INTRODUCTION
Foot drop constitutes a disabling condition of the lower limb. It is characterized by weakness or loss of ankle-dorsiflexion, ankle eversion, and toe extension. Typically, the sufferer displays a high steppage gait for clearing the ground during the swing phase of gait cycle. There is considerable functional deficit during walking. Resultantly, there is an awkward gait, greater than normal struggle and higher energy consumption, greater risk of injury to the forefoot, and falling during walking. The tendon transfer surgery aims to restore the lost dorsiflexion, and hence a balanced foot mobility and normalization of the gait cycle[1-3].
Foot drop represents a broad spectrum of possible etiologies. These include various injuries as well as neurological and chronic diseases that affect the brain, spinal cord and peripheral nerves. For instance, injury to the common peroneal nerve (CPN), injury to the sciatic nerve, tumors involving or compressing the CPN, lumbar disc prolapses, leg compartment syndrome or vascular injuries to the anterior leg compartment, tibiofibular fractures associated with leg compartment syndrome and dorsal ankle crush injuries involving the musculotendinous structures[4-9].
Not all patients with foot drop are candidates for the TP tendon transfer. Hence, identification of the underlying cause of the condition is of paramount importance. This helps to make prompt and appropriate treatment decisions. For instance, patients with foot drop secondary to a lumbar disc prolapse respond very well to the timely instituted neurosurgical intervention that entails decompression of the compressed nerve roots. Likewise, CPN compression caused by a tumor or space occupying lesion also responds very well to the timely removal of the tumor rather than performing tendon transfers[10-15].
In most instances, the foot drop results from traumatic events that involve the CPN or the sciatic nerve. The superficial and peculiar course of the CPN around the neck of the fibula makes it more vulnerable to injuries. Moreover, its regeneration potential is much poorer than that of the tibial division of the sciatic nerve. Although there have been considerable advances in the areas of nerve repair, nerve transfers and other microsurgical techniques; however, many of these patients continue to have persistent nerve deficits even after these interventions. Quite often, these patients have undergone initial procedures such as nerve repairs, nerve grafting and nerve transfers. These patients are the typical candidates for TP tendon transfer which provides more predictable results in the majority of cases[1,16-21]. The current study was carried out to document the clinical and epidemiological profile of foot drop patients and evaluate the outcome of TP tendon transfer for restoring the lost dorsiflexion of the foot.
MATERIALS AND METHODS
Study design and patient population
This prospective observational study was conducted at the National Institute of Rehabilitation Medicine in Islamabad over a period of 7 years (i.e. spanning from October 1, 2016 to September 30, 2023). Informed consent was taken from the patients. Convenience sampling technique was used. The study followed the ethical protocols of Helsinki’s Declaration-2013 revision. Anonymity of the participants was guaranteed.
The study included patients of all sexes and ages who presented with foot drop of at least 6 months duration and where there was no contraindication for TP tendon transfer. Exclusion criteria were patients who had contraindications for the procedure. For instance, patients who had paralyzed posterior leg compartment muscles, Achilles tendon contracture, stiff ankle or toes, unstable ankle joint, weak gastrocnemius or scarred skin spanning over the route of tendon transfer. Also, patients who had the foot drop as a result of disc prolapses or brain diseases were excluded.
Routine clinical evaluation with history, clinical examination and necessary investigations were employed for all patients. All of them had thorough musculoskeletal and neurological assessment of the affected limbs. Supple ankle joint, presence of plantar flexion and non-contracture of the Achilles tendon were confirmed on local examination. X-rays of the ankle and foot, electromyography, and nerve conduction studies of the lower limbs were performed. Preoperatively, the patients underwent physiotherapy and strengthening exercises for the isolated use of TP tendon for 6 weeks. Additionally, stretching exercises were instituted for the Achilles tendon in patients with reduced passive dorsiflexion.
Surgery and tendon transfer technique
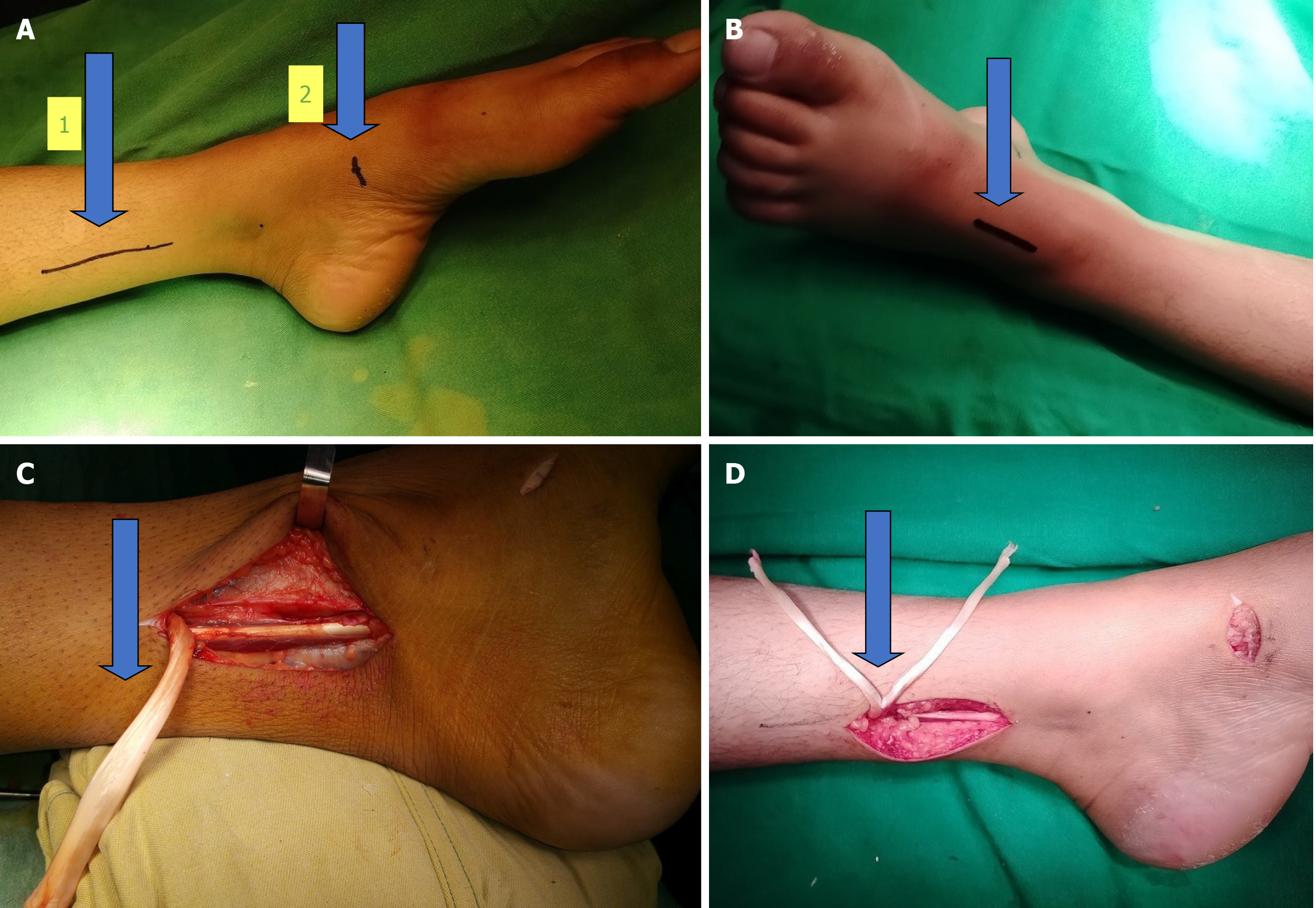
All the patients were admitted as in-patients for the operative procedure. The surgeries were undertaken under general or spinal anesthesia. Tourniquet control was employed among all cases. The circum-tibial route of TP tendon transfer was employed among all the patients. The procedure was performed by employing three standard incisions. The first incision (approximately 5-7 cm long) was made along the palpable posteromedial border of the distal tibia, ending about 2-3 cm proximal to the medial malleolus (Figure 1A). The second incision (approximately 2 cm long) was made over the area of the navicular tuberosity (Figure 1A). The TP was disinserted at this point and the tendon was retracted proximally through the aforementioned first incision. With careful finger dissection, the distal half of the muscle belly of TP was mobilized with preservation of the neurovascular structures. The third incision (approximately 4 cm long) was made over the dorsal aspect of the ankle to expose the tibialis anterior (TA), extensor hallucis longus (EHL), extensor digitorum longus (EDL), and peroneus tertius (PT) tendons (Figure 1B). Figure 1C shows the harvested TP tendon.
Figure 1 Photos of the tendon.
A: The arrow number 1 points towards the first incision which measures 5-7 cm. It is made along the palpable posteromedial border of the distal tibia. It ends about 2-3 cm proximal to the medial malleolus. The arrow number 2 indicates the second incision of 2 cm which is made over the navicular tuberosity (image date December 23, 2020); B: The third incision measures approximately 4 cm in length and is made over the dorsal aspect of the ankle to expose the tibialis anterior, extensor hallucis longus, extensor digitorum longus and peroneus tertius tendons (image date December 23, 2020); C: This clinical photograph shows the tibialis posterior tendon which has been disinserted from the navicular tuberosity and retracted proximally through the aforementioned first incision (image date December 23, 2020); D: This photograph shows the harvested tibialis posterior tendon which has been split into two slips (image date December 23, 2020).
The harvested TP tendon was split longitudinally into two slips. This technique helped to avoid the harvesting of flexor digitorum longus (FDL) (Figure 1D). These slips were delivered to the wound on the anterior aspect of the ankle through adequate subcutaneous transtibial tunnels. Adequate tunnels were created to ensure frictionless glide of the transferred tendon slips. One slip was Pulvertaft weaved to the tendons of TA and EHL whereas the other slip was weaved to the tendons of EDL and PT. Inclusion of the EHL, EDL, and PT helped to restore a balanced foot without producing an iatrogenic Varus deformity. The point of tenodesis was maintained proximal to the ankle joint. The points of fixation were altered in terms of medial to lateral locations on the distal leg, depending on the status of the muscular imbalance of the affected foot. Proline 2/0 sutures were employed to secure the tendons in the Pulvertaft weaves. Tension on the transfers was maintained with the ankle in 20-30° dorsiflexion. Setting the right amount of tension on the transfer was considered very crucial for achieving the desirable outcome. Generally, tension on the transferred tendons was set so that the tendons in the dorsum of the ankle and toes went into full extension with attempted foot plantar flexion. The TP tendon has only 2 cm excursion as compared to the 3-5 cm excursion of the TA tendon. Therefore, for restoring the desirable dorsiflexion, putting the right amount of tension on the tenodesis is imperative. It’s better to error on over-tension than under-tension[22].
The skin incisions were closed with Proline 4/0 interrupted sutures. Standard wound care was continued postoperatively and skin sutures were removed at 3 weeks. Postoperatively, the tendon transfers were protected with a below-knee plantar slab fashioned from plaster of Paris (POP). It was maintained for 6 weeks. During the next 6 weeks, an ankle foot orthosis was worn with neutral positioning of the ankle. Exercises with active dorsiflexion of the ankle were also instituted. During this phase the patients were advised to avoid plantar flexion. At the completion of 3 months postoperatively, full weight bearing was started. A follow-up of 1 year was ensured among all patients.
Clinical data collection and follow-up strategy
The social and demographic profile of the patients, various clinical entry parameters, and outcomes were all recorded. Active dorsiflexion, active plantar flexion and active range of motion (ROM) of the ankle were recorded preoperatively and at 12 months postoperatively as the outcome measures. The time-tested criteria devised by Carayon et al[23] were employed for this purpose. The outcomes were categorized as excellent, good, moderate and poor. The category was excellent when active dorsiflexion, active plantar flexion and active ROM were > 15°, > 30° and > 40° respectively. The category was marked as good when active dorsiflexion, active plantar flexion and ROM were 5°-15°, 15°-20° and 20°-30°, respectively. The results were considered moderate if there was no active dorsiflexion; however, the foot drop corrected and 10° plantar flexion was possible. The results were declared poor if there was presence of plantar flexion that prevented ankle mobility and allowed only minimal dorsiflexion.
Statistical analysis
The data were analyzed through the statistical package for social sciences (SPSS) version 21 (IBM Corp., Armonk, NY, United States). Descriptive statistics were used to calculate frequencies, percentages, means and standard deviation. The numerical data such as the patient’s age and duration of foot drop were expressed as mean ± standard deviation. The categorical data such as the causes of foot drop and the side affected were expressed as frequency and percentages.
DISCUSSION
Our study shows the high prevalence of foot drop cases in our population. The study serves as a surrogate measure of the high prevalence of CPN and sciatic nerve injuries among our patients. The issue is highly prevalent in our population; however, there is scarcity of published literature in this regard. Our institute receives disabled persons from all over the country for their rehabilitation. We also receive significant numbers of patients from the war-ravaged neighboring country of Afghanistan. Most of these patients with foot drop secondary to CPN or sciatic nerve palsies have already undergone some kind of preliminary surgical procedure such as nerve repair, nerve grafting or nerve transfers, but often to no avail.
In the present study, the established standard principles of tendon transfers were followed before embarking on the tibialis posterior (TP) tendon transfer. We ensured adequate passive mobility of the ankle joint; equilibrium and stability of the overlying skin and soft tissues; and functionality of the donor tendons preoperatively. Immobilization of the foot and ankle was ensured for 6 weeks immediately after surgery. Following this period of immobility, physiotherapy, re-education and rehabilitation were started to restore the lost ROM of the ankle and foot.
Our study predominantly included cases of foot drop secondary to the irreversible lesions of the CPN and iatrogenic sciatic nerve injuries. The CPN nerve is the smaller terminal branch of the sciatic nerve and receives fibers from the posterior divisions of L4, L5, S1, and S2. It courses along the upper lateral side of the popliteal fossa, deep to the biceps femoris and its tendon until it gets to the posterior part of the head of the fibula. It passes forward around the neck of the fibula within the substance of peroneus longus where it terminates by dividing into the superficial (L5, S1, S2) and deep peroneal (L4, L5, S1, S2) nerves. Foot drop may result from a number of neurological and muscular ailments. The CPN neuropathy may result from a host of causes. For instance, trauma and operative procedures on the pelvis, hip or knee; tumors and afflictions such as the leprosy and a variety of other neuromuscular illnesses affecting the lower limbs. Systemic conditions may sometimes also lead to foot drop, such as stroke, multiple sclerosis and spinal cord issues[1-3].
In our study, we performed TP tendon transfers at least 6x months after sustaining the nerve injury. The procedure was considered to be indicated when there was no clinical improvement and the nerve conduction studies/electromyography reinforced the same clinical finding. There is lack of consensus regarding the best timing for tendon transfer for foot drop. Most authorities have recommended waiting for at least 6 months before embarking on tendon transfers. During this time period the patient may show signs of nerve recovery and hence the major surgery can be avoided. Some authorities have included patients for tendon transfer who had the foot drop for at least 1 year[24]. On the other hand, other authors have performed earlier intervention in the form of tendon transfers[25-27]. Lingaiah et al[27] have advocated for early tendon transfer for addressing foot drop secondary to CPN and sciatic nerve palsies. They have observed that the early TP tendon transfer can serve one of the following three purposes: (1) They can serve as a helper; (2) The transfer can provide an internal splint; and (3) It can serve as a substitute for the lost dorsiflexion. All these three functions help in the early recovery and rehabilitation of the disabled patients.
In the published literature, all the authors have employed the TP tendon as the main motor to restore the lost functions of foot dorsiflexion and eversion. The TP tendon transfer is reported to be the best option when there is paralysis of the extensors as well as the evertors. In this way the unopposed inversion effect is also neutralized[27]. Over the years, several authorities have made innovative modifications in the standard TP tendon transfer. All these modifications have been made to achieve the best possible results or outcomes of the tendon transfers. These desired outcomes include better mobility, self-dependency and enhanced satisfaction of the patient. The relentless quest for finding the best procedure still continues[28]. Carayon et al[23] employed a dual tendon transfer. They sutured the TP tendon to the TA tendon; and the FDL to the EHL and EDL tendons. Vigasio et al[29] devised a new technique of rerouting the TP tendon through the third cuneiform bone. Additionally, they also employed FDL to power the affected EHL and EDL tendons. Leclère et al[30] reported the use of lateral gastrocnemius for addressing foot drop. Pinzur et al[31] employed transfer of TA to TP tendon to a neutral dorsiflexion point on the foot dorsum. Srinivasan et al[32] started the practice of splitting the TP tendon into two slips. The medial slip of the split tendon was used to power the EHL whereas the lateral slip was weaved to the EDL and PT tendons. The Bridle procedure was devised to weave the three tendons of TP, TA and peroneus longus[33,34]. Lipscomb and Sanchez[35] combined the tendon transfers with a triple arthrodesis.
In our study, we employed the TP tendon transfer through the circum-tibial route. The published studies have reported the successful use of tendon transfers through both the circum-tibial as well as interosseous routes. Both procedures have their own attended pros and cons. The circum-tibial route of transfer is technically easier and less time consuming. It is also found to be associated with a slightly increased degree of ankle dorsiflexion owing to its greater lever arm. On the downside, it may produce slight inversion deformity if attention to detail is not given. The interosseous route of tendon transfer produces a straight line of pull; however, it is more time consuming; has weaker action due to short lever arm; and is associated with an increased risk of vascular injuries as well as subsequent tendon adhesion formation along the route of tendon transfer[28,36,37]. A systematic review performed by Stevoska et al[28] revealed that 33% surgeons preferred the transtibial route whereas the remaining surgeons employed the interosseous route of TP tendon transfer.
In our study, we used the technique of tenodesis without anchoring the tendons to any bones. Recently a tendon to bone fixation has gained popularity, especially in the developed countries. The liberal availability of sophisticated implants allows easy and finer attachment of the tendons to the bones. These implants are usually in the form of bone suture anchors or specialized screws[27,38-41]. The majority of our poor patients have affordability issues and hence have no access to such sophisticated fixation equipment at present.
In our study, the point of tenodesis of the transferred tendons was kept proximal to the ankle joint. Maintaining this point proximal to the joint is technically straightforward and yields results which are comparable to other procedures[42]. The points of tenodesis were altered in terms of medial to lateral locations depending on the status of the muscular imbalance in a given foot. Cases where there was more remarkable weakness of the eversion, the points of fixation or tenodesis was kept more towards the lateral side of the foot, closer to the PT tendon. This modification allowed for achieving better foot stability as well as effecting the desired lateral lift of the affected foot[42-44].
In our study, we didn’t institute any adjunct preoperative or peri-operative procedures in our patients. Some authorities have reported undertaking Z-lengthening of the shortened Achilles tendon either in the preoperative phase or at the time of tendon transfer. This has been reported to help in achieving better active dorsiflexion of the ankle. Some authorities have been undertaking tendon transfer simultaneously with exploration and repair of the CPN. They have reported beneficial effects as internal splint as well as improved regeneration of the nerve. Others have reported the use of triple arthrodesis in cases where TP tendon has also been paralyzed or previous attempts at tendon transfers have failed. Similarly Bridle procedure has been reported in cases of sciatic nerve affliction, higher lesions of the spinal cord or when the tibial innervated muscles are also paralyzed. The procedure entails a dual anastomosis of the TP tendon to the TA tendon and a rerouted PT tendon anterior to the lateral malleolus[45-47].
In our study, it was observed that involvement was predominantly of male patients. Males are more frequently engaged in outdoor activities in our population. They are hence more vulnerable to road traffic accidents and other traumatic events in their daily lives. Such injuries may involve the CPN and the sciatic nerve. Several published papers conform to our observation of more frequent involvement of the males in foot drop injuries. Agarwal et al[24] in their series of 20 patients had 16 males and four females. Ozkan et al[47] in their series of 41 patients had 24 males and 17 females.
In this study, the bulk of the study subjects were constituted by the younger population with a mean age of 22 years. Several published studies have reported a similar young age group affliction with foot drop. Ozkan et al[47] reported a mean age of 32 years whereas Agarwal et al[24] reported it to be 31.4 years. In this series, more frequent involvement of the right side was observed. Agarwal et al[24] reported 13 right sided palsies and seven left sided palsies. However, Ozkan et al[47] reported more frequent involvement of the left side. There were 22 cases with left sided palsies whereas 19 with right sided palsy.
In our series, most of the cases of foot drop were secondary to trauma to the CPN or the sciatic nerve. Our finding conforms to most of the published literature wherein the CPN palsy has been reported to be the most frequently encountered post-traumatic mononeuropathy in the lower limb[1,3,33]. However, certain studies from India and Turkey have reported leprosy to be a common cause of CPN affliction and the cause of foot drop in their populations[27,28]. Stevoska et al[28] in their elegant systematic review found that TP tendon transfers were performed among the majority of cases (89%) for CPN palsies. These palsies had resulted from either traumatic injuries or infective neuropathy caused by leprosy.
In our study, we observed several cases of foot drop resulting from iatrogenic mechanisms such as orthopedic interventions and application of tight POP by non-doctors. Iatrogenic nerve injuries may be caused by a number of mechanisms. For instance, retraction or complete transection of the nerve during operative procedures; malposition and compression of the limb during surgery; the application of tight plaster to the lower limb; and tight application of compression stockings after surgery. One consistent issue with the iatrogenic cases of foot drop is their delayed presentation to the reconstructive surgeon. Owing to delayed presentation, most of them need secondary reconstructive procedures in the form of tendon transfer[11,48-51].
In our study, better outcomes were observed for patients with CPN palsy as compared to those with palsy secondary to the sciatic nerve or higher-level lesions. Our finding conforms to Yeap et al[52] who also shared similar observations. This observation should help the surgeon in proper preoperative counseling of patients regarding the likely prognosis of the tendon transfer surgery among foot drop patients with CPN palsy vs those with higher level nerve lesions. In the current study, most of the patients had good restoration of the lost dorsiflexion of the foot. With TP tendon transfer, most of the published literature has reported restoration of 15°-30° of active dorsiflexion[25,27,28,38].
In our study, wound infections were observed among three patients and hypertrophic scars among two patients. The published studies have reported a variety of complications among their patients. These complications mostly reflect the transfer techniques employed and the types of patients included in the study. Complications may emerge from factors such as the tendon being too short for attachment on the dorsum of the foot; and possible damage to bony, joint, and soft-tissue structures on the dorsum of the foot. Wagenaar and Louwerens[42] in their series reported the following two complications. One patient developed clawing of the 2nd to 5th toes. He had spasticity secondary to stroke. The other patient had recurrence of the equinovarus deformity.
In our study, we didn’t come across any case of foot drop secondary to leprosy. Many published studies, particularly from India and Turkey have reported leprosy patients to constitute the bulk of their studies[53-56]. Foot drop causes a considerable disability. It is associated with psychological repercussions and social issues. The patient faces problems with activities of daily living. He may lose working days and occupation. The disability as well as its treatment carries significant financial burden for the sufferer.
Strengths and limitations of the study
The current research has certain strengths as well as presents certain limitations. The strengths firstly included the fact that the study was the first of its kind to document the clinical and epidemiological presentation of foot drop cases in our population. Secondly, it objectively evaluated the outcome of TP tendon transfer through the circum-tibial route which we routinely perform among our patients with foot drop. The study has certain limitations as follows: the main limitation is that it was an observational study. It did not include any comparative groups for drawing more robust statistical comparisons and conclusions. Secondly, patients who had the foot drop as a result of disc prolapse diseases and brain disorders were not included. These latter patients received their management from neurosurgeons. The results of the study may be interpreted keeping in mind the aforementioned limitations. Future well-designed multicenter studies are recommended to overcome this limitation.