Published online Jun 18, 2023. doi: 10.5312/wjo.v14.i6.471
Peer-review started: January 15, 2023
First decision: February 21, 2023
Revised: March 19, 2023
Accepted: May 6, 2023
Article in press: May 6, 2023
Published online: June 18, 2023
Processing time: 154 Days and 10 Hours
Evidence-based guidance on return to sport following toe phalanx fractures is limited.
To systemically review all studies recording return to sport following toe phalanx fractures (both acute fractures and stress fractures), and to collate information on return rates to sport (RRS) and mean return times (RTS) to the sport.
A systematic search of PubMed, MEDLINE, EMBASE, CINAHL, Cochrane Li
Thirteen studies were included: one retrospective cohort study and twelve case series. Seven studies reported on acute fractures. Six studies reported on stress fractures. For the acute fractures (n = 156), 63 were treated with primary conservative management (PCM), 6 with primary surgical management (PSM) (all displaced intra-articular (physeal) fractures of the great toe base of the proximal phalanx), 1 with secondary surgical management (SSM) and 87 did not specify treatment modality. For the stress fractures (n = 26), 23 were treated with PCM, 3 with PSM, and 6 with SSM. For acute fractures, RRS with PCM ranged from 0 to 100%, and RTS with PCM ranged from 1.2 to 24 wk. For acute fractures, RRS with PSM were all 100%, and RTS with PSM ranged from 12 to 24 wk. One case of an undisplaced intra-articular (physeal) fracture treated conservatively required conversion to SSM on refracture with a return to sport. For stress fractures, RRS with PCM ranged from 0% to 100%, and RTS with PCM ranged from 5 to 10 wk. For stress fractures, RRS with PSM were all 100%, and RTS with surgical management ranged from 10 to 16 wk. Six cases of conservatively-managed stress fractures required conversion to SSM. Two of these cases were associated with a prolonged delay to diagnosis (1 year, 2 years) and four cases with an underlying deformity [hallux valgus (n = 3), claw toe (n = 1)]. All six cases returned to the sport after SSM.
The majority of sport-related toe phalanx fractures (acute and stress) are managed conservatively with overall satisfactory RRS and RTS. For acute fractures, surgical management is indicated for displaced, intra-articular (physeal) fractures, which offers satisfactory RRS and RTS. For stress fractures, surgical management is indicated for cases with delayed diagnosis and established non-union at presentation, or with significant underlying deformity: both can expect satisfactory RRS and RTS.
Core Tip: We performed a systematic review, assessing studies that recorded return rates (RRS) and return times (RTS) to sports following acute and stress fractures of the toe phalanges. Thirteen studies were included. Seven studies reported on acute fractures (n = 156); six studies on stress fractures (n = 26). For acute fractures, 63 underwent primary conservative management (PCM), 6 primary surgical management (PSM), and 1 sary surgical management (SSM). For stress fractures, 23 underwent PCM, 3 PSM, and 6 SSM. For acute fractures, PCM conferred acceptable RRS and RTS. PSM was indicated for displaced intra-articular proximal phalanx fractures. For stress fractures, PCM, when successful, conferred acceptable RTS. Significant delays to diagnosis or associated deformity often necessitated the conversion to SSM: this was invariably successful at returning athletes to sport.
- Citation: Robertson GAJ, Sinha A, Hodkinson T, Koç T. Return to sport following toe phalanx fractures: A systematic review. World J Orthop 2023; 14(6): 471-484
- URL: https://www.wjgnet.com/2218-5836/full/v14/i6/471.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i6.471
Acute toe phalanx fractures are a relatively common injury, comprising 3%-4% of all traumatic fractures[1-4]. Most of these fractures occur within the first and fifth toes, with the majority being undisplaced or minimally displaced, and suitable for conservative management[5]. The functional results following these injuries have shown promising results[5].
While 16% of all acute toe fractures occur during sport, the incidence and outcome of these fractures in the athlete remain poorly defined[6]. Traumatic toe phalanx fractures have been found to comprise 4.5% of all sport-related fractures, and occur at an incidence of 0.06 per 1000 of the general population[6].
By comparison to acute fractures, the epidemiology of toe phalanx stress fractures is less well described[7]. While a significant proportion of these fractures are sport-related, the current literature on this injury type comprises a limited number of case series and case reports[7]. While there are emerging theories that link biomechanical deformities to their occurrence (e.g. hallux valgus and great toe proximal phalanx stress fractures), a comprehensive description of this fracture type has yet to be presented[8].
The most common causative sports for acute toe phalanx fractures are soccer, gymnastics, and judo[9]. The most common causative sports for stress-toe phalanx fractures are sprinting, soccer and long-distance running[7]. For acute toe phalanx fractures, the common sporting mechanisms of injury include tackle and dismount[9].
Regarding treatment, with the vast majority of acute toe phalanx fractures being undisplaced or minimally displaced and extra-articular, they are managed conservatively, with toe strapping and protected weight-bearing[5,9]. Those that are significantly displaced or intra-articular, are often managed with closed +/- open reduction with k-wire or screw fixation[9]. Open fractures require fracture site washout +/- fixation[9]. Stress fractures of the toe phalanx are routinely managed conservatively in the first instance, with protected weight-bearing and avoidance of relevant sporting activities[7]. However, those with significantly delayed presentation (> 1 year) and established non-union, or those that are associated with a significant causative deformity, often require surgical intervention[7].
Despite this treatment framework, there is very limited information in the current literature to guide the optimal management of these fractures in the athlete[7,9-11]. Similarly, there is very limited published data, which illustrates the expected morbidity that such fractures will have on the athlete[7,9-11].
This systematic review aims to provide a comprehensive overview of the current literature which records return to sport following acute fractures and stress fractures of the toe phalanges in the athlete.
The authors performed a systematic analysis of the listed databases in December 2022: PubMed, MEDLINE, EMBASE, CINAHL, Cochrane Library, Physiotherapy Evidence Database (PEDro), and Google Scholar.
The search aimed to identify all peer-reviewed studies, which recorded return rates to sport (RRS) and return times to sport (RTS) in patients who sustained toe phalanx fractures. The search terms used were ‘toe’, ‘phalanx’, ‘fracture’, ‘injury’, ‘athletes’, ‘sports’, ‘non-operative’, ‘conservative’, ‘operative’, ‘surgical’, and ‘return to sport’. All articles were considered, regardless of the date of publication or level of the sport.
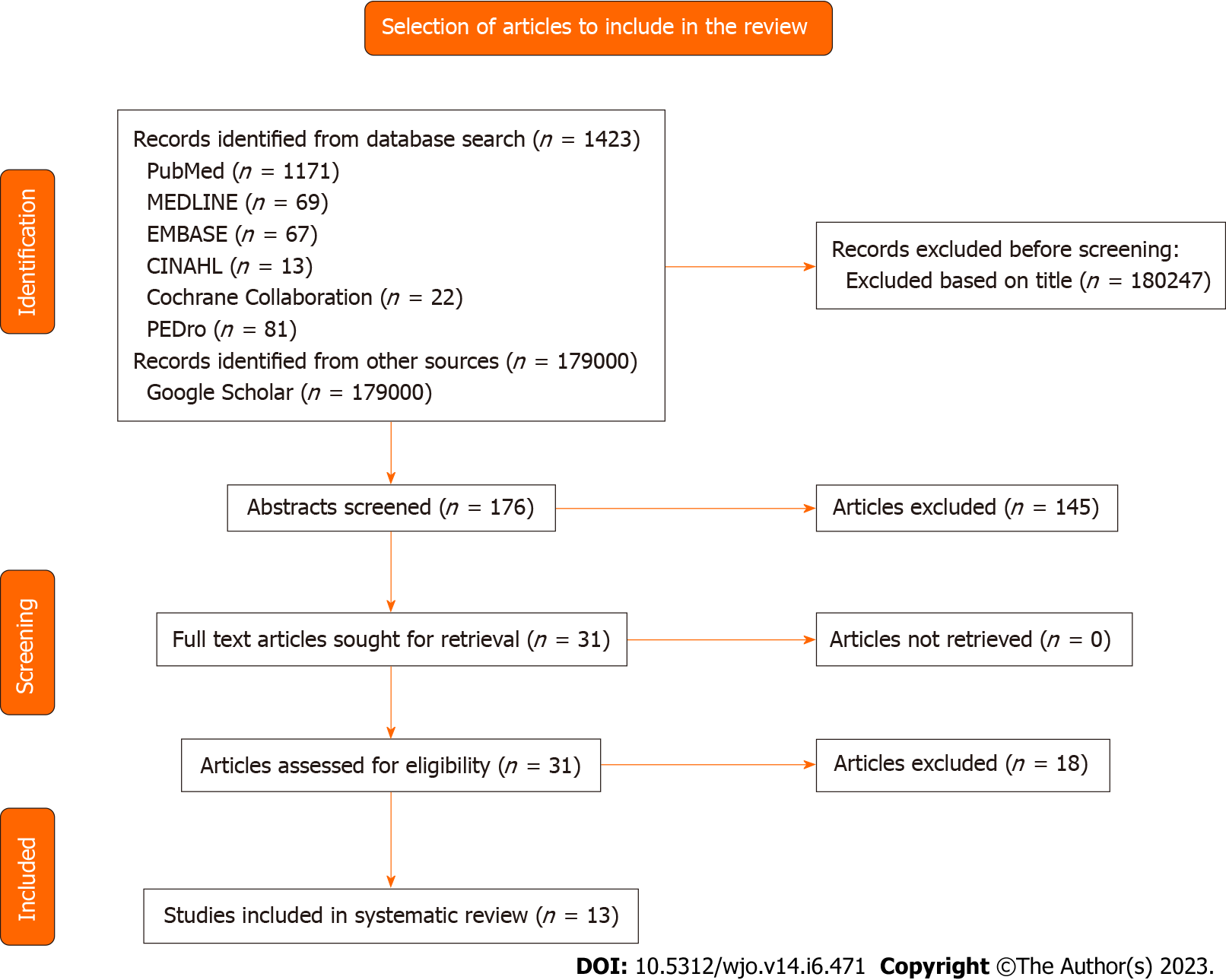
The review was structured along the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines[12]. Two authors (X.X.X., X.X.X.) searched for and reviewed the articles. Table 1 records the inclusion and exclusion criteria. The QUOROM Process for the review is illustrated in Figure 1.
| Inclusion criteria | Exclusion criteria |
| Acute toe phalanx fractures | Toe sesamoid fractures |
| Stress toe phalanx fractures | Toe joint dislocation without fracture |
| Elite or recreational athletes | Toe joint fracture dislocation |
| Return rate to sporting activity reported | Toe ligament injuries |
| Time to return to sporting activity reported | No sporting outcome data reported |
| Two or more injuries reported | Concomitant upper or lower limb fractures |
| Peer-reviewed journals | Reviews, case reports, abstracts, or anecdotal articles |
| English language | Animal, cadaver, or in vitro studies |
The authors excluded technical notes, case reports, instructional course reports, biomechanical reports, articles of expert opinion, and literature reviews, unless these manuscripts contained relevant patient data. Similarly, articles reporting on return to sport following toe sesamoid fractures were excluded. A stepwise process of article assessment was performed, first reviewing all the relevant titles, then abstracts, then full-length articles as required. Relevant reference lists and review studies were also assessed to locate further studies, which were appropriate for inclusion. Any disagreement in article inclusion was confirmed through consensus agreement or liaison with the senior author.
The recorded data from each study included: Demographic details, mechanism of injury (for acute fractures), duration of preceding symptoms (for stress fractures), pre-operative imaging investigations, fracture location, fracture nature (acute vs stress) and fracture severity, conservative and surgical treatment methods, RRS, RTS, return rates to pre-injury level of sport, complications, outcome scores recorded, and relevant predictive factors.
Acute fractures and stress fractures were grouped separately. For the acute fracture studies, some papers recorded the fractures with no differentiation regarding fracture type or location: These studies were grouped as ‘general cohort’ studies. Other studies specifically described the management of intra-articular (physeal) fractures of the base of the great toe proximal phalanx: These were grouped as ‘Intra-Articular (Physeal) Base of Proximal Phalanx Fractures’.
The primary outcome data was RRS and RTS. The secondary outcome data included ‘return to pre-injury level of sport’ rates and relevant complications.
RRS was defined as the percentage of athletes who successfully returned to sport with the designated treatment modality. Where conversion to a further treatment was required, with RRS not possible from the initial treatment method, this was recorded as a non-return to sport for the method in question. For conservative treatment, RTS was defined as the time from the commencement of conservative treatment to return to sport. For surgical treatment, RTS was defined as the time from the commencement of the relevant surgical treatment to return to sport[13].
If surgical management was chosen as the first-line treatment, this was referred to as ‘primary surgical management’ (PSM). If surgical management was chosen following failed conservative management, this was referred to as ‘secondary surgical management’ (SSM). Return times to sport for ‘secondary surgical management’ were recorded from the relevant surgical procedure.
Study quality was quantified by the modified Coleman Methodology Score (CMS), as described by Coleman et al[14]. Study quality was also assessed by the Methodological Index for Non-Randomized Studies (MINORS) Score. Two of the authors calculated the modified CMS and the MINORS Score for each study (X.X.X, X.X.X). Inter-observer reliability of the modified CMS and MINORS scoring processes were quantified using the intra-class correlation co-efficient statistic. For the modified CMS, this was 0.98 (95%CI: 0.96-1.00). For the MINORS scores, this was 0.92 (95%CI: 0.89-0.94).
There was insufficient data to perform data synthesis or meta-analysis comparisons within the data. Thus, the available data was presented as a systematic review, without the use of analytic statistics. The intra-class correlation co-efficient statistic was used to assess the inter-observer reliability of the Modified Coleman Scores and the Methodological Index for Non-Randomized Studies Scores using IBM SPSS Statistics, Version 27.0 (Armonk, NY, United States).
The details of the review process for the included articles are provided in Figure 1. In total, 176 abstracts and 31 articles were reviewed.
The mean CMS for all the studies was 49.6 (range 34-67)[8,15-26] (Tables 2 and 3). For the studies reporting on acute fractures, the mean CMS was 53.1 (range 39-67)[15-21] (Table 2). For the studies reporting on stress fractures, the mean CMS was 45.5 (range 34-55)[8,22-26] (Table 3).
| Ref. | n | Study type | Mean age (yr) | Male:Female | Follow-up, % | Sport | Level of sport | Most common MOI | Location | Modified coleman score | MINORS score |
| General cohort | |||||||||||
| Robertson et al[15], 2012 | 8 | Case series | 21.1 | 8:0 | 6 (75) | Soccer | General population | Tackle (50%) | Great toe (n = 6) 2nd Toe (n = 1); 3rd Toe (n = 1) | 44 | 12 |
| Larsson et al[16], 2016 | 18 | Case series | N/A | 18:0 | 18 (100) | Soccer | Elite/Professional | N/A | N/A | 39 | 12 |
| Chan et al[17], 2021 | 53 | Case series | N/A | 32:21 | 53 (100) | US Collegiate Sports | Collegiate | N/A | N/A | 54 | 12 |
| Diaz et al[18], 2022 | 69 | RCS | N/A | 69:0 | 69 (100) | Soccer | Elite | N/A | N/A | 41 | 18 |
| Intra-Articular (Physeal) base of proximal phalanx fractures | |||||||||||
| Maffulli[19], 2001 | 2 | Case series | 12.5 | 2:0 | 2 (100) | Soccer (n = 1), Judo (n = 1) | Recreational | Tackle | Great toe proximal phalanx | 65 | 9 |
| Perugia et al[20], 2014 | 4 | Case series | 13-15 | N/A | 4 (100) | Gymnastics | Adolescent high level | Dismount | Great toe proximal phalanx | 67 | 11 |
| Bariteau et al[21], 2015 | 2 | Case series | 12.5 | 0:2 | 2 (100) | Gymnastics | Elite | Dismount | Great toe proximal phalanx | 62 | 11 |
| Ref. | n | Study type | Mean age (yr) | Male:Female | Follow-up, % | Sport | Level of sport | Location | Associated deformity | Modified coleman score | MINORS score |
| Yokoe et al[22], 1986 | 3 | Case series | 16.3 (12-21) | 1:2 | 3 (100) | Sprinting (n = 1), Rugby (n = 1), Kendo (n = 1) | Amateur | Great Toe Proximal Phalanx | Hallux valgus (n = 3) | 34 | 8 |
| Shiraishi et al[23], 1993 | 3 | Case series | 13.7 (12-17) | 1:2 | 3 (100) | Volleyball (n = 1), Long Distance Running (n = 1), Soccer (n = 1) | Amateur | Great toe proximal phalanx | 51 | 9 | |
| Yokoe et al[8], 2004 | 10 | Case series | 16.3 (12-21) | 2:8 | 10 (100) | Sprinting (n = 6), Distance Running (n = 1), Basketball (n = 1), Rugby (n = 1), Kendo (n = 1) | N/A | Great toe proximal phalanx | Hallux valgus (n = 9) | 35 | 8 |
| Pitsis et al[24], 2004 | 2 | Case series | 29 (17-41) | 0:2 | 2 (100) | Triathlon (n = 1), Gymnastics (n = 1) | Non-professional/Elite | Great toe proximal phalanx | Hallux valgus (n = 1) | 46 | 8 |
| Munemoto et al[25], 2009 | 4 | Case series | 14.5 (13-17) | 2:2 | 4 (100) | Short track running (n = 3), Soccer (n = 1) | Amateur | Great toe proximal phalanx | Hallux valgus (n = 3) | 55 | 8 |
| Yamaguchi et al[26], 2017 | 4 | Case series | 14.8 (13-16) | 4:0 | 4 (100) | Soccer (n = 3), Baseball (n = 1) | N/A | 2nd toe proximal phalanx | Claw toe (n = 1) | 52 | 8 |
The mean MINORS score for all the studies was 10.3 (range 8-18)[8,15-26] (Tables 2 and 3). For the studies reporting on acute fractures, the mean MINORS score was 12.1 (range 9-18)[15-21] (Table 2). For the studies reporting on stress fractures, the mean MINORS score was 8.2 (range 8-9)[8,22-26] (Table 3).
13 relevant studies[8,15-26] were identified, (year of publication from 1986[22] to 2022[18]), which recorded return to sports data for patients who sustained toe phalanx fractures (Table 2). One of these studies was a retrospective cohort study[18], and 12 were case series[8,15-17,19-26].
There were 156 acute toe phalanx fractures and 26 stress fractures. Eight of the acute fractures were specifically described as intra-articular (physeal) (all great toe bases of the proximal phalanx). Of the acute fractures, 14 occurred in the great toe, 1 in the second toe, and 1 in the third toe, and the location was not specified for 140. Of the stress fractures, 22 occurred in the proximal phalanx of the great toe and 4 in the proximal phalanx of the second toe. Of the 26 stress fracture patients, 16 (of the 22 great toe proximal phalanx stress fracture patients) had associated ‘hallux valgus’ deformity, and 1 (of the 4-second toe proximal phalanx stress fracture patients) had associated ‘claw toe’ deformity (Table 3). Regarding the etiology of the deformities, only one case noted the deformity to have developed secondary to the stress fracture[26].
Of the 156 acute fractures, 129 (83%) occurred in male patients, 23 (15%) in female patients, and 4 (3%) failed to specify gender. None of the studies reported bilateral fractures. Follow-up data were available for 154 (99%) of the 156 acute fractures. The mean age at the time of injury ranged from 12.5 years[19,21] to 21.1 years[15], and the causative sports included soccer, gymnastics and judo (Table 2).
Of the 26 stress fractures, 10 (38%) occurred in male patients, and 16 (62%) in female patients. None of the studies reported bilateral fractures. Follow-up data were available for all 26 (100%) of the stress fractures. The mean age at the time of injury ranged from 13.7 years[23] to 29.0 years[24], and the causative sports included sprinting, soccer, long-distance running, rugby, Japanese Fencing/Kendo, triathlon, gymnastics, baseball and volleyball (Table 3). The recorded duration of symptoms before diagnosis ranged from 1 wk to 2 years[24,26].
Seven of the studies reported on acute toe phalanx fractures exclusively[15-21]. Three of these studies reported on acute intra-articular (physeal) fractures of the base of the great toe proximal phalanx specifically[19-21]. Six of the studies reported on stress-toe phalanx fractures exclusively[8,22-26].
Of the acute fracture studies, one ‘general cohort’ study used the AO classification to describe the fracture types[15]. All of the acute ‘intra-articular (physeal) fracture’ studies used the Salter-Harris Fracture Classification to describe the fracture types[19-21]. None of the stress fracture studies used classification systems to describe the fracture patterns[8,22-26].
Of the 156 acute fractures, 69 (44%) specified treatment modality. Of these, 63 (91%) were treated with ‘primary conservative management’, and 6 (9%) with ‘primary surgical management’. One fracture was converted to ‘secondary surgical management’ after failed conservative treatment (Table 4). Of the 8 intra-articular (physeal) acute fractures, all (100%) specified treatment modalities: 6 (75%) underwent ‘primary surgical management’ and 2 (25%) underwent ‘primary conservative management’. One intra-articular fracture was converted to ‘secondary surgical management’ after failed conservative treatment. This was following a re-fracture on return to sport (Table 4).
| Ref. | n | Treatment (%) | Return to sport (%) | Return to the same level of sport (%) | Return time to sport | Secondary surgery - return rate (RR)/Return time (RT) | Persisting symptoms (%) | Complications |
| General cohort | ||||||||
| Robertson et al[15], 2012 | 6 | PCM (100) | 3 (50) | 3 (50) | 7.0 wk (mean) | 3 (50) | Nil | |
| Larsson et al[16], 2016 | 18 | N/A | N/A | N/A | 26 d (mean) | N/A | 1 re-fracture | |
| Chan et al[17], 2021 | 53 | PCM (100) | 53 (100) | N/A | 8.5 d (median) | N/A | 1 re-fracture | |
| Diaz et al[18], 2022 | 69 | N/A | N/A | 30 d (median) | N/A | Nil | ||
| Intra-articular (Physeal) base of proximal phalanx fractures | ||||||||
| Maffulli[19], 2001 | 2 | PCM (50) PSM (50) | 2 (100) | 2 (100) | By 6 mo | 0 (0) | 0 (0) | |
| Perugia et al[20], 2014 | 4 | PSM (100) | 4 (100) | 4 (100) | By 3 mo | 0 (0) | 0 (0) | |
| Bariteau et al[21], 2015 | 2 | PCM (50) PSM (50) | 1 (50) (PSM) | 1 (50) (PSM) | 5 mo | 1 – RR 100%/RT 14 wk | 0 (0) | 1 re-fracture (PCM) |
Of the 26 stress fractures, all (100%) specified treatment modality: 23 (88%) were treated with ‘primary conservative management’, and 3 (12%) were treated with ‘primary surgical management’ (Table 5). Six stress fractures were converted to ‘secondary surgical management’ after failed conservative treatment (Table 5). Of these six, two were associated with a delayed diagnosis (1 year and 2 years respectively), and 4 were associated with an underlying deformity [hallux valgus (n = 3), claw toe (n = 1)] (Table 5).
| Ref. | n | Treatment (%) | Return to sport (%) | Return to the same level of sport (%) | Time to return to sport (mean) | Secondary surgery - return rate (RR)/Return time (RT) | Factors associated with secondary surgery | Persisting symptom (%) | Complications (%) |
| Yokoe et al[22], 1986 | 3 | PCM (67) PSM (33) | 3 (100) | N/A | PCM - 3 mo; PSM - N/A | 0 (0) | 0 (0) | ||
| Shiraishi et al[23], 1993 | 3 | PCM (100) | 3 (100) | 3 (100) | 6 wk | 1 (33) | 1 non-union for a patient who did not stop training (33) | ||
| Yokoe et al[8], 2004 | 10 | PCM (100) | 6 (60) | 6 (60) | N/A | 4 (40) – RR 100% | Hallux valgus deformity (n = 3) | 0 (0) | 3 delayed unions with PCM (50) |
| Pitsis et al[24], 2004 | 2 | PCM (100) | 0 (0)a | 0 (0)a | N/A | 1 (50) – RR 100% | 2-yr delay to diagnosis | 0 (0) | 1 non-union with PCM (50) |
| Munemoto et al[25], 2009 | 4 | PCM (50) PSM (50) | 4 (100) | 4 (100) | PCM - 8.5 wk, PSM - 10 wk | 0 (0) | 1 mild deformity with PCM (50) | ||
| Yamaguchi et al[26], 2017 | 4 | PCM (100) | 3 (75) | 3 (75) | 5 wk | 1 (25) – RR 100%/RT 4 mo | 1-yr delay to diagnosis/Claw toe deformity | 0 (0) | 1 non-union and claw toe deformity with PCM (25) |
Plain radiography was the diagnostic imaging modality used in acute fracture studies[15-21]. All the stress fracture studies used plain radiography as first-line diagnostic imaging[8,22-26]. In addition to this, one stress fracture study used magnetic resonance imaging/computed tomography Scan to aid diagnosis[26], and another study used Tc-99 Bone scanning as second-line imaging[22].
Acute fractures: Conservative management: There were 63 acute fractures treated with ‘primary conservative management’ (Table 4).
Only two of the ‘general cohort’ studies specified the type of management[15,17]. Both studies used conservative management for the fractures[15,17]. The type of conservative management was not described[15,17].
All the ‘intra-articular (physeal) fracture’ studies described the type of management selected[19-21]. Of the two which employed conservative management, the techniques included: heel weight-bearing in a forefoot offloading shoe for 6 wk, referral to physiotherapy at 6 wk, the commencement of training at 12 wk[19]; and 6 wk of non-weight bearing with immobilization, with a return to sport at 3 mo[21].
Surgical management: There were six acute ‘intra-articular (physeal) fractures’ treated with primary surgical management[19-21]. The described techniques included: open reduction with K-wire fixation (n = 4), open reduction with screw fixation and cancellous bone graft (n = 1), and open reduction with no fixation (n = 1)[19-21]. One fracture was managed with secondary surgical management, using open reduction and screw fixation[21].
The post-operative regimes included heel weight-bearing in a forefoot offloading shoe for 6 wk, with the removal of K-wire and referral to physiotherapy at 6 wk, and commencement of training at 12 wk[19]; non-weight bearing with cast immobilization for 4 wk, with subsequent removal of K-wire at 4 wk and commencement of weight-bearing[20]; non-weight bearing in a moon boot orthotic for 6 wk, with progressive weight-bearing for the next 4 wk in the orthotic, then gradual weaning from the orthotic, with the commencement of impact activities at 10 wk post-op[21].
Conservative management: There were 23 stress fractures treated with ‘primary conservative management’ (Table 5). All studies described the management techniques used[8,22-26].
The management techniques fell into three categories: cessation of sporting activities, with no formal immobilization or other restrictions, for 4 to 8 wk[22,23,25,26]; immobilization of the foot in a cast for 5 wk[25]; non-weight bearing on the affected side with crutches for 3 to 6 wk[24].
All regimes were then followed with a graduated return to sporting activities[8,22-26], which could be supplemented by shoes with shock-absorbing insoles[23], foot orthoses with medial arch support, and a metatarsal pad[26] or a 2nd to 5th metatarsal bar orthosis[24].
Surgical management: There were 3 stress fractures treated with ‘primary surgical management’ (Table 5). The reported techniques were: Open reduction with drilling, screw and K-wire fixation (n = 1), open reduction with drilling and screw fixation (n = 1), and osteotomy for hallux valgus correction (n = 1)[22,25]. There were 6 stress fractures treated with ‘secondary surgical management’ (Table 5). The reported techniques were: Open reduction internal fixation (n = 3), osteotomy for hallux valgus correction (n = 1), open reduction with scar tissue debridement, screw and K-wire fixation (n = 1), surgical excision of the non-union, open reduction with cancellous bone graft and screw fixation (n = 1)[8,24,26].
The post-operative regimes included: immediate weight-bearing, with the commencement of activities 8 wk post-operatively[25] (– ‘primary surgical management’); non-weight bearing for 4 wk, with the removal of K-wire and commencement of heel weight-bearing at 4 wk, and commencement of mobilization exercises at 6 wk[26] (– ‘secondary surgical management’); non-weight bearing for 6 wk, then partial weight bearing in a walker boot for 6 wk, then a graduated return to training[24] (– ‘secondary surgical management’).
Two of the acute fracture studies used formal scores to record post-treatment outcomes[20,21]. These included: a ‘Visual Analog Pain’ scale, the ‘American Orthopaedic Foot and Ankle Society (AOFAS) Hallux Metatarsal Phalangeal’ scale, the ‘Short Form-36 (SF-36) Physical Component Summary (PCS)’ and the ‘Short Form-36 (SF-36) Mental Component Summary (MCS)’[20,21].
None of the stress fracture studies used formal scores to record post-treatment outcomes[8,22-26].
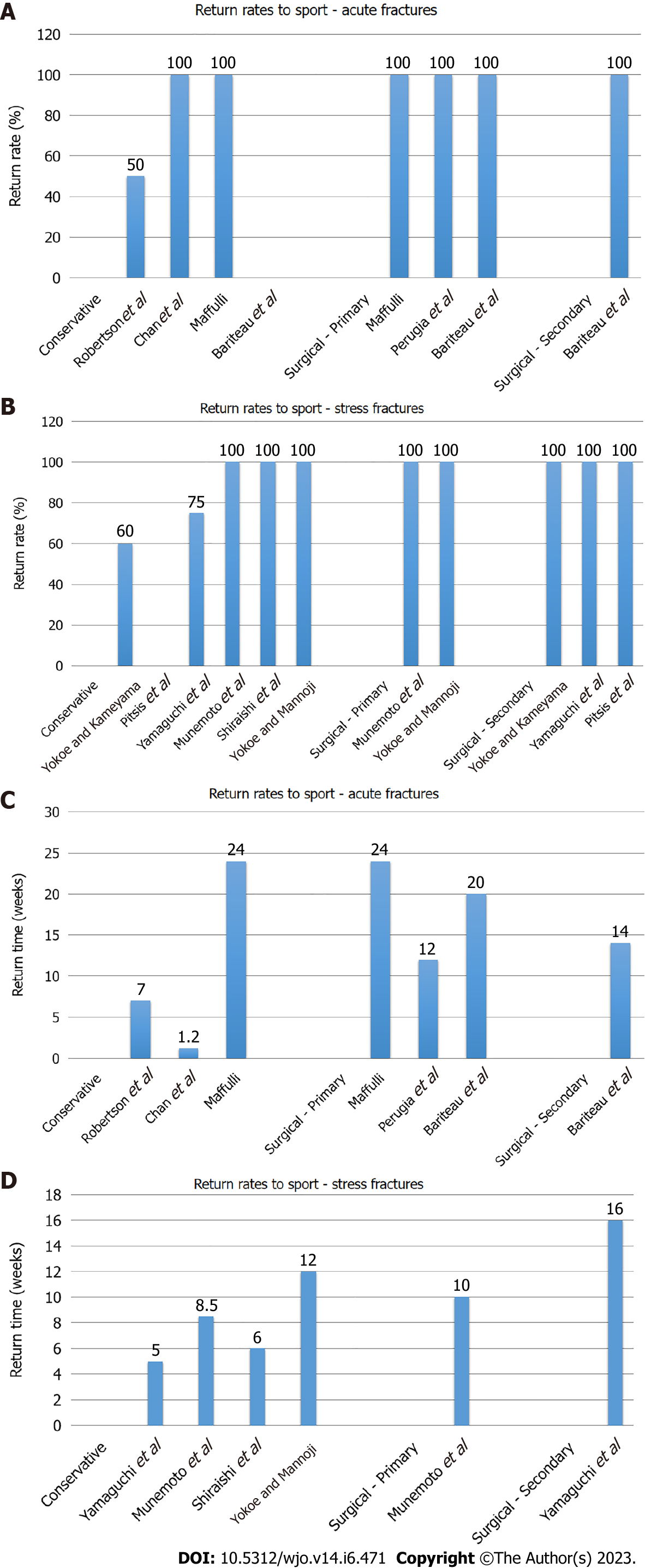
Acute fractures: Conservative management: Four studies recorded RRS following conservative management of acute fractures[15,17,19,21]. The RRS ranged from 0 to 100%[15,17,19,21] (Table 4 and Figure 2A).
The return rates to pre-injury level sports for the conservatively-managed acute fractures ranged from 0% to 100%[15,19,21] (Table 4).
Surgical management: Three studies recorded RRS following PSM of acute fractures[19-21], and one study recorded RRS following SSM of acute fractures[21]. The recorded RRS were 100% for PSM[19-21], and 100%% for SSM[21] (Table 4 and Figure 2A).
The return rates to pre-injury level sports for the surgically-managed acute fractures were all 100%[19-21] (Table 4).
Conservative management: Six studies recorded RRS following conservative management of stress fractures[8,22-26]. The RRS ranged from 0 to 100%[8,22-26] (Table 5 and Figure 2B).
The return rates to pre-injury level sports for the conservatively-managed stress fractures ranged from 0% to 100%[8,23-26] (Table 5).
Surgical management: Two studies recorded RRS following PSM of stress fractures[22,25], and three studies recorded RRS following SSM of stress fractures[8,24,26]. The recorded RRS was 100% for PSM[22,25], and 100% for SSM[8,24,26] (Table 5 and Figure 2B).
The return rates to pre-injury level sports for the surgically-managed stress fractures were 100%[25] (Table 5).
Acute fractures: Conservative management: Three studies recorded RTS following conservative management of acute fractures[15,17,19]. The RTS ranged from 8.5 d to 6 mo[15,17,19] (Table 4 and Figure 2C).
Surgical management: Three studies recorded RTS following PSM of acute fractures[19-21], and one study recorded RTS following SSM of acute fractures[21]. The RTS ranged 3 to 6 mo for PSM[19-21], and was 14 wk for SSM[21] (Table 4 and Figure 2C).
Conservative management: Four studies recorded RTS following conservative management of stress fractures[22,23,25,26]. The RTS ranged from 5 wk to 3 mo[22,23,25,26] (Table 5 and Figure 2D).
Surgical management: One study recorded RTS for PSM of stress fractures[25], and one study recorded RTS for SSM of stress fractures[26]. The recorded RTS for PSM was 10 wk[25], and for SSM was 4 mo[26] (Table 5 and Figure 2D).
One of the acute fracture studies recorded radiographic union, with a 100% final union rate[21]. Five of the stress fracture studies recorded radiographic union[22-26]. Four of the studies reported a 100% final union rate[22,24-26], and one study reported a 67% final union rate[23].
Acute fractures: Three of the acute fracture studies recorded complications, which were re-fracture (Table 4).
Stress fractures: Five of the stress fracture studies recorded complications, which were delayed union with primary conservative management, non-union with primary conservative management, and residual deformity (Table 5).
While the majority of sport-related toe phalanx fractures were treated with ‘primary conservative management’, acute intra-articular (physeal) fractures had high rates of ‘primary surgical management’, especially when displaced[19-21].
Sixteen of the twenty-two ‘great toe’ phalanx stress fractures had an associated hallux valgus deformity[8,22-25]. One of the four ‘second toe’ proximal phalanx stress fractures had an associated claw toe deformity[26].
Three of the four ‘second toe’ proximal phalanx stress fractures had a history of stress fractures at other locations, with two of the patients having a history of stress fractures at multiple locations[26].
Of the six stress fractures that required ‘secondary surgical management’, one-third of cases (n = 2) had a significant delay to diagnosis (1 year and 2 years respectively)[24,26], and two-thirds of cases (n = 4) had an associated deformity [hallux valgus (n = 3)/claw toe (n = 1)][8,26].
This systematic review found that the majority of sport-related toe phalanx fractures are treated with ‘primary conservative management’, with satisfactory results for RRS and RTS. For acute fractures, intra-articular (physeal) fractures, especially when displaced, had high rates of ‘primary surgical management’. Such fractures had uniform good RRS, though had prolonged RTS, due to the required post-operative restrictions. For stress fractures, those with significantly delayed diagnosis or with significant underlying causative deformity were at risk of requiring surgical intervention. Again, such fractures, when treated surgically, demonstrated good overall RRS, though with prolonged RTS due to the required post-operative restrictions. However, given the limited, heterogenous data available, it was difficult to draw firm conclusions from this review.
The quality of the included studies in this review was lower than that of similar studies[13,27-31], with a mean CMS of 49.6. This was particularly true for the stress fracture studies, with a mean CMS of 45.5.
From the review data, it is difficult to conclude the optimal management of acute sport-related toe phalanx fractures[15-21]. The results appear to support ‘primary conservative management’ of extra-articular, non or minimally displaced fractures, with overall acceptable RRS and RTS[15-21]. ‘Primary surgical management’ should be reserved for extra-articular fractures which are significantly displaced, rotated, or open[9]. However, there is no evidence to guide such recommendations[15-21]. Surgery is also indicated for displaced, intra-articular (physeal) fractures[9]. There is moderate evidence to support this recommendation, with the need to restore joint surface congruency, especially in the adolescent athlete[19-21]. However, if these fractures are non or minimally displaced, they can be treated with ‘primary conservative management’[19-21]. The review shows reasonable RRS and RTS for both primary conservative and surgical management of these fractures, however, surgical management has longer RTS, due to post-operative restrictions[15-21]. Refractures following ‘primary conservative management’ necessitating ‘secondary surgical management’ is associated with a notably prolonged RTS[21].
Regarding the optimal surgical technique for intra-articular fractures, several methods have been described, though the evidence is inadequate to conclude which is best[19-21]. Compared to K-wire fixation, screw fixation avoids the risk of pin-track infection and may allow for a quicker return to non-contact training activities (no risk of catching and dislodging the K-wire), but such theories are yet to be proved[19-21,32].
With a variety of rehabilitation techniques described, it is difficult to confirm which is the optimal method[15-21]. It would appear that heel weight-bearing in a forefoot offloading shoe can be recommended, both with ‘primary surgical management’ and ‘primary conservative management’[15-21]. This avoids the need for complete non-weight bearing, allowing more muscle mass preservation[15-21]. Following such restrictions, for between 4 to 6 wk, a graduated return to activities can be commenced[15-21].
Reviewing the common sporting mechanisms of injury (tackle and dismount), it would appear there may be a future role for improved protective footwear, to reduce the incidence of traumatic toe phalanx fractures[15,19-21]. Modification of technique, especially in gymnastics, may also allow for future reduction in the incidence of such fractures. However, further research on this topic is required to confirm such theories[32].
Similar to acute fractures, with the limited, heterogeneous data available, it remains difficult to conclude the optimal management for sport-related, toe phalanx stress fractures[8,22-26]. Anatomically, these should be ‘low-risk’ stress fractures, so conservative management should form the first line of treatment[7,33,34]. This has been shown to provide acceptable RRS and RTS[8,22-26]. However, due to variations in the anatomy of the foot, some of these fractures can be associated with an underlying deformity (e.g. hallux valgus), which can create a biomechanically ‘tension-sided’, ‘high risk’ type[8,22,24-26,33,34]. For instance, with hallux valgus, it has been advocated that the medial-sided structures (medial collateral ligament and abductor hallucis) provide an adverse traction force, that potentiates a shear force during exercise, which propagates the stress fracture[8]. In such cases, ‘primary surgical management’ may be necessary to correct the fracture or the deformity[8,22].
Assessing the data available, it would appear that conservative management is acceptable first-line management for all toe phalanx stress fractures[8,22-26]. ‘Primary surgical management’, however, can be considered for cases with significant underlying deformity, especially when they show delayed healing with initial conservative management. It can also be considered for cases with significant delays to diagnosis (> 1 year), with evidence of established non-union at presentation[8,22-26]. Such ‘primary surgical management’ could prevent delayed recovery, due to unnecessary prolonged initial conservative management[8,22-26].
Regarding the optimal surgical technique, there is insufficient data to conclude this[8,22,24-26]. One may consider that the surgeon must correct any underlying significant deformity, at the time of surgical treatment[8,22,24-26]. However, the available data shows that this is not always necessary, to facilitate a successful, timely return to sport[8]. Deformity correction at the time of surgery may reduce the chance of recurrence of the stress fracture on return to sport[8]. However, the more complex surgical technique required may incur a higher risk of complications, prolonged post-operative immobilization and a prolonged return to sport[8]. As such, the optimal strategy for this problem remains to be defined[8]. With established non-unions, the adjunct of biological stimulus (e.g. bone grafting) should be considered[24].
Regarding the optimal rehabilitation with ‘primary conservative management’, it would appear that initial cessation of sporting activities for around 4 to 8 wk is an appropriate first-line plan[8,22-26]. If successful, this should be followed by a graduated return to sport[8,22-26]. For surgical management, heel weight-bearing in a forefoot offloading shoe for 6 wk, followed by a graduated return to sports is similarly an appropriate regime[8,22,24-26].
While modifiable predisposing factors have been extensively reviewed for stress fractures as a whole, with important findings such as sub-optimal physiological condition (e.g. female athlete triad), excessive repetitive training, and abnormal physiological load, there is limited information regarding this for toe phalanx stress fractures[7,8,22,24-26,34]. As discussed previously, the associated deformity is a significant predisposing factor for these fractures, and this should be actively sought and monitored appropriately[8,22,24-26]. Similarly, tight footwear, which exacerbates such deformities, should be avoided[8]. Further research is required to determine optimal methods by which to prevent such injuries in the future[8,22-26].
There are several limitations to this study. These are predominantly based on the limited, heterogeneous data on the topic[8,15-26].
The lack of available literature on toe phalanx fractures has been previously highlighted[5]. This is likely a consequence of most toe phalanx fractures being managed directly from emergency departments, with limited input from orthopedic services[35]. Future collection of data on this subject should be encouraged, through the relevant services, to increase the information on this topic.
Despite this, of the studies retrieved, several of those with high cohort numbers failed to stratify the fractures by toe or phalanx injured, or by treatment type received[16-18]. Such limitations prevent accurate analysis of these datasets and subsequently preclude data synthesis and meta-analysis of the available studies.
As such, it was not possible to draw firm conclusions on the optimal treatment and rehabilitation of these injuries, nor the expected RRS and RTS[8,15-26]. Further more detailed, research on this topic is required, stratifying outcome data by fracture location and a treatment selected.
There is limited information on return to sport following toe phalanx fractures. The majority of acute fractures are treated with ‘primary conservative management’, with overall satisfactory RRS and RTS. ‘Primary surgical management’ is reserved for significantly displaced fractures or displaced intra-articular fractures and has been found to achieve good RRS and RTS. Conservative management forms the first line of treatment for sport-related, toe phalanx stress fractures. When successful, this can result in appropriate RTS. Surgical management is indicated with associated deformity and delayed union, or with significantly delayed presentation and established non-union. In both instances, good RRS and RTS can be achieved. Further research is required to better define the optimal treatment and rehabilitation of sport-related, toe phalanx fractures.
There is very little evidence available to guide the management of toe phalanx fractures in the athletic population.
This is the first systematic review to assess return to sport following toe phalanx fractures. It provides a comprehensive overview of the available literature, assessing both acute fractures and stress fractures.
To systemically review all studies recording return to sport following toe phalanx fractures (including acute fractures and stress fractures), and to collate information on return rates to sport (RRS) and return times (RTS) to the sport.
A systematic search of all relevant scientific databases was performed followed by manual screening of articles according to the eligibility criteria.
Most toe phalanx fractures were treated conservatively. Surgical management was reserved for displaced or intra-articular acute fractures, as well as symptomatic stress fracture non-unions, and stress fractures with significant underlying deformity. RRS for both acute fractures and stress fractures managed conservatively ranged from 0% to 100%. RRS for both acute fractures and stress fractures managed surgically was 100%. RTS after conservative management ranged from 8.5 d to 6 mo for acute fractures, and 5 wk to 3 mo for stress fractures. RTS after surgical management ranged from 3 to 6 mo for acute fractures, and 10 wk to 4 mo for stress fractures.
The majority of sport-related toe phalanx fractures (acute and stress) are managed conservatively with overall satisfactory RRS and RTS.
Currently, the available literature regarding return to sport after toe phalanx fractures is limited, with most studies being low-volume case series. Further research is required to better define the optimal treatment and rehabilitation of sport related toe phalanx fractures.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mesregah MK, Egypt; Shalaby MN, Egypt S-Editor: Liu JH L-Editor: A P-Editor: Ma YJ
| 1. | Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1916] [Cited by in RCA: 2181] [Article Influence: 114.8] [Reference Citation Analysis (0)] |
| 2. | Schnaue-Constantouris EM, Birrer RB, Grisafi PJ, Dellacorte MP. Digital foot trauma: emergency diagnosis and treatment. J Emerg Med. 2002;22:163-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Mittlmeier T, Haar P. Sesamoid and toe fractures. Injury. 2004;35 Suppl 2:SB87-SB97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Rennie L, Court-Brown CM, Mok JY, Beattie TF. The epidemiology of fractures in children. Injury. 2007;38:913-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 334] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 5. | Van Vliet-Koppert ST, Cakir H, Van Lieshout EM, De Vries MR, Van Der Elst M, Schepers T. Demographics and functional outcome of toe fractures. J Foot Ankle Surg. 2011;50:307-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Court-Brown CM, Wood AM, Aitken S. The epidemiology of acute sports-related fractures in adults. Injury. 2008;39:1365-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Saxena A, Anderson R, Bouchè RT, Fournier M, Fullem B, Gerdesmeyer L, Maffulli N. Stress Fractures in Sport: Foot. In: Robertson GA, Maffulli N, editors. Fractures in Sport. Switzerland: Springer Nature; 2021; 465-89. [DOI] [Full Text] |
| 8. | Yokoe K, Kameyama Y. Relationship between stress fractures of the proximal phalanx of the great toe and hallux valgus. Am J Sports Med. 2004;32:1032-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Patel KA, Richards SM, Day J, Drakos MC. Acute Fractures in Sport: Foot. In: Robertson GA, Maffulli N, editors. Fractures in Sport. Switzerland: Springer Nature; 2021; 283-303. [DOI] [Full Text] |
| 10. | Robertson GA, Wood AM. Fractures in sport: Optimising their management and outcome. World J Orthop. 2015;6:850-863. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 11. | Laird RC. Acute forefoot and midfoot injuries. Clin Podiatr Med Surg. 2015;32:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47074] [Article Influence: 2942.1] [Reference Citation Analysis (0)] |
| 13. | Robertson GAJ, Ang KK, Maffulli N, Keenan G, Wood AM. Return to sport following Lisfranc injuries: A systematic review and meta-analysis. Foot Ankle Surg. 2019;25:654-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 647] [Cited by in RCA: 765] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 15. | Robertson GA, Wood AM, Bakker-Dyos J, Aitken SA, Keenan AC, Court-Brown CM. The epidemiology, morbidity, and outcome of soccer-related fractures in a standard population. Am J Sports Med. 2012;40:1851-1857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | Larsson D, Ekstrand J, Karlsson MK. Fracture epidemiology in male elite football players from 2001 to 2013: 'How long will this fracture keep me out?'. Br J Sports Med. 2016;50:759-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Chan JJ, Geller JS, Chen KK, Huang HH, Huntley SR, Vulcano E, Aiyer A. Epidemiology of Severe Foot Injuries in US Collegiate Athletes. Orthop J Sports Med. 2021;9:23259671211001131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Diaz CC, Lavoie-Gagne OZ, Korrapati A, John NS, Diaz MI, Forlenza EM, Trasolini NA, Forsythe B. Return to Play and Player Performance After Foot Fracture in UEFA Soccer Players. Orthop J Sports Med. 2022;10:23259671221078308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Maffulli N. Epiphyseal injuries of the proximal phalanx of the hallux. Clin J Sport Med. 2001;11:121-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Perugia D, Fabbri M, Guidi M, Lepri M, Masi V. Salter-Harris type III and IV displaced fracture of the hallux in young gymnasts: A series of four cases at 1-year follow-up. Injury. 2014;45 Suppl 6:S39-S42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Bariteau JT, Murillo DM, Tenenbaum SA, Brodsky JW. Joint salvage after neglected intra-articular physeal fracture of the hallux in high-level gymnasts. Foot Ankle Spec. 2015;8:130-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Yokoe K, Mannoji T. Stress fracture of the proximal phalanx of the great toe. A report of three cases. Am J Sports Med. 1986;14:240-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Shiraishi M, Mizuta H, Kubota K, Sakuma K, Takagi K. Stress fracture of the proximal phalanx of the great toe. Foot Ankle. 1993;14:28-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Pitsis GC, Best JP, Sullivan MR. Unusual stress fractures of the proximal phalanx of the great toe: a report of two cases. Br J Sports Med. 2004;38:e31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Munemoto M, Sugimoto K, Takakura Y. Stress fractures of the proximal phalanx of the great toe: a report of four cases. Foot Ankle Int. 2009;30:461-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Vanhoutte PM, Lüscher TF. Serotonin and the blood vessel wall. J Hypertens Suppl. 1986;4:S29-S35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Robertson GAJ, Goffin JS, Wood AM. Return to sport following stress fractures of the great toe sesamoids: a systematic review. Br Med Bull. 2017;122:135-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Robertson GA, Wood AM. Return to Sport After Tibial Shaft Fractures: A Systematic Review. Sports Health. 2016;8:324-330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Robertson GA, Wood AM. Return to sports after stress fractures of the tibial diaphysis: a systematic review. Br Med Bull. 2015;114:95-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 30. | Robertson GA, Wood AM. Return to sport following clavicle fractures: a systematic review. Br Med Bull. 2016;119:111-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 31. | Goffin JS, Liao Q, Robertson GA. Return to sport following scaphoid fractures: A systematic review and meta-analysis. World J Orthop. 2019;10:101-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (2)] |
| 32. | Robertson GA, Wood AM, Ahluwalia RS, Keenan GF. Acute Fracture Injuries in Sport. In: Robertson GA, Maffulli N, editors. Fractures in Sport. Switzerland: Springer Nature; 2021; 35-60. [DOI] [Full Text] |
| 33. | Robertson GA, Wood AM. Lower limb stress fractures in sport: Optimising their management and outcome. World J Orthop. 2017;8:242-255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 41] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (2)] |
| 34. | Miller TL, Kaeding CC. Stress Fracture Injuries in Sport. In: Robertson GA, Maffulli N, editors. Fractures in Sport. Switzerland: Springer Nature; 2021; 61-74. [DOI] [Full Text] |
| 35. | Mackenzie S, Riddoch F, Martin D, McCann C, Bayram J, Duckworth A, White T. Intervention rates are low after direct discharge from the Edinburgh trauma triage clinic: Outcomes of 6,688 patients. Injury. 2022;53:3269-3275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |