Published online Oct 18, 2024. doi: 10.5312/wjo.v15.i10.973
Revised: September 1, 2024
Accepted: September 19, 2024
Published online: October 18, 2024
Processing time: 168 Days and 17.7 Hours
This article presents a rare case of a complex hip fracture involving the ipsilateral femoral neck, trochanter, and femoral head, that was accompanied by hip dislocation. Currently, there is no established standard treatment method for this specific type of fracture. Therefore, it is crucial to comprehensively consider factors such as patient age, fracture type, and degree of displacement to achieve a successful outcome.
A 38-year-old man sustained a comminuted fracture of his right hip as a result of a car accident. The injuries included a fracture of the femoral head, a fracture of the femoral neck, an intertrochanteric fracture of the femur, and a posterior dislocation of the hip on the same side. We opted for a treatment approach combining the use of a proximal femoral locking plate, cannulated screws, and Kirschner wires. Following the surgery, we developed an individualized rehabilitation program to restore patient limb function.
For this complex fracture, we selected appropriate internal fixation and for
Core Tip: We introduce a very rare hip fracture combined with a femoral head fracture, a femoral neck fracture, and a femoral intertrochanteric fracture. Locking plates combined with cannulated screws and Kirschner wires were used to treat the complex hip fractures and achieved good results. Complex hip fractures require appropriate internal fixation methods to be selected on the basis of specific classifications. After surgery, an individualized rehabilitation plan needs to be developed on the basis of the degree of internal fixation.
- Citation: Yu X, Li YZ, Lu HJ, Liu BL. Treatment of a femoral neck fracture combined with ipsilateral femoral head and intertrochanteric fractures: A case report. World J Orthop 2024; 15(10): 973-980
- URL: https://www.wjgnet.com/2218-5836/full/v15/i10/973.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i10.973
This article presents a rare case of a complex hip fracture. The patient experienced ipsilateral fractures of the femoral head, femoral neck, and intertrochanteric region, accompanied by posterior hip dislocation. The challenges in treating this type of fracture include restoring the normal anatomical structure, ensuring stable internal fixation, preventing and managing femoral head necrosis, and ultimately rehabilitating the patient to regain limb function.
A 38-year-old man was admitted to the hospital due to pain in the chest, back, and right hip, as well as mobility impairment, which had been occurring for 2 hours resulting from a car accident.
The patient collided with a truck from behind while driving, causing his chest to hit the steering wheel and resulting in pain in the chest, back, and right hip. The patient was then taken to our hospital by ambulance.
There was no history of fracture or surgery.
The patient declared no family history of genetic diseases.
The patient presented with swelling, bruising, and deformities in the chest, back, and right hip. Tenderness was observed in the chest, back, and right hip joints, and the thoracic compression sign was positive. Muscle strength and tone, as well as sensation, in both upper limbs were normal. The patient experienced tapping pain in the lower part of the right leg, restricted movement in the right hip joint, and increased reflexes in the left and right knees. The bilateral dorsalis extension muscle strength in the foot was Grade IV, and the sensation of the feet was normal. The patient had palpable bilateral dorsalis artery pulsation and normal terminal circulation in the feet. The patient was alert and showed no apparent abnormalities in the head or abdomen.
The patient's vital signs were as follows: temperature, 37.0 °C; pulse rate, 92 beats/min; respiration rate, 30 breaths/min; and blood pressure, 122/72 mmHg. A blood test revealed that the white blood cell count was 9.1 × 109/L, the neutrophil count was 72%, the haemoglobin level was 102 g/L, and the C-reactive protein level was 12 mg/L. The rest of the laboratory tests were unremarkable.
A computed tomography (CT) scan revealed compression fractures of the 8th thoracic vertebra, a fracture in the right femoral neck combined with ipsilateral femoral head fracture, an intertrochanteric fracture, and posterior dislocation of the right hip.
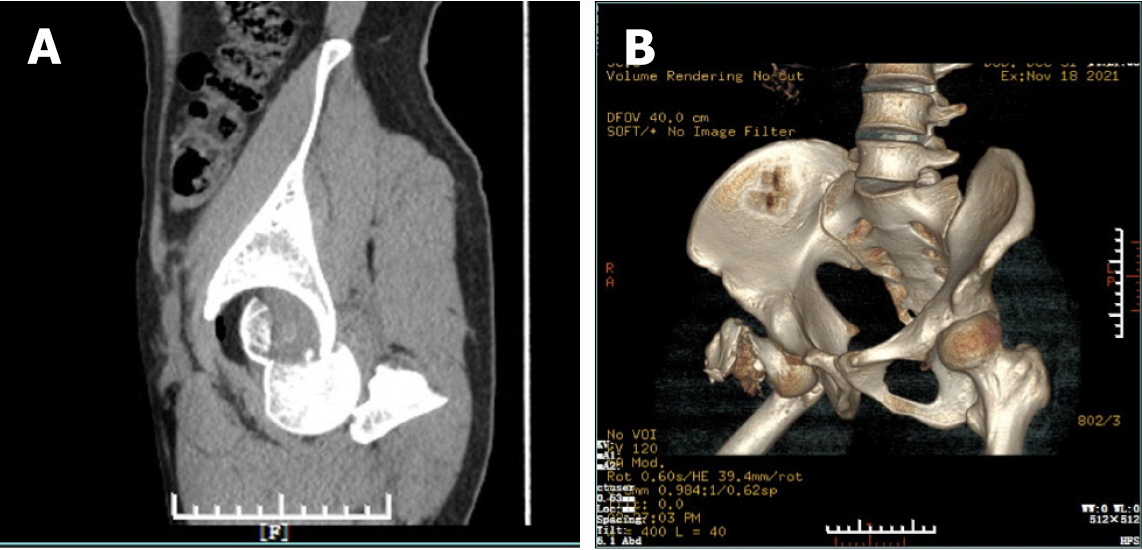
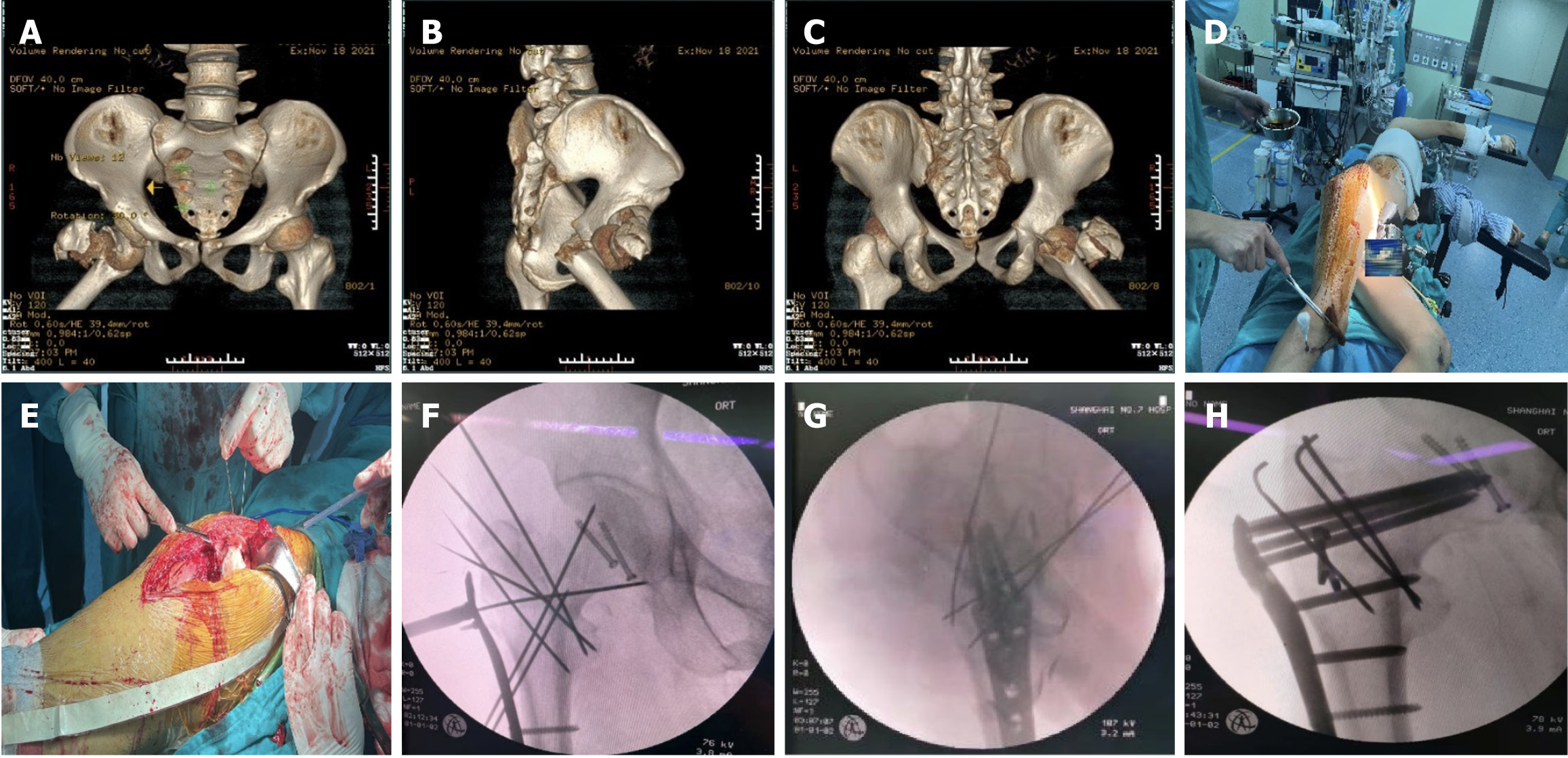
(1) Compression fracture of the 8th thoracic vertebra; (2) Right femoral head fracture (Pipink III, Figure 1A); (3) Right femoral neck fracture (AO/OTA B2.3, Figure 1B); (4) Right intertrochanteric fracture (AO/OTA A1.1, Figure 2A-C); (5) Posterior dislocation of the right hip; and (6) Bilateral traumatic pneumothorax.
Upon admission, the patient underwent right tibial tubercle traction and received various symptomatic treatments. After completing the preoperative preparations, the patient underwent open reduction of the right femoral neck combined with the femoral head and intertrochanteric fractures via a locking plate, cannulated nails, and Kirschner wires.
Following general anaesthesia, the patient was placed in the left lateral decubitus position (Figure 2D). A 20 cm incision was made at the apex of the greater trochanter, which was aligned with the long axis of the femoral shaft (Figure 2E). The incision involved the skin, subcutaneous tissue, and tensor fascia lata, exposing and incising the joint capsule. The femoral head was fractured into two fragments, with one fragment remaining in the acetabulum and the other fragment dislocated posteriorly. The soft tissue surrounding the joint and the damaged joint capsule were removed. The two parts of the femoral head were then reset and fixed in place with two 6.5 mm cannulated screws (Synthes Co., Ltd.). The firmly positioned femoral head was then returned to the acetabulum. The femoral neck fracture was observed to be an oblique fracture through the neck. After achieving good reduction, two 2.0 Kirschner wires were temporarily placed along the long axis of the femoral neck for fixation (Figure 2F). Additionally, the greater trochanter of the femur had a comminuted fracture. After achieving satisfactory reduction, three 2.0 Kirschner wires (Chuangshen Medical Co., Ltd.) were inserted from the greater trochanter to the lesser trochanter for fixation. Nonabsorbable sutures were used to cerclage the broken bone. A 9-well locking bone plate (Synthes Co., Ltd.) was inserted into the lateral side of the proximal femur, with several screws inserted into the distal and proximal ends for fixation. Four of the proximal screws penetrated deep into the femoral head through the femoral neck. To fix the bone fragments, two anatomical memory fixators (Lanzhou Ximai Co., Ltd.) were placed on the anterior and posterior sides of the trochanter. Intraoperative fluoroscopy confirmed satisfactory fracture reduction and internal fixation position (Figure 2G and H). The wound was thoroughly flushed with saline, a negative pressure drain was inserted, and the incision was sutured layer by layer.
The treatment timeline is shown in Table 1.
| Time | Clinical finding | Treatment |
| Two hours before hospital admission | Pain in the chest, back, and right hip, as well as mobility impairment resulting from a car accident | Ambulance to hospital |
| The day of admission | A compression fracture of the 8th thoracic vertebra, a right femoral head fracture (pipkin III, Figure 1A), a right femoral neck fracture (AO/OTA B2.3, Figure 1B), a right intertrochanteric fracture (AO/OTA A1.1, Figure 2A-C), and a posterior dislocation of the right hip | The patient underwent right tibial tubercle traction and received various symptomatic treatments |
| The 7th day of admission | Ipsilateral fractures of the femoral head, femoral neck, and intertrochanteric region | Operation |
| 3 days after the operation | The wound was slightly deep and the right lower limb was swollen | Start isometric training of the quadriceps while in bed |
| 1 week after the operation | The pain in the wound had begun to ease and the swelling in the lower limbs had been reduced | Knee joint flexion and extension exercises were initiated |
| 1 month after the operation | X-rays and CT scans indicated that the fracture was not displaced and that the internal fixation remained secure | Walk with crutches |
| 1 year after the operation | X-rays and CT scans demonstrated that the fractures had healed and no signs of avascular necrosis of the femoral head or osteoarthritis | The patient could already walk normally |
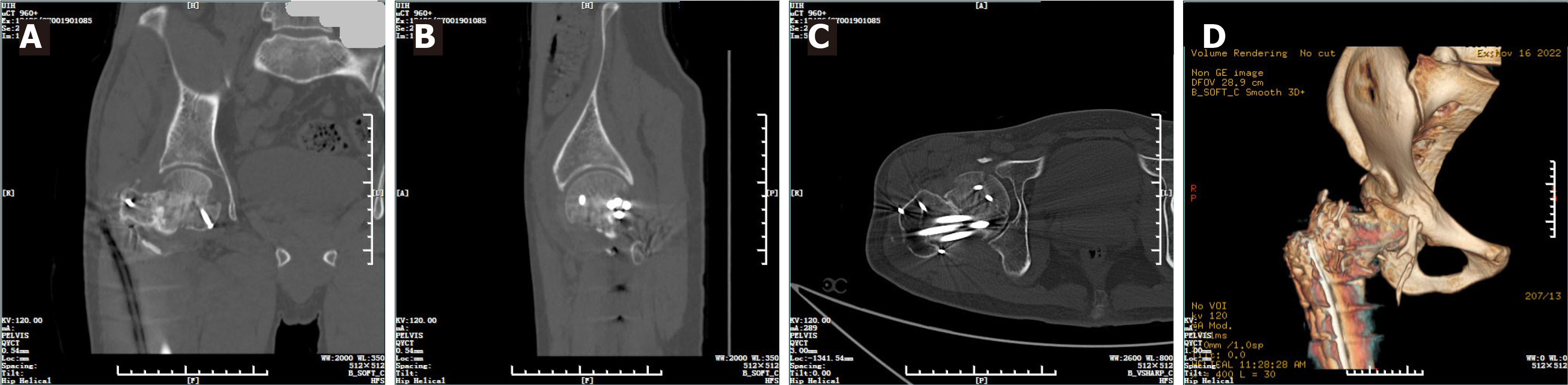
Postoperatively, cefuroxime was administered to prevent infection at the incision, and ankle pump training was implemented and low-molecular-weight heparin was administered to prevent deep vein thrombosis. On the 3rd day after the operation, the patient was instructed to start isometric training of the quadriceps while in bed, and 1 week after the operation, knee joint flexion and extension exercises were initiated. An X-ray was taken and reviewed 1 week after the operation, and it confirmed satisfactory fracture reduction (Figure 3A and B); the sutures on the wound were removed 2 weeks later. The patient returned to our hospital for follow-up examinations at one month (Figure 3C and D) and one year postoperation (Figure 3E and F). X-rays and CT scans of the hip joint revealed healed fractures, with no evidence of loosening or breakage of the internal fixation, and no signs of avascular necrosis of the femoral head or osteoarthritis (Figure 4). The Harris score of the hip joint at the last follow-up was 85 (Figure 5).
Femoral neck fractures and intertrochanteric fractures are both common types of hip fractures. The former accounts for approximately 3%-4% of all body fractures and approximately 40% of hip fractures[1]. The latter accounts for approximately 3.5% of all body fractures and 35%-40% of hip fractures[2]. The incidence of femoral head fractures is relatively low, with approximately 2 cases per million per year[3]. However, the incidence of femoral head fractures in patients with hip dislocation is relatively high, at approximately 11.7%[4]. The probability of two out of these three types of fractures occurring simultaneously is very low. According to the literature, the incidence of ipsilateral femoral neck fractures combined with intertrochanteric fractures out of all hip fractures is approximately 1.3%[5]. It is even rarer for all three types of fractures to occur simultaneously.
Chang et al[6] conducted an analysis on and assessed simultaneous occurrence of femoral neck and intertrochanteric fractures on the same side. They categorized these fractures into three types on the basis of the location of the femoral neck fracture and the fracture centre. Type II fractures extend outwards and superiorly from the femur neck to the trochanters and are known as transcervical fractures with one fracture centre. Chang et al[6] argued that type II fractures are essentially femoral neck fractures, where the fracture centre is at the femoral neck but the fracture line extends distally and involves the extracapsular outer and upper trochanter areas. In our case, the fracture type was similar, but the energy exerted by the injury was greater; this resulted in the continuation of violence along the femoral neck, resulting in posterior dislocation of the hip joint and fracture of the femoral head. Currently, there is no existing classification for this type of compound fracture. Therefore, in our case, we classified the fractures at three separate locations: femoral head fracture (Pipkin III type, Figure 1A), femoral neck fracture (AO/OTA B2.3, Figure 1B), and femoral intertrochanteric fracture (AO/OTA A1.1, Figure 2A-C).
Common implant options for hip fractures include dynamic hip screw (DHS), locking plates, proximal femoral nail antirotation (PFNA), and hip arthroplasty. In this particular case, the patient was a middle-aged male with strong bone tissue growth capacity and high exercise requirements. However, notably, the service life of artificial joint prostheses is limited. Therefore, the preference is to opt for femoral head-preserving treatment as much as possible without considering arthroplasty at the moment[7]. The patient's greater trochanter region suffered a comminuted fracture, making it difficult to maintain fracture stability through sliding compression via the DHS. Additionally, the patient's femoral neck fracture had a Pauwels angle greater than 70°, which results in a large shear force and an extremely unstable fracture[8]. Neither the goose-head nail of the DHS nor the spiral blade of PFNA can offer sufficient stability[9]. However, the patient's lesser trochanter and femoral calcar remained intact. Although the greater trochanter was crushed, the lateral wall of the trochanter was mostly undamaged, which allowed for the utilization of the lateral anatomic locking plate (LCP)[10]. The LCP functions as an internal fixation device and does not necessitate complete removal of the periosteum. The steel plate has limited contact with the bone surface, minimizing damage to the local blood supply. Moreover, threaded screw holes reduce the likelihood of screw withdrawal, even in cases where the screw holding force is insufficient for comminuted fractures[11]. Multiple long screws can be employed at the proximal end of the plate to traverse the femoral neck fracture line and extend beneath the femoral head. By adjusting the screw angle, the screws can be distributed evenly within the femoral neck, providing enhanced antirotation and support forces[12]. Cannulated screws are used to stabilize fractures of the femoral head[13]. Given the high degree of comminution in fractures of the greater trochanter, larger bone fragments are secured with memory alloy metal clips, whereas smaller bone fragments are fixed via multiple Kirschner wires and sutured with wire cerclage.
Rehabilitation is a fundamental aspect of fracture treatment, requiring clinicians to create personalized rehabilitation plans for patients on the basis of factors such as the extent of fracture comminution, stability of internal fixation, and soft tissue damage. In this particular case, the patient presented with three fractures, the ipsilateral femoral neck, femoral trochanter, and femoral head, with the greater trochanter exhibiting comminuted fracture. The method that was selected, internal fixation, involved a combination of a locking plate, cannulated screws, and Kirschner wires. While this approach restored the approximate anatomical shape of the proximal femur, it did not provide sufficient support, especially considering the patient's hip dislocation and significant soft tissue damage around the joint. Consequently, we assessed patient rehabilitation safety as low and developed a more conservative rehabilitation plan[14]. During the early postoperative period, our focus was on reducing swelling, providing pain relief, implementing antithrombotic treatment, and assisting patients with ankle pump training and lymphatic drainage. One week after surgery, we initiated knee and ankle flexion and extension activities. After four weeks of bed rest, a follow-up X-ray revealed proper alignment of the fracture with no evident loosening of the internal fixation. Only then did we allow the patient to engage in passive activities involving the hip joint. During the one-year follow-up, the patient regained normal walking ability without experiencing femoral head necrosis.
This case presents a highly comminuted hip fracture, which complicates the achievement of anatomical reduction during surgery. After the fracture ends were reduced, we utilized multiple Kirschner wires for temporary fixation; however, we could not avoid fracture ends that experienced partial displacement when long screws were inserted. Postoperative CT revealed a slight increase in the neck–shaft angle, and the long screw in the femoral neck was positioned posteriorly. Fortunately, the stability of the internal fixator remained intact, and the patient's hip function markedly improved.
This case presents a rare occurrence of ipsilateral femoral neck, femoral head, and intertrochanteric fractures. Considering the patient's age, general condition, and fracture classification, we opted for a treatment approach involving a proximal femoral locking plate in combination with cannulated screws and Kirschner wires. Postsurgery, we devised a personalized rehabilitation plan aimed at restoring the patient's hip joint function and walking ability. Ultimately, we achieved a satisfactory treatment outcome.
We wish to express our gratitude to the patient for his cooperation throughout the treatment and follow-up process. We also extend our thanks to Professor Qiu-gen Wang for his invaluable technical guidance during the surgery.
| 1. | Rashidifard CH, Romeo NM, Muccino P, Richardson M, DiPasquale TG. Palliative Management of Nonoperative Femoral Neck Fractures With Continuous Peripheral Pain Catheters: 20 Patient Case Series. Geriatr Orthop Surg Rehabil. 2017;8:34-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49:1458-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 561] [Article Influence: 80.1] [Reference Citation Analysis (0)] |
| 3. | Marecek GS, Scolaro JA, Routt MLC Jr. Femoral Head Fractures. JBJS Rev. 2015;3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Giannoudis PV, Kontakis G, Christoforakis Z, Akula M, Tosounidis T, Koutras C. Management, complications and clinical results of femoral head fractures. Injury. 2009;40:1245-1251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 127] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 5. | Videla-Cés M, Sales-Pérez JM, Girós-Torres J, Sánchez-Navés R, Videla S. A retrospective cohort study of concomitant ipsilateral extra-capsular and intra-capsular fractures of the proximal femur. Are they casual findings or an undervalued reality? Injury. 2017;48:1558-1564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Chang S, Wang Z, Tian K. [Patterns and research progress on the concomitant ipsilateral fractures of intracapsular femoral neck and extracapsular trochanter]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35:1079-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Mazur M, Steelman K, Sayeed Z, Chen C, Darwiche H, Little B. Total Hip Arthroplasty in the Ultrayoung. Arthroplast Today. 2023;23:101181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Ma J, Zhao Z, Zhi X, Wang H, Wang W. Finite element comparative analysis of three different internal fixation methods in the treatment of Pauwels type III femoral neck fractures. BMC Musculoskelet Disord. 2022;23:1030. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Inui T, Watanabe Y, Suzuki T, Matsui K, Kurata Y, Ishii K, Kurozumi T, Kawano H. Anterior Malreduction is Associated With Lag Screw Cutout After Internal Fixation of Intertrochanteric Fractures. Clin Orthop Relat Res. 2024;482:536-545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 10. | Gao Z, Lv Y, Zhou F, Ji H, Tian Y, Zhang Z, Guo Y. Risk factors for implant failure after fixation of proximal femoral fractures with fracture of the lateral femoral wall. Injury. 2018;49:315-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Basirom I, Daud R, Ijaz MF, Rojan MA, Basaruddin KS. Stability Analysis of Plate-Screw Fixation for Femoral Midshaft Fractures. Materials (Basel). 2023;16. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Wang T, Yin H, Zhao X, Ma C. Comparison of percutaneous compression plate to parallel screws in the treatment of nondisplaced femoral neck fractures in elderly patients: a prospective, randomized study. Arch Orthop Trauma Surg. 2023;143:7063-7071. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Wang S, Yu X, Li B, Ding Q, Wang T, Li Q, Liu L, Wu H. Pipkin type III femoral head fracture: which treatment strategy can be recommended? J Orthop Traumatol. 2023;24:28. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Runge M, Schacht E. [Proximal femoral fractures in the elderly: pathogenesis, sequelae, interventions]. Rehabilitation (Stuttg). 1999;38:160-169. [PubMed] |