Published online Nov 18, 2024. doi: 10.5312/wjo.v15.i11.1088
Revised: September 4, 2024
Accepted: October 15, 2024
Published online: November 18, 2024
Processing time: 276 Days and 5.3 Hours
Aneurysmal bone cyst (ABC) is a benign cystic of unknown etiology, characterized by multiple chambers and a high recurrence rate. Current treatment op
An 11-year-old boy was presented with an accidental fracture of his right leg. Despite having been examined at other hospitals, he had not received treatment. Given the potential for significant bone defects and the difficulty of the surgery, our doctors opted to use the Ilizarov technique to minimize harm to the patient. Upon admission, the patient underwent a needle biopsy and complete tumor resection-the Ilizarov technique assisted in the transport and reconstruction of the autologous femoral bone. Postoperatively, the patient exhibited regular follow-ups, during which bone transport was gradually performed, and the external fixation frame was removed on time. Follow-up X-rays of the right lower limb displayed no tumor recurrence, with a normal appearance. Bone formation at the cutting site was satisfactory, and the union of the bone ends indicated good healing. After two years of follow-up, the patient had essentially returned to normal.
We successfully applied the Ilizarov technique to treat ABC, reducing the financial burden of patients and the pain of multiple surgeries. In cases where significant bone defects occur, the Ilizarov technique has demonstrated satisfactory therapeutic outcomes.
Core Tip: This is a case report on the treatment of a pediatric patient with a large aneurysmal bone cyst of the distal femur using the Ilizarov technique. The surgical procedure of the patient was mainly documented. The patient was followed up for two years after the surgery, and the clinical healing and functional recovery of the patient were evaluated.
- Citation: Long XY, Sun F, Wang T, Li P, Tian Z, Wu XW. Ilizarov technique for treatment of a giant aneurysmal bone cyst at the distal femur: A case report. World J Orthop 2024; 15(11): 1088-1094
- URL: https://www.wjgnet.com/2218-5836/full/v15/i11/1088.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i11.1088
There are a variety of methods for benign bone neoplasia. Most of the early surgical methods are tumor lesion curettage and internal fixation with bone graft. However, long-term postoperative follow-up shows high recurrence rate, high rate of bone nonunion and high incidence of pathological fracture. There are more problems and challenges for children. For example, when the tumor is removed, where does the bone graft in children come from? The risk of bone resorption and rejection is greater when allogeneic bone is used. Therefore, after the introduction of bone transfer technology into China, following the principles of Lizarov technology, some doctors began to use external fixation system and single-arm external fixation system to carry out bone transfer technology to treat benign bone tumors, and problems such as postoperative tumor recurrence, bone graft difficulty, bone nonunion, pathological fracture and so on have been well solved. This case report describes the treatment of a pediatric patient with a large aneurysmal bone cyst (ABC) of the distal femur using the Ilizarov technique. The surgical procedure was thoroughly documented, and the patient was followed up for two years post-surgery to evaluate clinical healing and functional recovery.
Swelling and pain in the right knee, with limited movement for one week.
The mother reported that about a week ago, the child accidentally fell, resulting in swelling and pain in the right knee and restricted movement. They immediately sought medical attention at an external hospital, and after physical and X-rays examinations, the attending physician suspected a bone lesion in the distal right femur. However, no treatment was administered at that time. Currently, the family visits our outpatient clinic for continued care.
The little boy had been in good health before the fall.
There were no genetic disorders in his family.
Physical examination revealed general normal conditions. A focused examination of the right thigh indicated significant swelling on the outer side of the distal femur tenderness, and percussion tenderness. The skin temperature of the affected area was slightly higher than that of the healthy side, but the skin color appeared normal. There was limited movement in the affected limb, but peripheral blood circulation and nerve function were normal.
Nothing abnormal was detected.
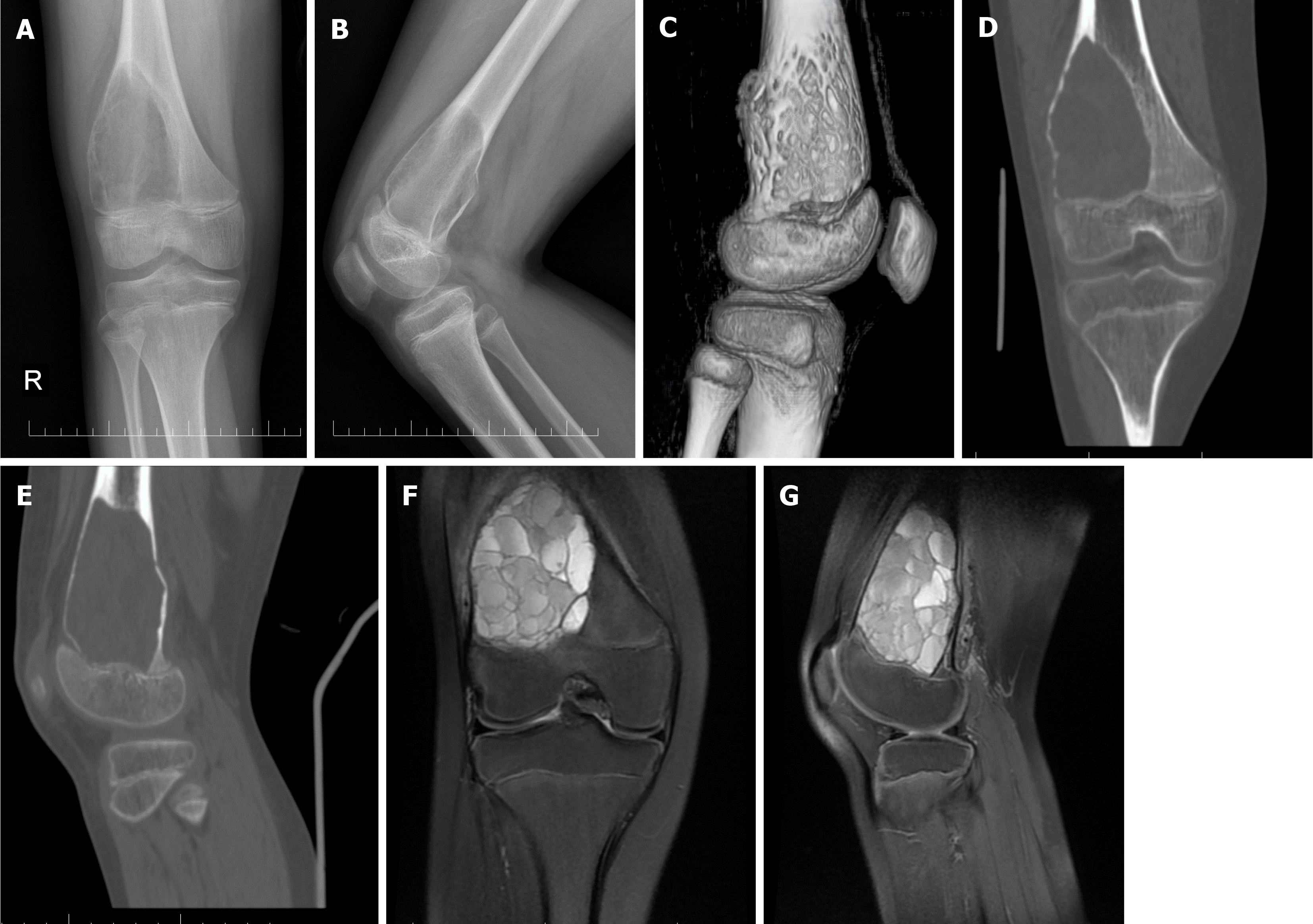
Auxiliary examinations, including X-rays from the external hospital, indicated bone changes at the distal right femur on the outer side, Laboratory tests revealed no significant abnormalities. Preoperative comprehensive imaging, including knee computerized tomography (CT), enhanced CT, and magnetic resonance imaging, revealed a translucent area on the outer side of the lower end of the femoral shaft, measuring approximately 77 mm × 46 mm × 49 mm, with precise edges, no sclerosis, and expansive growth. The bone cortex in the affected area was significantly thinned, with visible sieve-like pore shadows, and the growth plate was intact (Figure 1).
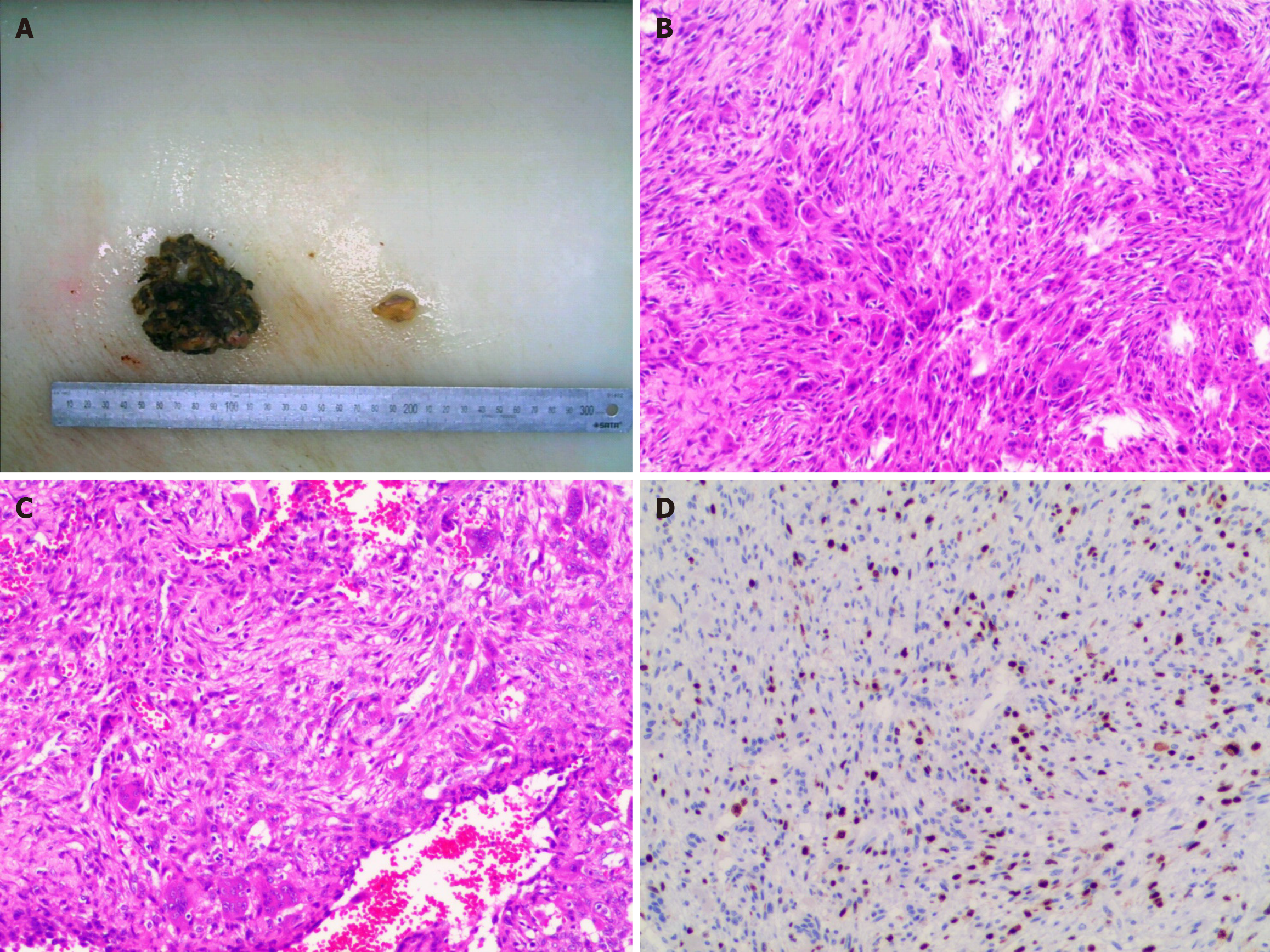
Pathological diagnosis: A large amount of cystic wall-like tissue is visible in the submitted specimen. Some cyst walls are filled with blood, and some show spindle-shaped fibroblastic proliferation accompanied by a large number of multinucleated giant cells, osseous matrix, and reactive woven bone components. Nuclear division is observed, and occasionally atypical cells are seen in the fibrous tissue (Figure 2). After consultation by pathology experts at Shanghai Sixth Hospital, the final diagnosis is ABC.
The final diagnosis was ABC.
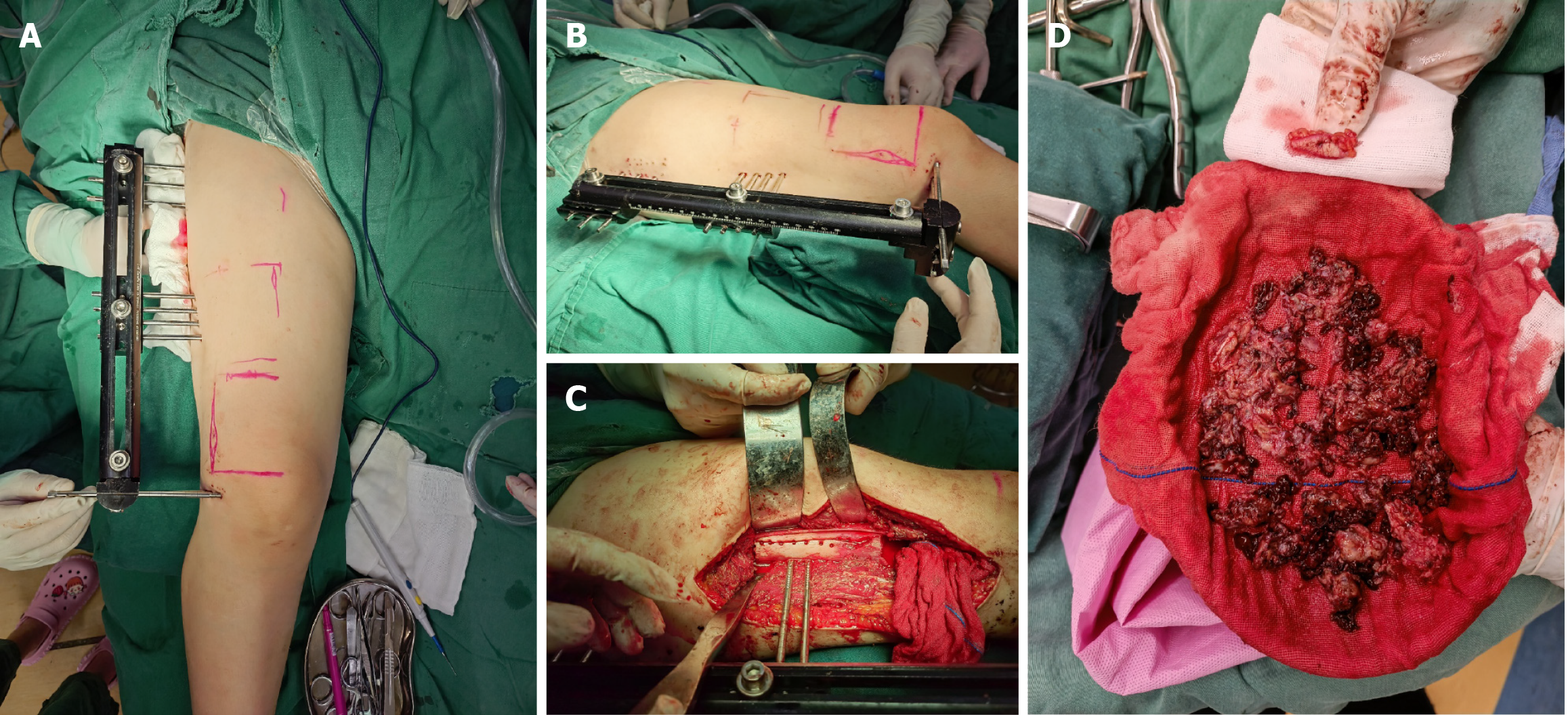
After admission, the patient underwent thorough examinations, and no surgical contraindications were found. On the sixth day of admission, under lumbar anesthesia, a "right femoral bone puncture biopsy" was performed. The posto
The patient had his stitches removed two weeks after the surgery and was discharged with instructions to wear a hip abduction orthosis for protection for two months. The family followed the doctor's advice to adjust the external fixation frame's length daily (approximately 1 mm of bone transportation per day) and attended check-ups every two weeks. The postoperative biopsy results indicated a non-ossifying fibroma combined with an arteriovenous malformation bone cyst.
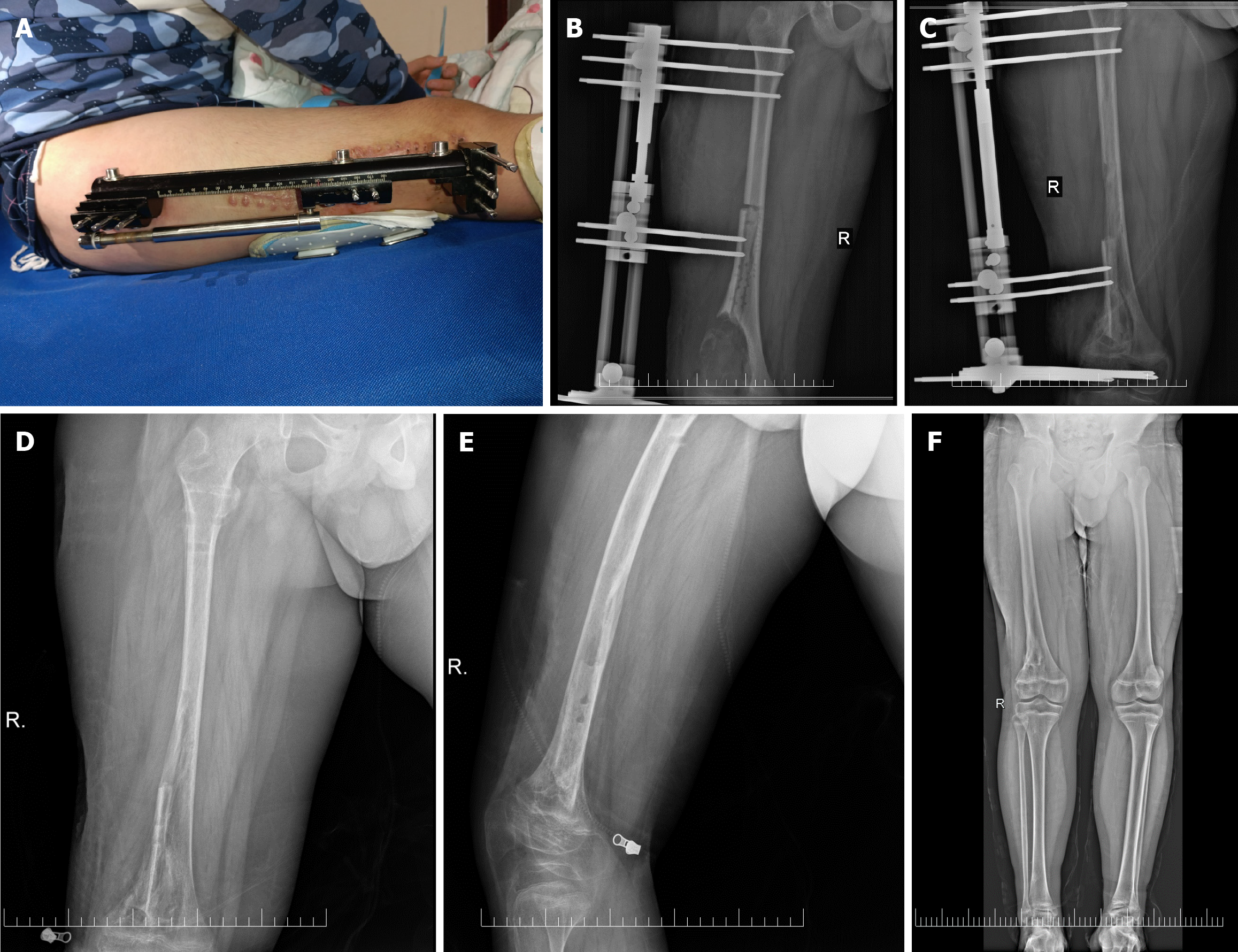
The X-ray also reveals that the patient's right lower limb is approximately 1cm longer than the left lower limb. The external appearance is entirely normal, and both the bone formation at the cut end and the union at the meeting point of the bones show excellent healing (Figure 4).
The Ilizarov technique, as a regenerative tissue technology, continues to play an indispensable role in treating bone defects[1]. ABC is a benign lytic bone lesion typically occurring at the metaphysis of long bones. Its biological characteristics include aggressive tumor growth, local solid invasiveness, and a high rate of postoperative recurrence[2]. According to the onset pattern, it is classified into secondary and primary forms. The lesion comprises numerous blood-filled channels and solid regions, often found in the pelvis, appendages of the spine, and metaphysis of long bones[3]. However, it can occasionally affect shorter bones, such as the hands and feet. Clinical presentations, including local skin warmth, pain, and swelling, are often nonspecific. Patients may occasionally seek medical attention due to pathological fractures[4]. ABC is a benign expansile and osteolytic bone tumor. After complete excision, bone grafting is the mine treatment for the primary ABC. When the tumor volume is large, inevitable bone defects occur after excision. The Ilizarov external fixation technique, based on the tension-stress principle, was initially developed in the former Soviet Union and has been widely adopted by physicians. It involves the gradual and steady pulling and fixation of the bone ends using an external fixator after surgically cutting the proximal or distal bone at the lesion site. This process stimulates bone tissue metabolism, activates the body's intrinsic repair mechanisms, promotes bone regeneration, and facilitates the gradual growth of surrounding nerves, tendons, connective tissues, and skin under the traction stimulus[5]. Since approximately 70% of ABC cases occur in children, protecting the growth plate becomes essential during surgery due to the unique nature of children's growth and development. In this case, our hospital employed the Ilizarov technique as an adjunctive treatment, yielding satisfactory results. The follow-up revealed ossification in the affected limb, and the child's growth and development remained largely unaffected. Both the patient and their family expressed a high satisfaction. This case report aims to contribute valuable insights for the future treatment of similar conditions.
Ilizarov technique, as a regenerative tissue technology, continues to play an irreplaceable role in the treatment of bone defects[5]. We present a unique case of ABC successfully treated with Ilizarov technique, which minimize harm to the patient. The two year's follow-up results were satisfactory. Doctors should be aware of the advantage of Ilizarov technique, and maximize its strength in similar cases.
Thank you to all the doctors who contributed to the patient's treatment.
| 1. | Aktuglu K, Erol K, Vahabi A. Ilizarov bone transport and treatment of critical-sized tibial bone defects: a narrative review. J Orthop Traumatol. 2019;20:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 132] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 2. | Flont P, Kolacinska-Flont M, Niedzielski K. A comparison of cyst wall curettage and en bloc excision in the treatment of aneurysmal bone cysts. World J Surg Oncol. 2013;11:109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Rapp TB, Ward JP, Alaia MJ. Aneurysmal bone cyst. J Am Acad Orthop Surg. 2012;20:233-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 113] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 4. | Grzegorzewski A, Pogonowicz E, Sibinski M, Marciniak M, Synder M. Treatment of benign lesions of humerus with resection and non-vascularised, autologous fibular graft. Int Orthop. 2010;34:1267-1272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Li J, Li M, Wang W, Li B, Liu L. Evolution and Development of Ilizarov Technique in the Treatment of Infected Long Bone Nonunion with or without Bone Defects. Orthop Surg. 2022;14:824-830. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |