Published online May 18, 2023. doi: 10.5312/wjo.v14.i5.268
Peer-review started: December 26, 2022
First decision: January 20, 2023
Revised: January 24, 2023
Accepted: April 6, 2023
Article in press: April 6, 2023
Published online: May 18, 2023
Processing time: 142 Days and 20.8 Hours
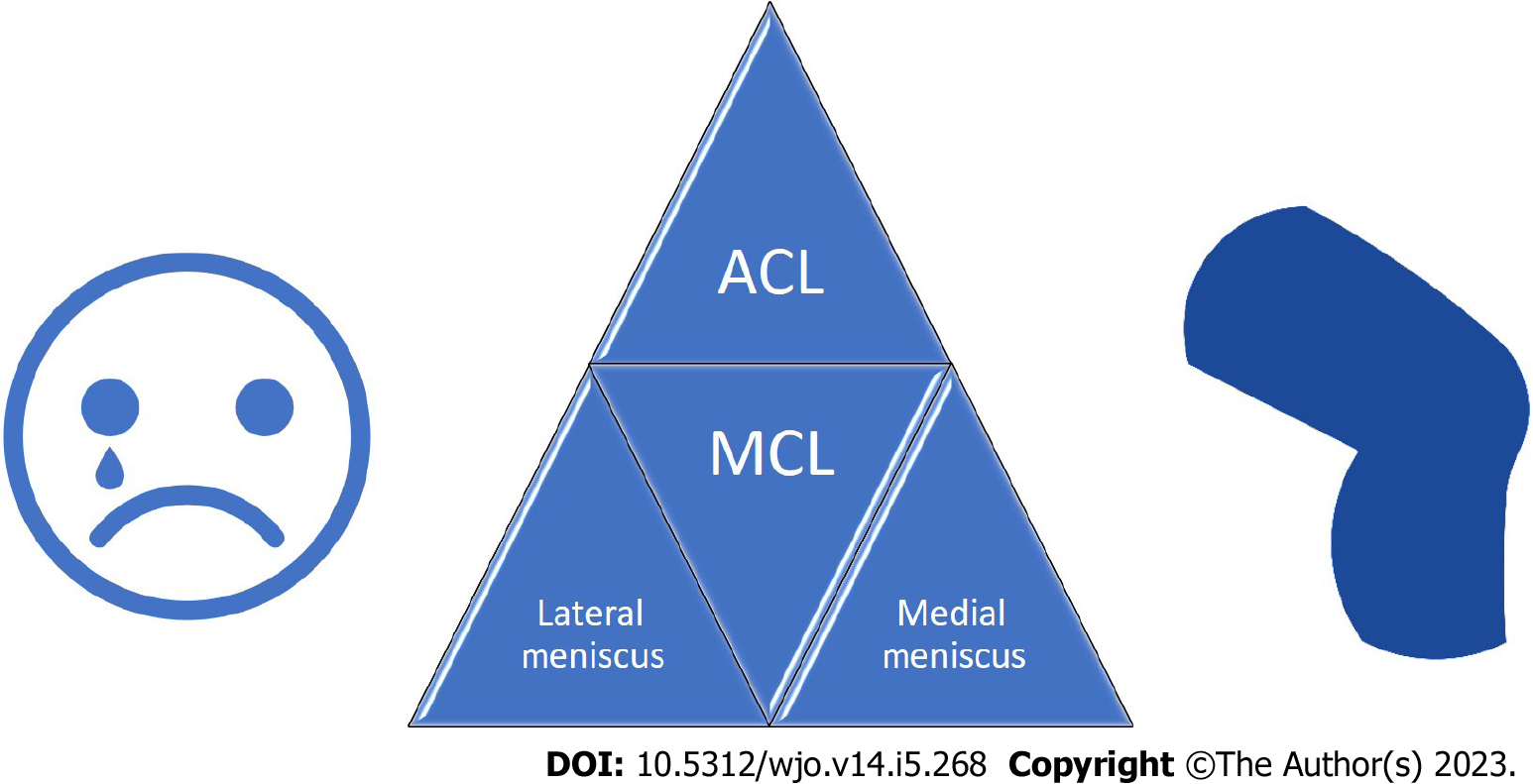
The association between injuries to the anterior cruciate ligament, medial collateral ligament, and medial meniscus (MM) has been known to orthopedic surgeons since 1936; O'Donoghue first used the term "unhappy triad" of the knee to describe this condition in 1950. Later studies revealed that involvement of the lateral meniscus is more common than MM in these cases, leading to a change in the definition. Recent studies have revealed that this triad may be primarily linked to knee anterolateral complex injuries. Although there is not a definite management protocol for this triad, we try to mention the most recent concepts about it in addition to expert opinions.
Core Tip: Traditionally, the anterior cruciate ligament (ACL), medial collateral ligament (MCL), and medial meniscus (MM) were thought to be the unhappy triad of the knee; however, lateral meniscus injuries are thought to be more common in association with ACL and MCL tears. Clinicians, radiologists, and orthopedic surgeons should be aware of the unhappy triad of the knee, while performing physical examinations, radiologic assessments, or knee arthroscopy. MCL spontaneous healing is possible in some cases with lower grades of tear; however, consideration of patient knee alignment and accuracy in MCL size for non-operative treatment decision-making is critical.
- Citation: Hoveidaei AH, Sattarpour R, Dadgostar H, Razi S, Razi M. Unhappy triad of the knee: What are the current concepts and opinions? World J Orthop 2023; 14(5): 268-274
- URL: https://www.wjgnet.com/2218-5836/full/v14/i5/268.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i5.268
Campbell first described a "combination" knee injury in 1936[1], which included injury to the anterior cruciate ligament (ACL), medial collateral ligament (MCL), and medial meniscus (MM), but the term "unhappy triad" was not used until O'Donoghue (1950) reported that about a quarter of all acute athletic knee injuries involve damage to the ACL, MCL, and MM. The MM was initially suspected as the main site of injury compared with lateral meniscal (LM) tears, and O'Donoghue found that only 3% of his sample of 33 patients had LM injuries[2,3]. However, arthroscopy studies showing the higher prevalence of LM tears shifted this dominance[4-6]. The definition of "medial meniscus injury" might have been misunderstood. Perhaps what O'Donoghue considered a MM injury was actually a capsular injury[7].
Extreme reflectoric muscle contractions brought on by rotational stress may result in chondromalacic lesions in the femoro-patellar joint, expanding the "unhappy triad" syndrome into the "unhappy tetrad[8]. According to Müller et al[9], the fourth component of this tetrad is antero-lateral femoro-tibial ligament lesions. These are the distal posterior portions of the iliotibial tract that pass from the linea aspra to Gerdy's tubercle[10]. The jerk test, a type of pivot-shift test, can be used to assess anterolateral rotatory instability[11], and magnetic resonance imaging (MRI) has been shown to be useful[12]. According to some studies, anterolateral ligament abnormalities can increase the risk of a complete ACL tear and collateral ligament injuries[13,14]. Nonetheless, the MM is intact in these patients[15].
The injury pattern in the lateral compartment is usually stretching and hemorrhage of the anterolateral capsule; Segond's fracture is less reported[10]. Ferretti et al[16] reported anterolateral capsule and ligament injuries in isolated ACL injuries. They also announced a new classification for this type of injury: Type I (stretching and bleeding in the anterolateral capsule alone), type II (stretching and bleeding from the front to the back), type III (complete tear of the anterolateral ligament [ALL]), and type IV (bone avulsion and Segond's fracture).
Recent studies have focused on the anterolateral femur-tibial ligament as a stabilizer of the knee's internal rotation and pivotal shift[17-19]. So, repairing these ligament injuries could help people who are getting their ACLs reconstructed.
Grading of MCL injuries is based on joint space widening by applying a valgus force on a 0-30° flexed knee[11,20,21]. Seventy-eight percent of MCL grade III injuries are associated with ACL injuries[22]. Shebourne and Posch proposed that parallel meniscus injuries have a relatively protective effect for higher-grade injuries[20,21].
In general, we can conclude that this triad should be defined as concomitant ACL, MCL, and MM/LM injuries, mostly associated with the anterolateral complex of the knee (Figure 1).
O'Donoghue reported an incidence as high as 25% of the "unhappy triad" in acute athletic knee injuries, and in a study of 22 patients with combined ACL and MCL injuries, it was found that 17 (or 77%) of them had an associated MM tear. However, later studies showed more dominant LM injuries. Shelbourne et al[23] found a 32-71% prevalence of LM injury while finding significantly lower rates of MM injury, even 0% in one of their study groups. The mechanism of injury in the unhappy knee triad is sudden valgus impact with external or internal rotation[16]. However, it is controversial whether the MCL or ACL is injured first[24,25].
This triad often occurs in contact and non-contact sports such as netball, basketball, soccer, skiing, and rugby[26,27]. A recent study, for example, discovered that the ACL was involved in all skiers' knee injuries[21], contrary to the popular belief about the MCL's dominance[28].
Immediately after trauma, the "unhappy triad" is observed. Swelling, hemorrhage, and serous effusion form after hours and accompany the meniscal and ligament injuries. However, in disrupted capsular injuries, effusion can be negated[29]. There is pain, impaired muscle control, edema, and reflex muscle inhibition in the acute phase. Through an accurate history and physical examination, we can determine injured structures. When rotating on a fixed knee, the majority of patients reported hearing a snapping click noise. Physical examinations, usually the Lachman test, pivot shift test, anterior drawer test, and valgus stress test, are positive, and patients have localized tenderness through the MCL[10,30]. Some patients have patellar instability because of a concomitant injury to the medial patellofemoral ligament and a superficial part of the MCL[27].
X-ray images are not used often because of their low input except for insertion site bone avulsions and lower limb alignment. Using valgus stress X-ray, we can classify injuries into complete medial side tears and isolated high-grade MCL injuries by measuring the opening of medial tears[31]. Valgus stress X-ray results depend on patients' pain and muscular relaxation and could not be accurate in patients with higher degrees of immobility[32]. MRI and arthroscopy are considered accurate diagnostic tools for ACL injuries (around 90% sensitivity), but a blind arthroscopic approach could result in inappropriate treatment for 35% of patients[33,34]. We can use MRI to detect medial side and meniscus injuries, as well as cartilage injuries. As said, lateral side bruises and MRI findings can indicate a higher grade of injury in the medial compartment[27].
Most cases require surgery and a recovery period of 6 to 9 mo. Reconstruction and repair of the ALL lesions should be considered to improve the control of rotational stability and future knee kinematics scores provided by ACL reconstruction. For high-risk patients, a combined ACL and ALL reconstruction improves rotational control and reduces the rate of re-rupture without increasing postoperative complication rates compared to an ACL-only reconstruction[35-39]. However, it needs further investigation for different degrees of injury[39,40]. Another important aspect of surgery is determining whether we can choose a conservative approach for MCL injuries in patients with an unhappy triad (tetrad). Treatment of MCL injuries evolved from an aggressive surgical approach[5,41] around 1960 to non-operative MCL treatment and early range of motion regarding the extra-articular healing ability of the MCL[42,43]. This healing potential is because of the enriched blood supply of the medial compartment of the knee. The Hughston grading system can be used to classify MCL injuries: Applying valgus stress opening in MCL tears between 1 and 5 mm is considered grade I; between 5 and 10 mm is considered grade II; and more than 10 mm is considered grade III[44]. In the original Hughston grading system, grades I and II injuries are named after incomplete MCL injuries, which are not present in the unhappy triad (tetrad). Several studies have highlighted that non-operative and operative managements of MCL injuries have similar satisfactory results, but these patients only had ACL injuries parallel to the MCL[27,45-47]. Patients with the unhappy knee triad (tetrad) with grades I and II MCL injuries can be treated conservatively (using injections and physiotherapy) with a delay in ACL reconstruction, allowing the MCL to heal by itself[48]. It is essential to note that early range of motion is recommended because of better collagen organization and healing outcomes[49]. Grade III injuries and competitive athletes are better treated surgically because of the risk of future ACL reconstruction failure, knee osteoarthritis, which has an increasing burden, and valgus knee instability[50,51]. The reason may be the disruption of menisco-tibial and menisco-femoral attachments during injuries involving deeper layers of the medial compartment (deep MCL). Even so, some studies show satisfactory outcomes in the non-operative management of isolated MCL grade III injuries, but confounding factors such as parallel ACL and meniscal injuries are not considered[52,53]. Meniscus repair is the other consideration that surgeons need to address. The MM is usually repaired because of its role in knee stability and protective effect on osteoarthritis[54].
The unhappy triad can cause osteoarthritis in 50% of patients in 10-20 years due to intra-articular processes initiated by injury. Also, MCL injuries can cause long-term knee instability and increase susceptibility to meniscus injuries[26,55]. The osteoarthritis risk is not covered by anyone, with its pain and function impairment playing a major role in these patients, but the most important question is its rate in these patients and treatment outcomes. In Lundberg's study, 13% of patients with MCL injuries treated non-operatively showed radiographic signs of osteoarthritis[56]. Ochiai et al[57] found that in patients with injuries to the ACL, MCL, and LM, reconstruction of the ACL with or without the MCL and LM significantly improved the outcome. However, scores were higher in the group with a conservative approach to MCL. Physiotherapy, early range of motion, and limited weight bearing after reconstruction can improve knee mobility[58]. Using knee braces in high-grade injuries can help keep the knee in correct healing alignment, but it needs further study for long-term outcomes[59].
Even with recent studies, choosing between the conservative and operative approaches remains controversial among clinicians. In some cases, spontaneous healing of the MCL occurs without a surgical intervention[60]. Using some expert recommendations, we propose that patients with the unhappy triad of the knee who have varus alignment in the physical examination could undergo a conservative approach, meaning MCL non-operative treatment and ACL reconstruction surgery. These patients should be observed for complications like patellofemoral subluxation and pain. Although some previous studies have mentioned that low grade MCL tearing may not require surgical intervention, considering the fact that MCL tear size estimation without performing arthroscopy may not be accurate, we recommend operative treatment in patients with valgus and normal alignments.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Iran
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hamoongard M, Iran; Wang H, China S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Zhao S
| 1. | Campbell WC. Repair of ligaments of the knee, report of a new operation for repair of the anterior crucial ligament. Surg Gvneeo/Oh Stet. 1936;62:8. |
| 2. | Cerabona F, Sherman MF, Bonamo JR, Sklar J. Patterns of meniscal injury with acute anterior cruciate ligament tears. Am J Sports Med. 1988;16:603-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 75] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 3. | Strong MJ, Grace GM, Freedman M, Lomen-Hoerth C, Woolley S, Goldstein LH, Murphy J, Shoesmith C, Rosenfeld J, Leigh PN, Bruijn L, Ince P, Figlewicz D. Consensus criteria for the diagnosis of frontotemporal cognitive and behavioural syndromes in amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2009;10:131-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 424] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 4. | DeHaven KE. Diagnosis of acute knee injuries with hemarthrosis. Am J Sports Med. 1980;8:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 242] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Hughston JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am. 1994;76:1328-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 121] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Nikolaou PK, Seaber AV, Glisson RR, Ribbeck BM, Bassett FH 3rd. Anterior cruciate ligament allograft transplantation. Long-term function, histology, revascularization, and operative technique. Am J Sports Med. 1986;14:348-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 135] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Shiwaku K, Kamiya T, Suzuki D, Yamakawa S, Otsubo H, Suzuki T, Takahashi K, Okada Y, Teramoto A, Ohnishi H, Fujie H, Yamashita T. The Role of the Medial Meniscus in Anterior Knee Stability. Orthop J Sports Med. 2022;10:23259671221132845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Schmitt O, Mittelmeier H. [The biomechanical significance of the vastus medialis and lateralis muscles (author's transl)]. Arch Orthop Trauma Surg (1978). 1978;91:291-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Müller W. The knee: form, function, and ligament reconstruction. (e-pub ahead of print 1983). [DOI] [Full Text] |
| 10. | Ferretti A, Monaco E, Ponzo A, Dagget M, Guzzini M, Mazza D, Redler A, Conteduca F. The unhappy triad of the knee re-revisited. Int Orthop. 2019;43:223-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | McCluskey G, Blackburn TA. Classification of knee ligament instabilities. Phys Ther. 1980;60:1575-1577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Helito PVP, Helito CP, Rodrigues MB. Anterolateral ligament MRI of the knee in ACL injuries: MRI abnormalities association with instability. Eur Radiol. 2023;33:1456-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Song Y, Yang JH, Choi WR, Lee JK. Magnetic Resonance Imaging-Based Prevalence of Anterolateral Ligament Abnormalities and Associated Injuries in Knees with Acute Anterior Cruciate Ligament Injury. J Knee Surg. 2019;32:866-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Helito CP, Helito PVP, Leão RV, Demange MK, Bordalo-Rodrigues M. Anterolateral ligament abnormalities are associated with peripheral ligament and osseous injuries in acute ruptures of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2017;25:1140-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 15. | Helito CP, Helito PVP, Assirati LFB, Longo CH, Bordalo-Rodrigues M, Souza FF. Magnetic Resonance Imaging Evaluation of the Anterolateral Ligament in Acute Anterior Cruciate Ligament Injuries in an Adolescent Population. Arthroscopy. 2019;35:2136-2142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Ferretti A, Monaco E, Fabbri M, Maestri B, De Carli A. Prevalence and Classification of Injuries of Anterolateral Complex in Acute Anterior Cruciate Ligament Tears. Arthroscopy. 2017;33:147-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 142] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 17. | Imbert P, Lutz C, Daggett M, Niglis L, Freychet B, Dalmay F, Sonnery-Cottet B. Isometric Characteristics of the Anterolateral Ligament of the Knee: A Cadaveric Navigation Study. Arthroscopy. 2016;32:2017-2024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 74] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 18. | Rasmussen MT, Nitri M, Williams BT, Moulton SG, Cruz RS, Dornan GJ, Goldsmith MT, LaPrade RF. An In Vitro Robotic Assessment of the Anterolateral Ligament, Part 1: Secondary Role of the Anterolateral Ligament in the Setting of an Anterior Cruciate Ligament Injury. Am J Sports Med. 2016;44:585-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 205] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 19. | Sonnery-Cottet B, Lutz C, Daggett M, Dalmay F, Freychet B, Niglis L, Imbert P. The Involvement of the Anterolateral Ligament in Rotational Control of the Knee. Am J Sports Med. 2016;44:1209-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 174] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 20. | Shelbourne KD, Patel DV. "Management of combined injuries of the anterior cruciate and medial collateral ligaments." JBJS 1995; 77: 800-806. [DOI] [Full Text] |
| 21. | Posch M, Schranz A, Lener M, Tecklenburg K, Burtscher M, Ruedl G. In recreational alpine skiing, the ACL is predominantly injured in all knee injuries needing hospitalisation. Knee Surg Sports Traumatol Arthrosc. 2021;29:1790-1796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 22. | Halinen J, Lindahl J, Hirvensalo E, Santavirta S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med. 2006;34:1134-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 134] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 23. | Shelbourne KD, Nitz PA. The O'Donoghue triad revisited. Combined knee injuries involving anterior cruciate and medial collateral ligament tears. Am J Sports Med. 1991;19:474-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 87] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 24. | Koga H, Bahr R, Myklebust G, Engebretsen L, Grund T, Krosshaug T. Estimating anterior tibial translation from model-based image-matching of a noncontact anterior cruciate ligament injury in professional football: a case report. Clin J Sport Med. 2011;21:271-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 25. | Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32:1002-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 821] [Cited by in RCA: 804] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 26. | Dacombe PJ. Shelbourne's update of the O'Donoghue knee triad in a 17-year-old male Rugby player. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Bollier M, Smith PA. Anterior cruciate ligament and medial collateral ligament injuries. J Knee Surg. 2014;27:359-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 28. | Warme WJ, Feagin JA Jr, King P, Lambert KL, Cunningham RR. Ski injury statistics, 1982 to 1993, Jackson Hole Ski Resort. Am J Sports Med. 1995;23:597-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 72] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Indelicato PA. Isolated Medial Collateral Ligament Injuries in the Knee. J Am Acad Orthop Surg. 1995;3:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 74] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 30. | Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part I. The medial compartment and cruciate liga-ments. JBJS. 1976;58:159-172. [RCA] [DOI] [Full Text] [Cited by in Crossref: 590] [Cited by in RCA: 452] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 31. | Laprade RF, Bernhardson AS, Griffith CJ, Macalena JA, Wijdicks CA. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med. 2010;38:330-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 125] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 32. | James EW, Williams BT, LaPrade RF. Stress radiography for the diagnosis of knee ligament injuries: a systematic review. Clin Orthop Relat Res. 2014;472:2644-2657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 112] [Cited by in RCA: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 33. | Miller GK. A prospective study comparing the accuracy of the clinical diagnosis of meniscus tear with magnetic resonance imaging and its effect on clinical outcome. Arthroscopy. 1996;12:406-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 34. | Jackson DW, Jennings LD, Maywood RM, Berger PE. Magnetic resonance imaging of the knee. Am J Sports Med. 1988;16:29-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 97] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 35. | Neri T, Dabirrahmani D, Beach A, Grasso S, Putnis S, Oshima T, Cadman J, Devitt B, Coolican M, Fritsch B, Appleyard R, Parker D. Different anterolateral procedures have variable impact on knee kinematics and stability when performed in combination with anterior cruciate ligament reconstruction. J ISAKOS. 2021;6:74-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 36. | Inderhaug E, Stephen JM, Williams A, Amis AA. Biomechanical Comparison of Anterolateral Procedures Combined With Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2017;45:347-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 204] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 37. | Geeslin AG, Moatshe G, Chahla J, Kruckeberg BM, Muckenhirn KJ, Dornan GJ, Coggins A, Brady AW, Getgood AM, Godin JA, LaPrade RF. Anterolateral Knee Extra-articular Stabilizers: A Robotic Study Comparing Anterolateral Ligament Reconstruction and Modified Lemaire Lateral Extra-articular Tenodesis. Am J Sports Med. 2018;46:607-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 143] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 38. | Sonnery-Cottet B, Daggett M, Fayard JM, Ferretti A, Helito CP, Lind M, Monaco E, de Pádua VBC, Thaunat M, Wilson A, Zaffagnini S, Zijl J, Claes S. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament - deficient knee. J Orthop Traumatol. 2017;18:91-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 189] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 39. | Devitt BM, Bell SW, Ardern CL, Hartwig T, Porter TJ, Feller JA, Webster KE. The Role of Lateral Extra-articular Tenodesis in Primary Anterior Cruciate Ligament Reconstruction: A Systematic Review With Meta-analysis and Best-Evidence Synthesis. Orthop J Sports Med. 2017;5:2325967117731767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 40. | Pontoh LA, Dilogo IH, Kamal AF, Widodo W, Kholinne E, Rhatomy S, Fiolin J. Double-bundle ACL reconstruction versus anatomic single-bundle ACL reconstruction combined with anterolateral ligament reconstruction: a comparative study of clinical outcome. Eur J Orthop Surg Traumatol. 2023;33:489-495. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 41. | Hughston JC. A surgical approach to the medial and posterior ligaments of the knee. Clin Orthop Relat Res. 1973;29-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Ballmer PM, Jakob RP. The non operative treatment of isolated complete tears of the medial collateral ligament of the knee. A prospective study. Arch Orthop Trauma Surg (1978). 1988;107:273-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 97] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 43. | Ellsasser JC, Reynolds FC, Omohundro JR. The non-operative treatment of collateral ligament injuries of the knee in professional football players. An analysis of seventy-four injuries treated non-operatively and twenty-four injuries treated surgically. J Bone Joint Surg Am. 1974;56:1185-1190. [PubMed] |
| 44. | Phisitkul P, James SL, Wolf BR, Amendola A. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006;26:77-90. [PubMed] |
| 45. | Zhang H, Sun Y, Han X, Wang Y, Wang L, Alquhali A, Bai X. Simultaneous Reconstruction of the Anterior Cruciate Ligament and Medial Collateral Ligament in Patients With Chronic ACL-MCL Lesions: A Minimum 2-Year Follow-up Study. Am J Sports Med. 2014;42:1675-1681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 46. | Grant JA, Tannenbaum E, Miller BS, Bedi A. Treatment of combined complete tears of the anterior cruciate and medial collateral ligaments. Arthroscopy. 2012;28:110-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 47. | Hara K, Niga S, Ikeda H, Cho S, Muneta T. Isolated anterior cruciate ligament reconstruction in patients with chronic anterior cruciate ligament insufficiency combined with grade II valgus laxity. Am J Sports Med. 2008;36:333-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 48. | Ferretti A, Mazza D. "The Unhappy Triad Revisited." Anterolateral Rotatory Instability in ACL Deficient Knee. Cham: Springer International Publishing, 2022; 57-69. [DOI] [Full Text] |
| 49. | Woo SL, Vogrin TM, Abramowitch SD. Healing and repair of ligament injuries in the knee. J Am Acad Orthop Surg. 2000;8:364-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 116] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 50. | Narvani A, Mahmud T, Lavelle J, Williams A. Injury to the proximal deep medial collateral ligament: a problematical subgroup of injuries. J Bone Joint Surg Br. 2010;92:949-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 51. | Hoveidaei AH, Nakhostin-Ansari A, Chalian M, Roshanshad A, Khonji MS, Mashhadiagha A, Pooyan A, Citak M. Burden of knee osteoarthritis in the Middle East and North Africa (MENA): an epidemiological analysis from 1990 to 2019. Arch Orthop Trauma Surg. Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 52. | Reider B, Sathy MR, Talkington J, Blyznak N, Kollias S. Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation. A five-year follow-up study. Am J Sports Med. 1994;22:470-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 96] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 53. | Kannus P. Long-term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop Relat Res. 1988;103-112. [PubMed] |
| 54. | Andrews K, Lu A, Mckean L, Ebraheim N. Review: Medial collateral ligament injuries. J Orthop. 2017;14:550-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 55. | Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756-1769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1542] [Cited by in RCA: 1592] [Article Influence: 88.4] [Reference Citation Analysis (0)] |
| 56. | Lundberg M, Messner K. Long-term prognosis of isolated partial medial collateral ligament ruptures. A ten-year clinical and radiographic evaluation of a prospectively observed group of patients. Am J Sports Med. 1996;24:160-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 49] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 57. | Ochiai S, Hagino T, Senga S, Yamashita T, Ando T, Taniguchi N, Haro H. Analysis of Health-Related Quality of Life and Clinical Evaluations in Patients with the Triad of Combined Knee Injuries. J Knee Surg. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 58. | Gramatikova M, Petrov B, Pacheva P, Gramatikova V. The Historical development of Bektashism in Bulgaria. [DOI] [Full Text] |
| 59. | Cinque ME, Chahla J, Kruckeberg BM, DePhillipo NN, Moatshe G, LaPrade RF. Posteromedial Corner Knee Injuries: Diagnosis, Management, and Outcomes: A Critical Analysis Review. JBJS Rev. 2017;5:e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 60. | Razi M, Soufali AP, Ziabari EZ, Dadgostar H, Askari A, Arasteh P. Treatment of Concomitant ACL and MCL Injuries: Spontaneous Healing of Complete ACL and MCL Tears. J Knee Surg. 2021;34:1329-1336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |