Published online May 18, 2023. doi: 10.5312/wjo.v14.i5.319
Peer-review started: December 15, 2022
First decision: March 14, 2023
Revised: March 31, 2023
Accepted: April 20, 2023
Article in press: April 20, 2023
Published online: May 18, 2023
Processing time: 154 Days and 9 Hours
Chronic large to massive rotator cuff tears are difficult to treat and re-tears are common even after surgical repair. We propose using a synthetic polypropylene mesh to increase the tensile strength of rotator cuff repairs. We hypothesize that using a polypropylene mesh to bridge the repair of large rotator cuff tears will increase the ultimate failure load of the repair.
To investigate the mechanical properties of rotator cuff tears repaired with a polypropylene interposition graft in an ovine ex-vivo model.
A 20 mm length of infraspinatus tendon was resected from fifteen fresh sheep shoulders to simulate a large tear. We used a polypropylene mesh as an inter
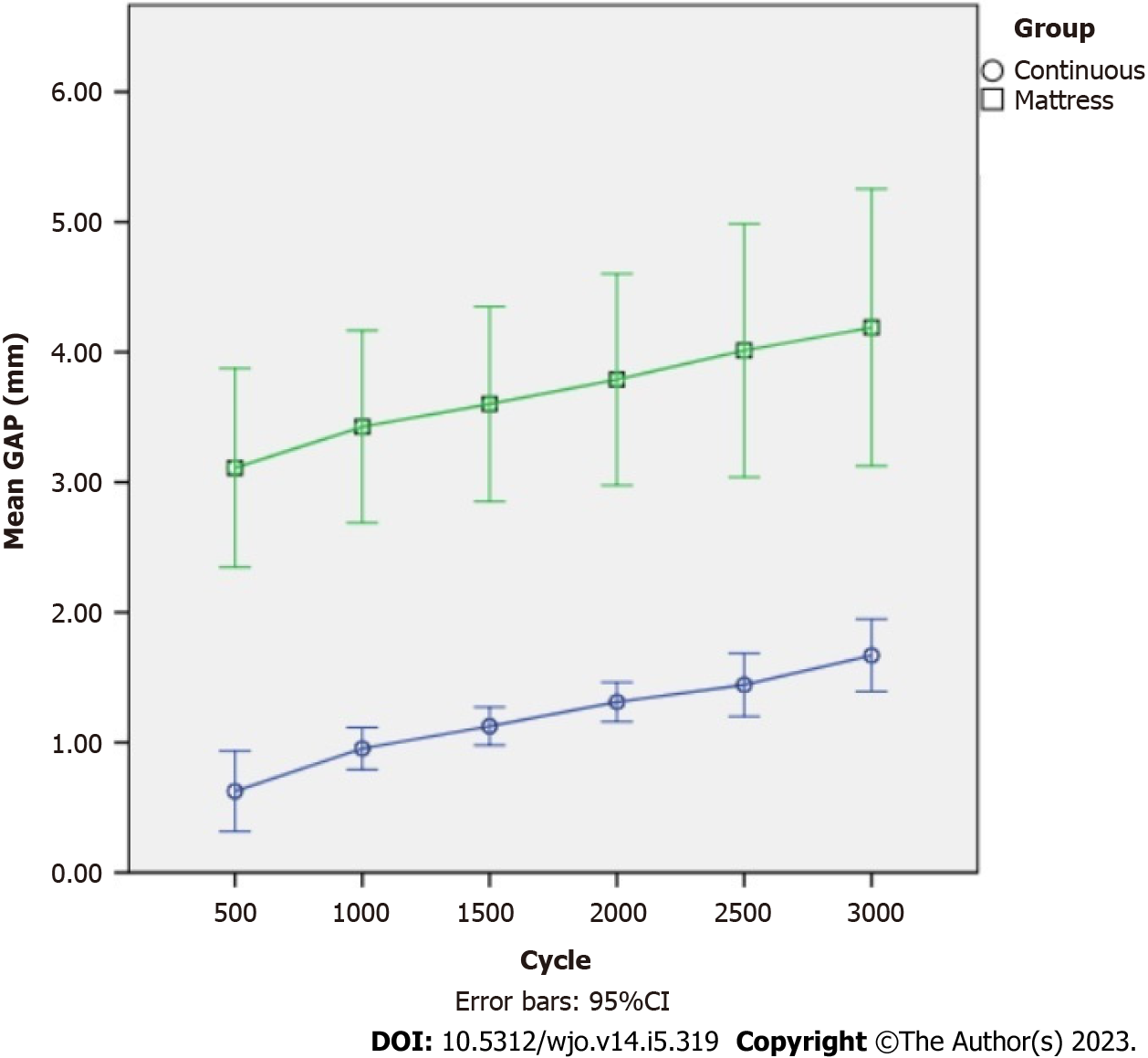
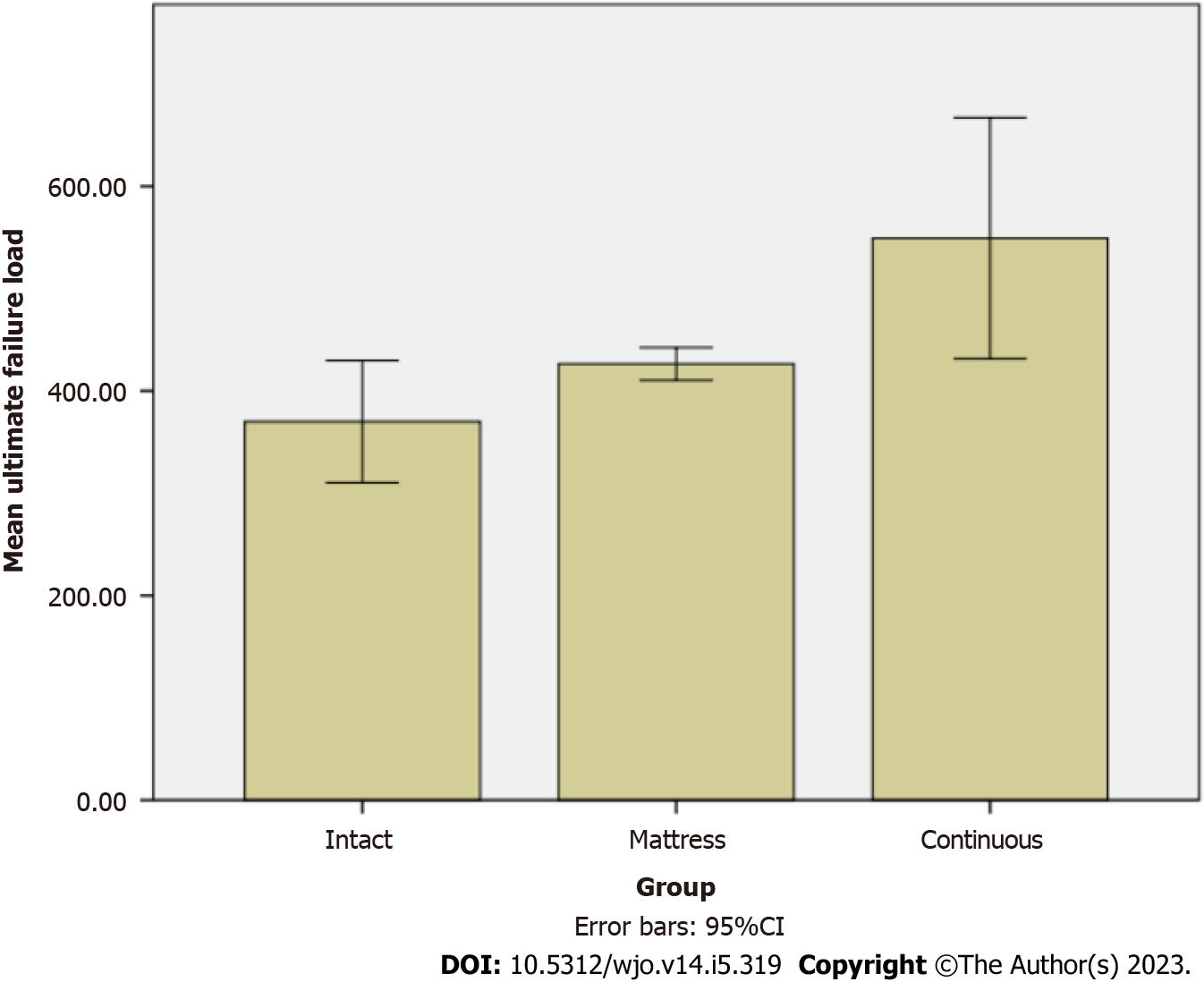
The mean gap formation after 3000 cycles was 1.67 mm in the continuous group, and 4.16 mm in the mattress group (P = 0.001). The mean ultimate failure load was significantly higher at 549.2 N in the continuous group, 426.4 N in the mattress group and 370 N in the intact group (P = 0.003).
The use of a polypropylene mesh is biomechanically suitable as an interposition graft for large irreparable rotator cuff tears.
Core Tip: Our ex-vivo ovine model demonstrates that the use of a polypropylene mesh is mechanically suitable as an interposition graft for large irreparable rotator cuff tears. Its use results in a repair that is at least as robust as an intact rotator cuff tendon. When paired with a continuous suturing technique, its resultant superior mechanical properties may potentially reduce re-tear rates after repairing large or massive rotator cuff tears.
- Citation: Lim WSR, Yew AKS, Lie H, Chou SM, Lie DTT. Rotator cuff repair with an interposition polypropylene mesh: A biomechanical ovine study. World J Orthop 2023; 14(5): 319-327
- URL: https://www.wjgnet.com/2218-5836/full/v14/i5/319.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i5.319
Rotator cuff tears are one of the most common shoulder conditions that orthopaedic surgeons treat. Chronic large to massive tears are difficult to treat due to development of tendon retraction, muscle atrophy and fatty infiltration. In addition, re-tear after primary repair of large to massive tears are common, reportedly between 40%[1] to 94%[2].
Complete, anatomic rotator cuff repair with restoration of the tendon footprint is the preferred treatment option, but it is often not possible in up to 20% of patients with large to massive rotator cuff tears[3]. Numerous joint-preserving procedures have been attempted to address this group of patients with an irreparable tear – tendon transfers of the latissimus dorsi or pectoralis major, superior capsular reconstruction and patch augmentation are among the salvage procedures described[4].
Several materials have been investigated for the purpose of augmenting the rotator cuff repair. The ideal material should provide a biomechanical advantage, be biocompatible and allow for ingrowth of host tissue. The fascia lata and human dermal allografts have been used in clinical practice to repair massive rotator cuff tears. Fascia lata autograft[5] or allograft[6], and human dermal allografts[7,8] have been used as interposition grafts and are also commonly used for superior capsular reconstruction[9]. Commercially available human dermal allograft has an ultimate load of 313 N at 1.4 mm thickness, while fascia lata allograft had a higher ultimate load of 350 N at 1 mm thickness[10]. In clinical studies, the healing rates when human dermal allograft is used is only between 59% to 74%[7,11].
To improve the healing rates, we propose using a synthetic polypropylene mesh to increase the tensile strength of the repair. The polypropylene mesh has been widely used in ventral abdominal and inguinal hernia repair for decades, and its safety and efficacy are well established[12]. However, the use of polypropylene mesh in rotator cuff repair is not well studied. A clinical study by Ciampi et al[13] found that the use of polypropylene patch augmentation for rotator cuff repair resulted in better function and strength, as well as lower re-tear rates compared to collagen patch augmentation or cuff repair alone.
We hypothesize that using a polypropylene mesh to bridge the repair of large rotator cuff tear is a biomechanically sound concept. If proven to be biomechanically viable, it will be the first step towards adopting this widely available, relatively inexpensive material in the clinical setting. Thus, we aim to investigate the time-zero mechanical properties of a rotator cuff repaired with a polypropylene interposition graft in an ovine infraspinatus ex-vivo model. In addition, we aim to compare if continuous stitching of the mesh to the remnant tendon on the greater tuberosity results in higher failure load compared to mattress stitching.
Twenty fresh shoulders from skeletally mature sheep were procured from a local abattoir and used in this study. Ethics approval was not required for this study as it involved commercially available animal specimens. The supraspinatus muscle and tendon, as well as the subscapularis tendon and gleno
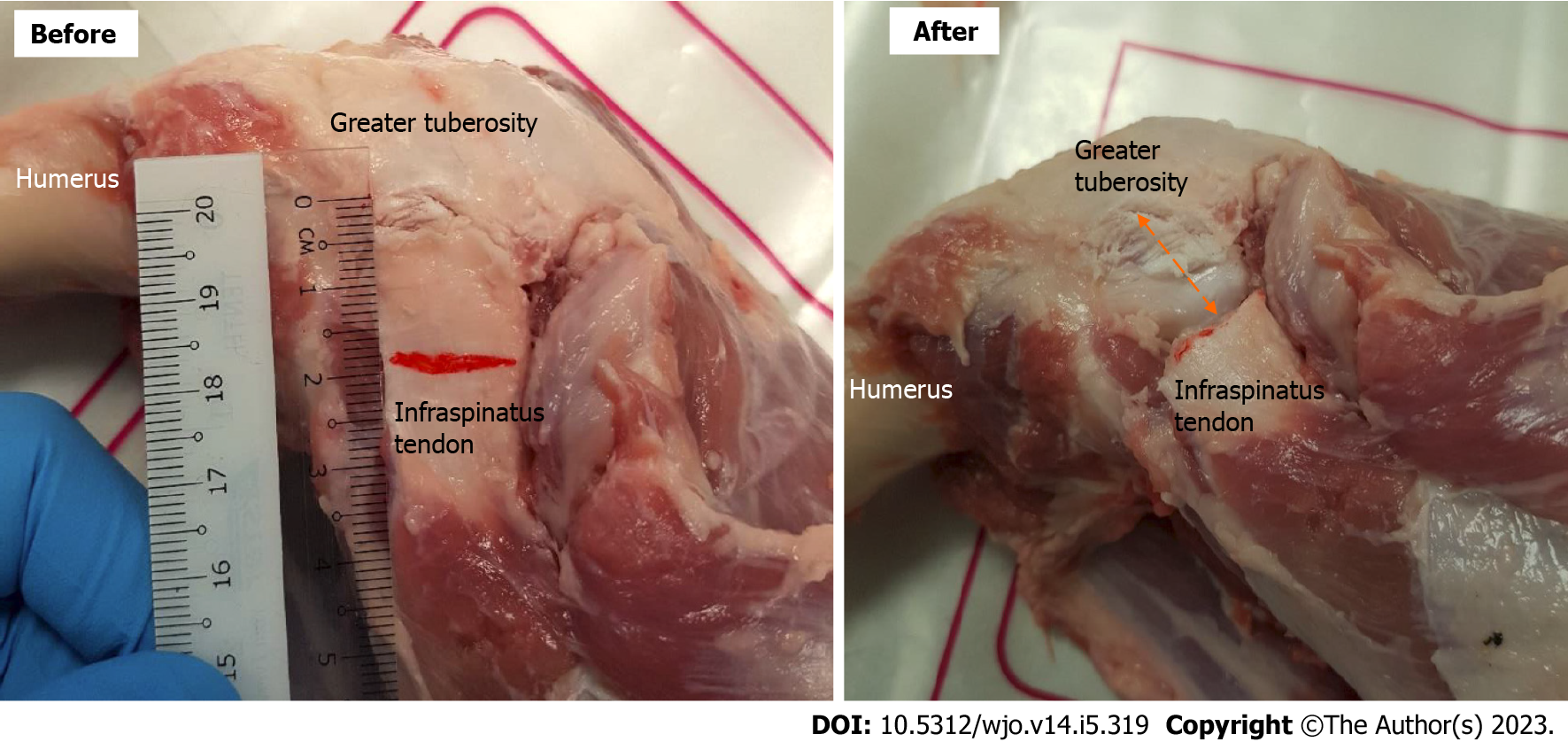
The infraspinatus tendon was sharply detached from its insertion on the greater tuberosity to simulate a full thickness tear in the remaining fifteen specimens. This was followed by resecting a section of tendon 20 mm in length (medial-to-lateral dimension) to further simulate tendon retraction and actual loss of tendon substance due to degeneration at the tendon insertion (Figure 1).
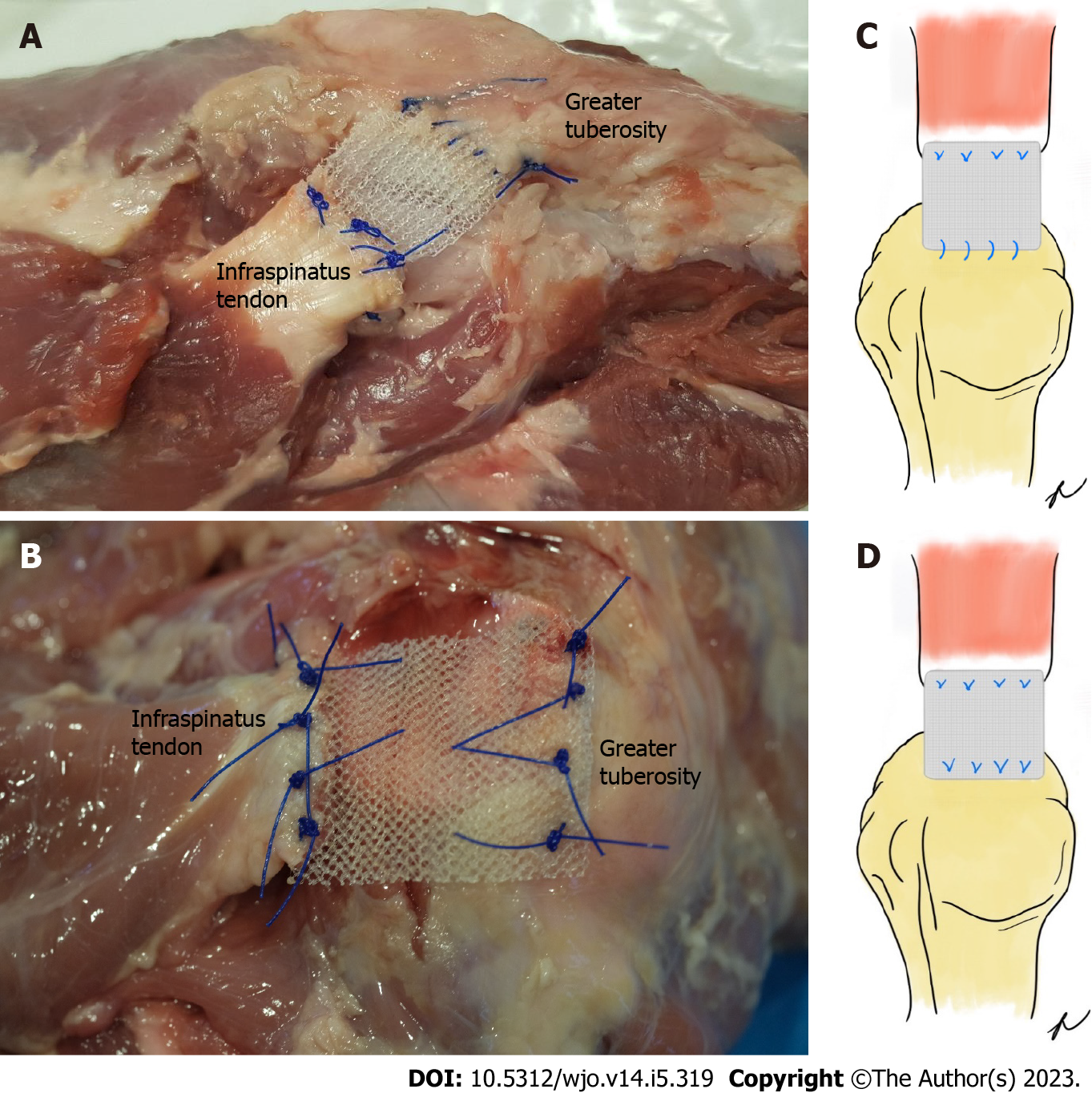
A polypropylene mesh (PROLENE™, ETHICON, NJ, United States) was cut to match the width of the remnant infraspinatus tendon. The length of the mesh was fixed at 60 mm to provide consistency in the test results. The mesh was then folded lengthwise over the tendon on the infraspinatus end and sutured together with four mattress stitches using Prolene 2-0. On the greater tuberosity side, the mesh was secured to the remnant tendon by continuous stitching with Prolene 2-0 in seven specimens (Con
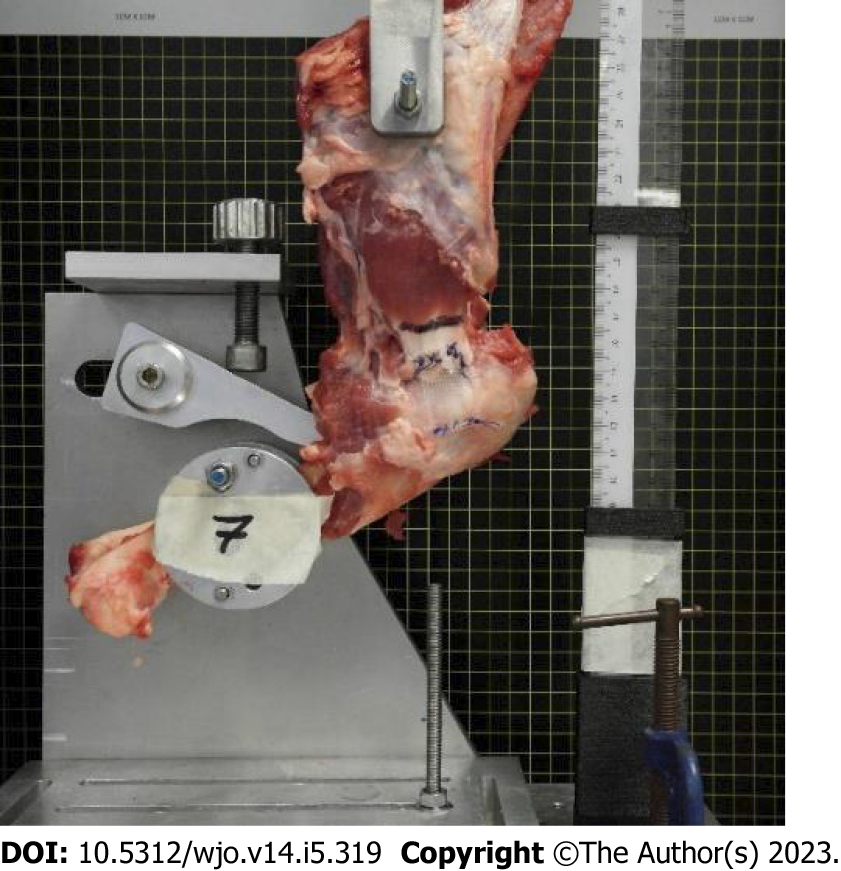
A custom-designed fixture was used to secure the specimens to a universal testing machine (Instron 5566, Instron, MA, United States) with a 10 kN load cell. A hole with diameter 6.5 mm was drilled through the scapula to mount the specimen onto the fixture. A two-piece clamp was used to secure the humerus at the desired abduction angle of 45° (Figure 3). The abduction angle represents the angle the humeral shaft makes with the vertical axis in the direction of cyclic loading.
Biomechanical testing was carried out in three phases – firstly, pre-cycle loading was conducted between 5 and 10 N for 10 cycles to account for the muscle’s elastic elements which are pre-stretched by the load. This was followed by cyclic loading between 10 and 180 N at a cross-head velocity of 8.33 mm/s for a total of 3000 cycles. The change in distance of the tendon lateral edge with loading is regarded as the amount of gap formation and this was measured at every 500 cycles. To record the gap formation, a ruler with marking pieces was mounted beside the test specimen’s tendon for reference (Figure 3). A digital camera mounted on a tripod with its lens facing the tendon perpendicularly was placed in front of the universal testing machine. After each 500 cycles, a high-resolution digital picture of the tendon was taken. The image is processed in ImageJ (version 1.53a) (National Institutes of Health, Bethesda, MA, United States) where a 50 mm line is drawn parallel to the ruler. The measurements were calibrated by comparing the image pixel value of the 50 mm line to 50 mm on the ruler. This was then used to measure the amount of gap formation in each image.
After 3000 cycles of cyclic loading, the specimen was loaded to failure at a cross-head velocity of 1 mm/s to determine the ultimate failure load. The universal testing machine was stopped manually at the first sign of rotator cuff repair failure, and the mode of failure was identified and recorded. For the intact tendon group, testing was terminated once a tear was observed in the tendon.
Statistical analysis was performed with SPSS v23.0 (IBM, SPSS Statistics, Armonk NY, United States) statistical software. Student’s t-test was used to compare gap formation between the two methods of stitching. One-way analysis of variance was used to compare the ultimate failure load between all three groups. Post hoc test was performed using Tukey honest significant difference if one-way analysis of variance was found to be significant. A P value of 0.05 was considered statistically significant.
The mean ultimate failure load in intact tendon was 370 (range 300 N to 425 N, standard deviation 48.1). For the intact group, 3000 cycles of loading could not be completed as tears appeared in the tendons after a mean of 590 cycles and testing was terminated.
In all fifteen specimens which underwent tendon repair, gap formation increased with progressive cyclic loading through the 3000 cycles. At each interval after 500 cycles, the mean gap formation was significantly lower in the continuous group compared to the mattress group (Figure 4). The mean gap formation after 3000 cycles was 1.7 mm (standard deviation 0.3) in the continuous group, while it was 4.2 mm (standard deviation 1.3) in the mattress group (P = 0.001).
All specimens in the Mattress and Continuous group failed through suture pull-out at the greater tuberosity end of the repair. There was no record of any mesh failure or suture breakage. The ultimate failure load in the continuous group ranged from 416.7 N to 755.9 N and ranged from 403.2 N to 466.1 N in the mattress group. The mean ultimate failure load for the continuous group and mattress group was 549.2 N (standard deviation 127.3) and 426.4 N (standard deviation 106.1) respectively.
The ultimate failure load in the continuous group was significantly higher when compared to the mattress group (P = 0.02) and intact group (P = 0.004). There was no statistically significant difference in ultimate failure load between mattress and intact group (P = 0.45) (Figure 5).
Large or massive rotator cuff tears continue to pose a challenge to shoulder surgeons. The use of scaffolds may play a role in the treatment of such tears. These scaffolds can be used to augment or reinforce an anatomically repairable tear. It can also be used to as an interposition graft, where the scaffold bridges the gap between the irreparable cuff and the humerus[14]. Allografts and xenografts extra-cellular matrix scaffold devices provide mechanical support during the early phases of rotator cuff healing but are eventually degraded to be replaced by a mixture of organized muscle cells, collagenous connective tissue and adipose connective tissue[15]. Mihata’s biomechanical analysis of grafts used in superior capsular reconstruction found that human dermal allografts would elongate by 15% with loading, while fascia lata grafts did not change significantly after testing and was also able to completely restore superior glenohumeral joint stability[16]. Due to the stiffness of fascia lata grafts, post-operative shoulder stiffness would be a concern. In addition, there are concerns that biologic grafts may potentially incite a host inflammatory response that may cause breakdown of the repair[15,17].
Synthetic materials, such as those made of polyurethane, polypropylene or expanded polytetrafluoroethylene (PTFE) are able to maintain their mechanical properties over a long period of time, thus stabilizing the repair till tissue healing occurs. Our study suggests that using a polypropylene mesh to augment rotator cuff tendon repair is at least as strong as an intact tendon. When continuous suturing is performed, the ultimate failure load is significantly increased compared to intact tendon.
One of the technical aims of a good rotator cuff repair is to achieve sufficient strength to withstand the pull of the rotator cuff during early passive motion. Burkhart calculated that the maximal contraction force across the rotator crescent to be 302 N[18]. Mall suggested that tendon repairs resist 300 N to 350 N of tensile force to allow for early post-operative motion to help prevent stiffness and maximize healing potential[19]. All our repaired specimens were able to withstand at least 350 N of cyclic loading. Our study also demonstrated that continuous suturing at the greater tuberosity was superior to mattress sutures, with lesser gap formation and higher ultimate failure load.
Several authors have suggested a gap formation of 5 mm at the repair site to be clinically significant[20,21]. In our study, only two specimens in the mattress group exceeded 5 mm of gap formation. In a rodent model, Killian found that the greater the gap between the post-repair tendon-to-bone attachment, the greater the scar formation and presence of disorganized tendon insertion to bone[22]. This suggests that gap formation plays an important role in repair outcomes. It is promising that our mean gap formation was only 1.7 mm in the continuous group, however, in vivo studies using relevant large ovine animal models are still required to determine if this will translate into better tendon-to-bone healing.
Clinical studies of interposition synthetic grafts have been encouraging. Nada et al[23] reported on the use of a polyester Dacron ligament in 21 patients with chronic massive rotator cuff tears. The mean Constant and Murley score increased from 46.7 pre-operatively to 84.5 post-operatively. Petrie et al[24] used the polyester Ligament Augmentation and Reconstruction System in 31 shoulders and reported a mean improvement of Oxford shoulder score from 46.7 to 30.6. Audenaert et al[25] also used a polyester (ethylene terephthalate) mesh in 41 patients and the mean Constant and Murley score increased from 25.7 pre-operatively to 72.1 post-operatively. Hirooka et al[26] used a Gore-Tex expanded PTFE patch in 28 shoulders and reported the average total Japanese Orthopaedic Association score increased from 57.7 to 88.7. Our study suggests that the inexpensive, widely available polypropylene mesh may have a potential role in strengthening the repair of chronic large rotator cuff tears. The polypropylene mesh may even be used in combination with a fascia lata graft to improve graft healing rate as demonstrated by Kholinne when done for superior capsular reconstruction[27].
There are limitations to an ex-vivo animal study. While our study has demonstrated that the polypropylene mesh has good mechanical properties, there have been concerns over its potential to incite a vigorous foreign body and chronic inflammatory response. This may lead to contracture, scar and adhesion formation and chronic pain, particularly troubling in up to 3.6% patients who undergo mesh repair for abdominal hernia[28-30]. However, it is encouraging to note that Ciampi’s study reported no adverse events such local inflammation, fibrosis, and subacromial adhesions affecting joint function in 52 patients with polypropylene mesh augmented rotator cuff repair[13]. Our study did not attempt to undertake histological analysis of the specimens to examine for host-tissue maturation and host-implant biocompatibility as the study was not performed on live animals.
Another limitation of our study is our use of healthy rotator cuff specimens from sheep. While the sheep infraspinatus tendon has similar geometry and mechanical properties to human supraspinatus tendon[31], the healthy rotator cuff specimens may not be representative of the typical degenerate tendon seen in patients with massive rotator cuff tears. In addition, the use of suture anchors to secure the mesh to the tuberosity side could have provided greater biomechanical strength to the repair and prevent suture pull out from the tuberosity, which was the mode of failure in all our specimens. Our study serves as a proof of concept that a polypropylene mesh as an interposition graft may be an option in rotator cuff repairs. Further studies such as comparing the biomechanical properties of the polypropylene mesh to other types of commercially available grafts, and an in-vivo ovine study should be undertaken before adopting its use in human patients.
The use of a polypropylene mesh is mechanically suitable as an interposition graft for large irreparable rotator cuff tears. Its use results in a repair that is at least as robust as intact rotator cuff tendon. When paired with a continuous suturing technique, its resultant superior mechanical properties may potentially reduce re-tear rates after repairing large or massive rotator cuff tears.
Augments and scaffolds are increasing in importance in patients with large to massive cuff tears. There is limited data on the mechanical properties of such materials.
The polypropylene mesh is a time tested, bio-compatible material with strong mechanical properties that may be used in rotator cuff repairs to improve the strength of the repair.
To investigate the mechanical properties of rotator cuff tears repaired with a polypropylene interposition graft in an ovine ex-vivo model.
We used a polypropylene mesh as an interposition graft between the ends of the tendon to repair a tear in the infraspinatus of fresh sheep shoulders. The mesh was secured to remnant tendon by continuous stitching in seven specimens while mattress stitches were used for eight specimens. Five specimens with an intact tendon were tested. The specimens underwent testing to determine the ultimate failure load and gap formation.
The mean gap formation after 3000 cycles was significantly lower in the continuous group than the mattress group. The mean ultimate failure load was also significantly higher in the continuous group when compared to mattress stitching or intact tendon.
The use of a polypropylene mesh is biomechanically suitable as an interposition graft for large rotator cuff tears.
Further studies such as comparing the biomechanical properties of the polypropylene mesh to other types of commercially available grafts, and an in-vivo ovine study should be undertaken before adopting its use in human patients.
The authors would like to acknowledge Muhammad Iylia Asyraf for his assistance in the biomechanical testing of the specimens.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhou Y, China S-Editor: Liu XF L-Editor: A P-Editor: Yuan YY
| 1. | Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007;89:953-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 537] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 2. | Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1579] [Cited by in RCA: 1529] [Article Influence: 72.8] [Reference Citation Analysis (0)] |
| 3. | Henry P, Wasserstein D, Park S, Dwyer T, Chahal J, Slobogean G, Schemitsch E. Arthroscopic Repair for Chronic Massive Rotator Cuff Tears: A Systematic Review. Arthroscopy. 2015;31:2472-2480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 125] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 4. | Greenspoon JA, Petri M, Warth RJ, Millett PJ. Massive rotator cuff tears: pathomechanics, current treatment options, and clinical outcomes. J Shoulder Elbow Surg. 2015;24:1493-1505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 135] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 5. | Mori D, Funakoshi N, Yamashita F, Wakabayashi T. Effect of Fatty degeneration of the infraspinatus on the efficacy of arthroscopic patch autograft procedure for large to massive rotator cuff tears. Am J Sports Med. 2015;43:1108-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Varvitsiotis D, Papaspiliopoulos A, Antipa E, Papacharalampous X, Flevarakis G, Feroussis J. Results of reconstruction of massive irreparable rotator cuff tears using a fascia lata allograft. Indian J Orthop. 2015;49:304-311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Gupta AK, Hug K, Berkoff DJ, Boggess BR, Gavigan M, Malley PC, Toth AP. Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Med. 2012;40:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 149] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 8. | Sharma N, El Refaiy A, Sibly TF. Short-term results of rotator cuff repair using GraftJacket as an interpositional tissue-matched thickness graft. J Orthop. 2018;15:732-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Makovicka JL, Chung AS, Patel KA, Deckey DG, Hassebrock JD, Tokish JM. Superior capsule reconstruction for irreparable rotator cuff tears: a systematic review of biomechanical and clinical outcomes by graft type. J Shoulder Elbow Surg. 2020;29:392-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 10. | Barber FA, Aziz-Jacobo J. Biomechanical testing of commercially available soft-tissue augmentation materials. Arthroscopy. 2009;25:1233-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Jones CR, Snyder SJ. Massive Irreparable Rotator Cuff Tears: A Solution That Bridges the Gap. Sports Med Arthrosc Rev. 2015;23:130-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | EU Hernia Trialists Collaboration. Repair of groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg. 2002;235:322-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 271] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 13. | Ciampi P, Scotti C, Nonis A, Vitali M, Di Serio C, Peretti GM, Fraschini G. The benefit of synthetic versus biological patch augmentation in the repair of posterosuperior massive rotator cuff tears: a 3-year follow-up study. Am J Sports Med. 2014;42:1169-1175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 149] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 14. | Steinhaus ME, Makhni EC, Cole BJ, Romeo AA, Verma NN. Outcomes After Patch Use in Rotator Cuff Repair. Arthroscopy. 2016;32:1676-1690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 15. | Derwin KA, Badylak SF, Steinmann SP, Iannotti JP. Extracellular matrix scaffold devices for rotator cuff repair. J Shoulder Elbow Surg. 2010;19:467-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 150] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 16. | Mihata T, Bui CNH, Akeda M, Cavagnaro MA, Kuenzler M, Peterson AB, McGarry MH, Itami Y, Limpisvasti O, Neo M, Lee TQ. A biomechanical cadaveric study comparing superior capsule reconstruction using fascia lata allograft with human dermal allograft for irreparable rotator cuff tear. J Shoulder Elbow Surg. 2017;26:2158-2166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 157] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 17. | Malcarney HL, Bonar F, Murrell GA. Early inflammatory reaction after rotator cuff repair with a porcine small intestine submucosal implant: a report of 4 cases. Am J Sports Med. 2005;33:907-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 134] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 18. | Burkhart SS. A stepwise approach to arthroscopic rotator cuff repair based on biomechanical principles. Arthroscopy. 2000;16:82-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 179] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 19. | Mall NA, Lee AS, Chahal J, Van Thiel GS, Romeo AA, Verma NN, Cole BJ. Transosseous-equivalent rotator cuff repair: a systematic review on the biomechanical importance of tying the medial row. Arthroscopy. 2013;29:377-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 20. | McCarron JA, Milks RA, Mesiha M, Aurora A, Walker E, Iannotti JP, Derwin KA. Reinforced fascia patch limits cyclic gapping of rotator cuff repairs in a human cadaveric model. J Shoulder Elbow Surg. 2012;21:1680-1686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 21. | Burkhart SS, Diaz Pagàn JL, Wirth MA, Athanasiou KA. Cyclic loading of anchor-based rotator cuff repairs: confirmation of the tension overload phenomenon and comparison of suture anchor fixation with transosseous fixation. Arthroscopy. 1997;13:720-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 288] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 22. | Killian ML, Cavinatto L, Shah SA, Sato EJ, Ward SR, Havlioglu N, Galatz LM, Thomopoulos S. The effects of chronic unloading and gap formation on tendon-to-bone healing in a rat model of massive rotator cuff tears. J Orthop Res. 2014;32:439-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Nada AN, Debnath UK, Robinson DA, Jordan C. Treatment of massive rotator-cuff tears with a polyester ligament (Dacron) augmentation: clinical outcome. J Bone Joint Surg Br. 2010;92:1397-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 24. | Petrie MJ, Ismaiel AH. Treatment of massive rotator-cuff tears with a polyester ligament (LARS) patch. Acta Orthop Belg 2013; 79: 620-625. |
| 25. | Audenaert E, Van Nuffel J, Schepens A, Verhelst M, Verdonk R. Reconstruction of massive rotator cuff lesions with a synthetic interposition graft: a prospective study of 41 patients. Knee Surg Sports Traumatol Arthrosc. 2006;14:360-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 114] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 26. | Hirooka A, Yoneda M, Wakaitani S, Isaka Y, Hayashida K, Fukushima S, Okamura K. Augmentation with a Gore-Tex patch for repair of large rotator cuff tears that cannot be sutured. J Orthop Sci. 2002;7:451-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 70] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Kholinne E, Kwak JM, Kim H, Koh KH, Jeon IH. Arthroscopic Superior Capsular Reconstruction With Mesh Augmentation for the Treatment of Irreparable Rotator Cuff Tears: A Comparative Study of Surgical Outcomes. Am J Sports Med. 2020;48:3328-3338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 28. | Cevasco M, Itani KM. Ventral hernia repair with synthetic, composite, and biologic mesh: characteristics, indications, and infection profile. Surg Infect (Larchmt). 2012;13:209-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 84] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 29. | Morris-Stiff GJ, Hughes LE. The outcomes of nonabsorbable mesh placed within the abdominal cavity: literature review and clinical experience. J Am Coll Surg. 1998;186:352-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 190] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 30. | Wu F, Zhang X, Liu Y, Cao D, Yu Y, Ma Y. Lightweight mesh versus heavyweight mesh for laparo-endoscopic inguinal hernia repair: a systematic review and meta-analysis. Hernia. 2020;24:31-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Santoni BG, McGilvray KC, Lyons AS, Bansal M, Turner AS, Macgillivray JD, Coleman SH, Puttlitz CM. Biomechanical analysis of an ovine rotator cuff repair via porous patch augmentation in a chronic rupture model. Am J Sports Med. 2010;38:679-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |