Published online May 18, 2023. doi: 10.5312/wjo.v14.i5.328
Peer-review started: November 18, 2022
First decision: March 24, 2023
Revised: April 6, 2023
Accepted: April 18, 2023
Article in press: April 18, 2023
Published online: May 18, 2023
Processing time: 150 Days and 15.8 Hours
The treatment of late stages of Legg-Calvé-Perthes disease (LCPD) is controversial. Although the concept of femoral head containment is a well-established technique of treatment, its use remains debatable in the late stages of the disease, as it does not improve symptoms in terms of limb length discrepancy and gait.
To assess the results of subtrochanteric valgus osteotomy in symptomatic patients with late-stage Perthes disease.
From 2000 to 2007, 36 symptomatic patients with late stage of Perthes disease were surgically treated with subtrochanteric valgus osteotomy and followed-up for 8 to 11 years using the IOWA score and range of motion (ROM) variables. The Mose classification was also assessed at the last follow-up to reflect possible remodeling. The patients were 8 years old or older at the time of surgery, in the post-fragmentation stage, and complaining of pain, limited ROM, Trendelenburg gait, and/or abductor weakness.
The preoperative IOWA score (average: 53.3) markedly improved at the 1-year post follow-up period (average: 85.41) and then slightly improved at the last follow-up (average: 89.4) (P value < 0.05). ROM improved, with internal rotation increased on average by 22° (from 10° preoperatively to 32° postoperatively) and abduction increased on average by 15.9° (from 25° preoperatively to 41° postoperatively). The mean Mose deviation of femoral heads was 4.1 mm at the end of the follow-up period. The tests used were the paired t-test and Pearson correlation test, where the level of significance was a P value less than 0.05.
Subtrochanteric valgus osteotomy can be a good option for symptomatic relief in patients with late-stage of LCPD.
Core Tip: This is a retrospective study on 36 patients with ages ranging from 8 to12 years with late stage Perthes disease (re-ossification and healing stages) underwent femoral valgus osteotomy with rotational component which result in pain relief, improved gait, and increased range of motion. In addition, relative neck lengthening is also achieved that can correct limb length discrepancy resulting from head deformity associated with the disease which for many patients may be the only problem encountered Preoperative hip arthrography is done to see the sphericity of the hip and whether there are lateral osteophytes or not.
- Citation: Emara KM, Diab RA, Emara AK, Eissa M, Gemeah M, Mahmoud SA. Mid-term results of sub-trochanteric valgus osteotomy for symptomatic late stages Legg-Calvé-Perthes disease. World J Orthop 2023; 14(5): 328-339
- URL: https://www.wjgnet.com/2218-5836/full/v14/i5/328.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i5.328
Legg-Calvé-Perthes disease is the childhood onset of osteonecrosis of the femoral head and its etiology remains poorly understood. The incidence of the disease among children varies from 0.2 per 100000 to 19.1 per 100000, with white populations being the most affected and East Asians being the least affected[1]. The prognosis of Perthes disease is controversial, with some studies showing a benign long-term outcome[2,3], while others suggest that it may lead to poor long-term sequalae (Stulberg classification type IV and V)[4-6]. Consequently, the optimal treatment approach for this condition remains debatable.
Although varus femoral osteotomy[7-10] and pelvic osteotomy[11-16] are well-established techniques for enhancing femoral head containment in the treatment of Perthes disease, their use in the late stages of the disease is controversial. They do not appear to improve symptoms such as limb length discrepancy (LLD) and may even worsen them[17-20]. Therefore, head containment should not be the primary target of treatment, particularly in the late stages of Perthes disease[7-9]. The prognosis depends more on the disease stage rather than the type of surgery performed[21], and there is no significant difference in outcomes using Stulberg radiographic criteria between conservative treatment and containment surgery in late Perthes disease[17,22].
Valgus femoral osteotomy is usually described for treatment of hinged abduction that is associated with late stages of Perthes disease[23-26]. The benefits are gained by moving the abutting epiphyseal fragment away from the acetabulum and lateralizing the greater trochanter increasing the abductor lever arm and the offset, and hence the abductor function. This results in pain relief, improved gait, and increased range of motion (ROM). In addition, relative neck lengthening is also achieved that can correct LLD resulting from head deformity associated with the disease[25]. Valgus osteotomy is also used to treat severely deformed Perthes disease, Herring classification system type B-C and C, in the fragmentation stage that showed greater congruency with adduction with improved clinical and radiological outcomes[27].
To our knowledge, no prior studies have investigated the role of femoral valgus osteotomy in the symptomatic late stages (re-ossification and healing) of Perthes disease in the absence of hinged abduction. Our hypothesis is that this approach can improve symptoms and function without targeting remodeling, as it is not possible after the fragmentation stage. We conducted a study to evaluate the clinical and radiological outcomes of this approach, with an average follow-up period of nine years.
This retrospective cohort case series study was conducted on human participants from 2000 to 2007, performed by a single surgeon at an institutional hospital, and followed-up over 8-11 years (mean 9.36). It was conducted in accordance with the 1964 declaration of Helsinki and its later amendments/clarifications and with approval from the ethics and search committee, approved and analyzed prior to invitation of the study. Inclusion criteria were: (1) Ages 8 years or older; (2) femoral heads in the re-ossification or healing stages according to the Waldenström classification[28]; and (3) exhibition of symptoms in the form of Trendelenburg gait, abductor weakness, limping, LLD, pain, and/or limited ROM. Exclusion criteria were: (1) Patients below 8 years of age; (2) a Waldenström classification of initial or fragmentation stages; (3) asymptomatic patients; (4) patients with hinge abduction deformity; and (5) history of previous hip or pelvic surgeries.
The study included 36 patients, 23 males and 13 females, with Perthes disease in re-ossification or healing stage, 11 and 25 respectively, presented by symptoms. The symptoms varied and included pain, abductor weakness (Trendelenburg gait), external rotation gait, LLD, and/or limited abduction (Table 1). Asymptomatic Perthes disease (20 cases) was excluded from the study. None of the patients included had hinged abduction deformity confirmed by examination under general anesthesia according to Kruse et al[14] and Rhienker et al[29] definitions. The age range was between 8-12 years (mean 9.41). All the patients in the study group were treated with subtrochanteric valgus osteotomy and fixation was by pre-contoured plate in 23 cases (63.9 %) or dynamic hip screw (DHS) in 13 cases (36.1 %) (Table 2)[30-32]. All patients reached skeletal maturity at the time of last follow up.
| Clinical picture | Count |
| Pain | 31 (86.1) |
| Trendlenburg gait and abductor weakness | 30 (83.3) |
| External rotation gait | 29 (80.5) |
| Limb length discrepancy | 34 (94.4) |
| Limited abduction | 3 (8.3) |
| Fixed flexion deformity | 9 (25) |
| Case | Sex | Age at surgery | Waldenström classification | Joseph classification[30] | Catterall classification[31] | Stulberg classification | Mose[32] at last F.U. (mm) | Follow up period | Implant |
| 1 | M | 9 | Re-ossification | IIIb | III | III | 3 | 9 | Contoured plate |
| 2 | M | 8 | Re-ossification | IIIa | III | III | 2 | 8 | Contoured plate |
| 3 | F | 9 | Healing | IV | IV | IV | 5 | 10 | DHS |
| 4 | M | 11 | Re-ossification | IIIb | III | IV | 8 | 11 | DHS |
| 5 | F | 10 | Re-ossification | IIIb | IV | III | 5 | 9 | Contoured plate |
| 6 | F | 8 | Healing | IV | III | III | 6 | 9 | Contoured plate |
| 7 | M | 9 | Re-ossification | IIIb | II | II | 1 | 8 | Contoured plate |
| 8 | M | 9 | Re-ossification | IIIa | II | II | 2 | 9 | Contoured plate |
| 9 | M | 12 | Healing | IV | IV | III | 4 | 10 | DHS |
| 10 | F | 10 | Healing | IV | IV | III | 5 | 9 | Contoured plate |
| 11 | M | 9 | Re-ossification | IIIa | III | IV | 9 | 8 | Contoured plate |
| 12 | F | 8 | Healing | IV | II | II | 1 | 8 | DHS |
| 13 | M | 9 | Healing | IV | III | III | 3 | 9 | Contoured plate |
| 14 | M | 10 | Re-ossification | IIIb | III | III | 4 | 10 | Contoured plate |
| 15 | F | 11 | Re-ossification | IIIb | IV | III | 4 | 9 | Contoured plate |
| 16 | M | 10 | Re-ossification | IIIb | III | IV | 8 | 9 | DHS |
| 17 | F | 11 | Healing | IV | II | II | 1 | 8 | Contoured plate |
| 18 | M | 9 | Healing | IV | IV | IV | 7 | 11 | Contoured plate |
| 19 | F | 8 | Re-ossification | IIIa | III | III | 2 | 9 | DHS |
| 20 | M | 9 | Healing | IV | III | III | 4 | 10 | Contoured plate |
| 21 | M | 8 | Healing | IV | II | II | 1 | 11 | DHS |
| 22 | M | 9 | Re-ossification | IIIb | III | II | 2 | 9 | Contoured plate |
| 23 | F | 9 | Re-ossification | IIIa | II | III | 6 | 8 | DHS |
| 24 | M | 8 | Re-ossification | IIIa | III | III | 5 | 9 | Contoured plate |
| 25 | F | 10 | Healing | IV | IV | IV | 8 | 10 | DHS |
| 26 | F | 11 | Healing | IV | III | II | 1 | 9 | Contoured plate |
| 27 | M | 9 | Healing | IV | IV | IV | 5 | 9 | Contoured plate |
| 28 | M | 9 | Re-ossification | IIIa | III | III | 2 | 9 | Contoured plate |
| 29 | F | 8 | Re-ossification | IIIa | II | II | 2 | 9 | DHS |
| 30 | M | 8 | Healing | IV | III | III | 4 | 10 | Contoured plate |
| 31 | M | 9 | Re-ossification | IIIb | III | III | 5 | 8 | DHS |
| 32 | M | 10 | Re-ossification | IIIb | III | IV | 4 | 8 | DHS |
| 33 | M | 11 | Re-ossification | IIIb | II | II | 2 | 9 | Contoured plate |
| 34 | M | 10 | Healing | IV | IV | IV | 6 | 9 | Contoured plate |
| 35 | M | 9 | Healing | IV | IV | IV | 10 | 9 | DHS |
| 36 | F | 12 | Healing | IV | III | II | 1 | 10 | Contoured plate |
The patients underwent a thorough clinical assessment focusing on functionality and pain history, as well as clinical examination that addressed gait, ROM, and deformity. Hence, the IOWA hip score[33] and ROM were evaluated once preoperatively and twice postoperatively (1st at 1 year postoperative and 2nd at the end of the follow-up period). The IOWA hip score is a 100-point scale that evaluates the hip by assessing different functional activities (35 points), freedom from pain (35 points), gait abnormality (10 points), deformity (10 points), and ROM (10 points), with the highest point scale indicating the best function[33]. Data collection was performed by the 2nd, 3rd, and 4th authors.
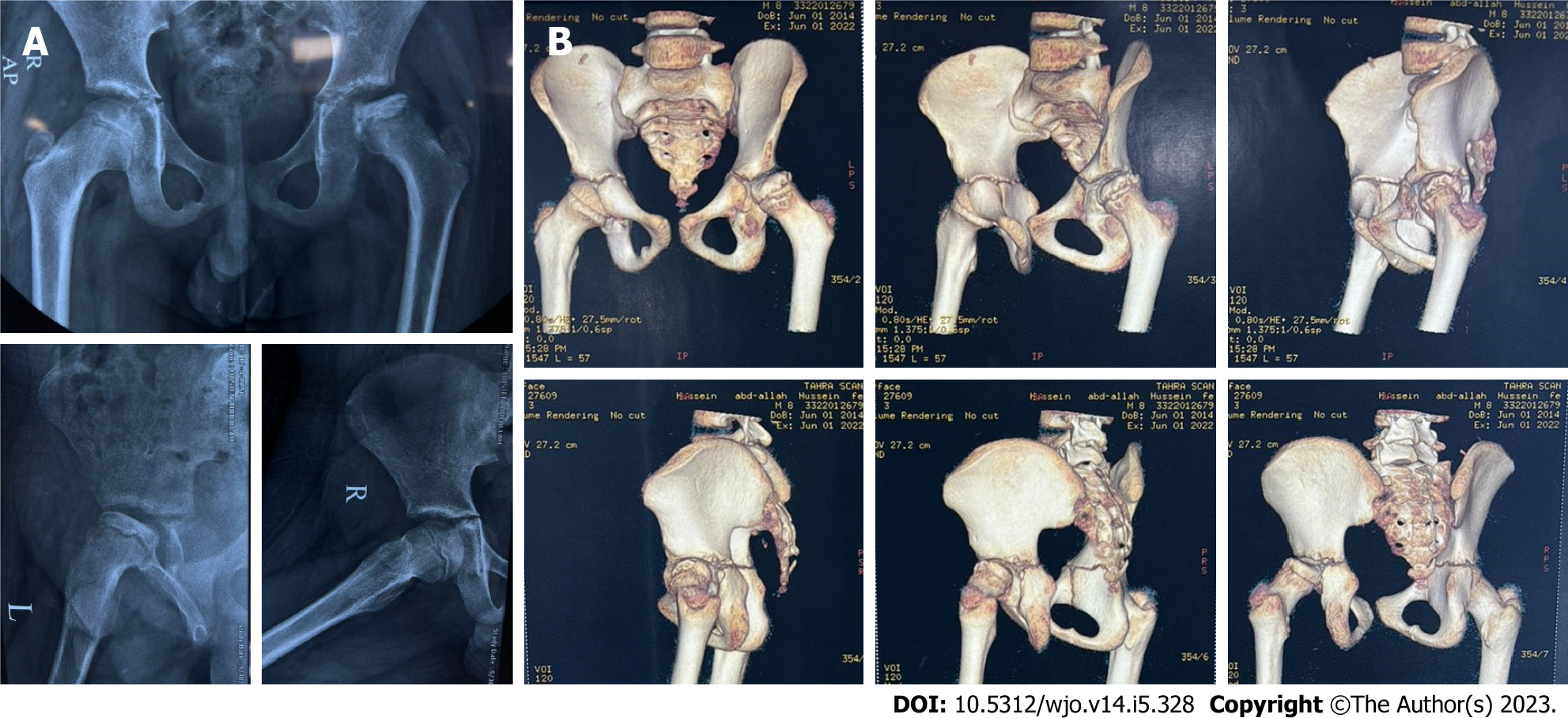
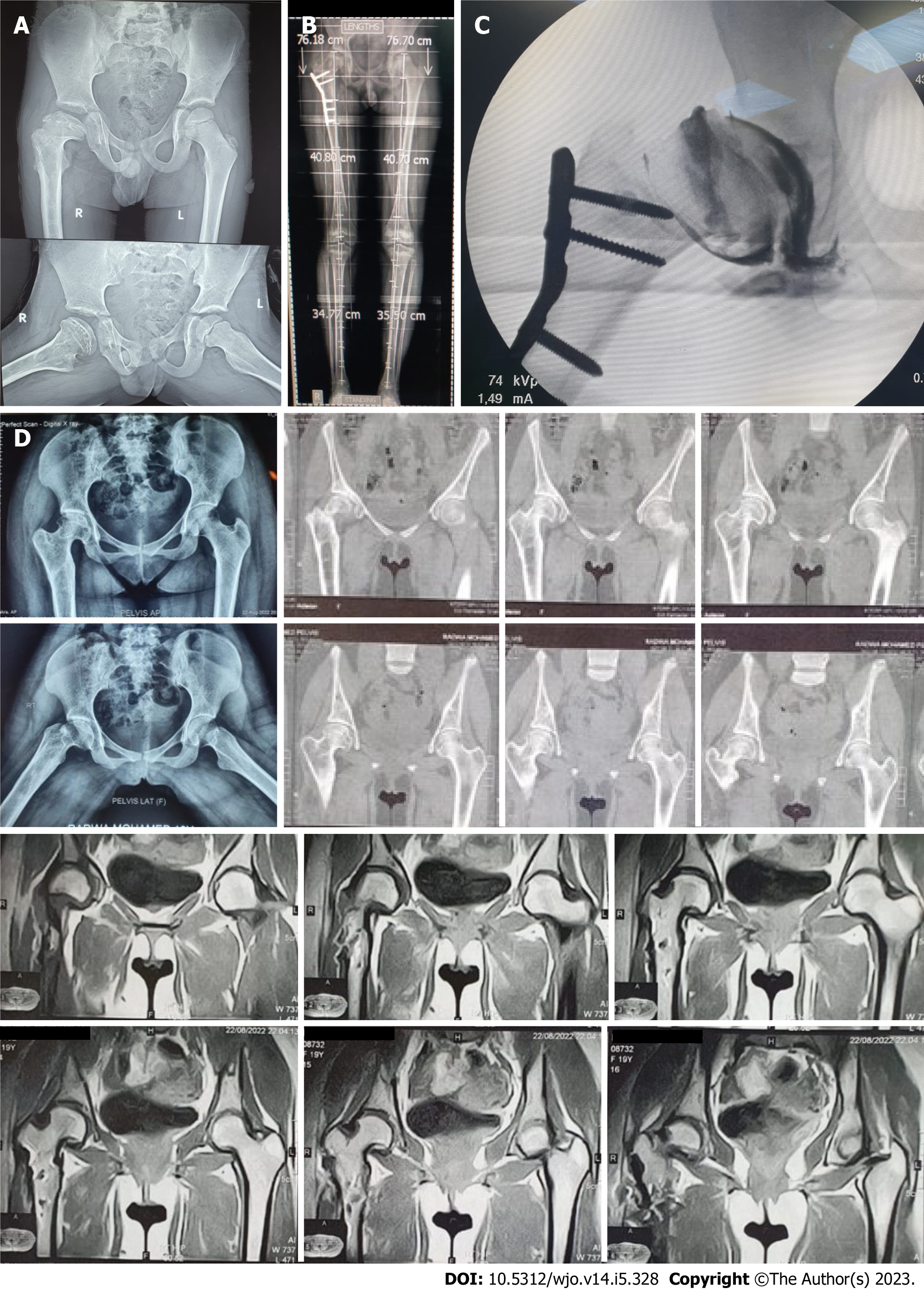
The extent of limb deformity was carefully evaluated both clinically and radiologically (using plain X-rays, computed tomography scans, and intraoperative arthrography) to plan for the required planes and degrees of correction and to identify the most deformed part of the femoral head, with the goal of unloading it (Figure 1). The degree of valgus and rotation performed was measured by using the unaffected limb as a reference. If the patient was affected bilaterally, we relied on hip arthrography and neck shaft angle (NSA) and performed the valgus and rotation to the degree that brought lateral osteophytes away from the required range of motion and made the NSA more than 130 degrees. Therefore, the degree of correction was tailored to each patient individually.
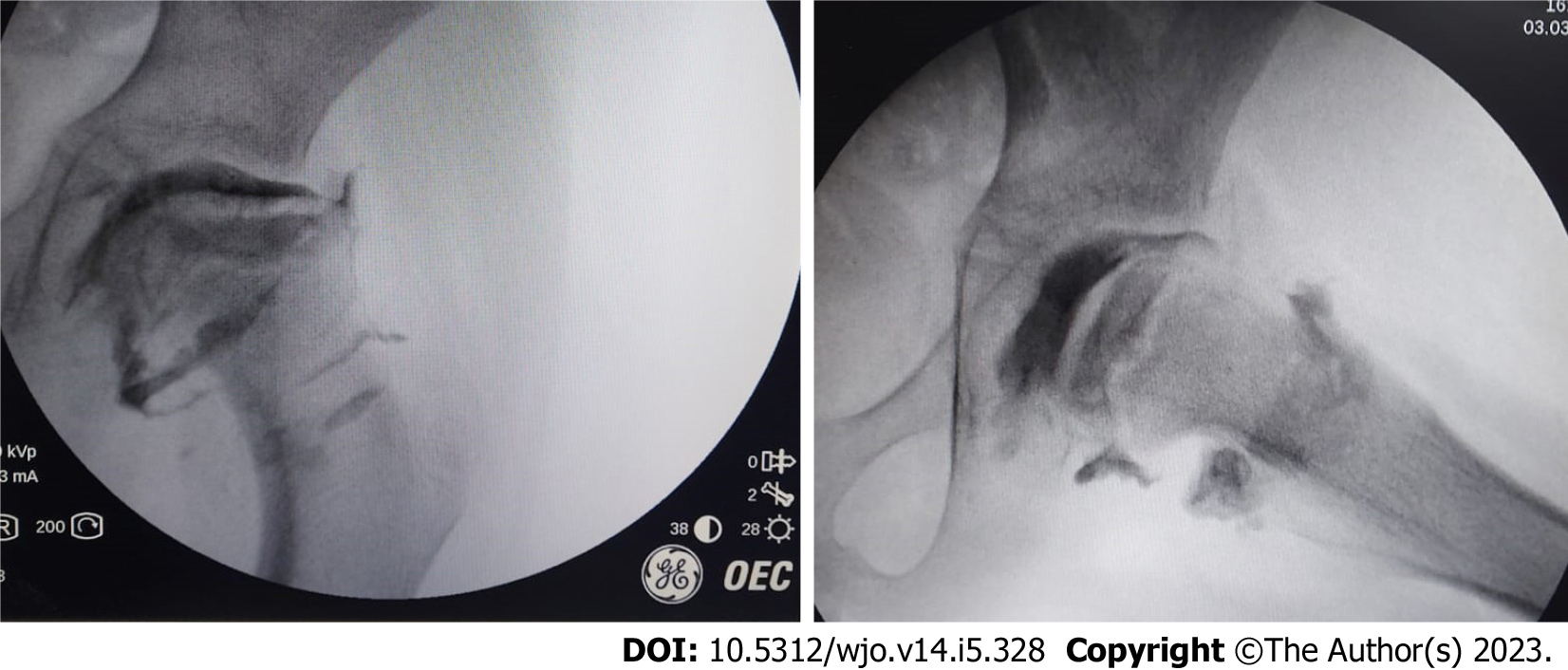
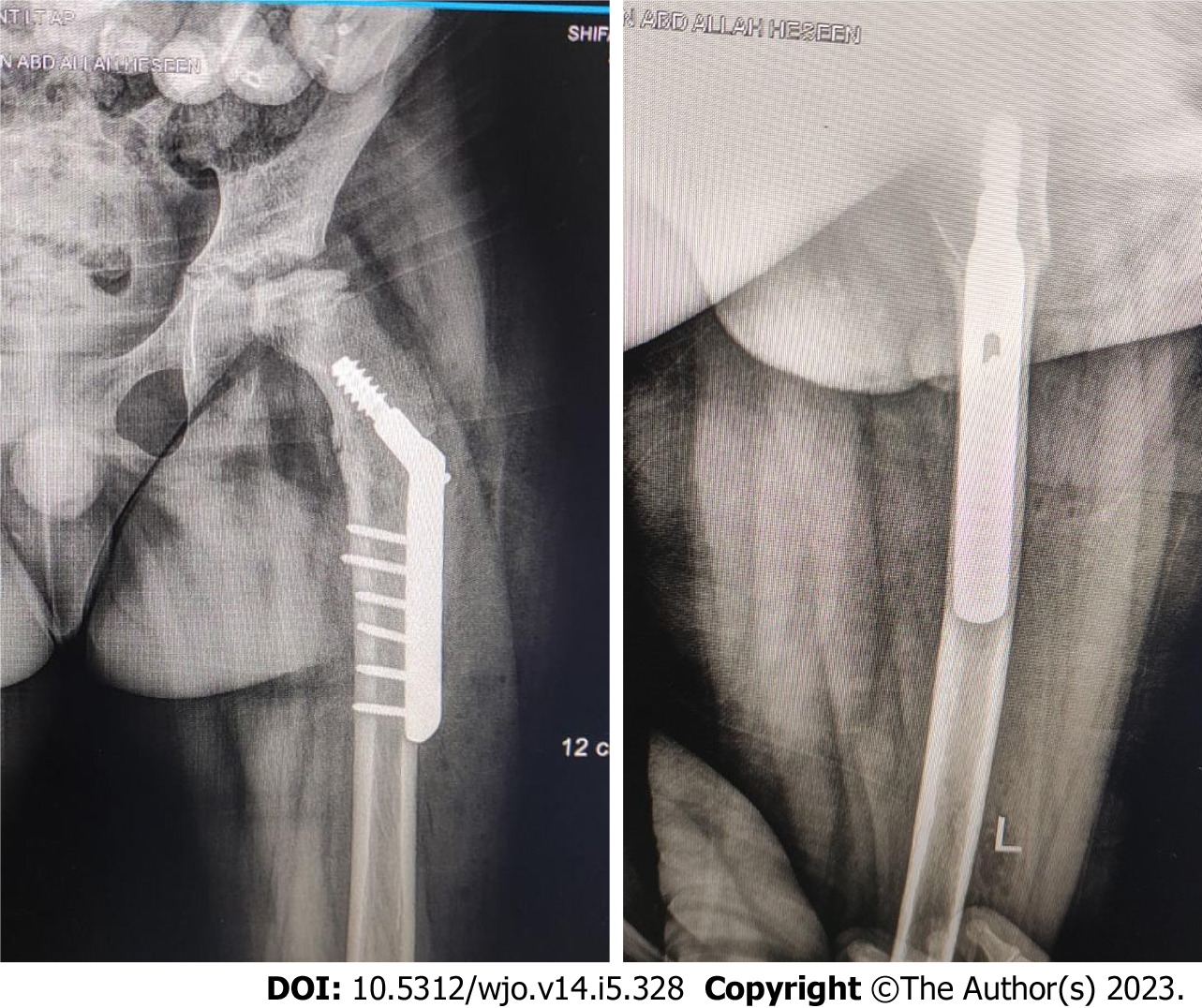
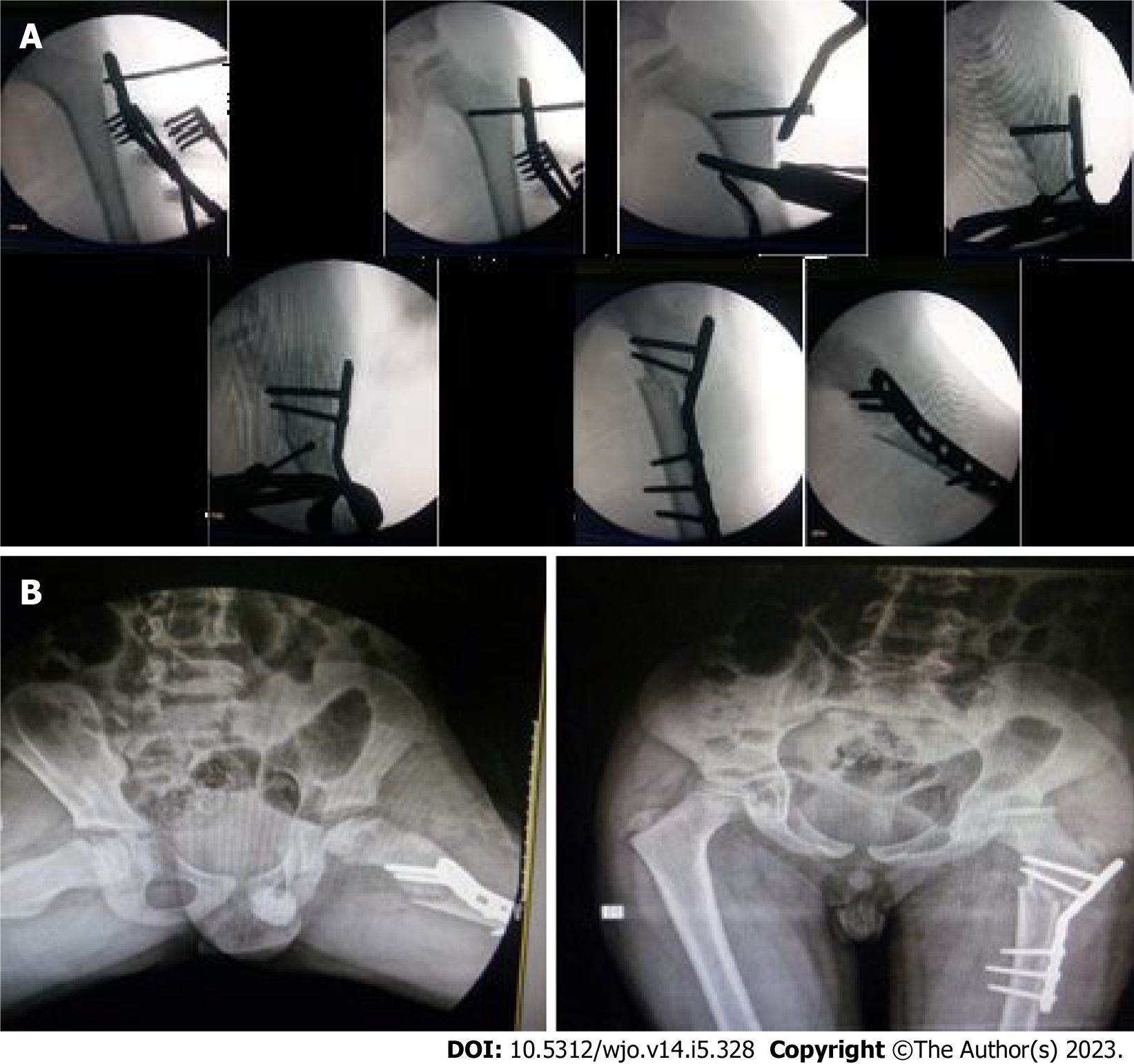
Patients were placed supine on a radiolucent table. A direct lateral approach was utilized to access the femur. First, hip arthrography is done to confirm the sphericity of the head and to see whether there are lateral osteophytes or not, also the hip arthrography determines the direction of our osteotomy according to the site of osteophytes as mentioned above (Figure 2). The level of osteotomy was determined under an image intensifier, which was always subtrochanteric. In some cases, a pre-contoured plate (narrow plate) was used, and the plate was contoured to the desired degree of valgus and loosely fixed with a screw to the neck. In cases involving DHS, the desired degree of valgus was achieved by adjusting the inclination of the guide wire of the lag screw accordingly. The osteotomy was performed using multiple drill holes to weaken the cortex then completed by an osteotome. The osteotomy aimed to perform valgus, internal rotation, lateral translation, and extension of the distal femur if any limitations in the preoperative flexion range were discovered. Additionally, the osteotomy was oblique to provide inherent stability, and a de-rotation element was added to unload the affected portion, thereby relieving pain and correcting the external rotational deformity that is frequently associated with Perthes disease. After plate fixation, frequent irrigation was performed, followed by tissue closure in layers (Figures 3 and 4).
Postoperative protocol included non-weight bearing for 6 wk, followed by physical therapy for gait training, balance, and abductor muscle strengthening. Subsequently, partial weight bearing was allowed with crutches, which was then progressed to full weight bearing without crutches.
Statistical analysis was conducted to determine the significance of functional outcomes, patients' age at the time of surgery, and the follow-up period for the improvement of symptoms. IBM SPSS statistics (version 24.0, IBM Corp., United States, 2016) was used for data analysis. The data were presented as mean ± SD for quantitative parametric measures and as numbers and percentages for categorized data. The following tests were performed: (1) Paired t-test was used to compare two dependent groups for parametric data; and (2) Pearson correlation test was used to analyze the possible association between each two variables among each group for parametric data. The level of significance was set at P < 0.05.
On average, the internal rotation increased by 22° (range: 10°-40°), from an average of 10° preoperatively to an average of 32° postoperatively with SD 5.72. Abduction increased by an average of 15.9° (range: 10°-35°) from an average of 25° preoperatively to an average of 41° postoperatively with SD 5.18. LLD improved in 30 cases (average improvement 0.9 cm) and remained unchanged in 6 cases. LLD was measured using the tape method and approximated to 0.5 cm, 1 cm, 1.5 cm, and so on. The difference between the preoperative and postoperative measures was statistically significant (P < 0.05) (Table 3).
| Descriptive statistics | n | Min | Max | mean ± SD |
| Age | 36 | 8 | 12 | 9.4 ± 1.5 |
| Follow up | 36 | 8 | 11 | 9.36 ± 2.2 |
| IOWA score preoperative | 36 | 30 | 70 | 53.3 ± 10.1 |
| Postoperative after 1 yr | 36 | 77 | 100 | 85.4 ± 5.4 |
| Final | 36 | 79 | 100 | 89.4 ± 5.2 |
| Internal rotation degree | 36 | 10 | 40 | 22.1 ± 5.26 |
| Abduction degree | 36 | 10 | 35 | 15.7 ± 6.2 |
Twenty-three boys and 13 girls underwent unilateral subtrochanteric valgus osteotomies. The average age was 9.4 years (range 8-12) with an average follow-up period of 9.1 years (range 8-11). Clinical outcomes were assessed using the IOWA hip score[33] preoperatively, at 1-year postoperative, and at the last postoperative follow-up. The preoperative IOWA score had an average of 53.3 and SD 10.1, and it showed a marked improvement at the 1-year postoperative follow-up, with an average of 85.4 and SD 5.4. There was a slight improvement at the final follow-up, with an average of 89.4 and SD 5.2. The improvement was significant in pain, with an average of 22.4 preoperative to an average of 36.2 postoperative, walking tolerance, with an average of 4.7 preoperative to an average of 8.7 postoperative, gait, with an average of 3.5 preoperative to an average of 12.9 postoperative, shortening, with an average of 1.2 preoperative to 2.6 postoperative, and Trendelenburg absence, with an average of 2 preoperative to 0 postoperative. The difference between preoperative and final outcomes was statistically significant (P < 0.05).
At the end of the follow-up period, Mose classification[32] was evaluated to assess any remodeling, with physis closure ensured. The mean Mose deviation was 4.11 mm, ranging from 1-10 mm.
Superficial infection occurred in four cases, which were treated with daily dressings and a parenteral antibiotic course with no sequels. Six cases required hardware removal due to pain.
The optimal treatment approach for late stages of Perthes disease is still debatable. Although achieving proper femoral head containment (such as varus femoral osteotomy and pelvic osteotomy) to promote head remodeling and delay the need for total hip replacement (THR) has been widely accepted in the surgical treatment of the disease, there are many clinical and pathological aspects that raise concerns about the use of this surgical method in late symptomatic stages[34]. Firstly, the relationship between Perthes disease and osteoarthritis (OA) is atypical. According to Stulberg classification[4], only aspherical incongruent cases carry a risk of severe OA, which usually doesn't develop before the 5th decade. Additionally, there is no correlation between symptom severity and osteoarthritic radiographic changes in Perthes disease. Furthermore, Perthes OA affects the medial joint compartment rather than the superior compartment, which is typically affected in age-related degenerative joint diseases. This different pattern of OA carries a better prognosis than the typical superior compartment one[5,22]. Larson et al[17] studied the outcomes of conservative management on 58 hips with a mean follow-up of 20.4 years, where only three patients required hip arthroplasty, and one patient required a pelvic osteotomy. This study supports the atypical relationship between Perthes disease and OA. Regarding varus femoral osteotomy, its use in treating Perthes disease has many limitations. Its effectiveness in providing the desired remodeling potential is restricted to cases in the early avascular and fragmentation stages. Therefore, its use in the re-ossification or healing stages is of questionable value[7,9]. It is also limited to cases with a skeletal age of 8 years or more at onset, particularly Herring classification system group B and B/C border[5,21]. Sponseller et al[10] even concluded that the use of varus femoral osteotomy in patients older than 10 years yielded poor results, indicating that its use may be restricted to Herring classification system group B and B/C border in patients aged 8-10 years in the early avascular or fragmentation stages. Moreover, although varus femoral osteotomy may relieve pain associated with the disease by providing containment, it exacerbates the symptoms of limping due to the shortening of the affected limb[8]. It also worsens the Trendelenburg gait by increasing the abductor weakness[18,20]. Watanabe et al[19] studied gait analysis after varus femoral osteotomy and found that the stance phase was shorter, cadence was faster, and the strength ratio of hip abductor muscles was lower in operated patients vs non-operated and healthy subjects.
Arthrodiastasis has been studied in cases of late-stage Perthes disease with advanced Catterall stages and has shown satisfactory clinical and radiological outcomes. However, its effect is most significant when the disease is in the early avascular or fragmentation stages, as it can prevent head collapse and speed up recovery[27,35].
Two surgical approaches have been utilized to treat patients with healed Perthes in adulthood; safe surgical dislocation and combined acetabular and femoral osteotomies[36-38]. Safe surgical dislocation has been used to treat complex femoral deformities resulting from Perthes disease, with positive outcomes and statistically significant results. Trochanteric advancement and osteochondroplasty have been performed to address short neck, chondral and labral lesions, and femoro-acetabular impingement that may complicate Perthes disease in adulthood[36-38]. Clohisy et al[37] described a combined periacetabular osteotomy and intertrochanteric valgus osteotomy to treat femoral head deformities complicated by acetabular dysplasia. The procedure was performed on 42 cases (mean age 22.7 years) and followed up over 4.5 years, with statistically significant improvement in the Harris hip score. However, none of these procedures were used to treat Perthes disease before healing during childhood.
In addition, head remodeling is not limited to the containment concept. Yoo et al[24] studied the effect of valgus extension osteotomy on remodeling potential in hinge abduction cases and observed favorable remodeling in young cases that were at the fragmentation or early re-ossification stages. This is supported by Kim et al[27], who studied valgus osteotomy on patients at the fragmentation stage who had better containment by adduction. All femoral head roundness measures and the Shenton line were improved, with the best results demonstrated in severely deformed heads with Herring classification type C. This indicates that patient characteristics and disease stage at the time of intervention are the main determinants of head remodeling, rather than the type of surgery performed[24]. In delayed stages of Perthes disease, such as re-ossification and healing stages, containment can no longer be achieved, and the potential for remodeling is lost[39]. Many of these cases develop hinged abduction, and several studies have described the use of valgus femoral osteotomy in an attempt to move the abutted head away, with good outcomes[23-26]. Bankes et al[25] described the use of extension valgus osteotomy in 48 cases in the re-ossification stage, resulting in improved symptoms with a ten-year follow-up, but no prospective scoring system was used to quantify the improvement. Yoo et al[24] added sagittal and coronal rotational components to accurately accommodate different hinging patterns, resulting in improved mean IOWA score from 71 to 92 in a long-term study on 31 patients. The same results were achieved by Myers et al[26] in a short-term study, with an improved mean Harris hip score by 41.
However, no studies have discussed valgus femoral osteotomy among symptomatic late-stage Perthes disease in the absence of hinged abduction. We conducted a retrospective study on such a population group with ages ranging from 8 to 12 years. Our chosen operative intervention was femoral valgus osteotomy with a rotational component, and we observed the patients over a period of 8-11 years, assessing them clinically using the IOWA score[33] (Figure 5). Preoperative hip arthrography was done to assess the sphericity of the hip and the presence of lateral osteophytes. This simple surgical procedure, femoral valgus osteotomy, can relieve existing symptoms such as pain, limping, limb length discrepancy, limited ROM, and abductor weakness, which for many patients may be the only problem encountered.
On the other hand, we considered the re-ossification and healing stages to be critical periods, as we could not guarantee containment via varus femoral or pelvic osteotomy, and the potential complication of OA later on was uncertain to have a significant impact on the functional activity of the diseased patients compared to other patients who might eventually develop it. The controversies regarding the prognosis of Perthes disease compelled us to focus on relieving existing symptoms and improving the quality of life of these patients. In this study, the clinical outcomes significantly improved from an average IOWA score of 53.3 preoperatively to 89.4 at the end of the follow-up period, with a highly significant P value (P < 0.01). ROM increased, which is reflected in the patient's quality of life. Internal rotation and abduction improved by an average of 22° and 15.9° degrees, respectively. The mean Mose deviation was 4.11 mm, reflecting the lack of remodeling in these stages, and this is consistent with results of Yoo et al[24], which showed no improved radiographic indices in such an entity. There was a positive relationship between the age at the time of surgery and functional improvement, with a P value of 0.001, making it a potential good option in the treatment of older symptomatic patients with Perthes disease. There was no correlation between the duration of the follow-up period and functional improvement, with a P value of 0.979. This necessitates further evaluation by long follow-up studies.
There is no proof that other types of surgery could change the natural history of late-stage Perthes disease or add value in improving patient symptoms, articular impingement, weak abduction, and limb length discrepancy. Therefore, our protocol to deal with symptomatic late-stage Perthes disease is either to leave the patient with no surgery, just conservative treatment for symptoms, or to do valgus de-rotation osteotomy to bring the osteophyte away from the joint articular surface. Hip arthrography is needed for proper dynamic assessment of the articular surface.
The limitations of this study include its retrospective nature and lack of control groups that receive other treatments such as conservative and other surgical procedures. Longer follow-up periods are also needed to assess the end fate of the hips and the risk of OA development, although the mid-term outcomes display promising efficacy and safety. It is also important to determine whether the deformity of the proximal femur would remodel or have any impact on future THR surgery. Further studies to tailor the use of sub-trochanteric valgus osteotomy according to the patient's age of onset and the disease stage are also required.
We hypothesize that valgus femoral osteotomy is a valid option for patients with late-stage Perthes disease. This procedure can effectively alleviate symptoms such as pain, limping, and limb length discrepancy, which may be the only problems encountered by many patients for an extended period of time. Therefore, valgus femoral osteotomy could be used beyond its role as a salvage option in hinge abduction cases.
Legg-Calvé-Perthes disease is a condition that affects the hip joint, most commonly in children between the ages of 4 and 10. In this disease, the blood supply to femoral head. The treatment of late-stage Perthes disease remains controversial, and there is debate about the most effective techniques for managing symptoms and improving long-term outcomes.
The motivation for this study was to contribute to the ongoing debate about the most effective treatment approaches for late-stage Perthes disease, and to evaluate the potential benefits of subtrochanteric valgus osteotomy in improving symptoms and long-term outcomes.
The objective of this study was to evaluate the outcomes of subtrochanteric valgus osteotomy in patients with late-stage Perthes disease.
The study included 36 symptomatic patients with late-stage Perthes disease who underwent subtrochanteric valgus osteotomy between 2000 and 2007. The patients were aged 8 or older at the time of surgery, in the post-fragmentation stage of the disease, and experiencing pain, limited range of motion, Trendelenburg gait, and/or abductor weakness.
The results of the study showed that subtrochanteric valgus osteotomy significantly improved hip function and range of motion in patients with late-stage Perthes disease.
The study concluded that subtrochanteric valgus osteotomy can be an effective treatment option for relieving symptoms and improving hip function and range of motion in patients with late-stage Perthes disease. The results of the study suggest that this surgical technique can be a valuable addition to the range of treatment options available for this condition.
The study provides important insights into the potential benefits of subtrochanteric valgus osteotomy for patients with late-stage Perthes disease. However, further research is needed to confirm the findings of this study and to evaluate the long-term outcomes of this treatment approach.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bhuyan BK, India; Jeyaraman M, India S-Editor: Zhang H L-Editor: A P-Editor: Zhao S
| 1. | Perry DC, Machin DM, Pope D, Bruce CE, Dangerfield P, Platt MJ, Hall AJ. Racial and geographic factors in the incidence of Legg-Calvé-Perthes' disease: a systematic review. Am J Epidemiol. 2012;175:159-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 2. | McAndrew MP, Weinstein SL. A long-term follow-up of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 1984;66:860-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 162] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Engelhardt P. [Late prognosis of Perthes' disease: which factors determine arthritis risk? Z Orthop Ihre Grenzgeb. 1985;123:168-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 1981;63:1095-1108. [PubMed] |
| 5. | Beer Y, Smorgick Y, Oron A, Mirovsky Y, Weigl D, Agar G, Shitrit R, Copeliovitch L. Long-term results of proximal femoral osteotomy in Legg-Calvé-Perthes disease. J Pediatr Orthop. 2008;28:819-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Ippolito E, Tudisco C, Farsetti P. The long-term prognosis of unilateral Perthes' disease. J Bone Joint Surg Br. 1987;69:243-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 97] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Axer A. Subtrochanteric osteotomy in the treatment of perthes' disease: a preliminary report. J Bone Joint Surg Br. 1965;47:489-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Canario AT, Williams L, Wientroub S, Catterall A, Lloyd-Roberts GC. A controlled study of the results of femoral osteotomy in severe Perthes' disease. J Bone Joint Surg Br. 1980;62-B:438-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Lloyd-Roberts GC, Catterall A, Salamon PB. A controlled study of the indications for and the results of femoral osteotomy in Perthes' disease. J Bone Joint Surg Br. 1976;58:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 111] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Sponseller PD, Desai SS, Millis MB. Comparison of femoral and innominate osteotomies for the treatment of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 1988;70:1131-1139. [PubMed] |
| 11. | Cahuzac JP, Onimus M, Trottmann F, Clement JL, Laurain JM, Lebarbier P. Chiari pelvic osteotomy in Perthes disease. J Pediatr Orthop. 1990;10:163-166. [PubMed] |
| 12. | Camurcu IY, Yildirim T, Buyuk AF, Gursu SS, Bursali A, Sahin V. Tönnis triple pelvic osteotomy for Legg-Calve-Perthes disease. Int Orthop. 2015;39:485-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Carsi B, Judd J, Clarke NM. Shelf acetabuloplasty for containment in the early stages of Legg-Calve-Perthes disease. J Pediatr Orthop. 2015;35:151-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Kruse RW, Guille JT, Bowen JR. Shelf arthroplasty in patients who have Legg-Calvé-Perthes disease. A study of long-term results. J Bone Joint Surg Am. 1991;73:1338-1347. [PubMed] |
| 15. | Thompson GH. Salter osteotomy in Legg-Calvé-Perthes disease. J Pediatr Orthop. 2011;31:S192-S197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Vukasinovic Z, Spasovski D, Vucetic C, Cobeljic G, Zivkovic Z, Matanovic D. Triple pelvic osteotomy in the treatment of Legg-Calve-Perthes disease. Int Orthop. 2009;33:1377-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Larson AN, Sucato DJ, Herring JA, Adolfsen SE, Kelly DM, Martus JE, Lovejoy JF, Browne R, Delarocha A. A prospective multicenter study of Legg-Calvé-Perthes disease: functional and radiographic outcomes of nonoperative treatment at a mean follow-up of twenty years. J Bone Joint Surg Am. 2012;94:584-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 18. | Matan AJ, Stevens PM, Smith JT, Santora SD. Combination trochanteric arrest and intertrochanteric osteotomy for Perthes' disease. J Pediatr Orthop. 1996;16:10-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Watanabe H, Shimada Y, Kagaya H, Sato K. Gait analysis following varus osteotomy of the femur for hip osteoarthritis. J Orthop Sci. 1999;4:89-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Weiner SD, Weiner DS, Riley PM. Pitfalls in treatment of Legg-Calvé-Perthes disease using proximal femoral varus osteotomy. J Pediatr Orthop. 1991;11:20-24. [RCA] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part II: Prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004;86:2121-2134. [RCA] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 227] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 22. | Arkader A, Sankar WN, Amorim RM. Conservative versus surgical treatment of late-onset Legg-Calve-Perthes disease: a radiographic comparison at skeletal maturity. J Child Orthop. 2009;3:21-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Choi IH, Yoo WJ, Cho TJ, Moon HJ. The role of valgus osteotomy in LCPD. J Pediatr Orthop. 2011;31:S217-S222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Yoo WJ, Choi IH, Moon HJ, Chang S, Cho TJ, Choi YH, Park MS, Chung CY. Valgus femoral osteotomy for noncontainable Perthes hips: prognostic factors of remodeling. J Pediatr Orthop. 2013;33:650-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Bankes MJ, Catterall A, Hashemi-Nejad A. Valgus extension osteotomy for 'hinge abduction' in Perthes' disease. Results at maturity and factors influencing the radiological outcome. J Bone Joint Surg Br. 2000;82:548-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Myers GJ, Mathur K, O'Hara J. Valgus osteotomy: a solution for late presentation of hinge abduction in Legg-Calvé-Perthes disease. J Pediatr Orthop. 2008;28:169-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Kim SS, Lee CW, Kim HJ, Kim HH, Wang L. Treatment of Late-Onset Legg-Calve-Perthes Disease by Arthrodiastasis. Clin Orthop Surg. 2016;8:452-457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Waldenström H. The Definite Form of the Coxa Plana. Acta Radiol. 2016;57:e79-e94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 29. | Reinker KA. Early diagnosis and treatment of hinge abduction in Legg-Perthes disease. J Pediatr Orthop. 1996;16:3-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Joseph B, Varghese G, Mulpuri K, Narasimha Rao K, Nair NS. Natural evolution of Perthes disease: a study of 610 children under 12 years of age at disease onset. J Pediatr Orthop. 2003;23:590-600. [PubMed] [DOI] [Full Text] |
| 31. | Catterall A. Legg-Calvé-Perthes syndrome. Clin Orthop Relat Res. 1981;41-52. [PubMed] |
| 32. | Mose K. Methods of measuring in Legg-Calvé-Perthes disease with special regard to the prognosis. Clin Orthop Relat Res. 1980;103-109. [PubMed] |
| 33. | Larson CB. Rating scale for hip disabilities. Clin Orthop Relat Res. 1963;31:85-93. [PubMed] |
| 34. | Noonan KJ, Price CT, Kupiszewski SJ, Pyevich M. Results of femoral varus osteotomy in children older than 9 years of age with Perthes disease. J Pediatr Orthop. 2001;21:198-204. [PubMed] |
| 35. | Kadhim M, Holmes L Jr, Bowen JR. The role of shelf acetabuloplasty in early and late stages of Perthes disease: a meta-analysis of observational studies. J Child Orthop. 2012;6:379-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 36. | Anderson LA, Erickson JA, Severson EP, Peters CL. Sequelae of Perthes disease: treatment with surgical hip dislocation and relative femoral neck lengthening. J Pediatr Orthop. 2010;30:758-766. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 37. | Clohisy JC, Nunley RM, Curry MC, Schoenecker PL. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am. 2007;89:1417-1423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 38. | Eid MA. Hip preservation surgery for adolescents and young adults with Post-Perthes Sequelae. Acta Orthop Belg. 2016;82:821-828. [PubMed] |
| 39. | Raney EM, Grogan DP, Hurley ME, Ogden MJ. The role of proximal femoral valgus osteotomy in Legg-Calvé-Perthes disease. Orthopedics. 2002;25:513-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |