Published online Jul 18, 2023. doi: 10.5312/wjo.v14.i7.505
Peer-review started: January 31, 2023
First decision: March 28, 2023
Revised: April 11, 2023
Accepted: May 15, 2023
Article in press: May 15, 2023
Published online: July 18, 2023
Processing time: 167 Days and 21.1 Hours
Shoulder pain is a common musculoskeletal complaint, and rotator cuff (RC) pathologies are one of the main causes. The RC undergoes various tendinopathic and avascular changes during the aging process. Other degenerative changes affecting its healing potential make it an appealing target for biological agents. Platelet-rich plasma (PRP) has demonstrated the potential to deliver a high concentration of several growth factors and anti-inflammatory mediators, and its clinical use is mainly supported by experiments that demonstrated its positive effect on muscle, ligaments, and tendinous cells. This review aimed to specify the role of PRP and its future applications in RC tendinopathies based on the current clinical evidence. Due to the different characteristics and conflicting outcomes, clinicians should use PRP with moderate expectations until more consistent evidence is available. However, it is reasonable to consider PRP in patients with contraindications to corticosteroid injections or those with risk factors for inadequate healing. Its autologous origin makes it a safe treatment, and its characteristics make it a promising option for treating RC tendinopathy, but the efficacy has yet to be established.
Core Tip: Platelet-rich plasma may be a promising treatment option for rotator cuff tendinopathy, but more consistent evidence is needed to establish its effectiveness. Therefore, clinicians should approach its use with moderate expectations and consider it a potential treatment option for patients who cannot receive corticosteroid injections or have risk factors for poor healing.
- Citation: Velasquez Garcia A, Ingala Martini L, Franco Abache A, Abdo G. Role of platelet-rich plasma in the treatment of rotator cuff tendinopathy. World J Orthop 2023; 14(7): 505-515
- URL: https://www.wjgnet.com/2218-5836/full/v14/i7/505.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i7.505
Shoulder pain and disability are common musculoskeletal complaints caused mainly by rotator cuff (RC) lesions[1]. Aging can promote the development of many tendinopathic and avascular changes in RC, altering its intrinsic healing capacity and increasing failure rates after surgical or non-surgical treatment[2]. RC lesions include a wide range of pathological states, beginning with acute tendinitis and progressing to tendinosis, degeneration, partial-thickness, and full-thickness tears[2,3]. Full-thickness RC tears represent the end stage of RC pathology and have an incidence of approximately 20% in adults. The prevalence of these tears increases to over 50% after the age of 60 years[4-6].
To ensure accurate management and effective communication among clinicians, it is necessary to establish a clear definition for tendinitis and tendinosis[7,8]. Tendinitis is associated with inflammation, stress, degeneration, and poor mechanics and is generally caused by overuse[9]. Tendinosis encompasses tendon degeneration with or without histological signs of inflammation, including impaired and disorganized collagen, increased vascularity, and cellularity[9,10]. In general, tendinopathy is a term attributed to different tendons pathologies with various etiological factors, mainly caused by overuse, that can cause discomfort when the tissue does not regenerate[7,11].
New biological therapies aim to improve tendon healing as part of the ongoing development for the treatment of RC tendinopathy. These therapies include platelet-rich plasma (PRP) injections, growth factors, mesenchymal stem cells (MSCs), adipose-derived, and bone marrow aspirate concentrate. These have been proposed to speed up tendon recovery based on encouraging results from experimental models and clinical trials[12,13]. Therefore, a wide range of the states of RC tendinopathy may be effectively treated with nonoperative treatment, particularly in those where the structural integrity of the tendon has not been fully involved[14]. This review aimed to summarize the current evidence for the effectiveness of PRP as a non-surgical treatment method for RC tendinopathy.
Several theories have described possible pathophysiological routes for RC tendinopathy. Intrinsic and extrinsic mechanisms have traditionally been associated with the development of RC tendinopathy[2]. Widely studied, the intrinsic pathway describes degeneration due to hypoperfusion of the RC tendons, cell degeneration, and apoptosis, and some authors state that these create the main link in the establishment of tendinopathy[2]. Extrinsic factors are related to mechanical theories, in which microtears occur due to overuse or repetition[15]. Disorders associated with biomechanical causes, such as chronic impingement, superior humeral head translation, and overuse, have been associated with progressive degeneration of the RC tendons[2]. Since the underlying mechanism or tendon pathology cannot be determined in routine clinical practice, tendinopathy is a common term that involves many different clinical diagnoses[16].
RC tendinopathy, including partial-thickness tears, could cause limited shoulder motion, discomfort at rest, a painful arc of motion, and external rotation weakness. It is common to cause symptoms with painful overhead and positive special testing[16]. Furthermore, sleep disturbances may be characterized by discomfort in the mid-lateral region of the humerus or the anterolateral aspect of the acromion[7,8]. Indeed, partial tears are usually more painful than full-thickness[17].
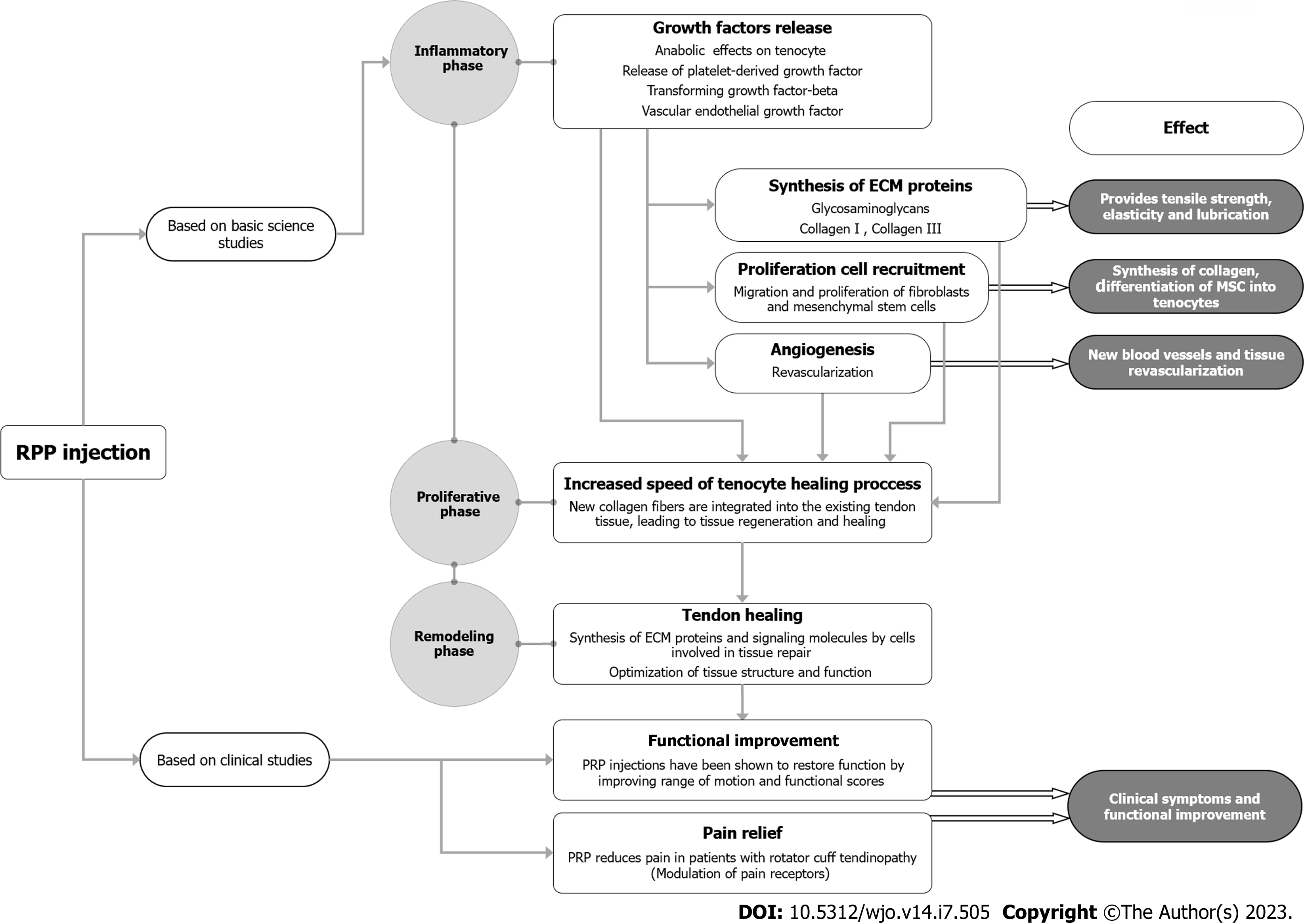
Regardless of the type of treatment applied, tendon healing occurs in three overlapping phases: Inflammatory, proliferative, and remodeling[18]. The inflammatory process produces cytokines near the injury site in the first 24 to 48 h, attracting neutrophils, macrophages, and red blood cells. The healing process continues with hematoma formation and cellular invasion into the surrounding areas of the tendon. Growth factors, such as platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and vascular endothelial growth factor, are released by platelets during this phase[19-21].
During the proliferative phase, MSCs migrate and differentiate, influenced by PDGFs[18]. The cells involved in tissue repair, such as fibroblasts and MSCs, proliferate and synthesize extracellular matrix (ECM) proteins[19-23]. Fibroblasts that migrate during this phase generate type III collagen and glycosaminoglycans, which enhances the tissue’s tensile strength, elasticity, and lubrication[24,25]. Tenocytes become the primary cell type responsible for producing and maintaining the ECM proteins that provide the necessary structure and mechanical properties to form new tissue[19].
Collagen cross-linking increases during the remodeling phase, and collagen type III is reabsorbed and replaced, resulting in an improved organization[25]. During this stage, tenocytes produce ECM proteins and other signaling molecules that amplify the upregulation of collagen type I gene expression and optimize the structure and function of the newly formed tissue[19,20,22,23]. However, complete tendon regeneration is not achieved, and the complex remodeling process usually leads to a steady decrease in tendon biomechanical strength[18,24]. Figure 1 illustrates the role of PRP in different stages of tendon healing.
Overall, clinical findings suggest that PRP injections for musculoskeletal pathologies, including supraspinatus tendinopathy, are safe[26], cost-effective, and easily administered outpatient procedures providing promising results compared to other treatment options[3]. The efficacy of various types of PRP is currently being evaluated in the shoulder and other joints[27]. Previous reports have shown inconsistent outcomes, with superior results in the PRP-treated group compared to the control groups, while others have shown similar or even inferior results[28-31]. The variability in the preparation techniques for PRP may explain the wide range of effectiveness among various studies[32]. Furthermore, factors such as the number of platelets available and the presence of anticoagulants and activators can significantly impact the growth factors present in the final PRP composition. As a result, it is difficult to compare research studies that differ substantially in design and methodology[33-35]. Furthermore, the intrinsic heterogeneity in the final composition of PRP and the various elements involved have been recognized as the main limitation of PRP injections for their wide recommendation in clinical practice[36-40].
Since these studies used different procedures to obtain the final PRP and varied the concentration of platelets and other components, the clinical results are inconsistent. This compositional variation can affect the advantages of a hypothetical healing effect[41]. Furthermore, factors such as concurrent physical therapy, exercise programs, and the impact of needle stimulation can contribute to some bias, which could also affect outcomes[42].
Natural growth factors, cytokines, and anti-inflammatory mediators are used in orthopedics to treat and recover tissues involved in diseases. As a result, a significant increase in the use of biological agents to treat common musculoskeletal injuries has been observed in recent years[43]. Different disorders have been treated with PRP, MSCs obtained from bone marrow aspirates, and adipose tissue[43]. PRP has gained recent popularity for treating shoulder disorders in clinical practice and as a viable method to enhance the surgical treatment of RC tears[44]. However, due to conflicting results, clinicians are still skeptical about the actual benefit and optimal use of these treatments in common shoulder diseases[43].
The clinical use of PRP is mainly supported by in vitro experiments that demonstrated its positive effect on muscle and tendinous cells[45]. Tenocytes exhibit enhanced proliferation and ECM production, improving tendon recovery. Additionally, when exposed to PRP, stem cells are stimulated to differentiate into tenocytes[45-48]. These characteristics show that PRP might enhance human tenocyte healing through cell proliferation and encourage ECM production[49]. Consequently, PRP could be a highly appealing therapy option for RC tendinopathy[49].
Authors in recent years have encompassed a wide range of preparations, presentations, and formulations under the term PRP. From a bioanalytical point of view, PRP consists of a fraction of whole blood with a supraphysiological concentration of platelets and other components[44]. The PRP therapy preparation process involves the separation of platelets from whole blood by centrifugation. In addition, platelet-activating chemicals can be added to enhance the effectiveness of the therapy. The growth factors released from the platelet alpha granules, approximately 7-10 d after PRP administration, coincide with the inflammation and healing phases of the tendon, promoting cellular differentiation and the healing process[32,50,51].
Growth factors, inflammatory mediators, and proteins that promote stromal and MSCs growth, including those derived from tendons, multiply once activated and hinder the repair process by creating fibrous scar tissue instead of healthy tissue[44]. Studies have shown that PRP injections can improve the structure of the ECM of tendons in the short term when injected directly into the tissue and administered through a matrix scaffold. This tendon healing and regeneration mechanism may be responsible for the clinical and structural improvements of the tendons after PRP therapy[28,33,44,52].
The comparative clinical efficacy of PRP, placebo (saline), autologous whole blood, and dry needling for ligament and tendon injury is unclear (Table 1). Lin et al[53] conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) to investigate the effectiveness of PRP therapy in patients with RC tendinopathy compared to sham injection, no injection, or physical therapy alone. The study found that PRP therapy produced significant long-term pain relief (> 24 wk) but did not show significant differences in functional results compared to the control groups. Notably, the study included trials using various numbers of injections, ultrasound-guided and non-guided injection techniques, and different injection approaches, but it found no specific approach to be more effective than others.
| Ref. | Level of evidence | Design | Groups (n) | Injections/dosis | Outcomes measure | Follow-up | Conclusions |
| Kesikburun et al[54], 2013 | I | Ultrasound-guided PRP injections vs saline injections | 40 patients PRP (20), placebo (20) | 1/5 mL | VAS, WORC, and SPADI | 3, 6, 12, 24 wk. 1 yr | PRP is not more effective in improving shoulder quality of life, pain, disability, and range of motion than placebo |
| Rha et al[57], 2013 | I | PRP injections vs dry needling | 39 patients. PRP (20), dry needling (20) | 1/3 mL | SPADI, passive ROM, global rating scale, ultrasound measurement | 24 wk | PRP leads to a progressive reduction in pain and disability compared to dry needling |
| Scarpone et al[59], 2013 | III | Ultrasound guided PRP injection at the lesion and surrounding tendon | 18 | 1/3.5 mL | MRI, VAS and three-item patient satisfaction scale | 8, 12, 52 wk | Improvement in MRI, pain and function with PRP |
| Lee et al[62], 2019 | III | PRP injection vs exercise treatment; leukocyte-poor vs leukocyte-rich PRP | 60. PRP (27), exercise (33) | 1/1.5 mL | ASES, CMS, and NRS | 12 wk, 24 wk | PRP is more effective than exercise therapy for the first 3 mo |
| Kim et al[55], 2019 | II | PRP injection vs exercise treatment | 30 patients. PRP (15), exercise (15) | 1/2 mL | ASES, CMS, and NRS | 12 wk, 24 wk | PRP had an advantage over exercise; improvement until 12 wk, slight decrease at 24 wk |
| Rossi et al[71], 2021 | II | Subacromial PRP injections | 50 patients | 1/5 mL | ASES, CMS, and VAS | 1 yr | PRP decreased pain, improved functional outcomes, and resolved sleep disturbances. Return to sports for most athletes |
| Oudelaar et al[77], 2021 | I | NACD + PRP vs NACD + CI | 88 patients. NACD + PRP (41), NACD + CI (47) | 1/5 mL | VAS, CMS, DASH, OSS, EQ-5D | 6 wk, 3 mo, 6 mo, 12 mo, 24 mo | NACD + PRP was worse at the 6-wk follow-up but better at the 6-mo follow-up. Comparable results at 12 and 24 mo |
Chen et al[26] conducted a systematic review and meta-analysis that evaluated the efficacy of PRP therapy in the healing of tendons and ligaments. The study analyzed 37 articles and included 1937 patients without restrictions on the tendons or ligaments studied. The authors found a wide variety of preparation methods used in the studies, and half of the studies did not use platelet activation or did not report the specific kit used. Despite this, the authors found no significant adverse events, highlighting the safety of PRP therapy. Overall, the PRP groups in the studies showed significantly less long-term pain than the control groups, particularly in lateral epicondylitis and RC injuries.
A randomized controlled study by Kesikburun et al[54] evaluated the effectiveness of PRP therapy in patients with RC tendinopathy who were treated with an exercise program. The study found that PRP was less effective than a placebo injection in several aspects, which can be attributed to leukocyte-rich PRP and shorter follow-up periods. However, another prospective open-label comparative trial compared a PRP group with an exercise group and found that PRP showed better American Shoulder and Elbow Surgeons Score (ASES) and Constant Murley Score (CMS) at 6 and 12 wk. However, at 24 wk, PRP was not superior to exercise. The PRP group had better rates of decreasing tendon thickness, but the concentration of leukocytes was not analyzed. Furthermore, the study found that higher levels of TGF-β1 and interleukin-1β growth factors were related to the clinical efficacy of PRP. This suggests that PRP provided more remarkable results than exercise alone, but exercise showed a cumulative positive effect in the long term, suggesting that more than a single injection may be necessary[55].
Wesner et al[56] reported results in a RCT that included 9 participants with RC tendinopathy receiving 4 mL of PRP injected into the supraspinatus or infraspinatus, and patients in the placebo group were injected with 4 mL of saline. All participants completed a 3-mo standardized home-based daily exercise program. The primary outcome measures were evaluated 3 and 6 mo after injection in RCT[56]. The study showed that patients who underwent PRP injections reported considerable improvements in pain and disability[56]. The authors concluded that intratendinous ultrasound-guided PRP injection could improve tendon pathology as documented by magnetic resonance imaging (MRI). This finding provides information for future studies examining PRP effectiveness[56]. However, the study’s limited sample size restricts the generalization of the results, and larger-scale studies are required to validate the findings.
A clinical trial compared the effectiveness of dry needling vs ultrasound-guided injection of PRP to treat RC ten
A recent systematic review and meta-analysis pooled the results of previous studies on the efficacy of PRP injections vs other treatments for patients with RC tendinopathy[58]. The study included 8 RCTs and found no significant differences between the PRP and control groups after three weeks of follow-up[58]. PRP was compared to saline injection in 4 trials, while rehabilitation programs and dry needling were control interventions in the other 4. PRP therapy’s medium- and long-term outcomes were superior, except for the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire. The most common adverse effect was mild and temporary pain[58].
In another long-term trial, 18 patients who had not responded to previous physical treatment but received a single 3.5 mL ultrasound-guided intralesional injection of PRP showed steady improvement on the Visual Analog Scale (VAS)[59]. At one year of follow-up, the median VAS dropped from 7.5 ± 0.3 before injection to 0.4 ± 0.2, and MRI alterations and functional outcomes similarly improved[59].
Subacromial corticosteroid injections (CI) or PRP have both seen an increase in comparative investigations in recent years[60-63] (Table 2). Some evidence supports that PRP could be a suitable substitute for patients who cannot use CIs, as suggested in a RCT of 40 patients with symptomatic partial-thickness RC tears, where PRP injections and CI were compared for pain control and patient-reported outcomes (PROs)[60]. Although both groups showed a significant improvement over the pre-injection condition at 12 wk, the PRP group showed a statistically significant improvement in pain and PROs at 24 wk. MRI at 6 mo of follow-up did not show significant differences between groups[60].
| Ref. | Level of evidence | Design | Groups (n) | Dosis/quantity | Outcomes measure | Follow-up | Conclusions |
| Barreto et al[66], 2019 | I | Subacromial PRP injections vs CI | 51 patients. PRP (26), CI (25) | 1/about 3 mL | DASH, UCLA- SRS, CMS | 3mo, 6 mo | No statistically significant differences |
| Dadgostar et al[63], 2021 | I | Ultrasound guided PRP injections vs CI | 58 patients. (30) PRP, (28) CI | 1/3 mL intra-articular, 3 mL intratendinoeus | VAS, ROM, WORC, DASH, US supraspinatus thickness | 3 mo | PRP with similar results to CI |
| Kwong et al[70], 2021 | I | Ultrasound-guided leokocyte-poor PRP injection vs CI | 99 patients. PRP (47), CI (52) | 1/(3-5) mL intratendineous (non-specific) and the rest at the subacromial space | VAS, ASES score, and WORC | 6, 12, 48 wk | The PRP group showed superior improvement in pain and function at short-term follow-up, without benefit at long-term follow-up |
| Ibrahim et al[68], 2019 | I | Ultrasound guided subacromial PRP vs CI | 30 patients. PRP (15), CI (15) | 1/2 mL | VAS, SDQ, ROM Clnical tests, US findings | 8 wk | Both groups showed significant improvement. PRP is safe and can be used for PRCT |
| Jo et al[78], 2020 | I | Ultrasound guided allogenic PRP vs CI | 60 patients. PRP (30), CI (30) | 1/4 mL | VAS, CMS, ASES, DASH, RC strength, ROM | 1, 4, 12, 24 wk | PRP reduced pain and improved overall function at 6 mo. DASH score, overall function, and external rotation were significantly better in the PRP group |
| Pasin et al[79], 2019 | I | PRP vs CI vs exercise | 60 patients. PRP (30), CI (30) | 1/4 mL | VAS, quick DASH, UCLA SRS, SF-36 | 3, 8 wk | PRP had better scores than CI and Physical Therapy even in a long time |
| Sabaah et al[80], 2020 | I | Prolotherapy vs CI and PRP | 40 patients. PRP (20), CI (20) | 2/5 mL | VAS, WORC-Index, ROM and US findings | 12 wk | Prolotherapy was superior. PRP improve tendon healing |
| Sari et al[81], 2020 | I | Ultrasound guided PRP vs CI, prolotherapy and lidocaine | 60 patients. PRP (30), CI (30) | 1/5 mL | VAS, ASES and WORC | 3, 12, 24 wk | CI were better at 3 wk. NO difference at 12 wk. PRP had better outcomes at 24 mo |
| Thepsoparn et al[82], 2021 | I | Ultrasound guided leukocyte-poor PRP vs CI | 31 patients. PRP (15), CI (16) | 1/5 mL | VAS and OSS | 4, 24 wk | No difference at 4 wk. PRP had better results at 24 wk for PRCT. No complications |
PRP has proven advantages, such as the possibility of repeat injections if symptoms worsen. It could even be administered 1 to 6 mo before surgery due to its safety, which contrasts with CI, and its recognized risk of perioperative complications[64,65]. However, the cost-effectiveness of PRP has not been established. Other reports have shown similar effectiveness between PRP and CI. In a randomized, double-blind trial, patients were evaluated using the DASH score, the University of California Los Angeles (UCLA) shoulder rating scale, and CMS at baseline and 1, 3, and 6 mo after treatment. Results showed no statistically significant differences (P < 0.05) between the PRP and CI groups in any outcome measures at any time. Both groups showed a significant improvement in DASH and UCLA scores (P < 0.05) compared to baseline, but the CMS score 6 mo after corticosteroid treatment was lower than baseline. These findings suggest that PRP is a safe treatment option for RC impingement syndrome and may be a valuable alternative, as it was found to be equally effective as corticosteroids[66]. Similar results were found in a prospective study with 60 patients with RC tendinosis or partial tendon tear. The authors used 2.5 mL of activated PRP or 40 mg methylprednisolone during the trial. The CMS improved from 41 to 53 points at 6 mo in the PRP group and from 38 to 66 points in the CI group[67].
In a study of 30 patients with RC tendinopathy, two groups of 15 were randomly chosen to receive a subacromial ultrasound-guided injection of PRP or corticosteroids. Pain in patients was evaluated using the VAS, shoulder function using the Shoulder Disability Questionnaire, and range of motion (ROM) before and 8 wk after injection. The study found that PRP and CI were similarly effective in the treatment of RC tendinopathy, showing significant improvements in pain, function, and ROM. These results suggest that PRP is a safe alternative to CI, decreasing inflammation and improving outcomes[68].
In another double-blind clinical trial, 58 patients with RC tendinitis were randomized to receive 3 mL of PRP or 1 mL of Depo-medrol 40 mg. The study found that both treatments resulted in similar significant improvements in pain, ROM, Western Ontario Rotator Cuff scores, DASH scores, and supraspinatus thickness during follow-ups[63]. A recent systematic review and meta-analysis of RCTs that included 639 patients revealed that at short-term follow-up, CI was more effective than PRP in the short term, but, in the mid-term, PRP was superior to CI in DASH and ASES scores. However, both treatments achieved minimal clinical important difference for each score, indicating no significant clinical differences between the two treatment modalities in managing RC disease[69].
A double-blind, randomized controlled study compared ultrasound-guided PRP injection with conventional CI in patients who had completed a detailed physical therapy protocol. Ninety-nine patients with MRI or ultrasound documented partial-thickness RC tears or tendinopathy were included. Patients treated with leukocyte-poor PRP ultrasound-guided injections showed superior improvement in pain and function at short-term follow-up. However, at 12 mo, there was no persistent effect of PRP over CI and no variations in the incidence of failure or conversion to surgery[70]. Ultrasound-guided injection of PRP potentially improves the precision and safety of the infiltration method, thus leading to improved effectiveness of the treatment[3,68]. However, the benefit has not been demonstrated extensively.
In contrast, a recent systematic review and meta-analysis of 12 RCTs have shown that while CI may have better short-term outcomes in treating RC tendinopathy, PRP therapy may have superior medium-term outcomes. These results suggest that while CI may provide faster pain relief, PRP therapy may be more effective in promoting long-term healing and tissue regeneration[69]. However, it should be noted that the studies included in the review had significant heterogeneity in their preparation of PRP (such as using the buffy-coat method vs the tube method and using one vs two centrifugation steps) and their treatment protocols after injection[69].
Similarly, a prospective cohort study included 50 patients with MRI-diagnosed tendinopathy, no tendon rupture, and 3 mo of failed conservative treatment. Two spin protocols were performed, and 5 mL of leukocyte-rich PRP was used to treat patients in combination with physical therapy. Results included pain relief, positive clinical results, and a return to sports at the pre-injury level at high rates[71].
Kieb et al[72] introduced an innovative method to standardize PRP growth factor concentrations using allogeneic lyophilized PRP powder. This technique involves creating a powder using twelve pooled platelet concentrations from various donors and comparing the growth factor concentration achieved using this technique to that found in whole blood. Theoretically, this approach allows the precise composition of the PRP to be chosen to provide a specific amount of growth factors based on the treated pathology. This advantage may provide a more controlled and efficient way to use the benefits of PRP therapy.
In a separate study, 17 patients with RC tendinopathy were treated with an injection of allogeneic PRP, while a control group received CI. Both groups experienced a significant reduction in pain and improved outcomes, with the CI group showing a faster recovery. No adverse effects were reported. The results of this trial suggest that allogeneic PRP may be a safe and potentially beneficial treatment option for RC tendinopathy, but further research is needed to confirm these findings and establish its long-term effectiveness[73].
High-quality evidence supports the use of PRP after RC repair[74]. However, the clinical evidence on the benefits of PRP in the nonoperative treatment of RC disorders is inconsistent. This makes it difficult to draw firm conclusions about PRP’s advantages in treating RC disorders. Although some in vitro studies have shown promising results for PRP, clinical studies have not consistently supported its therapeutic impact.
Additionally, the effectiveness of PRP can depend on the type and concentration of the specific components used. Therefore, more research is needed to fully understand PRP’s potential benefits and limitations in treating RC disorders. This situation highlights the need for a detailed investigation to define the optimal composition, efficient dose, and mechanism of action of PRP[73,75,76].
PRP therapy has been proposed as a treatment option for RC tendinopathy, but the available evidence is conflicting due to variability in settings, indications, and clinical outcomes. As a result, clinicians should approach PRP therapy with moderate and realistic expectations until more reliable evidence is available. While the basic science literature supports the potential of PRP to manage RC tendinopathy, there is not yet enough clinical data to support its effectiveness. However, PRP therapy is considered a safe treatment option because it uses a patient’s blood, decreasing the risk of allergic reactions or other complications associated with the use of foreign substances. Therefore, it is reasonable to consider PRP injections in patients with a contraindication to CI or patients with risk factors for inadequate healing as a promising treatment option for RC tendinopathy.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Chile
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Iossifidis A, United Kingdom; Rezus E, Romania S-Editor: Wang JJ L-Editor: A P-Editor: Cai YX
| 1. | Chard MD, Hazleman R, Hazleman BL, King RH, Reiss BB. Shoulder disorders in the elderly: a community survey. Arthritis Rheum. 1991;34:766-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 212] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 2. | Via AG, De Cupis M, Spoliti M, Oliva F. Clinical and biological aspects of rotator cuff tears. Muscles Ligaments Tendons J. 2013;3:70-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (2)] |
| 3. | Niazi GE, Hassan MS, Elfawy DM. Ultrasound-guided injection of platelet-rich plasma (PRP) in rotator cuff tendinopathy: effect on patients' symptoms and supraspinatus tendon thickness. Egypt J Radiol Nucl Med. 2020;51:111. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | DeFranco MJ, Bershadsky B, Ciccone J, Yum JK, Iannotti JP. Functional outcome of arthroscopic rotator cuff repairs: a correlation of anatomic and clinical results. J Shoulder Elbow Surg. 2007;16:759-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 119] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Minagawa H, Yamamoto N, Abe H, Fukuda M, Seki N, Kikuchi K, Kijima H, Itoi E. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J Orthop. 2013;10:8-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 378] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 6. | Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31:589-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 449] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 7. | Andres BM, Murrell GA. Treatment of tendinopathy: what works, what does not, and what is on the horizon. Clin Orthop Relat Res. 2008;466:1539-1554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 308] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 8. | Umer M, Qadir I, Azam M. Subacromial impingement syndrome. Orthop Rev (Pavia). 2012;4:e18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Factor D, Dale B. Current concepts of rotator cuff tendinopathy. Int J Sports Phys Ther. 2014;9:274-288. [PubMed] |
| 10. | Bhabra G, Wang A, Ebert JR, Edwards P, Zheng M, Zheng MH. Lateral Elbow Tendinopathy: Development of a Pathophysiology-Based Treatment Algorithm. Orthop J Sports Med. 2016;4:2325967116670635. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (1)] |
| 11. | Maffulli N, Wong J, Almekinders LC. Types and epidemiology of tendinopathy. Clin Sports Med. 2003;22:675-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 407] [Cited by in RCA: 395] [Article Influence: 18.0] [Reference Citation Analysis (1)] |
| 12. | Fealy S, Adler RS, Drakos MC, Kelly AM, Allen AA, Cordasco FA, Warren RF, O'Brien SJ. Patterns of vascular and anatomical response after rotator cuff repair. Am J Sports Med. 2006;34:120-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 13. | Randelli P, Cucchi D, Ragone V, de Girolamo L, Cabitza P, Randelli M. History of rotator cuff surgery. Knee Surg Sports Traumatol Arthrosc. 2015;23:344-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Randelli PS, Menon A, Nocerino E, Aliprandi A, Feroldi FM, Mazzoleni MG, Boveri S, Ambrogi F, Cucchi D. Long-term Results of Arthroscopic Rotator Cuff Repair: Initial Tear Size Matters: A Prospective Study on Clinical and Radiological Results at a Minimum Follow-up of 10 Years. Am J Sports Med. 2019;47:2659-2669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 15. | Seitz AL, McClure PW, Finucane S, Boardman ND 3rd, Michener LA. Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both? Clin Biomech (Bristol, Avon). 2011;26:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 287] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 16. | Shin KM. Partial-thickness rotator cuff tears. Korean J Pain. 2011;24:69-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Fukuda H. Partial-thickness rotator cuff tears: a modern view on Codman's classic. J Shoulder Elbow Surg. 2000;9:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 132] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 18. | Sharma P, Maffulli N. Biology of tendon injury: healing, modeling and remodeling. J Musculoskelet Neuronal Interact. 2006;6 (2):181-190. [PubMed] |
| 19. | Chalidis B, Givissis P, Papadopoulos P, Pitsilos C. Molecular and Biologic Effects of Platelet-Rich Plasma (PRP) in Ligament and Tendon Healing and Regeneration: A Systematic Review. Int J Mol Sci. 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 20. | Zhang J, Li F, Augi T, Williamson KM, Onishi K, Hogan MV, Neal MD, Wang JH. Platelet HMGB1 in Platelet-Rich Plasma (PRP) promotes tendon wound healing. PLoS One. 2021;16:e0251166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Greimers L, Drion PV, Colige A, Libertiaux V, Denoël V, Lecut C, Gothot A, Kaux JF. Effects of Allogeneic Platelet-Rich Plasma (PRP) on the Healing Process of Sectioned Achilles Tendons of Rats: A Methodological Description. J Vis Exp. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Chen L, Dong SW, Liu JP, Tao X, Tang KL, Xu JZ. Synergy of tendon stem cells and platelet-rich plasma in tendon healing. J Orthop Res. 2012;30:991-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Halpern BC, Chaudhury S, Rodeo SA. The role of platelet-rich plasma in inducing musculoskeletal tissue healing. HSS J. 2012;8:137-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Maffulli N, Moller HD, Evans CH. Tendon healing: can it be optimised? Br J Sports Med. 2002;36:315-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | Sharma P, Maffulli N. Biology of tendon injury: healing, modeling and remodeling. J Musculoskelet Neuronal Interact. 2006;6:181-190. [PubMed] |
| 26. | Chen X, Jones IA, Park C, Vangsness CT Jr. The Efficacy of Platelet-Rich Plasma on Tendon and Ligament Healing: A Systematic Review and Meta-analysis With Bias Assessment. Am J Sports Med. 2018;46:2020-2032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 178] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 27. | Martini LI, Via AG, Fossati C, Randelli F, Randelli P, Cucchi D. Single Platelet-Rich Plasma Injection for Early Stage of Osteoarthritis of the Knee. Joints. 2017;5:2-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 28. | Unlu MC, Kivrak A, Kayaalp ME, Birsel O, Akgun I. Peritendinous injection of platelet-rich plasma to treat tendinopathy: A retrospective review. Acta Orthop Traumatol Turc. 2017;51:482-487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 29. | Castricini R, Longo UG, De Benedetto M, Panfoli N, Pirani P, Zini R, Maffulli N, Denaro V. Platelet-rich plasma augmentation for arthroscopic rotator cuff repair: a randomized controlled trial. Am J Sports Med. 2011;39:258-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 333] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 30. | Tsikopoulos K, Tsikopoulos I, Simeonidis E, Papathanasiou E, Haidich AB, Anastasopoulos N, Natsis K. The clinical impact of platelet-rich plasma on tendinopathy compared to placebo or dry needling injections: A meta-analysis. Phys Ther Sport. 2016;17:87-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 31. | Fitzpatrick J, Bulsara M, Zheng MH. The Effectiveness of Platelet-Rich Plasma in the Treatment of Tendinopathy: A Meta-analysis of Randomized Controlled Clinical Trials. Am J Sports Med. 2017;45:226-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 214] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 32. | Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang CQ, Pinto NR, Bielecki T. Classification of platelet concentrates (Platelet-Rich Plasma-PRP, Platelet-Rich Fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J. 2014;4:3-9. [PubMed] |
| 33. | Randelli P, Arrigoni P, Ragone V, Aliprandi A, Cabitza P. Platelet rich plasma in arthroscopic rotator cuff repair: a prospective RCT study, 2-year follow-up. J Shoulder Elbow Surg. 2011;20:518-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 301] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 34. | Mei-Dan O, Carmont MR. The role of platelet-rich plasma in rotator cuff repair. Sports Med Arthrosc Rev. 2011;19:244-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Boswell SG, Cole BJ, Sundman EA, Karas V, Fortier LA. Platelet-rich plasma: a milieu of bioactive factors. Arthroscopy. 2012;28:429-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 384] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 36. | Mazzocca AD, McCarthy MB, Chowaniec DM, Cote MP, Romeo AA, Bradley JP, Arciero RA, Beitzel K. Platelet-rich plasma differs according to preparation method and human variability. J Bone Joint Surg Am. 2012;94:308-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 316] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 37. | Jo CH, Kim JE, Yoon KS, Shin S. Platelet-rich plasma stimulates cell proliferation and enhances matrix gene expression and synthesis in tenocytes from human rotator cuff tendons with degenerative tears. Am J Sports Med. 2012;40:1035-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 164] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 38. | Arora S, Doda V, Kotwal U, Dogra M. Quantification of platelets and platelet derived growth factors from platelet-rich-plasma (PRP) prepared at different centrifugal force (g) and time. Transfus Apher Sci. 2016;54:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 39. | Perez AG, Lana JF, Rodrigues AA, Luzo AC, Belangero WD, Santana MH. Relevant aspects of centrifugation step in the preparation of platelet-rich plasma. ISRN Hematol. 2014;2014:176060. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 40. | Xiong G, Lingampalli N, Koltsov JCB, Leung LL, Bhutani N, Robinson WH, Chu CR. Men and Women Differ in the Biochemical Composition of Platelet-Rich Plasma. Am J Sports Med. 2018;46:409-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 84] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 41. | Collins T, Alexander D, Barkatali B. Platelet-rich plasma: a narrative review. EFORT Open Rev. 2021;6:225-235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 103] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 42. | Ilhanli I, Guder N, Gul M. Platelet-Rich Plasma Treatment With Physical Therapy in Chronic Partial Supraspinatus Tears. Iran Red Crescent Med J. 2015;17:e23732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 43. | Carr JB 2nd, Rodeo SA. The role of biologic agents in the management of common shoulder pathologies: current state and future directions. J Shoulder Elbow Surg. 2019;28:2041-2052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 44. | Everts P, Onishi K, Jayaram P, Lana JF, Mautner K. Platelet-Rich Plasma: New Performance Understandings and Therapeutic Considerations in 2020. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 451] [Article Influence: 90.2] [Reference Citation Analysis (0)] |
| 45. | Anitua E, Andía I, Sanchez M, Azofra J, del Mar Zalduendo M, de la Fuente M, Nurden P, Nurden AT. Autologous preparations rich in growth factors promote proliferation and induce VEGF and HGF production by human tendon cells in culture. J Orthop Res. 2005;23:281-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 314] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 46. | Geaney LE, Arciero RA, DeBerardino TM, Mazzocca AD. The Effects of Platelet-Rich Plasma on Tendon and Ligament: Basic Science and Clinical Application. Oper Tech Sports Med. 2011;19:160-164. [RCA] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 47. | Zhang J, Wang JH. Platelet-rich plasma releasate promotes differentiation of tendon stem cells into active tenocytes. Am J Sports Med. 2010;38:2477-2486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 169] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 48. | Zhou Y, Wang JH. PRP Treatment Efficacy for Tendinopathy: A Review of Basic Science Studies. Biomed Res Int. 2016;2016:9103792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 143] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 49. | Hoppe S, Alini M, Benneker LM, Milz S, Boileau P, Zumstein MA. Tenocytes of chronic rotator cuff tendon tears can be stimulated by platelet-released growth factors. J Shoulder Elbow Surg. 2013;22:340-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 50. | Gulotta LV, Rodeo SA. Growth factors for rotator cuff repair. Clin Sports Med. 2009;28:13-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 125] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 51. | Randelli P, Randelli F, Ragone V, Menon A, D'Ambrosi R, Cucchi D, Cabitza P, Banfi G. Regenerative medicine in rotator cuff injuries. Biomed Res Int. 2014;2014:129515. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 52. | Randelli PS, Arrigoni P, Cabitza P, Volpi P, Maffulli N. Autologous platelet rich plasma for arthroscopic rotator cuff repair. A pilot study. Disabil Rehabil. 2008;30:1584-1589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 135] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 53. | Lin MT, Wei KC, Wu CH. Effectiveness of Platelet-Rich Plasma Injection in Rotator Cuff Tendinopathy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Diagnostics (Basel). 2020;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 115] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 54. | Kesikburun S, Tan AK, Yilmaz B, Yaşar E, Yazicioğlu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: a randomized controlled trial with 1-year follow-up. Am J Sports Med. 2013;41:2609-2616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 189] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 55. | Kim SJ, Yeo SM, Noh SJ, Ha CW, Lee BC, Lee HS, Kim SJ. Effect of platelet-rich plasma on the degenerative rotator cuff tendinopathy according to the compositions. J Orthop Surg Res. 2019;14:408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 56. | Wesner M, Defreitas T, Bredy H, Pothier L, Qin Z, McKillop AB, Gross DP. A Pilot Study Evaluating the Effectiveness of Platelet-Rich Plasma Therapy for Treating Degenerative Tendinopathies: A Randomized Control Trial with Synchronous Observational Cohort. PLoS One. 2016;11:e0147842. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 57. | Rha DW, Park GY, Kim YK, Kim MT, Lee SC. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: a randomized controlled trial. Clin Rehabil. 2013;27:113-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 186] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 58. | A Hamid MS, Sazlina SG. Platelet-rich plasma for rotator cuff tendinopathy: A systematic review and meta-analysis. PLoS One. 2021;16:e0251111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 59. | Scarpone M, Rabago D, Snell E, Demeo P, Ruppert K, Pritchard P, Arbogast G, Wilson JJ, Balzano JF. Effectiveness of Platelet-rich Plasma Injection for Rotator Cuff Tendinopathy: A Prospective Open-label Study. Glob Adv Health Med. 2013;2:26-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 60. | Shams A, El-Sayed M, Gamal O, Ewes W. Subacromial injection of autologous platelet-rich plasma versus corticosteroid for the treatment of symptomatic partial rotator cuff tears. Eur J Orthop Surg Traumatol. 2016;26:837-842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 107] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 61. | Annaniemi JA, Pere J, Giordano S. Platelet-rich plasma versus corticosteroid injections for rotator cuff tendinopathy: a comparative study with up to 18-month follow-up. Clin Shoulder Elb. 2022;25:28-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 62. | Lee HW, Choi KH, Kim JY, Yang I, Noh KC. Prospective Clinical Research of the Efficacy of Platelet-rich Plasma in the Outpatient-based Treatment of Rotator Cuff Tendinopathy. Clin Shoulder Elb. 2019;22:61-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 63. | Dadgostar H, Fahimipour F, Pahlevan Sabagh A, Arasteh P, Razi M. Corticosteroids or platelet-rich plasma injections for rotator cuff tendinopathy: a randomized clinical trial study. J Orthop Surg Res. 2021;16:333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 64. | Lobo-Escolar L, Ramazzini-Castro R, Codina-Grañó D, Lobo E, Minguell-Monyart J, Ardèvol J. Risk factors for symptomatic retears after arthroscopic repair of full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2021;30:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 65. | Puzzitiello RN, Patel BH, Nwachukwu BU, Allen AA, Forsythe B, Salzler MJ. Adverse Impact of Corticosteroid Injection on Rotator Cuff Tendon Health and Repair: A Systematic Review. Arthroscopy. 2020;36:1468-1475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 66. | Barreto RB, Azevedo AR, Gois MC, Freire MRM, Silva DS, Cardoso JC. Platelet-Rich Plasma and Corticosteroid in the Treatment of Rotator Cuff Impingement Syndrome: Randomized Clinical Trial. Rev Bras Ortop (Sao Paulo). 2019;54:636-643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 67. | Say F, Gurler D, Bulbul M. Platelet-rich plasma versus steroid injection for subacromial impingement syndrome. J Orthop Surg (Hong Kong). 2016;24:62-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 68. | Ibrahim DH, El-Gazzar NM, El-Saadany HM, El-Khouly RM. Ultrasound-guided injection of platelet rich plasma vs corticosteroid for treatment of rotator cuff tendinopathy: Effect on shoulder pain, disability, range of motion and ultrasonographic findings. Egypt Rheumatol. 2019;41:157-161. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 69. | Adra M, El Ghazal N, Nakanishi H, Smayra K, Hong SS, Miangul S, Matar RH, Than CA, Tennent D. Platelet-rich plasma versus corticosteroid injections in the management of patients with rotator cuff disease: A systematic review and meta-analysis. J Orthop Res. 2023;41:7-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 70. | Kwong CA, Woodmass JM, Gusnowski EM, Bois AJ, Leblanc J, More KD, Lo IKY. Platelet-Rich Plasma in Patients With Partial-Thickness Rotator Cuff Tears or Tendinopathy Leads to Significantly Improved Short-Term Pain Relief and Function Compared With Corticosteroid Injection: A Double-Blind Randomized Controlled Trial. Arthroscopy. 2021;37:510-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 71. | Rossi LA, Piuzzi N, Giunta D, Tanoira I, Brandariz R, Pasqualini I, Ranalletta M. Subacromial Platelet-Rich Plasma Injections Decrease Pain and Improve Functional Outcomes in Patients With Refractory Rotator Cuff Tendinopathy. Arthroscopy. 2021;37:2745-2753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 72. | Kieb M, Sander F, Prinz C, Adam S, Mau-Möller A, Bader R, Peters K, Tischer T. Platelet-Rich Plasma Powder: A New Preparation Method for the Standardization of Growth Factor Concentrations. Am J Sports Med. 2017;45:954-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 73. | Jo CH, Lee SY, Yoon KS, Oh S, Shin S. Allogenic Pure Platelet-Rich Plasma Therapy for Rotator Cuff Disease: A Bench and Bed Study. Am J Sports Med. 2018;46:3142-3154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 74. | Hurley ET, Lim Fat D, Moran CJ, Mullett H. The Efficacy of Platelet-Rich Plasma and Platelet-Rich Fibrin in Arthroscopic Rotator Cuff Repair: A Meta-analysis of Randomized Controlled Trials. Am J Sports Med. 2019;47:753-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 139] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 75. | Anitua E, Sánchez M, Orive G. The importance of understanding what is platelet-rich growth factor (PRGF) and what is not. J Shoulder Elbow Surg. 2011;20:e23-4; author reply e24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 76. | Chahla J, Cinque ME, Piuzzi NS, Mannava S, Geeslin AG, Murray IR, Dornan GJ, Muschler GF, LaPrade RF. A Call for Standardization in Platelet-Rich Plasma Preparation Protocols and Composition Reporting: A Systematic Review of the Clinical Orthopaedic Literature. J Bone Joint Surg Am. 2017;99:1769-1779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 379] [Article Influence: 47.4] [Reference Citation Analysis (0)] |
| 77. | Oudelaar BW, Huis In 't Veld R, Ooms EM, Schepers-Bok R, Nelissen RGHH, Vochteloo AJH. Efficacy of Adjuvant Application of Platelet-Rich Plasma After Needle Aspiration of Calcific Deposits for the Treatment of Rotator Cuff Calcific Tendinitis: A Double-Blinded, Randomized Controlled Trial With 2-Year Follow-up. Am J Sports Med. 2021;49:873-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 78. | Jo CH, Lee SY, Yoon KS, Oh S, Shin S. Allogeneic Platelet-Rich Plasma Versus Corticosteroid Injection for the Treatment of Rotator Cuff Disease: A Randomized Controlled Trial. J Bone Joint Surg Am. 2020;102:2129-2137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 79. | Pasin T, Ataoğlu S, Pasin Ö, Ankarali H. Comparison of the Effectiveness of Platelet-Rich Plasma, Corticosteroid, and Physical Therapy in Subacromial Impingement Syndrome. Arch Rheumatol. 2019;34:308-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 80. | Sabaah HMAE, Nassif MA. What is better for rotator cuff tendinopathy: dextrose prolotherapy, platelet-rich plasma, or corticosteroid injections? A randomized controlled study. Egypt Rheumatol Rehabil. 2020;47:40. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 81. | Sari A, Eroglu A. Comparison of ultrasound-guided platelet-rich plasma, prolotherapy, and corticosteroid injections in rotator cuff lesions. J Back Musculoskelet Rehabil. 2020;33:387-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 82. | Thepsoparn M, Thanphraisan P, Tanpowpong T, Itthipanichpong T. Comparison of a Platelet-Rich Plasma Injection and a Conventional Steroid Injection for Pain Relief and Functional Improvement of Partial Supraspinatus Tears. Orthop J Sports Med. 2021;9:23259671211024937. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |