Published online Apr 18, 2023. doi: 10.5312/wjo.v14.i4.248
Peer-review started: November 28, 2022
First decision: January 20, 2023
Revised: February 4, 2023
Accepted: April 4, 2023
Article in press: April 4, 2023
Published online: April 18, 2023
Processing time: 140 Days and 20.1 Hours
Advances in minimally invasive surgery and improved post-operative pain management make it possible to consider performing even major foot/ankle operations as day-case. This could have significant benefits for patients and the health service. However there are theoretical concerns about post-operative complications and patient satisfaction due to pain.
To scope the current practice of foot and ankle surgeons on day-case surgery for major foot and ankle procedures in the United Kingdom (UK).
An online survey (19 questions) was sent to UK foot and ankle surgeons via the British Orthopaedic Foot & Ankle Society membership list in August 2021. Major foot and ankle procedures were defined as surgery that is usually performed as an inpatient in majority of centres and day-case as same day discharge, with day surgery as the intended treatment pathway.
132 people responded to the survey invitation with 80% working in Acute NHS Trusts. Currently 45% of respondents perform less than 100 day-case surgeries per year for these procedures. 78% felt that there was scope to perform more procedures as day-case at their centre. Post-operative pain (34%) and patient satisfaction (10%) was not highly measured within their centres. Lack of adequate physiotherapy input pre/post-operatively (23%) and lack of out of hours support (21%) were the top perceived barriers to performing more major foot and ankle procedures as day-case.
There is consensus among UK surgeons to do more major foot/ankle procedures as day-case. Out of hours support and physiotherapy input pre/ post-op were perceived as the main barriers. Despite theoretical concerns about post-operative pain and satisfaction this was only measured by a third of those surveyed. There is a need for nationally agreed protocols to optimise the delivery of and measurement of outcomes in this type of surgery. At a local level, the provision of physiotherapy and out of hours support should be explored at sites where this is a perceived barrier.
Core Tip: We have identified an appetite to increase the number of major foot and ankle procedures within United Kingdom foot and ankle surgeons who completed our survey. Despite theoretical concerns about post-operative pain and satisfaction this was only measured by a third of those surveyed. Out of hours support and physiotherapy input pre/post-op were perceived as the main barriers to doing day-case surgery in foot and ankle surgery.
- Citation: Berry A, Houchen-Wolloff L, Crane N, Townshend D, Clayton R, Mangwani J. Perceived barriers and facilitators of day-case surgery for major foot and ankle procedures? A cross-sectional survey of United Kingdom surgeons. World J Orthop 2023; 14(4): 248-259
- URL: https://www.wjgnet.com/2218-5836/full/v14/i4/248.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i4.248
Day-case surgery is defined as surgery performed where the patient is undergoing a planned procedure, where day surgery is the intended management plan and the patient is admitted, operated upon and discharged on the same day[1]. Day-case surgery brings recognised benefits for both patients and the healthcare system in relation to patient quality and experience, reduced bed days and significant financial savings[2]. The British Association of Day Surgery (BADS) is a multidisciplinary professional organisation which promotes day surgery by setting standards for day surgery and has developed national benchmarking for day surgery performance[1]. The Academy of Medical Royal colleges also strongly recommended that patients be given the option of day surgery wherever possible and guidelines have been produced to this effect[3]. This guideline has helped to increase the number of day-case surgeries performed. Their recommendations are aimed at surgeons and anaesthetists to offer updated guidance on changes within day surgery and how they may implement these within their practice. These were to offer guidance on day/short-stay surgery, including: The selection of patients; Social, medical and surgical factors in day-case surgery; Pre-operative preparation; Urgent cases; Management and staffing; Postoperative recovery and discharge.
There are many factors in choosing these surgeries to be inpatient or day-case such as the injury sustained, patient health and social circumstances, hospital bed availability, hospital protocols, surgical team, anaesthesia protocol etc[4]. There is disparity across the UK in day-case provision. In terms of orthopaedic procedures, some hip and knee surgeries are commonly performed as day-case and are effective, safe and cost-saving[5-7]. The most recent figures from Model Health System (NHS England) for the proportion of all admissions for trusts that were day-cases for all procedures was 69% (in this quartile July 2022 data based on the latest 3 months of activity with primary total replacements of hips/knees excluded from the total). For orthopaedic surgery this day-case rate was 78% (NHS England Model Health System, July 2022). However there are only 3 procedures listed within the BADS day-case directory of procedures (January 2022[1]) for foot and ankle day-case surgery (bunion operation, open reduction and fixation of ankle, lengthening/ shortening of tendons). Therefore day-case rates for foot and ankle procedures are low.
Major foot and ankle surgery in the UK is usually carried out as an inpatient due to the complexity of surgery, pain post-surgery requiring opiates and ongoing observations required[8]. Major foot and ankle procedure include ankle and hindfoot fusion, joint replacements and tendon repair[9]. However in many cases, day-case surgery can be highly satisfactory for patients and providers in major foot and ankle cases in adults[9] and children[10]. Day-case foot and ankle surgery is known to be safe for the patient with high satisfaction rates as well as being cost effective for the service[11]. There is recent evidence showing there were little to no differences in complication rates or readmissions following foot/ankle surgeries (total ankle replacements, ankle fractures, total ankle arthroplasty and hindfoot fusions) that were performed as day-case vs inpatient[12-17]. However there are no specific guidelines for foot and ankle day-case surgery.
As previously outlined, there is evidence to suggest there are benefits to performing foot and ankle surgeries as day-case over inpatient procedures as well as guidance on performing surgeries as day-case. However there is a gap within the literature around what are the perceived barriers and facilitators to performing major foot and ankle surgeries as day-case and no specific guidelines for foot and ankle day-case surgery. The aim of this survey therefore was to scope the current practice of UK foot and ankle surgeons in terms of perceived barriers and facilitators to performing day-case surgery for major foot/ankle procedures.
A cross-sectional survey (Table 1) consisting of 19 questions was created using the online platform SurveyMonkey. The questionnaire was designed following a qualitative synthesis of published literature. The questions were broken into 3 separate categories to evaluate: current practices and protocols, pre-operative and post-operative management and what are the perceived barriers and facilitators of performing major foot and ankle surgeries as day-case.
| Question 1 |
| What is your occupation? |
| Open-response |
| Question 2 |
| In what setting do you work? Select all that apply |
| Acute NHS Trust -specialist foot and ankle unit |
| Acute NHS Trust – non specialist foot and ankle unit |
| District General Hospital |
| Community care |
| Private practice |
| Question 3 |
| Please estimate the number of major foot and ankle procedures that your primary centre performs in 1 calendar year |
| Less than 20 |
| 20-50 |
| 50-75 |
| 75-100 |
| 100-200 |
| 200-500 |
| 500-1000 |
| Over 1000 |
| Don't know |
| Question 4 |
| Please estimate what percentage of these major ankle and hindfoot procedures are performed as day case procedures |
| Open response |
| Question 5 |
| Do you think there is potential for more of these cases to be done as day case in your own unit? |
| Yes |
| No |
| Question 6 |
| Do you follow a protocol for day case procedures? |
| Yes- national |
| Yes- local |
| No |
| Unsure |
| Question 7 |
| If you follow a national protocol for day case surgery, please state which one |
| Open-response |
| Question 8 |
| Which type of anaesthesia do you offer for day case procedures? Tick all that apply |
| Don't know |
| Regional |
| General |
| Combination of GA and regional |
| Specific blocks |
| Question 9 |
| If you use blocks, please state which |
| Open-response |
| Question 10 |
| Do you routinely discharge day case patients with opiate/controlled drugs such as oxycodone/oromorph? |
| Yes |
| No |
| Unsure |
| Question 11 |
| What post-op analgesia do you offer for day case procedures? Tick all that apply |
| Don't know |
| Amitriptyline |
| Gabapentin |
| Ibuprofen |
| Paracetamol |
| Codeine |
| Other: Please state |
| Question 12 |
| Are all patients seen by physiotherapy pre-op for walking aid/ weight bearing instruction and education? |
| Yes |
| No |
| Unsure |
| Question 13 |
| Are all patients seen by physiotherapist post-op (before discharge) for walking aid instruction and education? |
| Yes |
| No |
| Unsure |
| Question 14 |
| Is a post-op phone call/email/text message made to the patient? |
| Yes |
| No |
| Unsure |
| Question 15 |
| If yes who provides this contact? |
| Open-Response |
| Question 16 |
| Which outcome measures are recorded for day-case patients? Tick all that apply |
| pain levels using Visual Analogue Score (VAS) |
| patient satisfaction, please state which measure |
| complication rate and type |
| MOX-FQ |
| EQ-5D |
| Other (please specify) |
| Question 17 |
| What are the barriers for day case surgery for major foot and ankle procedures in your unit? |
| No provision of physiotherapist out of hours |
| No anaesthetist to perform peripheral nerve blocks |
| Lack of managerial support |
| Out of hours support/ point of contact for patients not available |
| Never done it before |
| No physiotherapy input at pre-assessment |
| Other: Please state |
| Question 18 |
| Which complications have you witnessed or heard about in major foot and ankle procedures done as a day case? Tick all that apply |
| Wound healing problems |
| Wound infection |
| Breakthrough pain |
| Patient dissatisfaction |
| Unplanned readmission |
| Need for further surgery |
| Delayed/non-union |
| Other, please state |
| Question 19 |
| When and how are patients first re-evaluated after discharge? Tick all that apply for |
| 24 h face to face |
| 24 h telephone call |
| 1 wk face to face |
| 1 wk telephone call |
| 2 wk face to face |
| 2 wk telephone call |
| 6 wk face to face |
| 6 wk telephone call |
| Other: Please state |
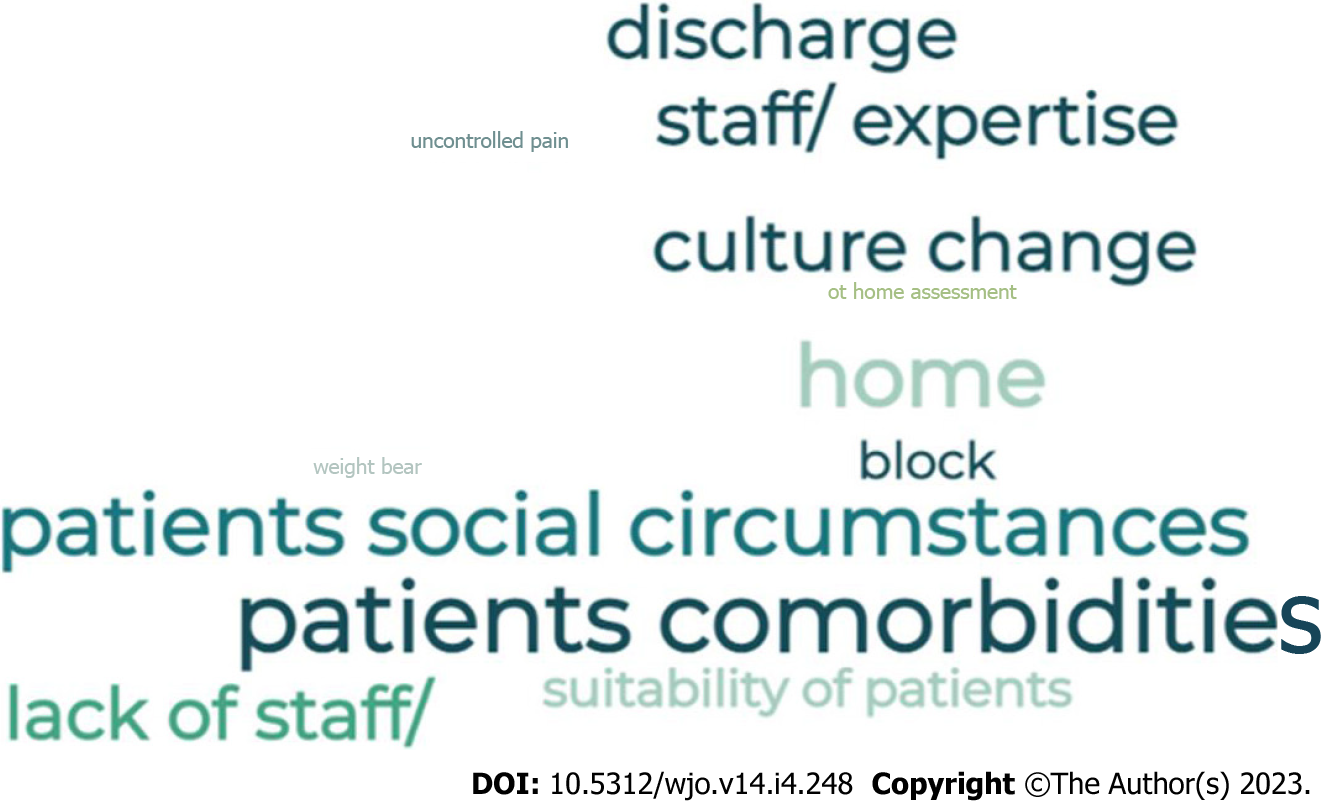
The study was reviewed and approved by the British Orthopaedic Foot and Ankle Society (BOFAS) Scientific Committee who also deemed the proposed statistical methods as appropriate. The questionnaire was sent to the membership of BOFAS via an administrator. It was sent to 605 recipients of whom 482 were full BOFAS members. A total of 365 recipients opened the email and 152 started the survey. For the purpose of this survey a major foot and ankle procedure was defined as surgery that is usually performed as an inpatient (e.g. ankle fusion, reconstruction). Day-case surgery was defined as patients that were discharged on the same day, with day surgery as the intended treatment pathway. There were two rounds of communication via email, the survey was then closed and data extracted into Microsoft Excel. The available data was analysed (as proportions/percentages) and free-text responses were tabulated for word clouds to be generated.
The survey design allowed multiple responses to some of the questions and this was taken into account in the final analysis.
Out of 132 respondents, 120 were foot and ankle surgeons and 12 were trauma and orthopaedic consultants. The majority (80%) worked in acute NHS care trusts and a proportion (28%) had additional work within private or district healthcare. 20% worked in just private or district general hospitals. 11% of those working in private practice only, 29% work in district general hospitals and 7% work in both private practice and district general hospitals.
Table 2 outlines the responses for current practices and protocols. The most responses when asked approximately how many major foot and ankle surgeries are performed in their centre in 1 calendar year was less than 100 (45%) and 200-500 (22%) with an average of 31.5% being performed as day-case. 78% of all respondents think there is a potential for more major foot and ankle surgeries to be performed as day-case in their centres. From the total respondents 48% said they did follow a protocol, 90% following their local protocol and 10% following generic national guidance.
| Factor | Result |
| Estimated number of major foot and ankle surgeries performed in 1 calendar year | Less than 100 (n = 60) (45) |
| 100-200 (n = 25) (19) | |
| 200-500 (n = 29) (22) | |
| 500-1000 (n = 9) (7) | |
| Over 1000 (n = 2) (2) | |
| Unsure (n = 7) (5) | |
| Estimated procedures performed as day-case | 0-50 (n = 99) (75) |
| 50-100 (n = 30) (23) | |
| Unsure (n = 3) (2) | |
| Is there a potential for more to be done as day-case | Yes (n = 103) (78) |
| No (n = 29) (22) | |
| Follow a protocol for day-case | Yes Local (n = 57) (43) |
| Yes national (n = 6) (5) | |
| No (n = 50) (38) | |
| Unsure (n = 19) (14) | |
| Types of Anaesthesia offered for day-casea | Regional (n = 63) (48) |
| General (n = 69) (52) | |
| Combination of regional & general (n = 107) (81) | |
| Specific blocks (n = 100) (76) | |
| Unsure (n = 3) | |
| Routinely discharge with controlled drugs | Yes (n = 34) (26) |
| No (n = 85) (64) | |
| Unsure (n = 13) (10) |
The most common type of anaesthetic used was a combination of general and regional anaesthetic (81%) the second highest was specific blocks e.g. popliteal, ankle etc. (76%). 64% of respondents put both a combination of regional and general as well as specific blocks. 64% of respondents do not routinely discharge patients with opiate/controlled drugs post-surgery.
Table 3 shows all responses for pre-operative and post-operative management. Physiotherapy assessment was performed pre-operatively (61%) and post-operatively (70%). The most common post-operative analgesic drugs used are paracetamol (86%) and codeine (84%) or a combination of the two (80%). 42% offer ibuprofen, paracetamol and codeine. The majority of surgeons responded that they did not routinely discharge patients with opiates/controlled drugs such as; oramorph or oxycodone (64%).
| Factor | Result |
| All patients seen pre-operatively by physiotherapy | Yes (n = 80) (61) |
| No (n = 45) (34) | |
| Unsure (n = 7) (5) | |
| All patients seen post-operatively by physiotherapy | Yes (n = 92) (70) |
| No (n = 28) (21) | |
| Unsure (n = 12) (9) | |
| Post-operative contact made to the patient | Yes (n = 20) (15) |
| No (n = 92) (70) | |
| Unsure (n = 20) (15) | |
| Outcome measures recorded for day-casea | VAS (n = 45) (34) |
| Complication rate & type (n = 41) (31) | |
| Patient satisfaction (n = 13) (10) | |
| MOX-FQ (n = 42) (32) | |
| EQ-5D (n = 31) (23) | |
| Other (n = 7) (5) | |
| Types of post-op analgesia offered for day-casea | Amitriptyline (n = 1) (1) |
| Gabapentin (n = 5) (4) | |
| Paracetamol (n = 114) (86) | |
| Ibuprofen (n = 64) (48) | |
| Codeine (n = 111) (84) | |
| Unsure (n = 9) (7) | |
| Other (n = 18) (14) | |
| Paracetamol & codeine (n = 105) (80) | |
| Ibuprofen, codeine & paracetamol (n = 55) (42) | |
| Ibuprofen & paracetamol (n = 6) (5) |
The top two perceived barriers to performing day-case surgery were lack of physiotherapy input pre/post operatively (23%) and no of out of hours support (21%). Free text responses from respondents were tabulated and created into a word cloud diagram (Figure 1). The main complications respondents have witnessed/heard about in major foot and ankle surgery done as day-case were breakthrough pain (64%) and unplanned readmission (45%). Respondents most commonly reported re-evaluating patients 2 weeks post operatively, and this being face to face (90%) (Table 4).
| Factor | Result |
| Barriers to performing day-case | No out of hours support (n = 28) (21) |
| No Physio pre/post-op (n = 31) (23) | |
| No Anaesthetist (n = 12) (9) | |
| Lack of managerial support (n = 10) (8) | |
| Never been done before (n = 9) (7) | |
| Non-response (n = 15) (11) | |
| Unsure (n = 23) (17) | |
| Other (n = 7) (5) | |
| Complications heard/witnessed from day-casea | Wound healing (n = 33) (25) |
| Wound Infection (n = 23) (17) | |
| Breakthrough pain (n = 84) (64) | |
| Patient dissatisfaction (n = 33) (25) | |
| Unplanned readmission (n = 60) (45) | |
| Further surgery (n = 12) (9) | |
| Delayed non-union (n = 12) (9) | |
| How are patients first re-evaluated after dischargea | 24 h (Face to face, n = 3, 2%) (Telephone, n = 14, 11%) |
| 1 wk (Face to face, n = 15, 11%) (Telephone, n = 3, 2%) | |
| 2 wk (Face to face, n = 119, 90%) (Telephone, n = 1, 1%) | |
| 6 wk (Face to face, n = 54, 41%) (Telephone, n = 2, 2%) | |
| Other (n = 9) (7) |
This survey found that there are a small number of major foot and ankle surgeries taking place as day-case within the centres of respondents. The majority of those who responded believed that there was scope to perform more major foot and ankle procedures as day-case. The main perceived barriers for performing more major foot and ankle procedures as day-case were lack of adequate physiotherapy input before or after surgery and lack of out of hours support for patients to contact in an emergency following their surgery. Although lack of physiotherapy input was one of the top perceived barriers, the majority of respondents selected yes to whether patients were seen by physiotherapy pre and post-operatively. This response was in relation to surgeon’s current management with no specificity to whether this was inpatient or day-case surgery management.
Previous evidence has suggested that a concern for patients’ pain and satisfaction levels post-surgery is a reason for major foot and ankle surgeries to be performed as inpatient over outpatient[8]. This survey found that majority of respondents have heard or witnessed breakthrough pain and unplanned readmissions as the top two complications to day-case surgery, however patients’ pain and satisfaction levels was only measured by a third of respondents. The top two highest complications heard/witnessed by respondents agrees with previous evidence however the low response rate to measuring post-operative pain/satisfaction means it is not possible to determine whether these are a barrier to major foot and ankle surgeries being performed as day-case.
When observing the outcomes following outpatient total ankle replacements Sadoun and colleagues found that re-admission for acute care did not occur for any patient for haematoma or uncontrolled pain; only 1 patient had delayed wound healing but this did not require any implant revision[18]. The evidence for foot and ankle surgeries such as total ankle replacement and other hind foot procedures is promising and shows that they can be performed safely as day-case. There is, howevera lack of evidence around other major procedures such as ankle fusions being performed as day-case. The safety of outpatient compared with inpatient ankle surgery is comparable and therefore they suggest that outpatient ankle surgeries should be considered for patients that are suitable[19].
Recently, the Get It Right First Time (GIRFT) initiative has been working with British Association of Day Surgery (BADS) to ‘address common misconceptions and making the case for expanding and increasing day case surgery, especially at a time when the NHS needs to re-start and catch up with demand for elective surgery following the Covid-19 pandemic’[2]. Part of the work of the GIRFT initiative is to develop a generic day case pathway which can be applied to specific surgical areas. Alongside this, specific best practice pathways, templates and checklists will be produced[2]. Nearly half of the respondents reported that they do follow a protocol for day-case surgeries and this was predominately a local protocol. To our knowledge there are no known national protocols for day-case foot and ankle surgery which could account for the lack of day surgeries taking place within this patient population. This is in contrast to other lower-limb orthopaedics procedures. Therefore by achieving consensus on guidelines and making them more specific for foot and ankle procedures, this may increase the amount of day-case surgeries for foot and ankle. Thereby extending the list of day-case procedures in the BADS directory [1].
There are limitations within this scoping survey. The survey design in itself relies on accurate self-report by the respondents who may over/underestimate data from their unit. Therefore, the data should be interpreted with caution. The number of responses from the survey was relatively low (37% response rate from those who read the email invitation). This is a fairly typical response rate; however may not be representative of the BOFAS organisation as a whole. Also the survey was only sent to surgeons; therefore there were no responses from other health professionals who manage this patient group (e.g. physiotherapists, plaster technicians). It may be important to capture the views of these professionals in future work. More in depth responses may also be valuable in the form of qualitative interviews/focus groups. For example, it would be useful to know more about in-operative anaesthesia, catherisation and on discharge pain medication.
Moving forwards to further explore/overcome the facilitators and barriers for performing major foot and ankle surgeries as day-case would include; out of hours support, therapy input pre and post-op, standardising outcome measures, patient education and culture shifts within patient and professionals mind sets. Breakthrough pain and unplanned readmissions were the most prevalent complications heard about/witnessed from day-case surgery in respondents and could therefore influence decisions about performing this type of surgery. Further work to address these risks is warranted. Future work should explore a cost effectiveness analysis of increasing day-case surgery in major foot and ankle procedures.
We have identified an appetite to increase the number of major foot and ankle procedures within UK foot and ankle surgeons who completed our survey. Post-operative pain and patient satisfaction was only measured by a third of those surveyed; despite theoretical concerns about these outcomes. Out of hours support and physiotherapy input were perceived as the main barriers to doing day-case surgery in foot and ankle surgery.
There is a need for nationally agreed protocols to optimise the delivery of and measurement of outcomes in this type of surgery. At a local level, the provision of physiotherapy and out of hours support should be explored at sites where this is a perceived barrier.
There is consensus amongst United Kingdom (UK) surgeons to do more major foot and ankle procedures as day-case. Despite theoretical concerns about post-operative pain and satisfaction this was only measured by a third of those surveyed. Out of hours support and physiotherapy input were perceived as the main barriers.
A total of 132 respondents completed the survey and 80% worked in Acute NHS Trusts. Currently 45% of respondents perform less than 100 day-case surgeries per year for these procedures. Post-operative pain (34%) and patient satisfaction (10%) was not highly measured within their centres. The top perceived barriers to performing more major foot and ankle procedures as day-case were: Lack of adequate physiotherapy input and lack of out of hours support.
Online survey sent to British orthopaedic foot and ankle society members. Quantitative and qualitative data collected.
To scope the current practices of UK foot and ankle surgeons on day-case surgery for major foot and ankle procedures.
Day-case is used in other orthopaedic procedures with benefits of patients and providers.
There are currently no specific guidelines for day-case surgery in major foot and ankle procedures.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Indino C, Italy; Yang WY, China S-Editor: Liu JH L-Editor: A P-Editor: Yuan YY
| 1. | British association of day surgery. Accessed 24/08/2022. Available from: https://bads.co.uk/. |
| 2. | GIRFT Report. Accessed 24/08/ 2022. Available from: https://www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/08/National-Day-Surgery-Delivery-Pack_Aug2021_final.pdf. |
| 3. | Bailey CR, Ahuja M, Bartholomew K, Bew S, Forbes L, Lipp A, Montgomery J, Russon K, Potparic O, Stocker M. Guidelines for day-case surgery 2019: Guidelines from the Association of Anaesthetists and the British Association of Day Surgery. Anaesthesia. 2019;74:778-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 174] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 4. | Martín-Ferrero MÁ, Faour-Martín O, Simon-Perez C, Pérez-Herrero M, de Pedro-Moro JA. Ambulatory surgery in orthopedics: experience of over 10,000 patients. J Orthop Sci. 2014;19:332-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Lazic S, Boughton O, Kellett CF, Kader DF, Villet L, Rivière C. Day-case surgery for total hip and knee replacement: How safe and effective is it? EFORT Open Rev. 2018;3:130-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 6. | Thompson JW, Wignadasan W, Ibrahim M, Beasley L, Konan S, Plastow R, Magan A, Haddad FS. Day-case total hip arthroplasty: a literature review and development of a hospital pathway. Bone Jt Open. 2021;2:93-102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Larsen JR, Skovgaard B, Prynø T, Bendikas L, Mikkelsen LR, Laursen M, Høybye MT, Mikkelsen S, Jørgensen LB. Feasibility of day-case total hip arthroplasty: a single-centre observational study. Hip Int. 2017;27:60-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Elbashir M, Uzoigwe C, Kurup H. Day case ankle arthroplasty: are they safe and cost effective? J Clin Orthop Trauma. 2022;30:101919. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Mangwani J, Williamson D, Allan T. Is it possible to do major hindfoot and ankle operations as day surgery? Orthopaedic Proceedings: The British Editorial Society of Bone & Joint Surgery 2012; 94: 46-46. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Jagodzinski NA, Gul R, Khanum S, Prem H. Day surgery for major paediatric foot and ankle procedures. J Orthop Surg (Hong Kong). 2011;19:69-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Athar MS, Fazal MA, Ashwood N, Arealis G, Buchanan D, Okoth FH. Daycase trauma list: a safe and cost-effective service delivery. Ann R Coll Surg Engl. 2019;101:519-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Jantzen C, Ebskov LB, Andersen KH, Benyahia M, Rasmussen PB, Johansen JK. Overnight Admission After Total Ankle Replacement: Is It Safe? J Foot Ankle Surg. 2021;60:89-92. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Albright D, Hinderstein C. The centrifuge connection. Bull At Sci. 2004;60:61-66. [DOI] [Full Text] |
| 14. | Ahluwalia R, Cook J, Raheman F, Karuppaiah K, Colegate-Stone T, Tavakkolizadeh A, Kavarthapu V, Sinha J. Improving the efficiency of ankle fracture care through home care and day-surgery units: Delivering safe surgery on a value-based healthcare model. Surgeon. 2021;19:e95-e102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Langan TM, Rushing CJ, McKenna BJ, Berlet GC, Hyer CF. The Safety Profile of Same-Day Outpatient Total Ankle Arthroplasty. J Foot Ankle Surg. 2022;61:123-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Malik AT, Quatman CE, Khan SN, Phieffer LS, Rao P, Ly TV. Outpatient Versus Inpatient Surgical Fixation of Isolated Ankle Fractures: An Analysis of 90-Day Complications, Readmissions, and Costs. J Foot Ankle Surg. 2020;59:502-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Moon AS, McGee AS, Patel HA, Cone R, McGwin G Jr, Naranje S, Shah A. A Safety and Cost Analysis of Outpatient Versus Inpatient Hindfoot Fusion Surgery. Foot Ankle Spec. 2019;12:336-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Sadoun M, Hardy A, Cladière V, Guichard L, Bauer T, Stiglitz Y. Outpatient total ankle replacement. Int Orthop. 2021;45:2429-2433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Plantz MA, Sherman AE, Kadakia AR. A propensity score-matched analysis comparing outpatient and short-stay hospitalization to standard inpatient hospitalization following total ankle arthroplasty. J Orthop Surg Res. 2020;15:292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |