Published online Jul 18, 2023. doi: 10.5312/wjo.v14.i7.516
Peer-review started: February 22, 2023
First decision: April 13, 2023
Revised: May 10, 2023
Accepted: June 6, 2023
Article in press: June 6, 2023
Published online: July 18, 2023
Processing time: 146 Days and 10.5 Hours
The timing of operative treatment for pediatric supracondylar humerus fractures (SCHF) and femoral shaft fractures (FSF) remains controversial. Many fractures previously considered to be surgical emergencies, such as SCHF and open fractures, are now commonly being treated the following day. When presented with an urgent fracture overnight needing operative treatment, the on-call surgeon must choose whether to mobilize resources for a late-night case or to add the case to an elective schedule of the following day.
To describe the effect of a program allowing an early operating room (OR) start for uncomplicated trauma prior to an elective day of surgery to decrease wait times for surgery for urgent fractures admitted overnight.
Starting in October 2017, patients were eligible for the early slot in the OR at the discretion of the surgeon if they were admitted after 21:00 the previous night and before 05:00. We compared demographics and timing of treatment of SCHF and FSF treated one year before and after implementation as well as the survey responses from the surgical team.
Of the 44 SCHF meeting inclusion criteria, 16 received treatment before imple
Our findings demonstrate significantly reduced wait times for surgery for uncomplicated SCHF presenting overnight while discussing the importance of shared decision-making with the stakeholders. Although the program produced promising results, it also created new conflicts within the OR staff that led to its discontinuation at our institution. Future implementations of such programs should involve stakeholders early in the planning process to better address the needs of the OR staff.
Core Tip: This study describes the effect of a program allowing an early operating room start for uncomplicated trauma prior to an elective day of surgery to decrease wait times for surgery for urgent fractures admitted overnight. After imple
- Citation: Kym D, Kaur J, Pham NS, Klein E, Langner JL, Wang E, Vorhies JS. Effectiveness of an early operating room start time in managing pediatric trauma. World J Orthop 2023; 14(7): 516-525
- URL: https://www.wjgnet.com/2218-5836/full/v14/i7/516.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i7.516
The timing of operative care for pediatric orthopedic injuries is a subject of controversy. Recent studies comparing early vs delayed intervention for supracondylar humerus fractures (SCHF) in children have challenged the conventional wisdom that postponing cases leads to unsatisfactory results[1-3]. Many fractures that were previously considered to be surgical emergencies, such as SCHF and open fractures, are now commonly being treated the following day. This avoids potentially inefficient provision of care by an on-call team who may not be as well-rested or as familiar with pediatric orthopedic care as a day team[4,5]. Despite this shift away from overnight care, a safe and expeditious provision of care remains in the best interest of the patient and family. The timely provision of care for urgent fractures thus presents a logistical challenge to hospitals.
SCHF and femoral shaft fractures (FSF) are among the most common surgically treated pediatric fractures, with SCHF accounting for 60% of pediatric elbow fractures and FSF being the most common diaphyseal fracture in children[6-10]. Given their high incidences, the timeliness of their treatment continues to be a metric used for United States News and World Report’s ranking of children’s hospitals[8]. This presents a challenge for hospitals with moderate trauma volume that is insufficient to justify a daily trauma room. When presented with an urgent fracture overnight needing operative treatment, the on-call surgeon must choose whether to mobilize resources for a late-night case or to add the case to an elective schedule of the following day.
Here we describe the effect of the 6 AM start quality improvement program implemented at a suburban level I trauma center. This program was designed to decrease wait times for urgent trauma cases while minimizing surgeon fatigue, thereby increasing the efficiency of care and improving compliance with United States News and World Report’s standard for timely management.
Implemented at our facility in October 2017, the 6 AM start program allowed the orthopedic surgeon on call overnight to book an uncomplicated case for an early start in the operating room (OR) at 06:00 prior to the start of a typical elective surgery weekday (Monday through Friday, excluding holidays) at 07:30. Patients with SCHF and FSF were eligible if they were admitted to the ED after 21:00 the prior day and indicated for surgical treatment at the discretion of the surgeon. Surgeon-controlled time in the OR also had to be projected at less than 75 min.
We received IRB approval (IRB #46989) which granted a waiver of consent and assent. We queried our electronic medical record system for all pediatric patients who underwent surgical fixation for closed isolated SCHF (CPT codes: 24538, 24545, 24546) or FSF (CPT codes: 27502, 27506, 27507) from October 2016 to October 2018. We included patients who were admitted to the ED between 19:00 and 05:00 as the program was often applied to patients technically admitted earlier than 21:00 who had a long wait for an orthopedic consult. Patients admitted on Friday or Saturday nights as well as on the eve of a holiday were excluded. Those over age 12 for SCHF and eight for FSF were excluded since they were more likely to have adult or transitional fracture patterns indicating fixation methods that exceed the projected-surgeon control time of 75 min. Complicated cases including open fractures, threatened vascular status, concurrent ipsilateral fractures, and pathological fractures were excluded.
Patient charts were screened for patient and fracture characteristics. The outcome measure of this study was the wait time for surgery, defined as the time between ED admittance and the patient’s arrival at the OR. Balancing measures included the operative duration (time between start and end of the procedure), post anesthesia care unit (PACU) length-of-stay (LOS), time between arrival and departure from the PACU, and wait time for discharge (time between departure from the PACU and discharge). Cases were further classified as overnight cases, 6 AM start cases, and add-on cases based on their scheduled start time as more than 1.5 h prior, 1.5-1 h prior, and after the start of the elective surgery weekday, respectively. The percentage of eligible cases that utilized the 6 AM start program served as the process measure for this study.
For additional balancing measures, all OR staff received an anonymous electronic survey through the internal hospital distribution lists. The survey asked respondents to score their level of agreement on a Likert scale with five statements regarding the beneficiaries of the program and the effectiveness of the program. Additional text boxes allowed providers to explain their responses and provide general feedback.
Statistical analyses were performed with RStudio (Boston, MA) using a two-sided level of significance of 0.05. Baseline characteristics among groups were tested using two-sample t-tests, Mann-Whitney U-tests, and Fisher’s exact tests. Wait time for surgery, operative duration, PACU LOS, and wait time for discharge were compared between patients admitted before and patients admitted after the implementation of the program using two-sample t-tests or Mann-Whitney U-tests. The same outcome variables were compared among patients whose surgeries were scheduled at the three aforementioned time points (overnight cases, 6 AM start cases, and add-on cases) using one-way ANOVA tests and Kruskal-Wallis tests, with Tukey-adjusted P values and Dunn’s test for pairwise comparisons. For the survey analysis, responses to the five survey items were compared between various roles in the surgical team using one-way ANOVA tests with Bonferroni-adjusted P values for pairwise comparisons.
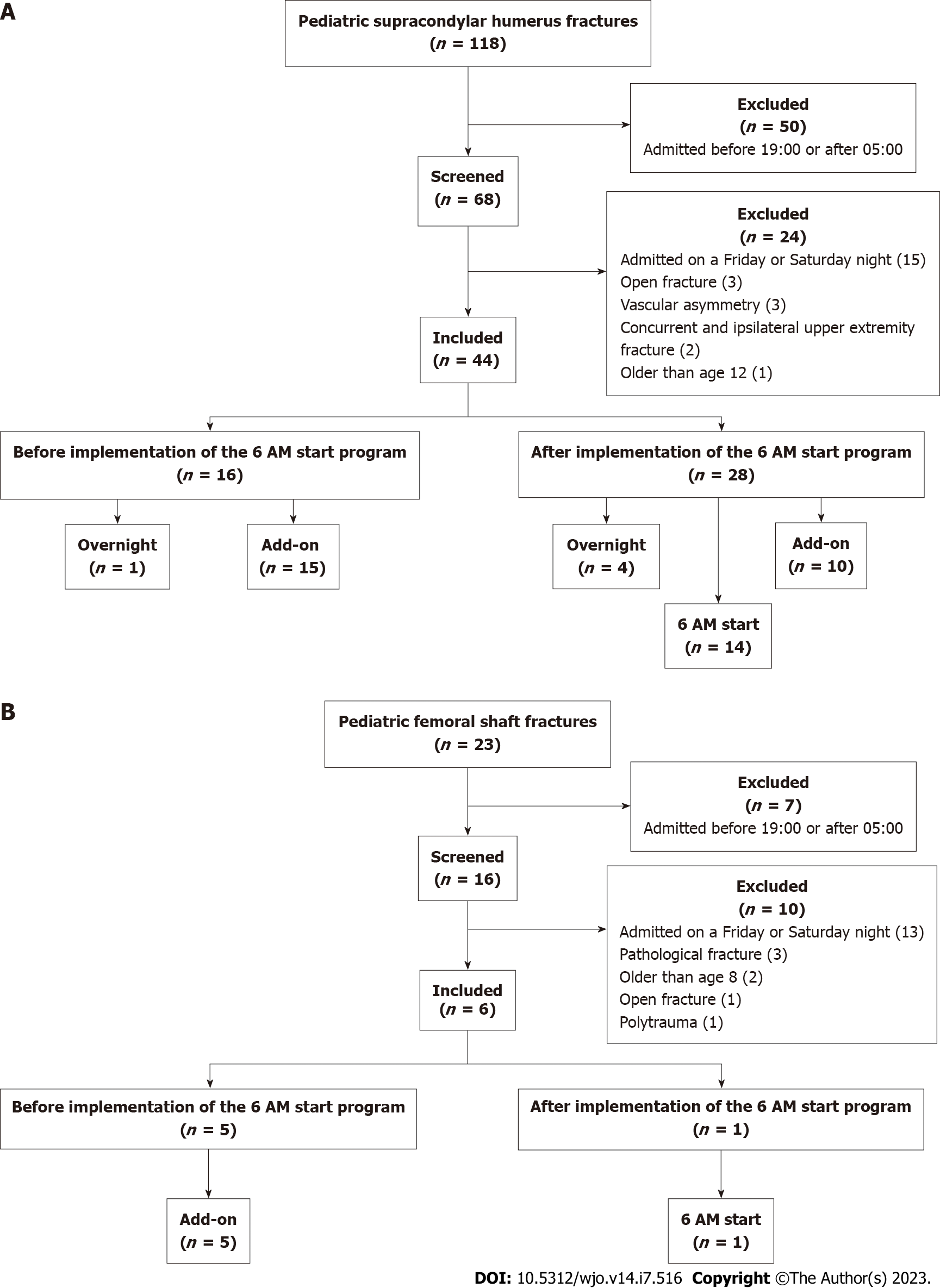
We initially identified 118 pediatric patients with SCHF and 23 with FSF treated during the study period. After applying the exclusion criteria, 44 SCHF and six FSF were included in the study (Figure 1). For SCHF, 16 patients received operative treatment before the program’s implementation and the other 28 were treated after. There were no significant differences in patient and fracture characteristics between the two groups (Table 1). After the implementation of the 6 AM start program, the mean wait time for surgery for patients presenting overnight with uncomplicated SCHF decreased by 4.8 h or 35.4% (13.4 h vs 8.7 h; P = 0.001). There were no significant differences in the operative duration, PACU LOS, or wait time for discharge (Table 2). The before-implementation group for SCHF included one (6%) overnight case and 15 (94%) add-on cases. The after-implementation group was composed of four (14%) overnight cases, 14 (50%) 6 AM start cases, and 10 (36%) add-on cases. Other than the significantly decreased wait time for surgery, the three subgroups in the after-implementation group showed no differences in demographics and subsequent phases of patient care (Tables 3 and 4).
| Total (n = 44) | Before implementation (n = 16) | After implementation (n = 28) | P value | |
| Female, % (n) | 61 (27) | 56 (9) | 64 (18) | 0.182 |
| Age | 5.1 | 5.1 | 5.1 | 0.912 |
| Gartland classification, % (n) | 0.686 | |||
| Type I | 0 (0) | 0 (0) | 0 (0) | |
| Type II | 38.6 (17) | 31.3 (5) | 42.9 (12) | |
| Type III | 52.2 (23) | 56.3 (9) | 50 (14) | |
| Type IV | 9.09 (4) | 12.5 (2) | 7.14 (2) | |
| Reduction, % (n) | 0.732 | |||
| Closed | 95.5 (42) | 100 (16) | 92.9 (26) | |
| Open | 4.6 (2) | 0 (0) | 7.14 (2) |
| Total (n = 44) | Before implementation (n = 16) | After implementation (n = 28) | P value | |
| Wait time for surgery, h | 10.4 ± 9.3 | 13.4 ± 8.6 | 8.6 ± 7.9 | 0.001 |
| Operative duration, min | 31.5 (24.5-35.3) | 30.5 (21.5-37.5) | 31.5 (24.5-35.3) | 0.817 |
| PACU LOS, h | 1.34 (1.2-1.6) | 2 ± 1.6 | 1.4 (1.2-1.6) | 0.060 |
| Wait time for discharge, h | 4.96 (3.5-9.7) | 3 (0.01-7.21) | 5 (3.5-9.7) | 0.924 |
| Overnight cases (n = 4) | 6 AM cases (n = 14) | Add-on cases (n =10) | P value | |
| Female, % (n) | 100 (4) | 57.1 (8) | 60 (6) | 0.271 |
| Age | 6 | 4 | 6.3 | 0.310 |
| Gartland classification, % (n) | 0.514 | |||
| Type I | 0 (0) | 0 (0) | 0 (0) | |
| Type II | 50 (2) | 42.9 (6) | 40 (4) | |
| Type III | 25 (1) | 50 (7) | 60 (6) | |
| Type IV | 25 (1) | 7.1 (1) | 0 (0) | |
| Reduction, % (n) | 0.210 | |||
| Closed | 75 (3) | 100 (14) | 90 (9) | |
| Open | 25 (1) | 0 (0) | 10 (1) |
| Night cases (n = 4) | 6 AM cases (n = 14) | Add-on cases (n = 10) | P value | |
| Wait time for surgery, h | 2.3 ± 0.2 | 8.2 ± 2.4 | 11.8 ± 3.1 | 1.19e-06 |
| Operative duration, min | 30.5 (27.5-71.5) | 33.5 ± 7.7 | 25.5 (19-35) | 0.229 |
| PACU LOS, h | 1.2 ± 0.3 | 1.4 (1.2-1.6) | 1.5 (1.1-1.6) | 0.681 |
| Wait time for discharge, h | 8.9 ± 6.6 | 6.5 ± 3.6 | 3.6 (0.9-3.9) | 0.410 |
This study identified five FSF cases treated before the program’s implementation and one case treated after. A case in the former group had an incorrectly recorded time of discharge and was thus excluded from the calculation for the wait time for discharge. All patients in the before-implementation group were add-on cases, while the one case in the after-implementation group was a 6 AM start case. Although sample size precludes a meaningful statistical analysis, the 6 AM start case had a shorter wait time for surgery by 4.2 h or 30.2% [13.9 (12.7-19.6) h vs 9.7 h] than the before-implementation group. Otherwise, it had a longer operative duration (61 ± 42 min vs 138 min), PACU LOS (1.6 ± 1.1 h vs 3.2 h), and wait time for discharge [12.4 (4.4-42.9) h vs 51.1 h].
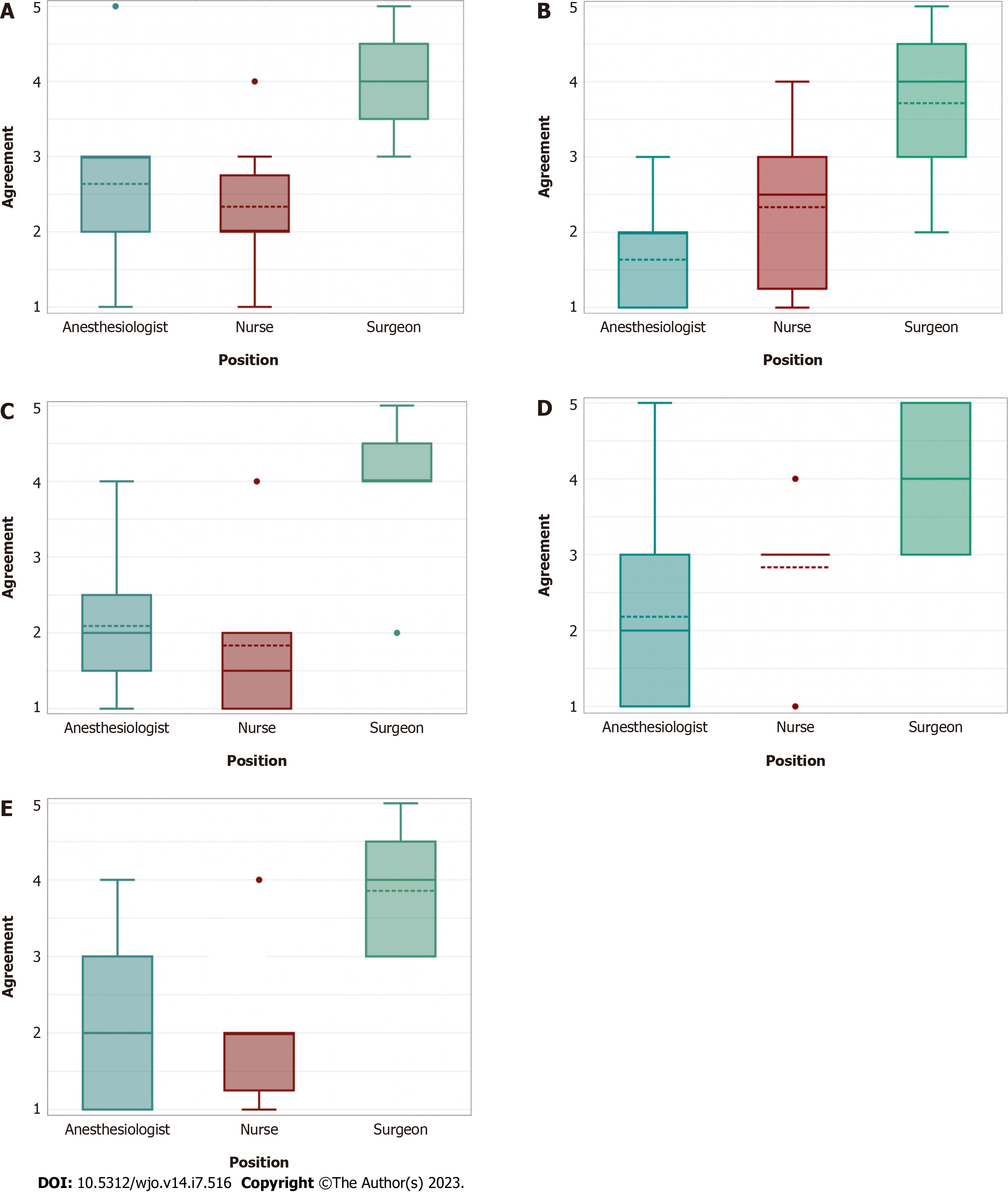
There were a total of 24 survey respondents which was composed of 11 (46%) anesthesiologists, seven (29%) surgeons, and six (25%) nurses. 17 (70.8%) respondents directly participated in a 6 AM surgery while five (20.8%) respondents did not; two (8.4%) respondents did not answer the prompt. Since many of the OR staff are involved in scheduling cases without directly participating in the surgery or may have participated in other surgeries that were affected by the program’s policy, all 24 respondents were included in the analysis.
Univariate analysis showed a significant difference in responses among anesthesiologists, nurses, and surgeons for all five survey questions. Further pairwise comparisons revealed that anesthesiologists reported more dissatisfaction than surgeons for all five items. Furthermore, nurses reported lower opinions on the program’s benefit to the patient, ease of placing urgent trauma cases, and overall effectiveness than surgeons (Figure 2). Seven (29%) providers cited that the program benefited patient care because of the efficiency, stating that “patients received surgical care more quickly”. However, four (17%) providers disagreed as they “felt that the timing of the 6 AM cases typically did not end at an appropriate time” and “caused delays for scheduled patients”. Regarding the program’s benefit to the staff, eight (33%) providers commented that the early hours were an issue with reports of being “frustrated having to come back to the hospital for a 6 AM start” and concluding that it was “a horrible time to do a case”. In the feedback section, seven (29%) providers expressed their dislike of the program while seven (29%) providers liked the program as “it gave a time for patients to be scheduled in a timely manner” and “benefited patient care”. Six (25%) providers suggested that either “starting at 7:30 (or) having a bump room for quick ortho cases is preferred”. Regarding the program’s benefit to the hospital, while four (17%) providers believed that the program positively impacts the United States News and World Report scores, four (17%) staff members expressed that “the intangible negative effects on nursing and anesthesiologists far outweighed any USNWR points it got (the hospital)”.
The provision of consistent and timely pediatric orthopedic trauma care can present logistical challenges when available OR space and patient volumes render a daily trauma or add-on room inefficient. Our study evaluated the effectiveness of a program that made available an earlier slot in the OR for uncomplicated fractures presenting to the ED overnight, thus facilitating timely care without disrupting the daily elective schedule or mobilizing resources for an urgent case at night. Before the implementation of this program, it was not uncommon for an urgent case presenting overnight to wait until the end of a scheduled day of elective cases in the following afternoon or evening. Our findings suggest that the 6 AM start program facilitated more timely care for patients with uncomplicated fractures presenting overnight without significant consequences to subsequent phases of patient care.
The timeliness of operative treatment for SCHF and FSF continues to be in dispute in the medical community. Furthermore, studies use different standards for what is considered early and delayed intervention[11-13]. For the ranking of children’s hospitals, United States News and World Report defines timely management as the treatment for SCHF and FSF within 18 h of presentation to the ED. For SCHF, hospitals receive one point for ≥ 75% and < 90% of cases that meet this definition and two points for ≥ 90%; for FSF, hospitals are awarded one point for ≥ 60% and < 80% of cases and two points for ≥ 80%[8]. A review of the literature calls into question the wisdom of rewarding hospitals for expedited care and in absence of literature support any improved patient outcomes with expedited care. For example, a study in Texas of 399 SCHF demonstrated that a delay in surgery of greater than 24 h did not result in increased rate of complications for type II SCHF[14].
At our own institution we previously published a review of 153 patients with SCHF and we found no significant differences in outcomes among SCHF operated on overnight vs daytime surgery however surgery between midnight and 6 AM was associated with slightly a higher rate of malunion[15].
The treatment of type III SCHF is perhaps more controversial. A retrospective review of 172 patients spanning different severities of from the United Kingdom found no increasing complications when supracondylar fractures arriving after hours are managed the following day vs overnight[16].
Similarly, a recent report from Japan including 244 patients found that delaying treatment more than 12 h did not affect the rate of complications after surgery for Gartland type II or III SCHF[17]. A recent paper from Boston Children’s Hospital demonstrated that at that institution 35% of type III and IV SCHF presenting overnight are operated on the night they presented while the remainder were treated the following day. No difference in complication rate was found based on timing of treatment. Based on their existing practice patterns they suggested that patients with potential neurovascular compromise or displacement of any cortex by greater than 25 mm should be considered for treatment overnight[18]. Despite the lack of any clinically demonstrable threshold for a delay in care that predicts poor outcomes, expediting care may have other benefits to families and patients. Furthermore timeliness of care continues to be a benchmark process metric of quality.
In this study, the percentage of cases with wait times for surgery within 18 h of ED admittance increased from 81% to 100% for SCHF and 56% to 100% for FSF after the implementation of the program. This translates to an additional award of two points to achieve the maximum of four points in this category. These findings support the 6 AM start program as an effective alternative to designated trauma rooms for reducing wait times for operative treatment for uncomplicated fractures, benefiting both patients and the institutions that do not have the OR space or trauma volume to render a trauma room cost-effective.
However, the survey responses highlight issues to address for future attempts at implementation of similar programs. The survey uncovered a significant disparity in opinions about the program amongst the staff, in particular those of surgeons vs those of anesthesiologists and nurses. This is partly attributed to the time of transition from overnight calls to daytime shifts at our institution. Surgeons typically take a home call followed by a clinic or OR day. In contrast, the on-call anesthesiologist has a 24-h shift from 07:00 to 07:00, making the 6 AM start case the 24th h of their shift. Nurses also change shifts at 07:00. Thus surgeons would take on the 06:00 fracture cases as their first or only surgery of the day while overnight anesthesiologists and nurses would have to either come in from home or stay until the last hour of their shift. This led nurses and anesthesiologists to feel that the program took advantage of OR staffing to facilitate the surgeon’s schedule. Several nurses and anesthesiologists voiced concerns that the elective schedule was often delayed if the 06:00 case did not start on time or ran over the expected time. The nursing staff also felt that mobilizing for an urgent case at 06:00 was inefficient because the 06:00 h is typically spent preparing the following day’s cases. Several nurses questioned the logic of waiting until 06:00 if the OR and staff were available to do the case sooner.
While the 6 AM start program was effective in reducing wait times for surgery, it was ultimately discontinued at our institution after one year, based in large part on the aforementioned inefficiencies and the extreme unpopularity of the program with non-surgeons. This outcome could potentially have been mitigated had anesthesiologists, nurses, and surgical technologists been invited earlier to plan and facilitate the implementation of the program. Many authors have stressed the importance of multidisciplinary teams in the success of quality improvement initiatives[19]. We recommend other institutions consider adopting similar programs to engage stakeholders early in the planning process to minimize the risks of unintended consequences and customize the program to best fit the structure of each institution.
With this study’s retrospective design, we were also unable to ensure adherence to the protocol of scheduling eligible cases and starting the case on time which influenced the opinions of some OR staff. Factors other than the imple
We have demonstrated that our 6 AM start program was effective in reducing the wait time for operative treatment for uncomplicated SCHF presenting overnight. This is of interest and benefit to institutions as United States News and World Report uses timeliness of operative treatment for SCHF and FSF as a metric for ranking children’s hospitals. Although the program produced promising results, it also created new conflicts within the OR staff that led to its discontinuation at our institution. This information may be useful to surgeons and hospital administrators as they undertake quality improvement programs to enhance the timeliness of care. Future implementations of such programs should involve stakeholders early in the planning process to better address the needs of the OR staff.
This study describes the effect of a program allowing an early operating room (OR) start for uncomplicated trauma prior to an elective day of surgery to decrease wait times for surgery for urgent fractures admitted overnight.
The timing of operative treatment for pediatric supracondylar humerus fractures (SCHF) and femoral shaft fractures (FSF) remains controversial.
We present the impact of the quality improvement program initiated at a suburban level I trauma center, aiming to enhance the efficiency of care and adhere to United States News and World Report’s standard for timely management. The program specifically focuses on reducing wait times for urgent trauma cases and mitigating surgeon fatigue by implementing a 6 AM start.
From October 2017 onwards, patients admitted between 21:00 the previous night and 05:00 were considered for the early slot in the OR, subject to the surgeon’s judgment. To evaluate the effects of this change, we analyzed the demographic characteristics and treatment timelines of patients with SCHF and FSF, comparing data from one year before and one year after the implementation. Additionally, we gathered survey responses from the surgical team for further insights.
Out of the 44 SCHF cases that met the inclusion criteria, 16 underwent treatment prior to the program’s implementation, while 28 received treatment afterward. Following the implementation, the average wait time for surgery decreased by 4.8 h or 35.4% (from 13.4 h to 8.7 h; P = 0.001). However, no significant differences were observed in operative duration, post anesthesia care unit stay, or discharge wait time. Survey responses indicated a decline in the program’s popularity among nurses and anesthesiologists compared to surgeons. While 57% of surgeons believed the program was effective, only 9% of anesthesiologists and 16% of nurses shared the same opinion. Due to the overall dissatisfaction, the program was eventually discontinued.
The results of our study highlight a significant decrease in surgery wait times for uncomplicated SCHF cases admitted overnight. Additionally, we emphasize the significance of engaging stakeholders in shared decision-making. While the program yielded promising outcomes, it also gave rise to conflicts among the OR staff, ultimately leading to its discontinuation at our institution. Moving forward, it is essential to involve stakeholders early on during the planning phase of similar programs to effectively address the OR staff’s requirements and concerns.
Surgeons and hospital administrators engaging in quality improvement initiatives to improve the timeliness of care can find value in this information. It is recommended that future implementations of such programs involve stakeholders from the outset of the planning process to ensure better alignment with the needs of the OR staff.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: Ruth Jackson Orthopaedic Society (RJOS); J. Robert Gladden Orthopaedic Society; Active Fellow of the Scoliosis Research Society (SRS); American Orthopaedic Association (AOA) Emerging Leaders; Fellow of the American Academy of Orthopaedic Surgeons (AAOS); American Orthopaedic Association (AOA) Emerging Leaders Program; Active Member of the Pediatric Orthopaedic Society of North America (POSNA).
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Amornyotin S, Thailand; Meng FZ, China; Moshref L, Saudi Arabia S-Editor: Wang JJ L-Editor: A P-Editor: Ju JL
| 1. | Farrow L, Ablett AD, Mills L, Barker S. Early versus delayed surgery for paediatric supracondylar humeral fractures in the absence of vascular compromise: a systematic review and meta-analysis. Bone Joint J. 2018;100-B:1535-1541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Ramachandran M, Skaggs DL, Crawford HA, Eastwood DM, Lalonde FD, Vitale MG, Do TT, Kay RM. Delaying treatment of supracondylar fractures in children: has the pendulum swung too far? J Bone Joint Surg Br. 2008;90:1228-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Larson AN, Garg S, Weller A, Fletcher ND, Schiller JR, Kwon M, Browne R, Copley LA, Ho CA. Operative treatment of type II supracondylar humerus fractures: does time to surgery affect complications? J Pediatr Orthop. 2014;34:382-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Gerdes J, Kahol K, Smith M, Leyba MJ, Ferrara JJ. Jack Barney award: the effect of fatigue on cognitive and psychomotor skills of trauma residents and attending surgeons. Am J Surg. 2008;196:813-9; discussion 819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 78] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Ricci WM, Gallagher B, Brandt A, Schwappach J, Tucker M, Leighton R. Is after-hours orthopaedic surgery associated with adverse outcomes? A prospective comparative study. J Bone Joint Surg Am. 2009;91:2067-2072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 117] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Lins RE, Simovitch RW, Waters PM. Pediatric elbow trauma. Orthop Clin North Am. 1999;30:119-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 53] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Hunter JB. Femoral shaft fractures in children. Injury. 2005;36 Suppl 1:A86-A93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Olmsted MG, Powell R, Murphy J, Bell D, Stanley M, Sanchez RT. Methodology: U.S. News & World Report 2020-21 Best Hospitals: Specialty Rankings. [cited 15 December 2022]. Available from: https://health.usnews.com/media/best-hospitals/BH_Methodology_2020-21. |
| 9. | Yeranosian M, Horneff JG, Baldwin K, Hosalkar HS. Factors affecting the outcome of fractures of the femoral neck in children and adolescents: a systematic review. Bone Joint J. 2013;95-B:135-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 10. | El-Menyar A, Muneer M, Samson D, Al-Thani H, Alobaidi A, Mussleman P, Latifi R. Early versus late intramedullary nailing for traumatic femur fracture management: meta-analysis. J Orthop Surg Res. 2018;13:160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Suganuma S, Tada K, Yasutake H, Horii T, Takata M, Shimanuki K, Tsuji D, Takagawa S, Asano Y, Tsuchiya H. Timing of Surgery for Pediatric Supracondylar Humerus Fractures and Early Postoperative Results. J Hand Surg Asian Pac Vol. 2020;25:226-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Iyengar SR, Hoffinger SA, Townsend DR. Early versus delayed reduction and pinning of type III displaced supracondylar fractures of the humerus in children: a comparative study. J Orthop Trauma. 1999;13:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 98] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Cashman JP, Guerin SM, Hemsing M, McCormack D. Effect of deferred treatment of supracondylar humeral fractures. Surgeon. 2010;8:71-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Payvandi SA, Fugle MJ. Treatment of pediatric supracondylar humerus fractures in the community hospital. Tech Hand Up Extrem Surg. 2007;11:174-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Paci GM, Tileston KR, Vorhies JS, Bishop JA. Pediatric Supracondylar Humerus Fractures: Does After-Hours Treatment Influence Outcomes? J Orthop Trauma. 2018;32:e215-e220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Abdelmalek A, Towner M, Clarke A. Are we staying up too late? Timing of surgery of displaced supracondylar fractures in children. Clinical audit in a paediatric tertiary UK trauma centre and literature review. Arch Orthop Trauma Surg. 2022;142:3863-3867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Okkaoglu MC, Ozdemir FE, Ozdemir E, Karaduman M, Ates A, Altay M. Is there an optimal timing for surgical treatment of pediatric supracondylar humerus fractures in the first 24 hours? J Orthop Surg Res. 2021;16:484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Mahan ST, Miller PE, Park J, Sullivan N, Vuillermin C. Fully displaced pediatric supracondylar humerus fractures: Which ones need to go at night? J Child Orthop. 2022;16:355-365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 19. | Leviton LC, Melichar L. Balancing stakeholder needs in the evaluation of healthcare quality improvement. BMJ Qual Saf. 2016;25:803-807. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |