Published online Jul 18, 2023. doi: 10.5312/wjo.v14.i7.562
Peer-review started: December 28, 2022
First decision: April 13, 2023
Revised: April 14, 2023
Accepted: May 19, 2023
Article in press: May 19, 2023
Published online: July 18, 2023
Processing time: 201 Days and 13.7 Hours
Reconstruction of the pelvic ring anatomy in unstable anterior pelvic ring injuries is a significant step to reduce the mortality rate associated with these injuries efficiently. There is a debate on using either an anterior subcutaneous pelvis internal fixator (INFIX) or an anterior supra-acetabular external fixator (EXFIX) to manage an unstable anterior pelvic ring fracture.
To compare the functional and radiological outcomes and complications of INFIX vs EXFIX in managing unstable pelvic ring injuries.
A prospective cohort study included 54 patients with unstable pelvic ring fractures. The patients were divided into two groups; the INFIX group, in which 30 cases were fixed by INFIX, and the EXFIX group, in which 24 patients were treated by EXFIX. The average age in the EXFIX group was 31.17 years (16-57 years), while in the INFIX group, it was 34.5 years (17-53 years). The study inclu
The results revealed a statistically significant difference between both groups (P = 0.013) regarding radiological outcomes, according to Matta and Tornetta's score in favor of the INFIX group. Sitting, standing, and walking abilities were measured at a 3-mo follow-up visit using Majeed score modules. It was significantly better among the INFIX group than the EXFIX group in all three modules. At the final follow-up, both groups had no statistically significant difference according to the Majeed score; 92.35 in the INFIX group and 90.99 in the EXFIX group (P = 0.513). A lower surgical site infection rate was noticed in the INFIX group (P = 0.007).
Anterior subcutaneous pelvis INFIX is associated with better radiological outcomes and a lower infection rate than anterior supra-acetabular EXFIX in managing patients with unstable anterior pelvic ring fractures.
Core Tip: Reconstruction of the pelvic ring anatomy in unstable anterior pelvic ring injures is considered to be a great step to efficiently reduce the mortality rate associated with these types of injures. There is a debate on the use of either anterior subcutaneous pelvis internal fixator (INFIX) or anterior supra-acetabular external fixator (EXFIX) in the management of anterior unstable pelvic ring fracture. This study aimed to compare the functional, radiological outcomes as well as complications of INFIX vs EXFIX in management of unstable pelvic ring injuries. This study showed that anterior subcutaneous pelvis INFIX is associated with better radiological outcome and less rate of infection than anterior supra-acetabular EXFIX in management of patients with anterior unstable pelvic ring fractures.
- Citation: Abo-Elsoud M, Awad MI, Abdel Karim M, Khaled S, Abdelmoneim M. Internal fixator vs external fixator in the management of unstable pelvic ring injuries: A prospective comparative cohort study. World J Orthop 2023; 14(7): 562-571
- URL: https://www.wjgnet.com/2218-5836/full/v14/i7/562.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i7.562
Unstable pelvic fractures represent a complex pathology that is often life-threatening and associated with significant morbidity[1]. Although stabilization of the injured pelvis is sustained by posterior ring fixation, concurrent anterior stabilization significantly improves biomechanical stability as the anterior ring provides about 30% of the pelvic stability[2,3].
The management of anterior ring injuries is still a matter of debate. Open reduction and internal fixation using plates and screws have been traditionally prescribed. While this has proven biomechanically superior for pure ligamentous disruption of the symphysis[4], it has the disadvantage of extensive soft tissue dissection, particularly when used for proximal ramus fractures[5].
Percutaneous external fixation in unstable pelvic ring injuries has also been used as an emergency treatment and a method for definitive fixation, which can be left in place until the consolidation of the injuries. This technique aims to stabilize anterior injuries of the pelvic ring, with posterior lesions being treated as required[6,7].
The two primary technical modalities for external fixation of the anterior pelvic ring are the iliac crest and supra-acetabular routes.
The main advantage of choosing the iliac crest route is its fast application without fluoroscopic imaging. However, iliac crest frames are more likely to be associated with primary or secondary reduction failure, particularly in obese patients[8]. In contrast to the iliac crest frame, supra-acetabular pins provide a large corridor of excellent quality bone stock, which allows for a solid purchase of a single Schanz pin; however, it needs fluoroscopically guided pin placement. This technique requires high expertise to find the perfect corridor[8].
Anterior pelvic external fixator (EXFIX) has some disadvantages as it can limit patient mobilization, particularly hip flexion and side rolling, and has a high rate of pin-track infection, fixator loosening, and skin problems[9]. To avoid some of these disadvantages associated with traditional external fixation, a subcutaneous anterior pelvic internal fixator (INFIX) was described[10-12].
Technically, in the anterior pelvic INFIX, two pedicle screws are fixed into the ilium and connected to a curved subcutaneous rod. It had been reported that INFIX is associated with less pin tract infection and loosening than the anterior pelvic EXFIX, but transient neuropraxia of the lateral cutaneous nerve of the thigh and discomfort were reported as complications[11,13-15].
This study aimed to compare both fixation methods regarding the radiological quality of fracture reduction, functional outcomes, and rate of complications.
From December 2018 to December 2021, a prospective comparative cohort study included skeletally mature patients presenting with rotationally and/or vertically unstable pelvic ring fractures (Tile-type B and C) at our level 1 trauma center.
The ethical committee approved the study on December 8, 2018 with the number "N-147-2023". Exclusion criteria included stable pelvic ring fractures (Tile-type A), fractures with anterior injuries in the form of pure ligamentous symphysis pubis injuries, and pathological fractures. Furthermore, patients aged < 16 or > 65 years and those with incomplete follow-up records were also excluded.
Fifty-four patients were divided into two groups: 30 had an INFIX for anterior pelvic stabilization (the INFIX group), while the remaining 24 were treated using a supra-acetabular EXFIX group.
Standard preoperative radiographic evaluation included anteroposterior, inlet, and outlet X-ray views and computed tomography scans of the pelvis with coronal and 3-D reconstruction. Prophylaxis against deep venous thrombosis using low-molecular-weight heparin was started upon admission, stopped 12 h before surgery, and resumed for 28 d post-operation.
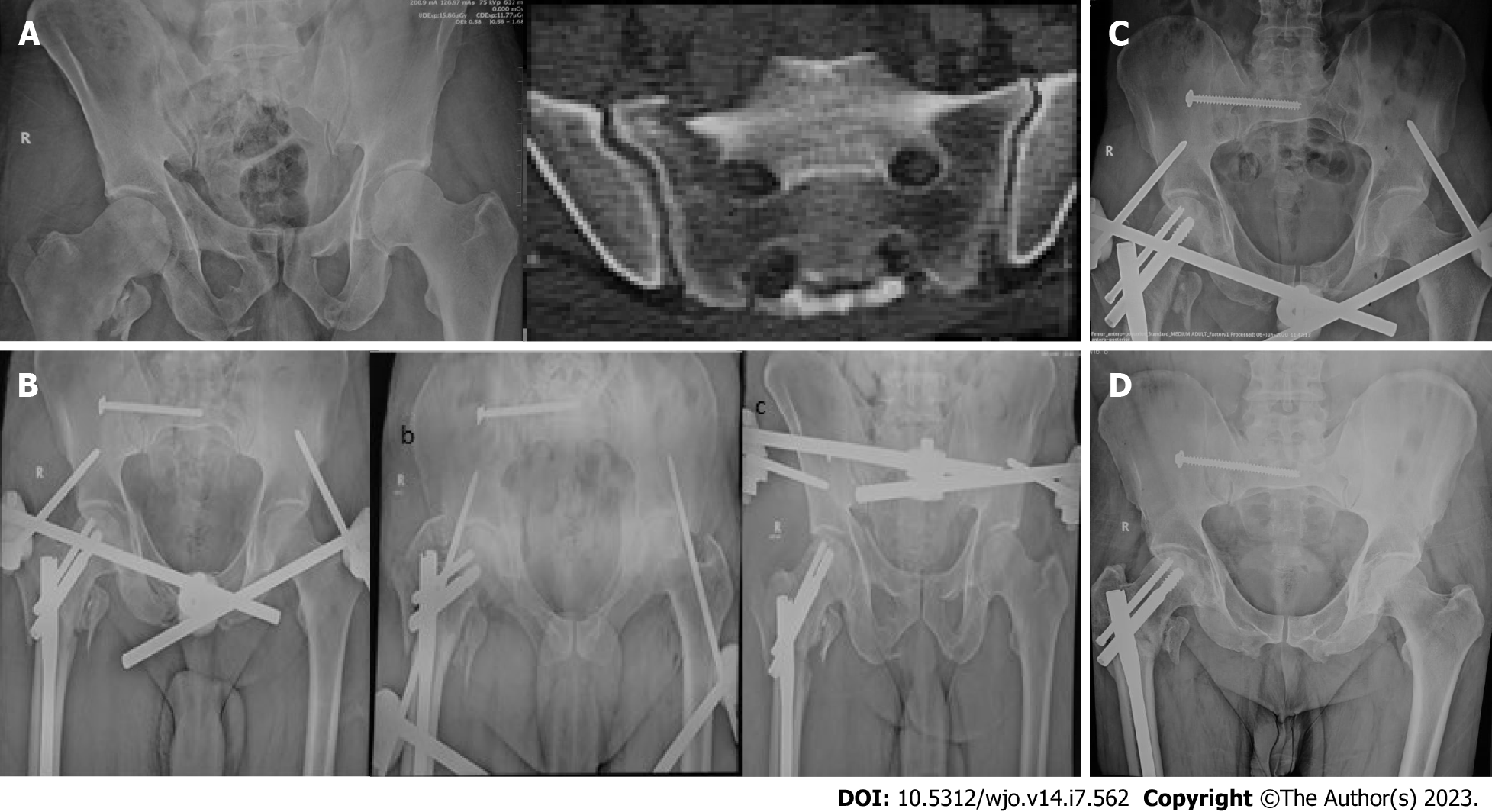
Proper fixation of the posterior pelvic ring injury was performed first, as dictated by the patho-anatomy of the fracture. For both techniques, patients were placed supine on a radiolucent table, and fluoroscopy was adjusted to identify the anterior inferior iliac spine (AIIS) as an osseous entry on the obturator outlet view (teardrop) before starting (Figure 1). In addition, fluoroscopy was used to obtain anteroposterior, inlet, outlet, iliac, and obturator inlet views.
A 3-cm longitudinal incision was then centered over the AIIS. The AIIS is not easily palpable in obese patients but generally lies 3 to 4 cm distal and 2 cm medial to the anterior superior iliac spine.
In the INFIX group, blunt dissection was performed medially to the sartorius and tensor fascia lata muscles to gain access to the AIIS. A starting awl was placed in the middle of the AIIS (the center of the teardrop) and used to open the cortex. Next, a pedicle finder was used to establish a bony tunnel toward the posterior superior iliac spine. The obturator inlet view was utilized to confirm that the tunnel had not penetrated the inner or outer tables of the iliac bone. The iliac oblique view was used to ensure the pedicle finder was clear of the hip joint and greater sciatic notch (Figure 1).
The 6.5-7.3 mm diameter and 70-100 mm length U-shaped-headed polyaxial pedicular screws (local manufacture; EgyFix spinal system: EgyFix, Cairo, Egypt) were inserted bilaterally in supra-acetabular bone. Screw heads were left proud at the level of the sartorial fascia to avoid compression of neuromuscular structures. A subcutaneous 6 mm diameter pre-contoured (short lateral transverse limbs and curved central parts with an anteroinferior bow) connecting rod was maneuvered into the screw heads to connect the screws. The screw caps were then fixed to retain the rod in place (Figure 2). Polyaxial screw heads greatly facilitate rod placement.
In the EXFIX group, a similar approach was used until the AIIS, with the difference of using the interval between the sartorius and tensor fascia lata muscles. 6 mm pins were inserted bilaterally in supra-acetabular bone with an extracorporeal connecting rod system (pins connected to each other by either one or two extracorporeal connecting rods with clamps) (Figure 3).
Reduction of the pelvis was achieved using C-rings, laminar spreaders, compression or distraction using pins in the ASIS, or even injured leg traction, according to the characteristics and morphology of the fracture. The final reduction and fixation device positions were checked with fluoroscopy.
Anteroposterior, inlet, and outlet X-ray views of the pelvis were obtained on the first postoperative day and used to grade reduction quality according to Matta and Tornetta's score[16].
Bed-to-chair mobilization was allowed from the first postoperative day, guided by the injury pattern and associated injuries. Moreover, touch weight-bearing was allowed immediately from the 2nd day up to the 6th week. Partial weight-bearing was allowed from the 6th week. After achieving full union, full-weight bearing was allowed.
Follow-up evaluations were performed at 2 and 6 wk, 3 and 6 mo, and then yearly after the operation. Sitting, standing, and walking abilities were measured at a 3-mo follow-up visit (before implant removal) using Majeed score modules[17]. The total Majeed score[17] was measured among the two groups using its six questionnaire parameters, starting at six months and at the final follow-up.
In both groups, implant removal was scheduled starting in the 12th postoperative week, guided by fracture union and a non-painful straight leg raising test. While removal of the EXFIX was usually an outpatient procedure performed in the clinic, removing the INFIX required a second anesthetic session to remove the implants. This was achieved using the same incisions as implantation.
Data were analyzed using IBM SPSS software package version 20.0 (Armonk, NY: IBM Corp.). Qualitative data were described using frequency and percent. Furthermore, quantitative data were described using the range, mean, standard deviation, median, and interquartile range. The Kolmogorov-Smirnov test was used to verify the normality of the distribution. For comparing groups, quantitative variables were analyzed using a student t-test or Mann-Whitney test, as appropriate. Chi-square and Fisher's exact tests were used for categorical data. The significance of the obtained results was judged at the 5% level.
Fifty-nine patients were recruited for the study; five were lost during follow-up and were excluded. Fifty-four patients were left for analysis; 30 for the INFIX and 24 for the EXFIX groups. These were 30 (55.6%) males and 24 (44.4%) females with a mean follow-up of 15.4 mo (range: 12-20 mo). The average age in the INFIX group was 34.5 years (range: 17-53 years) while in the EXFIX group, it was 31.2 years (range: 16-57 years). Patients’ demographics and fracture characteristics are shown in Table 1. No significant differences in age, gender, associated comorbidities, ASA score, injury mechanism, fracture classification, fracture side, preoperative displacement, operative delay and intra-operative blood loss were noticed between both groups. However, operative time was significantly shorter among the EXFIX group (mean = 20.9 ± 2.6 min, range: 16-25 min) compared to the INFIX group (mean = 41.2 ± 7.7 min, range: 28-60 min) (P < 0.001) (Table 2). The INFIX group had significantly better quality of fracture reduction scores with 93% of the patients having excellent to good reduction (compared to 70% in the EXFIX group) (P = 0.022). All fractures united by an average of 13 wk (range; 10-16 wk) with no significant difference among the two groups (P = 0.536). Implants were removed in both groups starting at 3 mo postoperatively. However, patients tended to retain INFIX for longer periods (P < 0.001) which was in-part related to better tolerance of the implant as well as logistics related to hospital surgical schedule. Moreover, 2 patients were even reluctant to remove the implant and had them retained for more than 18 mo. Lateral femoral cutaneous nerve (LFCN) injury (22%) and surgical site infection (11%) were the most common complications reported. LFCN injury was equally observed among both the INFIX and the EXFIX groups with a frequency of 23.3 and 20.8 % respectively (P = 0.826). There was a transient nerve irritation that usually improved after implant removal except for two patients (one in each group) that experienced no improvement of their symptoms. Nevertheless, these patients had mild to moderate symptoms that were medically controlled and required no further intervention. On the contrary, surgical site infection was significantly higher among the EXFIX group (P = 0.007). Eight (33.4%) patients experienced pin-track infections that were classified according to Meléndez and Colón system[18]. Fortunately, five of these were grade I infections that responded well to daily wound dressing. In addition, two patients had grade III infection that needed intravenous antibiotic therapy together with surgical wound debridement during removal of the implants after union was achieved. One patient had a severe surgical site infection (grade V) causing loosening of the pins and very early fixation failure after 2 wk. EXFIX had to be prematurely removed with wound debridement and intravenous antibiotics for two weeks. After infection clearance, revision fixation of the anterior ring fractures was done using a 3.5 mm reconstruction plate and screws. The fracture eventually united with good function at last follow-up. As regards the INFIX group, there was a single case (3.3%) of superficial surgical site infection that was treated by intravenous antibiotics and local wound dressing. No implant loosening, loss of reduction and/or fixation failures were noted for this group. In a trial to assess patients’ function before implant removal, sitting, standing, and walking abilities were measured at the 3-mo follow-up visit using Majeed score modules. INFIX group was found to have significantly better scores in all modules (Table 2). Nevertheless, patients’ function at the time of final follow-up showed no significant difference between both groups. The total Majeed score had an average of 92.3 (range: 71-100) and 91 (range: 75-100) for the INFIX and the EXFIX groups, respectively.
| EXFIX group (n = 24) | INFIX group (n = 30) | P value | |
| Age (years, mean ± SD) | 31.2 ± 10.95 | 34.5 ± 8.35 | 0.205 |
| Sex | 0.066 | ||
| M, n (%) | 10 (41.7) | 20 (66.7) | |
| F, n (%) | 14 (58.3) | 10 (33.3) | |
| Follow-up (months) | 0.0468 | ||
| Range | 12-18 | 12-20 | |
| mean ± SD | 14.8 ± 0.8 | 15.9 ± 2.4 | |
| Mode of trauma | 0.873 | ||
| Falling from height | 10 | 12 | |
| Road traffic accident | 13 | 17 | |
| Train accident | 1 | 0 | |
| Heavy object | 0 | 1 | |
| Tile classification | 0.650 | ||
| B1 | 2 | 0 | |
| B2 | 8 | 8 | |
| B3 | 3 | 7 | |
| C1 | 9 | 12 | |
| C2 | 1 | 2 | |
| C3 | 1 | 1 | |
| ASA score | 0.978 | ||
| ASA1 | 13 | 17 | |
| ASA2 | 7 | 8 | |
| ASA 3 | 4 | 5 |
| EXFIX group | INFIX group | P value | |
| Operative time (minutes) | < 0.001a | ||
| Range | 16-25 | 28-60 | |
| mean ± SD | 20.9 ± 2.6 | 41.2 ± 7.7 | |
| Quality of reduction (Matta and Torrenta score) | |||
| Excellent | 10 | 14 | 0.022a |
| Good | 7 | 14 | |
| Fair | 6 | 0 | |
| Poor | 1 | 2 | |
| Duration of fixation till removal (months) | < 0.001a | ||
| Range | 3-4 | 3-18 | |
| Median (IQR) | 3 (3-4) | 5 (3-6) | |
| Function before removal | |||
| Sitting abilities (n) | |||
| Painful | 0 | 0 | < 0.001a |
| Painful if prolonged or awkward | 8 | 0 | |
| Uncomfortable | 15 | 29 | |
| Free | 0 | 1 | |
| Standing abilities (n) | |||
| Bedridden or almost | 1 | 0 | 0.008a |
| Wheelchair | 1 | 0 | |
| Two crutches | 8 | 2 | |
| Two sticks | 4 | 2 | |
| One stick | 6 | 18 | |
| No sticks | 3 | 8 | |
| Walking abilities (n) | |||
| Cannot walk or almost | 0 | 0 | 0.042a |
| Shuffling small steps | 9 | 4 | |
| Gross limp | 6 | 4 | |
| Moderate limp | 5 | 7 | |
| Slight limp | 2 | 8 | |
| Normal | 1 | 7 | |
| Total Majeed score at the end of the follow-up | |||
| Range | 75-100 | 71-100 | 0.513 |
| mean ± SD | 91 ± 7.8 | 92.4 ± 7.2 | |
| LFCN affection, n (%) | 5 (20.8) | 7 (23.3) | 0.826 |
| Surgical site infection, n (%) | 8 (33.3) | 1 (3.3) | 0.007a |
Injuries of the pelvic ring represent 3%-8% of all fractures and are usually associated with high-energy trauma[19,20]. Combined anterior and posterior fixation is usually needed to restore pelvic stability; anterior pelvic fixation adds stability and protects the posterior fixation[2,21,22]. Open reduction and plate fixation of anterior ring fractures usually require extension lateral to the hip joint with extensive soft tissue dissection and a high risk of damaging the neurovascular structures[5]. EXFIX and, more recently, INFIX have been used for less invasive surgical options for anterior pelvic fixation.
Both techniques have provided adequate fixation, high fracture union rates, and ultimate good functional recovery[2,5,11,12,23-25]. In our series, except for one early failure due to pin-track infection, all fractures united by an average of 13 wk, and patients had good functions at the final follow-up in both groups.
However, several authors have argued that INFIX has been better tolerated than EXFIX in the postoperative period, particularly in obese patients[12]. Patients could sit, stand, lie prone, and lie on their sides normally. In addition, Vaidya et al[11] reported that nursing care for INFIX patients was easier than for EXFIX patients, especially in the intensive care unit setting, with more patient independence.
Nevertheless, these have been largely subjective opinions of treating surgeons and intensive care unit nursing staff. We measured sitting, standing, and walking abilities using Majeed score modules at the 3-mo follow-up visit for a better and more objective assessment of the patients' early functional recovery. The INFIX group showed significantly better scores in all modules. Similarly, Gardner et al[12] assessed hip flexion before INFIX removal. They found the mean hip flexion among their patients to be 96° (range: 60-120°), with 60% of them achieving flexion of 90° or more.
Moreover, better implant tolerance is reflected in the fact that patients tended to keep the INFIX for longer periods after fracture union, with some of them even declining the removal surgery. Vaidya et al[13] even reported on a patient conceiving twice (she even had normal vaginal deliveries) with the device in place. This observation, however, should be taken cautiously, as INFIX (contrary to EXFIX) requires removal inside the operating room.
Owing to its extracorporeal location, the main disadvantage of EXFIX, besides being cumbersome and limiting patient mobility, is a very high incidence of infection[9,26,27]. This is especially evident in obese patients with larger surgical wounds and greater soft tissue mobility around the transcutaneous pins[11]. This is the main selling point for INFIX. Our study highlights this fact with a highly significant difference between study groups regarding infection rates. Besides, infection with EXFIX is often associated with pin loosening, which may even lead to premature fixation failure and loss of reduction[21,26].
Moreover, EXFIX stability is affected by the distance between the bar and the bone-pin interface. In this regard, INFIX benefits from its subcutaneous location, with improved biomechanics superior to EXFIX in overall stiffness[4]. This might partially explain the better reduction quality achieved with INFIX.
However, failures were reported with INFIX. These were mostly related to the posterior fixation (mostly iliosacral screws) rather than the INFIX[5]. Nevertheless, unfamiliarity with the INFIX technique with improperly secured screw caps was reported to result in a loss of reduction requiring revision[11].
LFCN injury is a known complication with EXFIX using supra-acetabular Schanz pins. However, its incidence is usually low. On the contrary, the reported incidence of cutaneous nerve affection with INFIX was usually higher, reaching up to 55%[5]. This could be explained by the increased nerve irritation caused by the subcutaneous location of the implants, particularly the screw-rod junction. Moreover, excessive lateral rod overhang may be another contributor to nerve irritation. Several authors recommended a more medial soft tissue dissection to protect the nerve[15,21,28]. We believe that the low incidence in our series (comparable between the two groups) could be explained by the technique we adopted using the intermuscular interval between the sartorius and psoas muscles.
Femoral nerve palsy is another devastating condition; however, rare complications were reported to occur after INFIX use for pelvic fractures. Patients usually complain of delayed quadriceps weakness with gait affection in addition to anterior thigh pain and altered sensations[29]. Nevertheless, acute cases of postoperative palsy, sometimes associated with vascular compression, were reported[21,29]. It is thought that this neural affection is usually the result of the too-deep insertion of the pedicle screw heads, leading to nerve compression within the psoas muscle fascia. Despite the more medial approach we used, we had no cases of femoral nerve affection, and we believe this highlights the importance of paying careful attention to the technique and leaving the screw heads and the screw-rod junctions above the sartorial fascia. We did not use routine postoperative sonographic examination. Nevertheless, there have been reports on the safety of the INFIX with no femoral vessel compression and up to 90 degrees of hip flexion[11,15].
One last point is that INFIX is a relatively time-consuming procedure (up to one hour in some reports) requiring full fluoroscopic control[12]. Although there is a learning curve with improvements in the INFIX operative time towards the end of our study, we still found EXFIX to be a significantly more rapid procedure. Similar results were reported by Bi et al[21] comparing EXFIX to a modified three-screw INFIX technique. Thus, we strongly recommend against INFIX use for hemodynamically unstable patients. EXFIX is still the recommended technique in emergencies to rapidly reduce pelvic volume and allow for hematoma stabilization. Strengths of the study include being prospective, utilizing a similar approach for all patients, and using the Majeed score to determine the function between fixation and implant removal. Limitations of the current study include a small sample size, heterogenicity of posterior pelvic ring fractures, which may affect the failure rate of the fixation, including cases from a single trauma center, and a lack of randomization of cases in each group.
Both INFIX and EXFIX can provide anterior pelvic ring fracture stability to achieve comparable good functional and radiological outcomes. This study suggests that the anterior subcutaneous pelvis INFIX is associated with better radiological outcomes and a lower infection rate than the anterior supra-acetabular EXFIX in the management of patients with unstable anterior pelvic ring fractures. Benefits of INFIX use include easiness of sitting, standing, and walking with the implant and a low incidence of surgical site infection. On the other hand, the operative time of EXFIX is shorter, making it more suitable for emergencies.
Reconstruction of the pelvic ring anatomy in unstable anterior pelvic ring injures is considered to be a great step to efficiently reduce the mortality rate associated with these types of injures. There is a debate on the use of either anterior subcutaneous pelvis internal fixator (INFIX) or anterior supra-acetabular external fixator (EXFIX) in the management of anterior unstable pelvic ring fracture.
This is one of the very few studies comparing the INFIX vs EXFIX in management of unstable anterior pelvic ring injuries.
The objective of this study was to compare the functional, radiological outcomes as well as complications of INFIX vs EXFIX in management of unstable pelvic ring injuries.
A prospective cohort study was carried including 54 patients with unstable pelvic ring fractures. The patients were divided into two groups: INFIX group in which 30 cases were fixed by INFIX and EXFIX group in which the 24 patients were treated by EXFIX. The average age in the EXFIX group was 31.17 years (16-57 years) while in the INFIX group, it was 34.5 years (17-53 years). The study included 20 (66.7%) males and 10 (33.3%) females in the INFIX group and 10 (41.7%) males and 14 (58.3%) females in the EXFIX group. Evaluation of the radiological outcomes was done using Matta and Tornetta score and functional outcomes using Majeed score.
Fifty nine patients were recruited for the study; five were lost during follow-up. Fifty-four patients were left; 30 for the INFIX and 24 for the EXFIX groups. Operative time was shorter among the EXFIX group compared to the INFIX group (P < 0.001). INFIX group had significantly better quality of fracture reduction scores (P = 0.022). All fractures united by an average of 13 wk (range; 10-16 wk) (P = 0.536). Implants were removed in both groups starting at 3 mo postoperatively. Lateral femoral cutaneous nerve injury and infection were the most common complications reported. Infection was significantly higher among the EXFIX group (P = 0.007). Eight (33.4%) patients experienced pin-track infections that were classified according to Meléndez and Colón system. One patient had a severe surgical site infection (grade V) causing loosening of the pins and fixation failure after 2 wk. As regards the INFIX group, there was a single case (3.3%) of superficial infection that was treated by intravenous antibiotics and wound dressing. INFIX group was found to have significantly better Majeed scores in all modules. The total Majeed score had an average of 92.3 and 91 for the INFIX and the EXFIX groups, respectively.
This study suggests that anterior subcutaneous pelvis INFIX is associated with better radiological outcome and less rate of infection than anterior supra-acetabular EXFIX in management of patients with anterior unstable pelvic ring fractures. Benefits of INFIX use include easiness to sit, stand and walk with the implant and low incidence of surgical site infection. On the other hand, operative time of EXFIX is shorter which makes it more suitable for emergency situations.
Further research studies that would have more sample size, and randomization of the patients (if feasible) are required.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mayr JM, Switzerland S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Davarinos N, Ellanti P, Morris S, Mc Elwain JP. Epidemiology of pelvic and acetabular trauma in a Dublin tertiary hospital: a 10-year experience. Ir J Med Sci. 2012;181:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Bi C, Wang Q, Nagelli C, Wu J, Wang J. Treatment of Unstable Posterior Pelvic Ring Fracture with Pedicle Screw-Rod Fixator Versus Locking Compression Plate: A Comparative Study. Med Sci Monit. 2016;22:3764-3770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Hao T, Changwei Y, Qiulin Z. Treatment of posterior pelvic ring injuries with minimally invasive percutaneous plate osteosynthesis. Int Orthop. 2009;33:1435-1439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Vigdorchik JM, Esquivel AO, Jin X, Yang KH, Onwudiwe NA, Vaidya R. Biomechanical stability of a supra-acetabular pedicle screw internal fixation device (INFIX) vs external fixation and plates for vertically unstable pelvic fractures. J Orthop Surg Res. 2012;7:31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 81] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 5. | Dahill M, McArthur J, Roberts GL, Acharya MR, Ward AJ, Chesser TJS. The use of an anterior pelvic internal fixator to treat disruptions of the anterior pelvic ring: a report of technique, indications and complications. Bone Joint J. 2017;99-B:1232-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Kellam JF. The role of external fixation in pelvic disruptions. Clin Orthop Relat Res. 1989;66-82. [PubMed] |
| 7. | Kellam JF, Helfet DL, Tile M, Vrahas M. Fractures of the pelvis and acetabulum: Principles and methods of management. Stuttgart. Thieme. 2015;. [DOI] [Full Text] |
| 8. | Stahel PF, Mauffrey C, Smith WR, McKean J, Hao J, Burlew CC, Moore EE. External fixation for acute pelvic ring injuries: decision making and technical options. J Trauma Acute Care Surg. 2013;75:882-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Mason WT, Khan SN, James CL, Chesser TJ, Ward AJ. Complications of temporary and definitive external fixation of pelvic ring injuries. Injury. 2005;36:599-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 109] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 10. | Kuttner M, Klaiber A, Lorenz T, Füchtmeier B, Neugebauer R. [The pelvic subcutaneous cross-over internal fixator]. Unfallchirurg. 2009;112:661-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 11. | Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A. Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma. 2012;26:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 142] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 12. | Gardner MJ, Mehta S, Mirza A, Ricci WM. Anterior pelvic reduction and fixation using a subcutaneous internal fixator. J Orthop Trauma. 2012;26:314-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 13. | Vaidya R, Martin AJ, Roth M, Tonnos F, Oliphant B, Carlson J. Midterm Radiographic and Functional Outcomes of the Anterior Subcutaneous Internal Pelvic Fixator (INFIX) for Pelvic Ring Injuries. J Orthop Trauma. 2017;31:252-259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Vaidya R, Kubiak EN, Bergin PF, Dombroski DG, Critchlow RJ, Sethi A, Starr AJ. Complications of anterior subcutaneous internal fixation for unstable pelvis fractures: a multicenter study. Clin Orthop Relat Res. 2012;470:2124-2131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 15. | Fang C, Alabdulrahman H, Pape HC. Complications after percutaneous internal fixator for anterior pelvic ring injuries. Int Orthop. 2017;41:1785-1790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Matta JM, Tornetta P 3rd. Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res. 1996;129-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 298] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 17. | Majeed SA. External fixation of the injured pelvis. The functional outcome. J Bone Joint Surg Br. 1990;72:612-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 74] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Meléndez EM, Colón C. Treatment of open tibial fractures with the Orthofix fixator. Clin Orthop Relat Res. 1989;224-230. [PubMed] |
| 19. | Gänsslen A, Pohlemann T, Paul C, Lobenhoffer P, Tscherne H. Epidemiology of pelvic ring injuries. Injury. 1996;27 Suppl 1:S-A13. [PubMed] |
| 20. | Giannoudis PV, Pape HC. Damage control orthopaedics in unstable pelvic ring injuries. Injury. 2004;35:671-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 175] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 21. | Bi C, Wang Q, Wu J, Zhou F, Zhang F, Liang H, Lyu F, Wang J. Modified pedicle screw-rod fixation vs anterior pelvic external fixation for the management of anterior pelvic ring fractures: a comparative study. J Orthop Surg Res. 2017;12:185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Tile M. The management of unstable injuries of the pelvic ring. J Bone Joint Surg Br. 1999;81:941-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 50] [Reference Citation Analysis (0)] |
| 23. | Arazi M, Kutlu A, Mutlu M, Yel M, Kapiciğlu MI. The pelvic external fixation: the mid-term results of 41 patients treated with a newly designed fixator. Arch Orthop Trauma Surg. 2000;120:584-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Scaglione M, Parchi P, Digrandi G, Latessa M, Guido G. External fixation in pelvic fractures. Musculoskelet Surg. 2010;94:63-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Tucker MC, Nork SE, Simonian PT, Routt ML Jr. Simple anterior pelvic external fixation. J Trauma. 2000;49:989-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 77] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Lindahl J, Hirvensalo E, Böstman O, Santavirta S. Failure of reduction with an external fixator in the management of injuries of the pelvic ring. Long-term evaluation of 110 patients. J Bone Joint Surg Br. 1999;81:955-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 96] [Reference Citation Analysis (0)] |
| 27. | Solomon LB, Pohl AP, Sukthankar A, Chehade MJ. The subcristal pelvic external fixator: technique, results, and rationale. J Orthop Trauma. 2009;23:365-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Wang Q, Wang Q, Wang J. Treatment of type B pelvic fracture using anterior subcutaneous internal fixator with triple pedicle screws: a new surgical technique. Arch Orthop Trauma Surg. 2017;137:887-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 29. | Hesse D, Kandmir U, Solberg B, Stroh A, Osgood G, Sems SA, Collinge CA. Femoral nerve palsy after pelvic fracture treated with INFIX: a case series. J Orthop Trauma. 2015;29:138-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |