Published online Aug 18, 2023. doi: 10.5312/wjo.v14.i8.604
Peer-review started: May 10, 2023
First decision: June 14, 2023
Revised: June 23, 2023
Accepted: July 10, 2023
Article in press: July 10, 2023
Published online: August 18, 2023
Processing time: 98 Days and 16.7 Hours
Fractures around the shoulder girdle in children are mainly caused by sports accidents. The clavicle and the proximal humerus are most commonly involved. Both the clavicle and the proximal humerus have a remarkable potential for remodeling, which is why most of these fractures in children can be treated conservatively. However, the key is to understand when a child benefits from surgical management. Clear indications for surgery of these fractures are lacking. This review focuses on the available evidence on the management of clavicle and proximal humerus fractures in children. The only strict indications for surgery for diaphyseal clavicle fractures in children are open fractures, tenting of the skin with necrosis, associated neurovascular injury, or a floating shoulder. There is no evidence to argue for surgery of displaced clavicle fractures to prevent malunion since most malunions are asymptomatic. In the rare case of a symptomatic malunion of the clavicle in children, corrective osteosynthesis is a viable treatment option. For proximal humerus fractures in children, treatment is dictated by the patient's age (and thus remodeling potential) and the amount of fracture displacement. Under ten years of age, even severely displaced fractures can be treated conservatively. From the age of 13 and onwards, surgery has better outcomes for severely displaced (Neer types III and IV) fractures. Between 10 and 13 years of age, the indications for surgical treatment are less clear, with varying cut-off values of angulation (30-60 degrees) or displacement (1/3 – 2/3 shaft width) in the current literature.
Core Tip: Fractures of the clavicle and proximal humerus in children can be treated conservatively in most patients because of their large remodeling potential. The difficulty is to understand when a child is better off with surgical treatment of his/her clavicle or proximal humerus fracture. This review aims to provide a better understanding of the indications for surgical management of these fractures in the skeletally immature based on the latest literature.
- Citation: Kraal T, Struijs PA, Langenberg LC, van Bergen CJA. Fractures around the shoulder in the skeletally immature: A scoping review. World J Orthop 2023; 14(8): 604-611
- URL: https://www.wjgnet.com/2218-5836/full/v14/i8/604.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i8.604
Fractures of the shoulder girdle in the skeletally immature are relatively rare, and most fractures can be treated conservatively. However, precisely this situation makes deciding which pediatric shoulder fracture needs surgical treatment difficult. Of the pediatric shoulder girdle injuries, fractures of the clavicle and proximal humerus are the most common. This review article updates treatment recommendations for these fractures in the skeletally immature.
The clavicle is the most commonly fractured shoulder girdle bone in children. It accounts for 10%-15% of all pediatric fractures, more common in boys compared to girls[1]. Most clavicle fractures occur during sports activities like bike accidents or horse riding. About 90% of clavicle fractures are diaphyseal, and most are Allman type 1 fractures, in the middle third of the shaft[2]. More than 50% of clavicle shaft fractures in children and adolescents are completely displaced with substantial shortening[3]. Clavicle fractures due to obstetrical injury are beyond the scope of this review.
The clavicle has a medial and lateral ossification center which usually fuse around the seventh week of gestation. A congenital pseudoarthrosis can develop if this fusion does not occur, leading to a painless protuberance[4]. Eighty percent of clavicular longitudinal growth occurs from the medial physis. The lateral physis closes around 18-19 years of age, and the medial physis is the last of the human body to close around 23 to 25 years of age. The clavicle is surrounded by a thick periosteum around both ends. Sternoclavicular (SC) injuries and, to a lesser extent, acromioclavicular (AC) injuries, are often trans-physeal fractures rather than true AC or SC joint dislocations[5,6].
There are few clear indications for surgical treatment of clavicle fractures in children; open fractures, irreducible fractures with significant tenting of the skin with impending skin necrosis, acute neurovascular injury, or concomitant fractures of the scapula (floating shoulder). In adults, substantial dislocation of a clavicular shaft fracture often indicates osteosynthesis to avoid non-union or symptomatic malunion. In children, however, these fractures can usually be treated non-operatively with a sling or figure-of-eight bandage. Your mentor might have told you the adage: “If the two ends of the child’s clavicle are in the same room, they will heal and remodel adequately”. There are several articles with typical radiographs showing consolidation and remodeling after displaced clavicle fractures[7,8]. Even an initial displacement of more than 2cm will most likely lead to union without clinically meaningful loss of shoulder motion or strength[9,10]. The degree of dislocation will most likely improve during the initial healing phase, and substantial remodeling can occur since clavicle growth continues up to 25 years of age[11,12]. However, there seems to be a tendency towards more surgical procedures for clavicle fractures in teenagers[13]. This is most likely the result of a similar trend toward surgical treatment of clavicle fractures in adults. In contrast to the situation in adults, however, little evidence supports this trend in the skeletally immature.
The potential advantages of surgical management are a quicker return to sports and avoiding non- and malunion. A recent review showed a quicker return to sports of 4-6 wk in the surgically treated group[14,15]. However, other studies do not show a significantly shorter return to sports[16]. The gain in weeks for return to sports is relatively minimal, but might be a consideration for young athletes who wish to return to high-level sports as soon as possible. Surgery is associated with higher healthcare costs and a higher complication rate. The most common complications are sensory loss at the chest region and implant prominence. Secondary surgery because of implant prominence is reported in 10%-20% of cases[8,17]. The pros and cons for young athletes should be used in shared decision-making if surgical treatment is considered, which is also highlighted in a current concepts review on this topic[18].
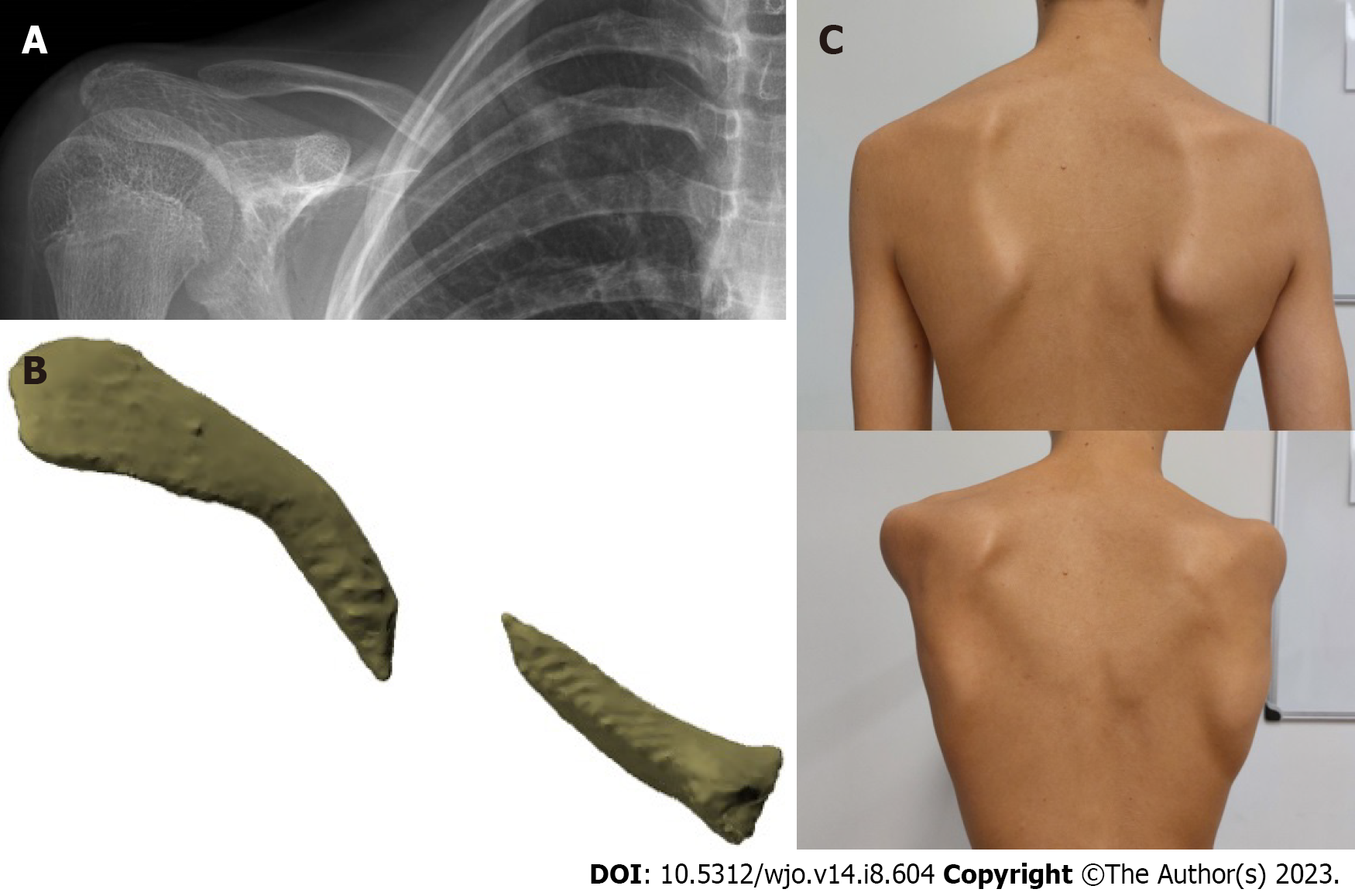
Whether surgery should be performed to prevent non- and symptomatic malunion in children is highly questionable. Clavicular non-unions in children do exist, but are exceedingly rare. Figure 1 shows a rare case of a 15 year old boy with scapular dyskinesia caused by shortening of his clavicle due to a nonunion. A large randomized trial comparing surgical treatment with conservative treatment for displaced clavicular fractures found a non-union rate of 0.4%[19]. With such low numbers of non-union, the incidence of non-union is difficult to establish, but is estimated to be less than 1%[20]. Although most non-unions occur in completely displaced fractures, they can even happen in minimally displaced fractures[20]. The primary risk factor for non-union is a re-fracture[20,21]. Non-unions are usually treated successfully with plate fixation. Bone grafting from the locally available non-union fracture site is usually enough, and iliac crest bone graft is not necessary in most cases[20,22].
Historically, symptomatic malunion has been a concern, potentially leading to decreased function or strength of the affected shoulder. This hypothesis was mainly based on anatomical and biomechanical studies[23]. In clinical reports, it is assumed that malunion can cause a wide variety of symptoms, such as functional limitations of the arm with or without pain, weakness of the arm, scapular dyskinesia, thoracic outlet syndrome or compression on the brachial plexus, and cosmetic dissatisfaction[24].
There is good quality evidence on this topic available at the moment, with a recent large multicenter cohort study comparing operative vs non-operative treatment for displaced clavicle fractures in adolescents[19]. Multiple upper limb functional outcome scores showed no significant differences between both groups. Only two out of 291 patients in this cohort developed a symptomatic malunion after non-operative treatment. For the rare patient who develops a symptomatic malunion, delayed (corrective) osteosynthesis is a good option. Adequate pre-operative 3D planning and patient-specific cutting guides can aid in correcting the three-dimensional deformity of the clavicle. However, no reports could be found explicitly aimed at children concerning malunion corrections[25].
The re-fracture risk of the clavicle in pediatric patients is around 2% to 6%. Interestingly, the re-fracture risk is higher after angulation only for completely displaced fractures[7]. It is hypothesized that this can be caused by more callus formation in completely displaced fractures compared to angulation-only fractures. Re-fractures occur in both surgically and non-operatively treated patients, perhaps even more frequently in surgically treated patients[14,19]. Just like initial diaphyseal clavicle fractures, most re-fractures can be treated non-operatively.
To conclude, the standard of care for all diaphyseal clavicle fractures in the skeletally immature is non-operative treatment. A quicker return to sport is a relative argument to opt for surgery in the adolescent (professional) athlete. Non-union is very rare in the skeletally immature and can be treated with osteosynthesis. Most cases of initial shortening will remodel, and even most malunions will recover without functional limitations in the long term. Osteosynthesis of the clavicle should not be chosen to prevent non-union, shortening, or malunion in the skeletally immature. Corrective osteosynthesis should be reserved for rare cases with symptomatic malunion.
Proximal humerus fractures in the pediatric population are quite rare and relatively uncommon compared to other upper limb fractures in children. This fracture accounts for approximately 0.5 to 3% of all pediatric fractures[26,27]. Pediatric proximal humerus fractures are more common in boys compared to girls in most geographical areas[28].
The trauma mechanism can be a backward fall on an extended and externally rotated arm. These injuries can result from sports, horse- or bike riding, and motor vehicle accidents. In the very young, especially under 18 mo of age, one must be aware of the possibility of child abuse[29].
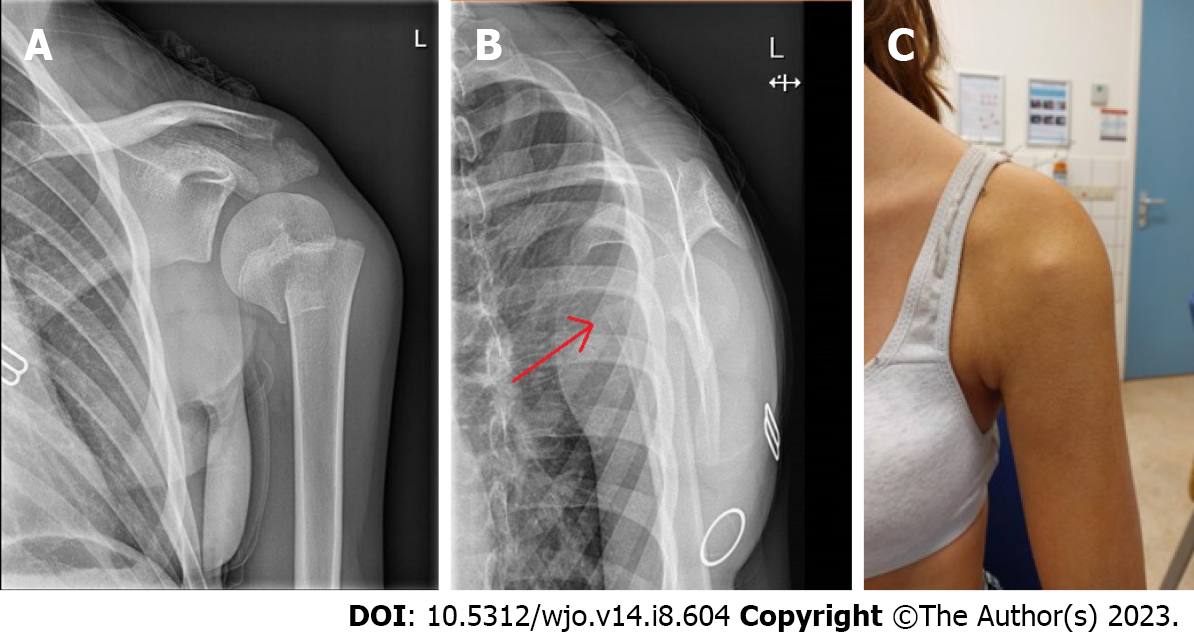
Radiographs should be carefully screened for intra-osseous pathologic lesions or cysts if a proximal humerus fracture is diagnosed after minimal trauma. Of all pathologic fractures, the proximal humerus and the proximal femur are the most common locations for a pathologic fracture to occur[30]. Unicameral or solitary bone cysts are the leading cause of these pathologic fractures. Also, the presence of pain preceding the fracture should raise the suspicion of a pathologic fracture.
Little League Shoulder is an entity on its own. This is a stress- or insufficiency fracture of the proximal humeral physis due to overuse, most commonly repetitive throwing, such as in young baseball players. Patients typically report pain while throwing. In addition, radiographs can show widening of the physis and lateral physeal fragmentation, calcification, and/or sclerosis.
The proximal humerus develops from three ossification centers (head, greater and lesser tuberosity). The ossification center of the head appears between birth and six months, followed by the ossification center of the greater tuberosity around the age of 6-18 mo. Lastly, the ossification center of the minor tuberosity appears around the age of five. These ossification centers merge into one single proximal humerus physis between the 4th and 7th year of age[31].
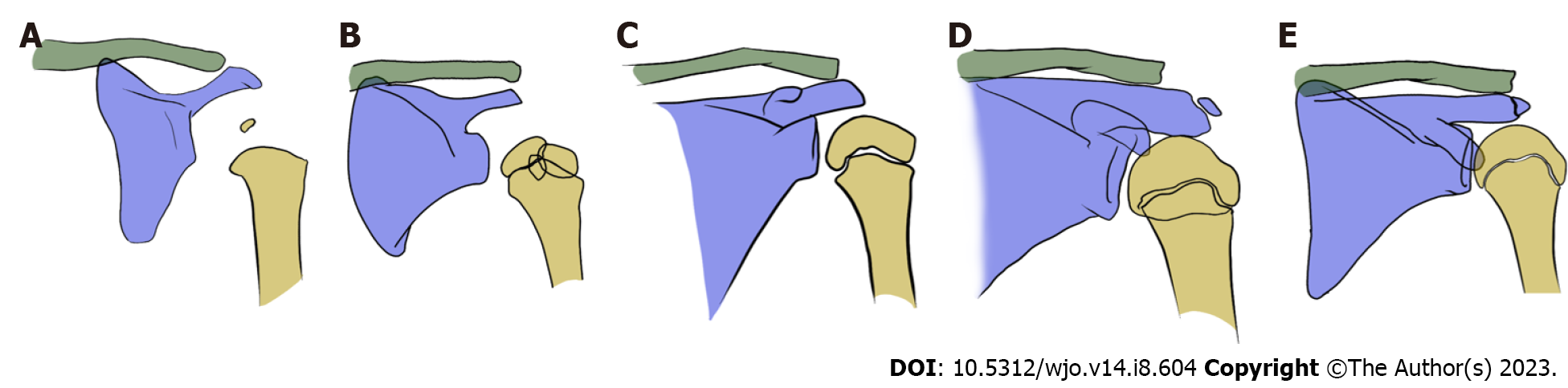
During growth, the shape of the physis changes from a rounded shape to a more V-shape or pyramidal shape, which is responsible for the double contour on an AP radiograph (Figure 2).
The physis of the proximal humerus is responsible for 80% of the longitudinal growth of the humerus and therefore has tremendous potential for remodeling. The blood supply of the humeral head is abundant and arises from the anterior and posterior humeral circumflex arteries with their anastomoses; both are branches of the axillary artery. Hence, in contrast to proximal humerus fractures in the elderly population, the risk of posttraumatic avascular necrosis is very low in the pediatric population.
Conventional radiographs are usually sufficient to diagnose this injury. AP, scapula Y (trans scapular), and axillary views are recommended. The axillary view is essential to rule out a glenohumeral dislocation or concomitant glenoid fracture. If it is impossible in the acute setting to obtain an axillary view with the arm in abduction, the Velpeau view with the arm in a sling is a valuable substitute[32]. Radiographs of the opposite shoulder can be taken for comparison if necessary. The indication for a CT scan in proximal humerus fractures is limited and should be used only in select cases, considering the ionizing radiation on the developing body.
Around 85% of all proximal humerus fractures in the pediatric population are non- or minimally displaced[28]. The amount of displacement can be graded with the Neer-Horwitz classification (Table 1). Type I and II are nondisplaced or minimally displaced fractures, less than 5 mm and less than one-third of the diameter of the shaft. Type III and IV are more severely displaced fractures with displacement of more than one-third of the shaft[33].
| Grade | Displacement |
| I | < 5 mm |
| II | < 1/3 shaft width |
| III | 1/3 – 2/3 shaft width |
| IV | > 2/3 shaft width |
The fracture type is influenced by the development of the physis, thus, the patient's age. Pre-puberty children tend to sustain more metaphyseal fractures (around 70%), and epiphyseal fractures occur more frequently in adolescents (around 30%) and are almost always Salter-Harris (SH) type I physeal separations, or SH type II with a wedge extending medially[34].
The direction of displacement is caused by the deforming forces of the muscles around the shoulder. The main direction of dislocation is varus. The supraspinatus, infraspinatus, and teres minor all pull the major tubercle, usually attached to the humeral head, posteriorly and medially, which causes the head to become dislocated in varus and external rotation. The pectoralis major pulls the shaft anteriorly and medially, a so-called "apex anterior fracture", potentially leading to a pro-curvatum deformity (Figure 3).
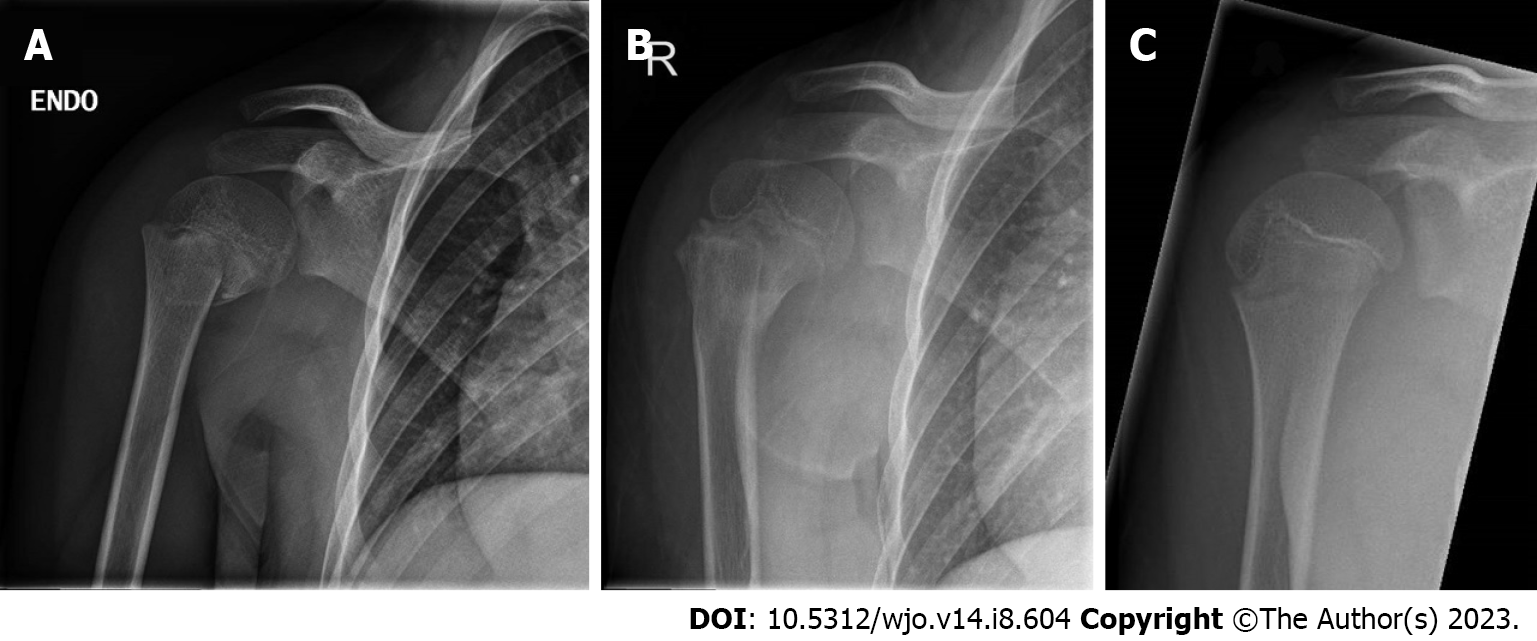
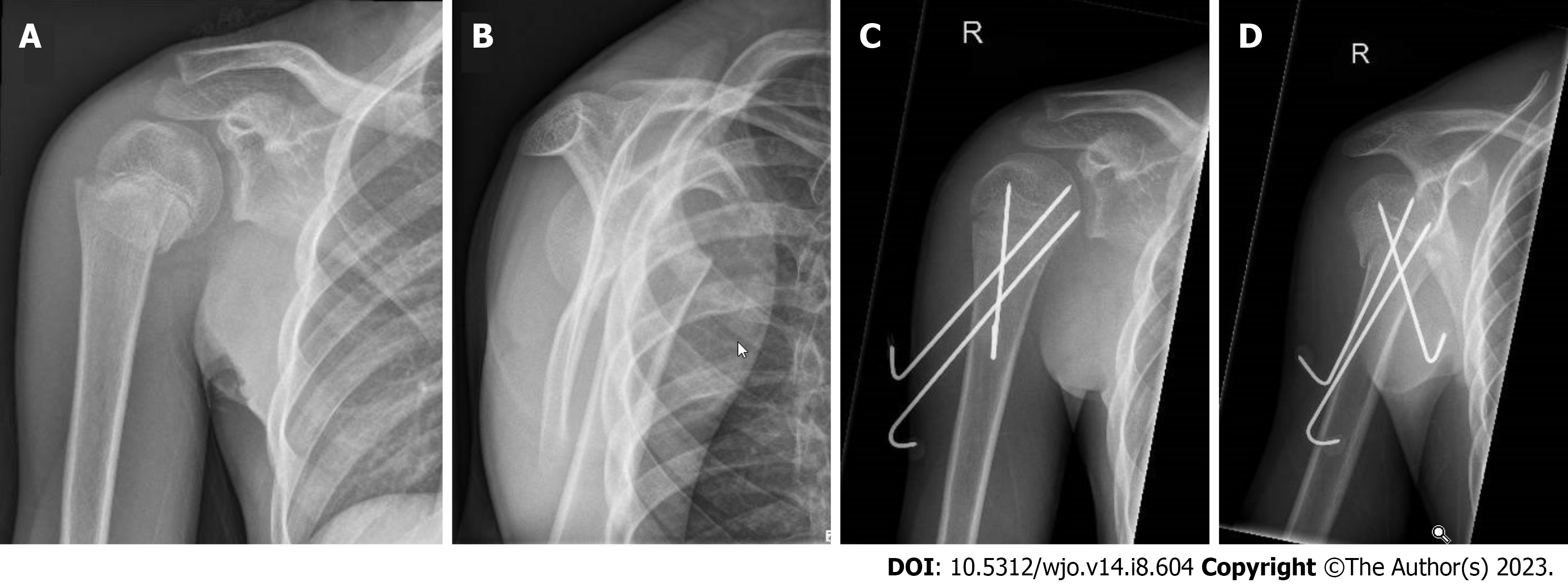
All non- or minimally displaced proximal humerus fractures (Neer types I and II) can be successfully treated conservatively without long-term shoulder complaints[35]. Treatment of displaced proximal humerus fractures remains controversial. The remaining potential for remodeling is an important factor to take into consideration. It is still difficult to judge what amount of deformity will lead to a less-than-desirable clinical outcome, and age does not correspond accurately with skeletal maturity. There are no generally accepted guidelines with clear cut-off values, and there are no randomized trials comparing conservative vs operative treatment for displaced proximal humerus fractures. However, modestly increasing trends of surgical treatment for these fractures were found in large database studies in the United States and Finland[28,36]. Most articles on this topic state that until age ten, conservative treatment is a safe option, even for severely displaced fractures[37,38]. In a comparative matched case-cohort study from Chaus et al[39], surgical treatment was compared to non-operative treatment for Neer type III and IV fractures. There were no patients younger than thirteen with a less-than-desirable outcome in the non-operative group. The risk of a poor (or less than desirable) outcome after conservative treatment of severely displaced fracture did increase substantially from the age of 13. Some authors advocate surgical treatment under the age of ten in case of 100% displacement or over 70 degrees of angulation[28,34]. But this is still debatable because of the remarkable potential of remodeling of the proximal humerus under age 10 (Figure 4).
Surgical treatment should be considered for displaced (Neer type III or IV) fractures in patients older than ten years. Kim et al[32] have shown varying cut-off values in the current relevant literature on this topic. In children aged 13 and older, cut-off values from 20 – 40 degrees angulation and over one-third of shaft displacement are found. The least consensus exists in the age group of 10 to 13 years, with 40 to 60 degrees of angulation as cut-off values as an indication for surgical treatment[32]. From the age of 13, surgery seems to have a higher success rate compared to conservative treatment in severely displaced fractures (Neer III/IV or more than 20 degrees of angulation)[37].
If surgical treatment is opted for, one should strive to avoid open reduction because deltopectoral incisions at a young age can lead to unsightly hypertrophic scar formation. Closed reduction should be attempted first. The arm should be brought into abduction (to correct the varus), and the proximal shaft should be pushed posteriorly (to counteract the anterior pull of the pectoralis major)[34]. In a minority of cases, closed reduction cannot be achieved because of interposition of soft tissue, such as the long head of the biceps, periosteum, or deltoid muscle. In these cases, open reduction through the deltopectoral approach should be considered, which is most commonly used[40]. If the reduction is adequate, fixation can be achieved by either percutaneous K-wires or retrograde elastic stable intramedullary nailing (ESIN). The advantage of percutaneous K-wires is that the surgery is quick, inexpensive, and relatively easy to perform without the need for secondary surgery. Figure 5 Immobilization in a sling or a shoulder immobilizer is required until removal of the K-wires, usually after 3-4 wk. The technique of retrograde ESIN can be somewhat more challenging but is an elegant option to treat these fractures. Two nails, diverging in the proximal fragment, should be used. Both nails should be inserted just proximal to the lateral epicondyle, taking care not to injure the radial nerve. Sharp-tipped nails should be used to perforate into the humeral head, as blunt-tipped nails may push the proximal fragment away. Immobilization can be quite minimal after ESIN, with a sling worn for two weeks. A disadvantage of ESIN is the need for a second surgical procedure to remove the nails. Removing the nails relatively early, starting from the fifth postoperative week, is recommended, given the risk of complete distal penetration into the humeral shaft caused by growth[34,37]. The functional outcome did not differ significantly between surgical treatment options in the most extensive meta-analysis[37].
According to a large meta-analysis, the overall complication rate of ESIN and K-wires was not significantly different, with 7% and 9%, respectively[37]. No cases of radial nerve injury (ESIN group) or axillary nerve injury (K-wires group) were found in this systematic review. However, premature closure of the physis with arm length discrepancy did occur more frequently in the K-wires group, up to 19% in severely displaced fractures. Although it is uncertain to what extent this was clinically relevant. Specific complications for ESIN are penetration of the humeral head, loss of reduction, and temporary elbow stiffness. However, most complications are preventable with an adequate ‘two nail’ surgical technique.
In summary, proximal humerus fractures can often be treated conservatively because of the large potential for remodeling of the proximal humerus physis, especially under age 10. However, surgery is recommended for displaced fractures (Neer types III and IV) in patients older than 13 years. Closed reduction should be attempted, and fixation with either two retrograde elastic intramedullary nails or K-wires is acceptable. For children between 10 and 13 years of age, the indication for surgical treatment is less clear, with varying cut-off values of angulation (30-60 degrees) or displacement (1/3 – 2/3 shaft width) in the current literature.
In conclusion, both clavicle and proximal humerus fractures have a large potential for remodeling in the pediatric population. Expected residual growth, and thus remodeling, is an important factor in decision-making for these fractures. Although rarely mentioned in the relevant literature, especially in young teenagers around 10 to 15 years, there is a considerable difference in residual growth for boys compared to girls at the same age. Future research, such as pediatric trauma registry data with long-term follow-up, should ideally give better insight into cut-off values of the indication for surgery in these fractures, thereby enabling evidence-based, more detailed flowcharts. Because pediatric fractures around the shoulder that need surgical intervention are uncommon, guidelines with clear indications for surgery could take pediatric trauma care to a higher level. Without clear guidelines, there is a potential risk of overtreatment (too much surgery) and the rare case that will benefit from surgery going unrecognized.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Netherlands
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dreyfuss D, Israel; Iossifidis A, United Kingdom S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Robinson CM. Fractures of the clavicle in the adult. J Bone Joint Surg Br. 1998;80-B:476-484. [RCA] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 317] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 2. | Allman FL. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am 1967; 49: 774-784. Available from: http://www.ncbi.nlm.nih.gov/pubmed/6026010. |
| 3. | Ellis HB, Li Y, Bae DS, Kalish LA, Wilson PL, Pennock AT, Nepple JJ, Willimon SC, Spence DD, Pandya NK; FACTS Study Group, Kocher MS, Edmonds EW, Farley FA, Gordon JE, Kelly DM, Busch MT, Sabatini CS, Heyworth BE. Descriptive Epidemiology of Adolescent Clavicle Fractures: Results From the FACTS (Function after Adolescent Clavicle Trauma and Surgery) Prospective, Multicenter Cohort Study. Orthop J Sports Med. 2020;8:2325967120921344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | van der Water L, Macken AA, Eygendaal D, van Bergen CJA. Pediatric Clavicle Fractures and Congenital Pseudarthrosis Unraveled. Children (Basel). 2022;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Whyte NSB, Veerkamp MW, Parikh SN. Medial clavicle shaft fractures in children and adolescents: differences from adults and management. J Pediatr Orthop B. 2022;31:417-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Kraus R, Zwingmann J, Jablonski M, Bakir MS. Dislocations of the acromioclavicular and sternoclavicular joint in children and adolescents: A retrospective clinical study and big data analysis of routine data. PLoS One. 2020;15:e0244209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Masnovi ME, Mehlman CT, Eismann EA, Matey DA. Pediatric refracture rates after angulated and completely displaced clavicle shaft fractures. J Orthop Trauma. 2014;28:648-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Vargas-Vila MA, Mehlman CT, Pennock AT. The Community Orthopaedic Surgeon Taking Trauma Call: Pediatric Midshaft Clavicle Fracture Pearls and Pitfalls. J Orthop Trauma. 2019;33 Suppl 8:S1-S5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Bae DS, Shah AS, Kalish LA, Kwon JY, Waters PM. Shoulder motion, strength, and functional outcomes in children with established malunion of the clavicle. J Pediatr Orthop. 2013;33:544-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Nordqvist A, Redlund-Johnell I, von Scheele A, Petersson CJ. Shortening of clavicle after fracture. Incidence and clinical significance, a 5-year follow-up of 85 patients. Acta Orthop Scand. 1997;68:349-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 75] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Pennock AT, Heyworth BE, Bastrom T, Bae DS, Boutelle KE, Busch MT, Edmonds EW, Ellis HB, Hergott K, Kocher MS, Li Y, Liotta ES, Pandya NK, Perkins C, Sabatini CS, Spence DD, Willimon SC, Wilson PL; FACTS Study Group, Nepple JJ. Changes in superior displacement, angulation, and shortening in the early phase of healing for completely displaced midshaft clavicle fractures in adolescents: results from a prospective, multicenter study. J Shoulder Elbow Surg. 2021;30:2729-2737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 12. | Hughes JL, Newton PO, Bastrom T, Fabricant PD, Pennock AT. The Clavicle Continues to Grow During Adolescence and Early Adulthood. HSS J. 2020;16:372-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Suppan CA, Bae DS, Donohue KS, Miller PE, Kocher MS, Heyworth BE. Trends in the volume of operative treatment of midshaft clavicle fractures in children and adolescents: a retrospective, 12-year, single-institution analysis. J Pediatr Orthop B. 2016;25:305-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Gao B, Dwivedi S, Patel SA, Nwizu C, Cruz AI Jr. Operative Versus Nonoperative Management of Displaced Midshaft Clavicle Fractures in Pediatric and Adolescent Patients: A Systematic Review and Meta-Analysis. J Orthop Trauma. 2019;33:e439-e446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Vander Have KL, Perdue AM, Caird MS, Farley FA. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J Pediatr Orthop. 2010;30:307-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 16. | Hagstrom LS, Ferrick M, Galpin R. Outcomes of operative versus nonoperative treatment of displaced pediatric clavicle fractures. Orthopedics. 2015;38:e135-e138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 17. | Li Y, Helvie P, Farley FA, Abbott MD, Caird MS. Complications After Plate Fixation of Displaced Pediatric Midshaft Clavicle Fractures. J Pediatr Orthop. 2018;38:350-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 18. | Patel M, Heyworth BE, Dehghan N, Mehlman CT, McKee MD. Clavicular Fractures in the Adolescent. J Bone Joint Surg Am. 2023;105:713-723. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Heyworth BE, Pennock AT, Li Y, Liotta ES, Dragonetti B, Williams D, Ellis HB, Nepple JJ, Spence D, Willimon SC, Perkins CA, Pandya NK, Kocher MS, Edmonds EW, Wilson PL, Busch MT, Sabatini CS, Farley F, Bae DS. Two-Year Functional Outcomes of Operative vs Nonoperative Treatment of Completely Displaced Midshaft Clavicle Fractures in Adolescents: Results From the Prospective Multicenter FACTS Study Group. Am J Sports Med. 2022;50:3045-3055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Pennock AT, Edmonds EW, Bae DS, Kocher MS, Li Y, Farley FA, Ellis HB, Wilson PL, Nepple J, Gordon JE, Willimon SC, Busch MT, Spence DD, Kelly DM, Pandya NK, Sabatini CS, Shea KG, Heyworth BE. Adolescent clavicle nonunions: potential risk factors and surgical management. J Shoulder Elbow Surg. 2018;27:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | Yahya A, Mehlman CT, Kim J, Little KJ, Parikh SN. Nonunion of the Clavicle Among Children: A Review of the Literature and a Report of Three New Cases. Orthopedics. 2022;45:e190-e195. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Endrizzi DP, White RR, Babikian GM, Old AB. Nonunion of the clavicle treated with plate fixation: a review of forty-seven consecutive cases. J Shoulder Elbow Surg. 2008;17:951-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Andermahr J, Jubel A, Elsner A, Prokop A, Tsikaras P, Jupiter J, Koebke J. Malunion of the clavicle causes significant glenoid malposition: a quantitative anatomic investigation. Surg Radiol Anat. 2006;28:447-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Sidler-Maier CC, Dedy NJ, Schemitsch EH, McKee MD. Clavicle Malunions: Surgical Treatment and Outcome-a Literature Review. HSS J. 2018;14:88-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Roner S, Bersier P, Fürnstahl P, Vlachopoulos L, Schweizer A, Wieser K. 3D planning and surgical navigation of clavicle osteosynthesis using adaptable patient-specific instruments. J Orthop Surg Res. 2019;14:115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Rose SH, Melton LJ 3rd, Morrey BF, Ilstrup DM, Riggs BL. Epidemiologic features of humeral fractures. Clin Orthop Relat Res. 1982:24-30. [PubMed] |
| 27. | Landin LA. Epidemiology of children's fractures. J Pediatr Orthop B. 1997;6:79-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 261] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 28. | Cruz AI Jr, Kleiner JE, Gil JA, Goodman AD, Daniels AH, Eberson CP. Inpatient surgical treatment of paediatric proximal humerus fractures between 2000 and 2012. J Child Orthop. 2018;12:111-116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 29. | Pandya NK, Baldwin KD, Wolfgruber H, Drummond DS, Hosalkar HS. Humerus fractures in the pediatric population: an algorithm to identify abuse. J Pediatr Orthop B. 2010;19:535-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Ortiz EJ, Isler MH, Navia JE, Canosa R. Pathologic fractures in children. Clin Orthop Relat Res. 2005;116-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Peterson H. Epiphyseal Growth plate fractures. In: Epiphyseal Growth Plate Fractures. Springer Verlag Berlin Heidelberg; 2007: 549-594. |
| 32. | Kim AE, Chi H, Swarup I. Proximal Humerus Fractures in the Pediatric Population. Curr Rev Musculoskelet Med. 2021;14:413-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 33. | Neer CS 2nd, Horwitz BS. Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res. 1965;41:24-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 112] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 34. | Lefèvre Y, Journeau P, Angelliaume A, Bouty A, Dobremez E. Proximal humerus fractures in children and adolescents. Orthop Traumatol Surg Res. 2014;100:S149-S156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 35. | Baker C, Larson N, Shaughnessy W, Stans A, Milbrandt T. Rate of Complications and Subsequent Shoulder Complaints for Non-operatively Managed Pediatric Proximal Humerus Fractures. Front Surg. 2020;7:48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Hannonen J, Hyvönen H, Korhonen L, Serlo W, Sinikumpu JJ. The incidence and treatment trends of pediatric proximal humerus fractures. BMC Musculoskelet Disord. 2019;20:571. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 37. | Hohloch L, Eberbach H, Wagner FC, Strohm PC, Reising K, Südkamp NP, Zwingmann J. Age- and severity-adjusted treatment of proximal humerus fractures in children and adolescents-A systematical review and meta-analysis. PLoS One. 2017;12:e0183157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 38. | Pahlavan S, Baldwin KD, Pandya NK, Namdari S, Hosalkar H. Proximal humerus fractures in the pediatric population: a systematic review. J Child Orthop. 2011;5:187-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 39. | Chaus GW, Carry PM, Pishkenari AK, Hadley-Miller N. Operative versus nonoperative treatment of displaced proximal humeral physeal fractures: a matched cohort. J Pediatr Orthop. 2015;35:234-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 40. | Binder H, Tiefenboeck TM, Payr S, Schurz M, Aldrian S, Sarahrudi K. Treatment of proximal humerus fractures in children and young adolescents. Wien Klin Wochenschr. 2016;128:120-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |