has been reported in the ultrasonography study by Zheng et al[5], to our knowledge, no studies and reports have ever documented synovial structural alteration directly through diagnostic arthroscopy or biopsy. In our case, after the follow-up period, partial synovectomy was found to successfully eliminated the recurrent knee effusion symptoms related to synovial hyperplasia. Nevertheless, our report had a limited follow-up duration. Further studies should include a longer follow-up to determine the long-term outcomes of arthroscopic partial synovectomy for synovial hyperplasia in chronic KGA.
We reported an unusual case of chronic KGA in which the patient complained of recurrent knee effusion related to synovial hyperplasia. The symptoms persisted despite adequate conservative treatment. Arthroscopic synovectomy successfully addressed the patient's symptoms. This report suggests that synovial hyperplasia should be considered as a cause of recalcitrant knee effusion among patients with chronic KGA. Arthroscopic procedure should be offered as a definitive diagnostic procedure and definitive treatment for synovial hyperplasia.
| 1. | Wang Q, Chen B, Zhang Z, Tang X, Li Y. Correlations of characteristics with tissue involvement in knee gouty arthritis: Magnetic resonance imaging analysis. Heliyon. 2024;10:e31888. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Weaver JS, Vina ER, Munk PL, Klauser AS, Elifritz JM, Taljanovic MS. Gouty Arthropathy: Review of Clinical Manifestations and Treatment, with Emphasis on Imaging. J Clin Med. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 3. | Ragab G, Elshahaly M, Bardin T. Gout: An old disease in new perspective - A review. J Adv Res. 2017;8:495-511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 299] [Cited by in RCA: 307] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 4. | Singh JA. Quality of life and quality of care for patients with gout. Curr Rheumatol Rep. 2009;11:154-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Zheng W, Lu P, Jiang D, Chen L, Li Y, Deng H. An ultrasonographic study of gouty arthritis: Synovitis and its relationship to clinical symptoms: A retrospective analysis. Health Sci Rep. 2023;6:e1312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Carter JD, Patelli M, Anderson SR, Prakash N, Rodriquez EJ, Bateman H, Sterrett A, Valeriano J, Ricca LR. An MRI assessment of chronic synovial-based inflammation in gout and its correlation with serum urate levels. Clin Rheumatol. 2015;34:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Kraev KI, Geneva-Popova MG, Hristov BK, Uchikov PA, Popova-Belova SD, Kraeva MI, Basheva-Kraeva YM, Stoyanova NS, Mitkova-Hristova VT. Celebrating Versatility: Febuxostat's Multifaceted Therapeutic Application. Life (Basel). 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 8. | Patel UJ, Freetly TJ, Yueh J, Campbell C, Kelly MA. Chronic Tophaceous Gout Presenting as Bilateral Knee Masses in an Adult Patient: A Case Report. J Orthop Case Rep. 2019;9:16-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Espejo-Baena A, Coretti SM, Fernandez JM, Garcia-Herrera JM, Del Pino JR. Knee locking due to a single gouty tophus. J Rheumatol. 2006;33:193-195. [PubMed] |
| 10. | Hwang HJ, Lee SH, Han SB, Park SY, Jeong WK, Kim CH, Lee DH. Anterior cruciate ligament rupture in gouty arthritis. Knee Surg Sports Traumatol Arthrosc. 2012;20:1540-1542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Lubis AMT, Reksoprodjo AY, Kuncoro MW, Ifran NN. Post-ACL Reconstruction Graft Failure in Severe Gout Arthritis Patient. Int Med Case Rep J. 2021;14:725-730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 12. | Gong Z, Xia L, Xu R, Luo M, Deng H, Kang Z, Liu L, Liu Y, Zhang F, Shi J. The Clinical Effects of Febuxostat Alone or Combined with Arthroscopic Surgery for Gout: A Single-Center Retrospective Study. J Inflamm Res. 2021;14:4509-4517. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Lipina M, Makarov M, Mukhanov V, Karpashevich A, Maglevaniy S, Amirdjапоvа V, Archipov S. Arthroscopic synovectomy of the knee joint for rheumatoid arthritis. Int Orthop. 2019;43:1859-1863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Ogilvie-Harris DJ, Basinski A. Arthroscopic synovectomy of the knee for rheumatoid arthritis. Arthroscopy. 1991;7:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Roch-Bras F, Daurès JP, Legouffe MC, Sany J, Combe B. Treatment of chronic knee synovitis with arthroscopic synovectomy: longterm results. J Rheumatol. 2002;29:1171-1175. [PubMed] |
| 16. | Agudelo CA, Schumacher HR. The synovitis of acute gouty arthritis. A light and electron microscopic study. Hum Pathol. 1973;4:265-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 53] [Article Influence: 1.0] [Reference Citation Analysis (0)] |