Published online Oct 18, 2024. doi: 10.5312/wjo.v15.i10.965
Revised: September 12, 2024
Accepted: September 20, 2024
Published online: October 18, 2024
Processing time: 212 Days and 0.1 Hours
Severe skeletal class II malocclusion is the indication for combined orthodontic and orthognathic treatment.
A woman with a chief complaint of a protruding chin and an inability to close her lips requested orthodontic camouflage. The treatment plan consisted of extracting the right upper third molar, right lower third molar, left lower second molar, and left upper third molar and moving the maxillary dentition distally using a convenient method involving microimplant nail anchors, push springs, long arm traction hooks, and elastic traction chains. After 52 months of treatment, her overbite and overjet were normal, and her facial profile was favorable.
This method can be used for distal movement of the maxillary dentition and to correct severe skeletal class II malocclusion in adults.
Core Tip: Severe skeletal class II malocclusion in adults can be effectively corrected using a method involving distal movement of the maxillary dentition using microimplant nail anchors, push springs, long-arm traction hooks, and elastic traction chains. After 52 months of treatment with this approach, the patient’s overbite and overjet were normal, and her facial profile improved.
- Citation: Xie LL, Chu DY, Wu XF. Simple and effective method for treating severe adult skeletal class II malocclusion: A case report. World J Orthop 2024; 15(10): 965-972
- URL: https://www.wjgnet.com/2218-5836/full/v15/i10/965.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i10.965
Skeletal class II malocclusion is a common condition[1] and is characterized by maxillary prognathism, mandibular hypoplasia, or both[1,2]. Severe skeletal class II malocclusion is an indication for combined orthodontic and orthognathic treatment to improve the facial profile[2,3]. However, patients’ willingness is low because of high costs and the risk of surgical trauma. Thus, patients prefer to improve their facial profile using orthodontic camouflage. We report the case of a patient with severe skeletal class II malocclusion who underwent distal movement of the maxillary dentition using a simple clinical approach and exhibited significant improvement in their facial profile.
A woman in her early 30 s visited the Hebei General Hospital with the chief complaint of a protruding chin and an inability to close her lips.
The patient has had protruding teeth since adolescence; the protrusion has gradually worsen with age.
There are no systemic diseases or contraindications.
There was family history of maxillary protrusion.
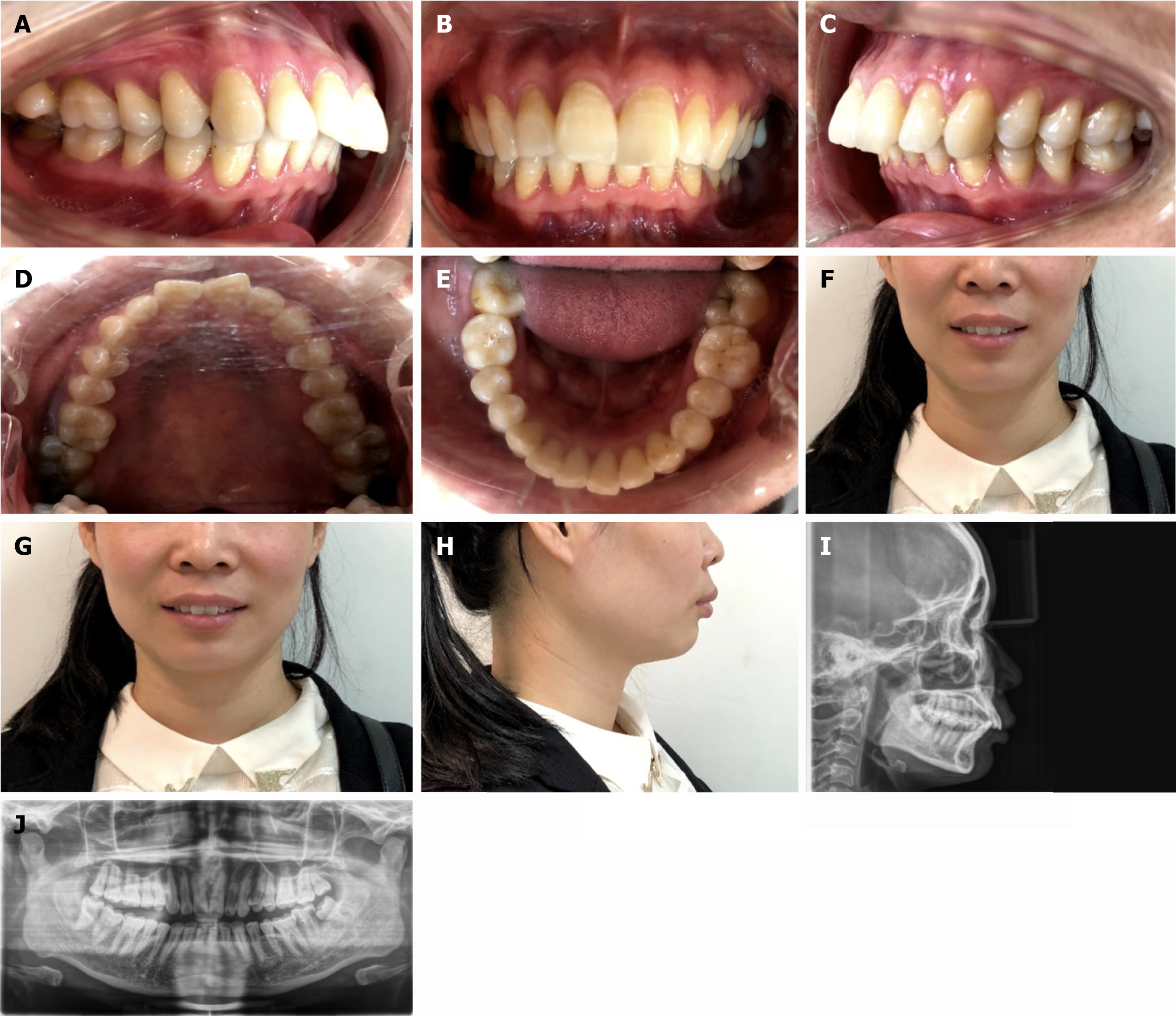
Clinical examination revealed that she had moderate lip incompetence, protrusion of the middle face, facial asymmetry with the chin deviating to the right, and plumpness of the right side. Examination of her joints revealed asymmetric bilateral mandibular condyles. Intraoral examination revealed mild alveolar bone resorption, a bilateral first permanent molar with a distal cusp-to-cusp relationship, third degree deep overbite, third degree deep overjet of the anterior teeth, mild crowding of the upper and lower anterior teeth, a normal upper midline, a lower midline deviating 1 mm to the right, a bilateral second molar buccal scissors bite, and chronic periapical periodontitis in the left lower second molar (tooth 37) with second degree tooth mobility.
No special notes.
Cone beam computed tomography (CBCT) revealed that the labial bone of the maxilla was thin and that there was periapical radiolucency of tooth 37. Panoramic radiographs revealed that the right upper third molar (tooth 18), left upper third molar (tooth 28), left lower third molar (tooth 38), and right lower third molar (tooth 48) had visible mesial impaction (Figure 1).
The patient was diagnosed with adult skeletal class II malocclusion and angle class II malocclusion.
The patient underwent 3 stages of orthodontic camouflage. In the preparation stage, teeth 37, 18, 28, and 48 were extracted. Two microimplant anchoring screws were placed on the buccal side between the bilateral maxillary first permanent molar and the second premolar at a 40° angle, and one microimplant nail was placed on the left lateral oblique line of the mandible. In the first stage of treatment, the buccal scissors bite of the second molar was corrected via interactive traction of the molars, which involved sticking the buccal tube to the maxillary second permanent molar, sticking the lingual button to the lingual side of the mandibular second permanent molar and interactive traction with 1/4 interarch elastics (3.5 OZ). Stable and normal occlusion of the posterior teeth with roots firmly embedded in the alveolar bone was necessary to ensure distal movement of the maxillary dentition.
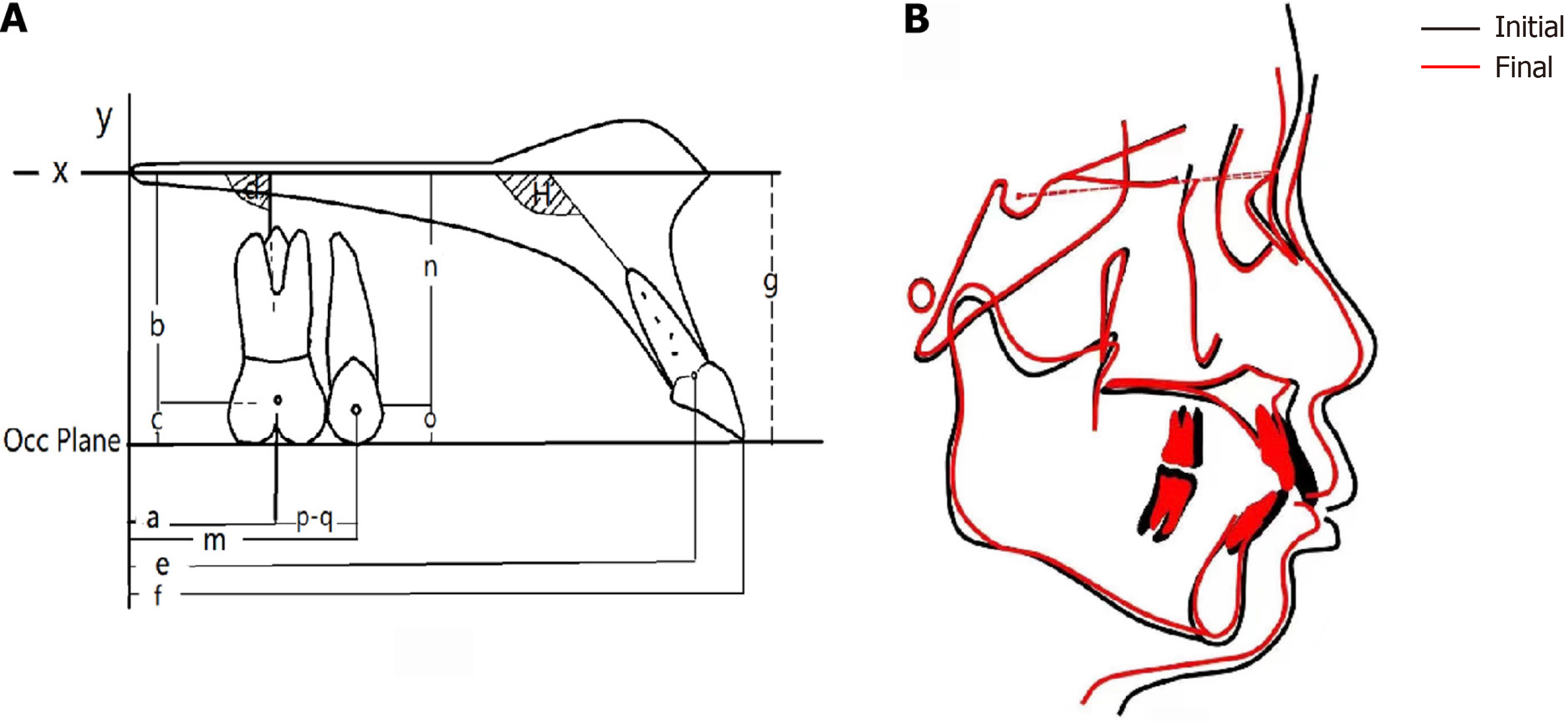
The second phase began 4 months after the buccal scissors bite of the second molar was corrected. Damon self-ligating brackets were used to align the dentition with the nickel titanium wire, and elastic bands were used for traction between the anchoring nail and the canines in the early stage to avoid labialinclination above the upper anterior teeth. After the teeth were aligned, stainless steel wire measuring 0.018 × 0025 inch was applied to each tooth, and distal movement of the dental arch was started (Figure 2). We used push springs, long-arm traction hooks, elastic traction chains, and anchoring nails to move the maxillary dentition distally. The entire process did not change the position of the nails, nor did the steel wires or traction hooks have to be replaced. We moved the maxillary dentition step by step, changing the position of the push spring in the dental arch twice—to the molar segment first, then the bicuspid segment. The push springs were placed between the first permanent molar and the second premolar on both sides to allow distal movement of the first and second molars, and the molar relationship was changed from a distal to a neutral relationship. Then, the position of the push springs was changed to allow distal movement of the first and second premolars and, finally, the anterior segment. The key to this stage is to keep the long-arm traction hook tightly attached to the mesial side of the lateral incisor bracket, maintain a traction force of 200 g between the self-traction hook and the microimplant nail with the elastic bands, and to replace the bands every month.
In the third phase of treatment, tooth 38 was moved mesially. To avoid reducing the deep overjet of the anterior teeth and occlusal trauma, microimplant nails were implanted in the left lateral oblique line of the mandible and the tongue was retracted to allow vertical forward movement of the lower teeth (35, 36, and 38) and intrusion of tooth 38.
The duration of treatment was 52 months. After orthodontic camouflage, relating the maxilla to the skull and relating the maxilla to the mandible were reduced by 2.5° and 3°, respectively, and the mandibular plane angle did not increase (Table 1, Figure 3). At the 6-month follow-up, the patient had stable occlusion, a normal overbite and overjet, and a favorable facial profile (Figure 4). The retainer was worn throughout the day.
| Cephalogram | Pretreatment | Posttreatment | Reference |
| SNA (°) | 86.5 | 84 | 82.8 ± 4.1 |
| SNB (°) | 77.5 | 78 | 80.1 ± 3.9 |
| ANB (°) | 9 | 6 | 2.7 ± 2 |
| NP-FH (°) | 85 | 86.5 | 85.4 ± 3.7 |
| NA-PA (°) | 18 | 13 | 6 ± 4.4 |
| U1-NA (mm) | 4 | 3 | 5.1 ± 2.4 |
| U1-NA (°) | 18.5 | 17 | 22.8 ± 5.7 |
| L1-NB (mm) | 11 | 9 | 6.7 ± 2.1 |
| L1-NB (°) | 47 | 43 | 30.3 ± 5.8 |
| U1-L1 (°) | 107 | 114 | 125.4 ± 7.9 |
| U1-SN (°) | 104 | 101 | 105.7 ± 6.3 |
| MP-SN (°) | 26 | 25.5 | 30.4 ± 5.6 |
| FH-MP (°) | 21 | 20 | 23.3 ± 6.1 |
| L1-MP (°) | 121 | 117 | 96.7 ± 6.4 |
| Yaix (°) | 61 | 59.5 | 66.3 ± 7.1 |
| Po-NB (mm) | 0 | 0 | 1.0 ± 1.5 |
| Wits (mm) | 3.5 | 1.5 | -0.81 ± 2.8 |
| APDI (°) | 79 | 74.5 | 83.18 ± 5.86 |
| ODI (°) | 85.5 | 80 | 76.8 ± 6.84 |
| Teeth movement1 | |||
| a (mm) | 4.5 | 10 | |
| b (mm) | 20 | 20 | |
| c (mm) | 3 | 2.5 | |
| d (°) | 66 | 69.5 | |
| e (mm) | 42.5 | 39 | |
| f (mm) | 46 | 42 | |
| g (mm) | 23.5 | 20 | |
| h (°) | 108 | 107.5 |
This study involved a 36-year-old woman who was unable to close her lips due to a protruding chin. For patients with skeletal class II malocclusion, orthodontic camouflage through distal movement of the maxillary dentition assisted by microimplant nails, push springs, long-arm traction hooks, elastic traction chains and self-ligating brackets might be feasible for improving the facial profile. Less force is used to move the entire dental arch distally, effectively controlling the overbite.
First, microimplant nails are easy to implant and do not loosen easily, and there is are lower risks of infection and soft tissue wrapping. In this case, microimplant nails were implanted between the maxillary first permanent molar and the second premolar, and there was no need for further surgery to change their positions, which was conducive to controlling the direction of movement. Second, the operation was simple and did not require archwire replacement; therefore, only the position of the push spring was changed, as the goal of treatment at each stage changed. Third, the key to this method is the transmission of force, and the long-arm traction hook should be tightly attached to the mesial side of the bracket attached to the canine teeth without leaving any space. During treatment, a long traction hook was placed on the archwire, the height of which was the same as that of the microimplant nails. The traction force of the elastic chain between the hook and nail was greater than that of the push spring. In this way, ideal root control adduction of the upper incisor teeth was achieved, as was effective control of the overbite. The traction force of the traction hook and the microimplant nail is then transmitted to the posterior teeth of the dental arch through the push spring.
For the treatment of skeletal class II malocclusion, mesial movement of the mandibular molars is difficult. To avoid reducing the deep overjet of the anterior teeth and occlusal trauma, microimplant nails were implanted in the left lateral oblique line of the mandible and the tongue was retracted to allow vertical movement of the lower teeth and intrusion of tooth 38. In this study, a reasonable mechanical system in which force transmission was convenient and feasible was established. Owing to the complex process of moving the mandibular third molars moving and then standing them upright in the mesial region, the overall treatment time was 52 months. Compared with the one-step method for distal movement of the maxillary dentition, the efficiency of stepwise distal movement is greater, and the elastic traction force required to achieve the same efficiency is lower. Therefore, the probability of the microimplant falling off is reduced, and the overall risk is decreased. For patients with prodromal and crowding profiles, the incisor is angled upright before treatment, and the risk of root resorption increases during distal movement of the maxillary dentition[4,5]. According to CBCT before treatment, the key to successful treatment is to estimate the space needed for adduction of the anterior teeth and whether there is sufficient bone mass for distal movement[6-8]. The capacity for alveolar bone remodeling in adults with skeletal class II malocclusion is limited. Therefore, after treatment, the upper incisor tooth was angled slightly upright to ensure that the root of the maxillary central incisors remained in the center of the alveolar bone, which also compensated for the skeletal malocclusion and prevented severe root resorption caused by the adjacent palatal cortex[6,9,10]. Notably, lip inclination and occlusion of the maxillary anterior teeth vary among patients, and the required direction of movement may also differ. Therefore, providing traction in different directions and locations may lead to different effects, which therefore need to be explored to reveal a better application of this method.
During the treatment process, because the position of the microimplant is relatively low and fixed, there is no need for a second surgery to change its position, so the patient does not experience any more discomfort or pain. After six months of follow-up observation after treatment, the occlusal relationship remained stable, and the protrusion of the anterior teeth was well maintained. Additional follow-ups will provide insight into the long-term effects of maintenance.
In conclusion, this simple method is suitable for distal movement of the maxillary dentition and the correction of severe skeletal class II malocclusion in adults, potentially improving the facial profile of patients.
We sincerely appreciate the team of doctors who completed this study, as well as Professor Chun-lei Xun, who helped design the treatment plan.
| 1. | Maetevorakul S, Viteporn S. Factors influencing soft tissue profile changes following orthodontic treatment in patients with Class II Division 1 malocclusion. Prog Orthod. 2016;17:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Guo Y, Han X, Xu H, Ai D, Zeng H, Bai D. Morphological characteristics influencing the orthodontic extraction strategies for Angle's class II division 1 malocclusions. Prog Orthod. 2014;15:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Baek ES, Hwang S, Choi YJ, Roh MR, Nguyen T, Kim KH, Chung CJ. Quantitative and perceived visual changes of the nasolabial fold following orthodontic retraction of lip protrusion. Angle Orthod. 2018;88:465-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Liou EJ, Chang PM. Apical root resorption in orthodontic patients with en-masse maxillary anterior retraction and intrusion with miniscrews. Am J Orthod Dentofacial Orthop. 2010;137:207-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Karnati PKR, Seth P, Zamzuri ATB, Tharwani P. Orthodontically Induced External Apical Root Resorption in Class II Malocclusion. Case Rep Dent. 2021;2021:8290429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Du YQ, Cui T, Yu YL, Hou FC, Song Y. [Clinical effect of upper molar distalization with micro-implant anchorage in premolar extraction for treatment of angle class II division 1 malocclusion in adults]. Qingdao Daxue Yixueyuan Xuebao. 2017;53. [DOI] [Full Text] |
| 7. | Oishi S, Ono T. A Case Treated with Maxillary Molar Distalization through the Maxillary Sinus: Three-Dimensional Assessment with a Cone-Beam Computed Tomography Superimposition. App Sci. 2022;12:9494. [DOI] [Full Text] |
| 8. | Wang Y, Shi Q, Wang F. Optimal Implantation Site of Orthodontic Micro-Screws in the Mandibular Anterior Region Based on CBCT. Front Physiol. 2021;12:630859. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Ma N, Li WR, Chen XH, Zheng X. [Root resorption analysis of the maxillary incisors during retraction stage]. Xiandai Kouqiang Yixue Zazhi. 2015;29:330-334. |
| 10. | Xu T. [Confusing anchorage]. Hua Xi Kou Qiang Yi Xue Za Zhi. 2012;30:225-228. [PubMed] |