Published online Apr 18, 2023. doi: 10.5312/wjo.v14.i4.231
Peer-review started: January 24, 2023
First decision: February 8, 2023
Revised: February 18, 2023
Accepted: March 27, 2023
Article in press: March 27, 2023
Published online: April 18, 2023
Processing time: 83 Days and 23.2 Hours
While Singapore attains good health outcomes, Singapore’s healthcare system is confronted with bed shortages and prolonged stays for elderly people recovering from surgery in acute hospitals. An Acute Hospital-Community Hospital (AH-CH) care bundle has been developed to assist patients in postoperative rehabilitation. The core concept is to transfer patients out of AHs when clinically recommended and into CHs, where they can receive more beneficial dedicated care to aid in their recovery, while freeing up bed capacities in AHs.
To analyze the AH length of stay (LOS), costs, and savings associated with the AH-CH care bundle intervention initiated and implemented in elderly patients aged 75 years and above undergoing elective orthopedic surgery.
A total of 862 1:1 propensity score-matched patients aged 75 years and above who underwent elective orthopedic surgery in Singapore General Hospital (SGH) before (2017-2018) and after (2019-2021) the care bundle intervention period was analyzed. Outcome measures were AH LOS, CH LOS, hospitalization metrics, postoperative 30-d mortality, and modified Barthel Index (MBI) scores. The costs of AH inpatient hospital stay in the matched cohorts were compared using cost data in Singapore dollars.
Of the 862 matched elderly patients undergoing elective orthopedic surgery before and after the care bundle intervention, the age distribution, sex, American Society of Anesthesiologists classification, Charlson Comorbidity Index, and surgical approach were comparable between both groups. Patients transferred to CHs after the surgery had a shorter median AH LOS (7 d vs 9 d, P < 0.001). The mean total AH inpatient cost per patient was 14.9% less for the elderly group transferred to CHs (S$24497.3 vs S$28772.8, P < 0.001). The overall AH U-turn rates for elderly patients within the care bundle were low, with a 0% mortality rate following orthopedic surgery. When elderly patients were discharged from CHs, their MBI scores increased significantly (50.9 vs 71.9, P < 0.001).
The AH-CH care bundle initiated and implemented in the Department of Orthopedic Surgery appears to be effective and cost-saving for SGH. Our results indicate that transitioning care between acute and community hospitals using this care bundle effectively reduces AH LOS in elderly patients receiving orthopedic surgery. Collaboration between acute and community care providers can assist in closing the care delivery gap and enhancing service quality.
Core Tip: This study evaluated the cost-effectiveness of an intervention that bundled Acute Hospital-Community Hospital (AH-CH) care. The AH-CH care bundle intervention effectively reduced AH length of stay (LOS) and costs for elderly patients aged 75 and above undergoing elective orthopedic surgery in Singapore General Hospital. Our findings indicate that systematically transitioning care between AH and CH using this care bundle reduces AH LOS and achieves cost savings. This intervention increases public hospital bed capacity and reduces inpatient hospitalization costs.
- Citation: Tan IEH, Chok AY, Zhao Y, Chen Y, Koo CH, Aw J, Soh MHT, Foo CH, Ang KA, Tan EJKW, Tan AHC, Au MKH. Acute hospital-community hospital care bundle for elderly orthopedic surgery patients: A propensity score-matched economic analysis. World J Orthop 2023; 14(4): 231-239
- URL: https://www.wjgnet.com/2218-5836/full/v14/i4/231.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i4.231
Singapore is one of the world’s fastest-aging countries, with a total population of 5.7 million people[1]. According to the forecasts of demographic statistics[1], the proportion of people aged 65 and beyond is anticipated to quadruple from 8% in 2005 to 20% in 2030 and 38% by 2050[2]. This demographic transition puts Singapore’s healthcare system under strain, as an aging population presents a mix of issues. For instance, an aging population increases the demand for joint replacement surgery, particularly among those aged 65 years and above[3]. Orthopedic surgery is sometimes associated with increased mortality and morbidity in the elderly patient population compared to the general population[4-7].
Additionally, the risk of hospitalization for those aged 65 years and above is higher and is associated with a longer length of stay (LOS) in acute hospitals (AHs)[8], resulting in an increased socioeconomic burden. In Singapore, age-adjusted per capita bed days in AHs have been gradually increasing since 2006, primarily due to an increase in admissions[9]. The proportion of patients aged 65 years and older admitted to public healthcare institutions has climbed from 28.6% in 2006 to 39.0% in 2020[9]. The requirement for postoperative rehabilitation and continuing care following discharge from AHs is also projected to increase as the elderly require a more extended recovery period. Therefore, any inter
Several care bundles or interventions have been adopted to improve patient care and decrease AH LOS in a general population undergoing surgery[10-12]. Most of them are interdisciplinary in nature and focus on optimizing all aspects of the patient’s perioperative management while also encouraging the patient to participate actively in their own recovery and rehabilitation. Similarly, Singapore’s Ministry of Health (MOH) has developed an AH-CH care bundle to improve the quality of care and provide ongoing postoperative care to assist patients in rehabilitating and reintegrating into their communities[13]. The core concept of this care bundle is to transfer patients out of AHs at the point when clinically necessary and into CHs, where they can receive more beneficial dedicated postoperative care to aid in their recovery while freeing up scarcer capacity in AHs. The AH-CH care bundle aims to recognize CH as an integral aspect of inpatient care by treating the AH and CH stay as a single episode. The workstream of this care bundle collaborates closely with inpatient teams at AHs to facilitate discharge planning and a smooth transfer to CHs.
This study aimed to evaluate the potential benefits and analyze the AH inpatient hospitalization costs and savings associated with this AH-CH care bundle in elderly patients undergoing orthopedic surgery in Singapore General Hospital (SGH).
This study was approved by our institutional review board (IRB No. 2022/2178) and reported following Consolidated Health Economic Evaluation Reporting Standards (CHEERS 2022) guidelines[14]. It was a retrospective single-center analysis of outcomes for elderly patients ≥ 75 years admitted to the orthopedic surgery department in SGH between two study periods: 2017-2018 (before the bundled-care period) vs 2019-2021 (after the bundled-care period). The inclusion criteria were all elderly patients aged 75 and above undergoing elective major orthopedic surgery between 2017 and 2021. Data was collected from our electronic health intelligence system and finance database. Patients who underwent emergency surgery were excluded from the evaluation.
Propensity score matching was performed to balance the comparison of elderly patients receiving orthopedic surgery in a 1:1 ratio before and after the care bundle periods based on age, sex, American Society of Anesthesiologists classification, Charlson Comorbidity Index (CCI), and surgical approach. The matched cohorts were examined for discharge deposition, AH LOS, and postoperative 30-d mortality. The CCI was calculated based on a patient’s diagnosis using the 10th revision of the International Statistical Classification of Disease and Related Health Problems (ICD-10) codes. Patients within the care bundle were further analyzed for CH LOS, total AH-CH LOS, referral waiting time from AH to CH, U-turn rates, and Modified Barthel Index (MBI) scores, which employs a 100-point rating scale that evaluates a patient’s capacity to execute ten distinct activities of daily living[15].
Costs were derived from inpatient billing data and indicated the total cost of the inpatient stay per case prior to the subsidy. Cost data were adjusted to 2021 Singapore dollars to account for healthcare inflation (approximately 1.02%-1.08% over the study period; Monetary Authority of Singapore, https://www.mas.gov.sg/). Cost breakdown was calculated and compared between the two matched cohorts.
Statistical analyses were performed in R Statistical Software (version 4.2.1). Continuous variables were reported as median (range) or mean ± SD. Categorical variables were reported as frequency (percentage). The Wilcoxon-Mann-Whitney test was used to analyze continuous variables, and χ2 or Fisher’s exact tests were used to analyze categorical variables. Cost data were presented as mean ± SD following CHEERS guidelines[14]. Statistical significance was set at a P value < 0.05.
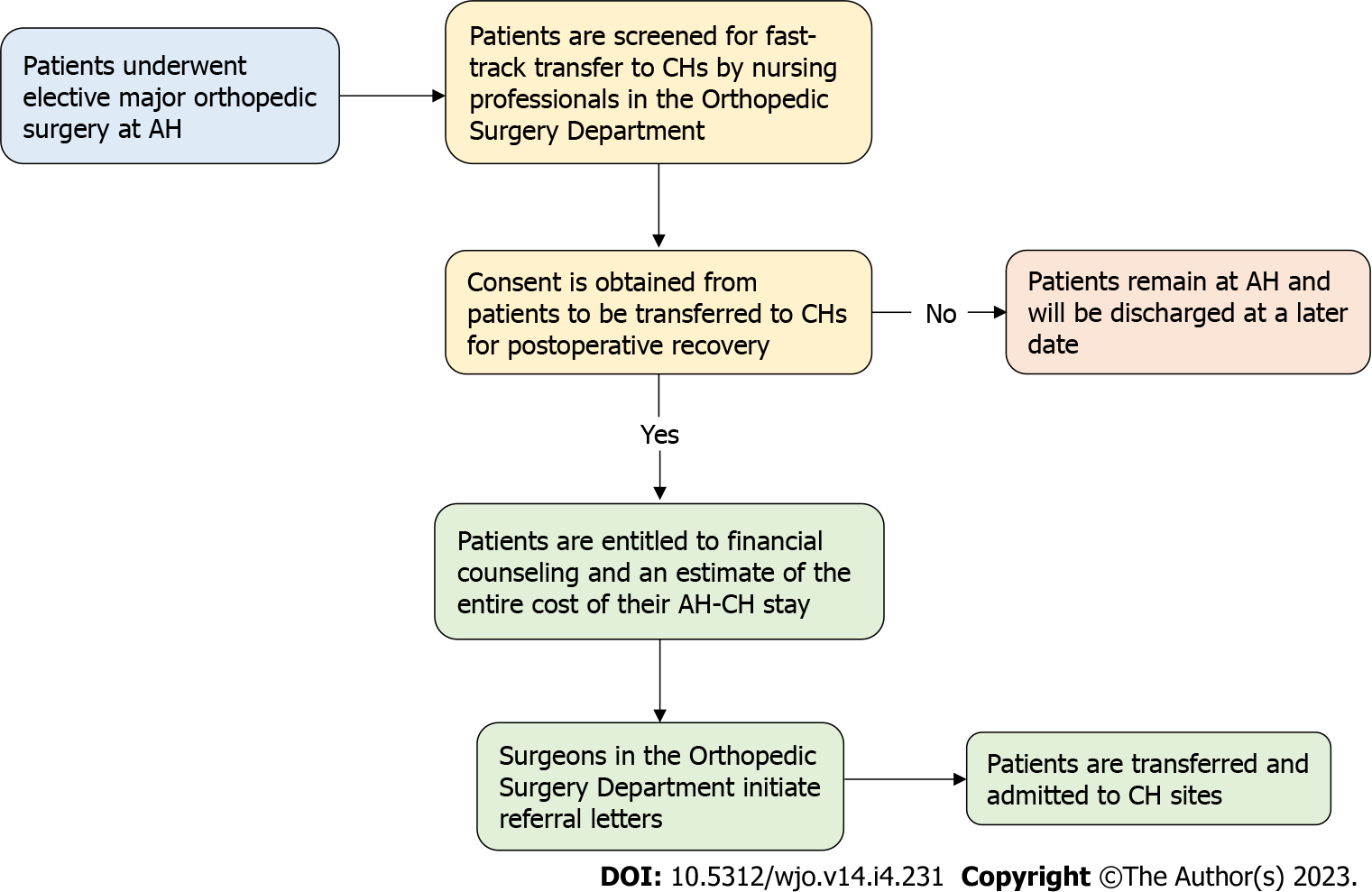
Following the AH-CH care bundle intervention, we have developed a rapid transfer pathway from AH to CH for elderly patients undergoing orthopedic surgery (Figure 1). Briefly, once patients have completed surgery at the AH site, they are screened for fast-track transfer to CH sites by nursing professionals from the orthopedic surgery department. Patients who consent to be treated in CH facilities are entitled to financial counseling for an estimated cost of their entire AH-CH stay. Afterward, surgeons initiate CH referral letters, and patients are transported and admitted to CH sites. We analyzed 862 elderly patients in total who underwent elective orthopedic surgery before and after the AH-CH care bundle intervention.
Patient demographics, clinical and surgical characteristics, and hospitalization metrics between the two matched cohorts are shown in Table 1. There was no significant difference in patient demographics, baseline characteristics, and discharge deposition. Elderly patients within the care bundle transferred to CHs after the surgery had a shorter median AH LOS of 7 d (range: 1-44; mean 8.83) compared to 9 d (range: 7-73; mean 12.5) in patients before the care bundle period (P < 0.001). The mortality rate for all included patients was 0% following orthopedic surgery.
| Variable | Before care bundle period (2017-2018) | After care bundle period (2019-2021) | P value |
| n (%) | n (%) | ||
| Matched patients | 431 | 431 | |
| Age (yr), median (range) | 79 (75-97) | 80 (75-99) | 0.184 |
| Gender | |||
| Male | 111 (25.8) | 123 (28.5) | 0.400 |
| Female | 320 (74.2) | 308 (71.5) | |
| ASA classification | |||
| 1 | 3 (0.7) | 8 (1.9) | 0.074 |
| 2 | 336 (78.0) | 311 (72.2) | |
| 3 | 92 (21.3) | 112 (26.0) | |
| 4 | 0 | 0 | |
| CCI | |||
| 0 | 3 (0.7) | 8 (1.9) | 0.200 |
| 1 | 12 (2.8) | 21 (4.9) | |
| 2 | 316 (73.3) | 292 (67.7) | |
| 3 | 16 (3.7) | 18 (4.2) | |
| ≥ 4 | 84 (19.5) | 92 (21.3) | |
| Surgical approach | |||
| Open | 346 (80.3) | 337 (78.2) | 0.502 |
| MIS | 85 (19.7) | 94 (21.8) | |
| AH LOS (d) | |||
| Median (range) | 9 (7-73) | 7 (1-44) | < 0.001 |
| Mean (SD) | 12.5 (13.8) | 8.83 (7.02) | < 0.001 |
| Discharged home | 431 (100) | 431 (100) | - |
| Postoperative mortality | 0 | 0 | - |
The AH inpatient stay of both groups is shown in Table 2. Elderly patients within the care bundle group had a significantly lower mean total AH inpatient hospitalization cost of S$24497.3 per patient, 14.9% lower than patients before the care bundle period of S$28772.8 per patient (P < 0.001). The detailed cost breakdown analysis revealed that the care bundle group had much lower costs for ward accommodation (S$5924.4 vs S$8748.8, P < 0.001), daily medical treatment (S$2932.4 vs S$3980.9, P < 0.001), nursing care (S$1379.9 vs S$1574.3, P = 0.040), investigation (S$1847.1 vs S$2173.2, P = 0.003), and rehabilitation (S$634.0 vs S$905.0, P < 0.001) services. There was no significant difference in the costs of surgery procedure, pharmacy, and consumables between the two groups.
| AH hospitalization cost (S$) | Before care bundle period (n = 431) | After care bundle period (n = 431) | % Difference | P value |
| Total inpatient cost per case | 28772.8 (28581.6) | 24497.3 (15281.8) | 14.9% decrease | < 0.001 |
| Cost breakdown | ||||
| Surgery procedure | 4861.8 (2076.2) | 4594.6 (1847.1) | 5.5% decrease | 0.561 |
| Ward accommodation | 8748.8 (15164.3) | 5924.4 (6277.9) | 32.3% decrease | < 0.001 |
| Daily medical treatment | 3980.9 (4875.8) | 2932.4 (2371.8) | 26.3% decrease | < 0.001 |
| Nursing | 1574.3 (1715.5) | 1379.9 (959.5) | 12.4% decrease | 0.040 |
| Investigation | 2173.2 (2086.3) | 1847.1 (1828.1) | 15.0% decrease | 0.003 |
| Rehabilitation | 905.0 (1474.5) | 634.0 (490.7) | 29.9% decrease | < 0.001 |
| Pharmacy | 479.6 (1149.3) | 414.8 (988.2) | 13.5% decrease | 0.369 |
| Consumables | 2231.4 (1883.8) | 2412.2 (1631.4) | 8.1% increase | 0.132 |
The CH hospitalization metrics are shown in Table 3. Our first CH was officially opened in August 2018, followed by the second in January 2019. There was no CH data available prior to the implementation of the AH-CH care bundle. The median CH LOS was 23 d, 24 d, and 22 d within the care bundle group from 2019 to 2021. The median total AH-CH LOS was reduced from 35 d in 2019 to 33 d in 2021. The overall referral time from AH to CH after surgery was around 3 d to 5 d. A U-turn occurs when a patient is readmitted to AH within 8 h of being transferred to CH. The overall U-turn was almost 0, with only one case in 2021 readmitted to AH. MBI scores of elderly patients were significantly increased at the time of being discharged from CHs. The average MBI score for all elderly patients within the care bundle group improved significantly from 50.9 (SD: 23.9) at admission to 71.9 (SD: 23.4) at discharge (P < 0.001).
| Item | 2019 | 2020 | 2021 |
| Total case | 135 | 170 | 126 |
| CH LOS (d) (median, range) | 23 (4-98) | 24 (2-175) | 22 (2-87) |
| Total AH-CH LOS (d) (median, range) | 35 (8-122) | 33 (5-184) | 33 (9-114) |
| Referral time from AH to CH (d) (median, range) | 4 (1-20) | 5 (1-14) | 3 (1-12) |
| U-turn from CH to AH within 8 h (%) | 0 | 0 | 1 (0.79) |
| MBI score (median, range) | |||
| Admission | 58 (11-98) | 47 (5-94) | 37 (10-97) |
| Discharge | 74 (14-100) | 65 (12-100) | 68 (13-99) |
This study demonstrates that the AH-CH care bundle intervention can directly reduce AH LOS in elderly patients undergoing orthopedic surgery. Regaining movement and strength cannot occur quickly enough for an elderly patient recovering after orthopedic surgery. Physical and occupational therapy are the most effective strategies for resuming normal activities as quickly as possible[16]. Postoperative rehabilitation assists elderly patients in learning to perform their exercise appropriately, monitor their performance, and identify potential problems that the clinician should be aware of. However, rehabilitation and physiotherapy are typically time-consuming, and AH LOS is a quality indicator used by healthcare systems to assess the efficiency of their hospital operation. Reduced AH LOS increases bed turnover, enabling AHs to meet the demand for acute admission and interhospital transfers with an available capacity[17,18]. In Singapore, it has been observed a growth in AH admissions that was disproportionate to the growth of the general population. The mean AH LOS for elderly patients increased from 7.8 d in 2010 to 8.2 d in 2013[19]. As a result, Singapore is implementing system-level strategies to provide excellent care and a safe discharge while preventing prolonged AH stays. Our results identified potential benefits of this care bundle in shortening median AH LOS by two days in elderly patients undergoing orthopedic surgery, without sacrificing postoperative complications, readmissions, and mortality.
The total costs of AH inpatient stay were consequently reduced. Cost savings were achieved from cost buckets associated with prolonged AH LOS. Applying the observed decrease in AH LOS to our elderly patient cohort would have resulted in an estimated bed day savings of S$184440.0 between 2019 and 2021 (200 beds reserved for the orthopedic surgery department with an estimated bed day cost of S$461.1). Furthermore, the reduced LOS would improve AH’s capacity due to cost savings. As a result, there would be substantial advantages for both patients and the hospital because the increased capacity may boost utilization and cut down on waiting lists.
Compared to AH LOS, a CH stay might last from a few days to a few weeks, depending on the patient’s condition. CH services are designed to enhance patient functional impairment statuses and maximize their physical capacities in preparation for discharge home or continuation of treatment at other community-based step-down care facilities. The benefits of admission to CHs for rehabilitation care include the following: (1) A good chance for patients, particularly elderly patients, to improve physical functions; (2) patients can participate in at least two hours of therapy daily; and (3) patients and caregiver can participate in rehabilitation and discharge planning. Patients undergoing orthopedic surgery in this care bundle had a median CH LOS of 22-24 d. One constraint of this study was the limited bed capacity of our two newly-constructed CHs, which resulted in a slower bed turnover rate. The median duration between AH site referral and CH site acceptance was observed to be approximately 3-5 d. To fulfill the demand for intermediate residential care, Singapore’s MOH is expanding its network of CHs that will be co-located with their cluster-run AHs to complement acute care services and assist patient care continuums.
Our results demonstrated that CH is critical in providing rehabilitation and continuing care to assist elderly patients in rehabilitation. When elderly patients were discharged from CHs, their MBI scores increased significantly. The second constraint was that we were unable to get MBI scores for the matched cohort before the care bundle period. As such, we were unable to compare MBI scores between matched elderly patients discharged directly from AH and those transferred to CHs for further rehabilitation. Even if patients are discharged immediately from AH following orthopedic surgery, many of them will most likely require weekly postoperative rehabilitation at AH. In comparison, support from CH care professionals is another factor related to positive results for patients referred to CHs for postoperative rehabilitation. CH care teams will work with patients, particularly the elderly, to establish daily, achievable goals for participating in a function-specific exercise to regain strength. This is of great benefit to both patients and healthcare providers.
This study has a few limitations. First, the AH-CH care bundle is designed for a specific patient population and may not be applicable to other populations or healthcare settings. Second, the exclusion of emergency surgery patients may limit the generalizability of the study’s findings to a broader patient population. Third, this care bundle may not capture the unique characteristics and complexities of each specific orthopedic surgery procedure. However, there are a few perspectives on our findings. The AH-CH care bundle is a promising approach to improving the quality and efficiency of care for elderly patients undergoing elective orthopedic surgery. It provides a standardized and evidence-based practice, which may lead to enhanced patient outcomes and reduced costs, as well as promote a multidisciplinary approach to improve communication and collaboration between healthcare providers.
Our results show that transitioning care between acute and community hospitals via the AH-CH care bundle effectively reduces AH LOS in elderly patients undergoing orthopedic surgery. A well-designed postoperative rehabilitation program at CH sites can help prevent complications that may have a lasting effect on the quality of life.
Singapore’s healthcare system has faced bed shortages and extended stays for elderly patients recovering from surgery in acute hospitals.
An Acute Hospital-Community Hospital (AH-CH) care bundle was created to transfer patients to CHs where they can receive specialized care and free up beds in AHs.
To evaluate the impact of the AH-CH care bundle on AH length of stay (LOS), costs, and savings for elderly patients aged 75 years and above who underwent elective orthopedic surgery.
The study examined a cohort of 862 patients aged 75 years and above undergoing elective orthopedic surgery at Singapore General Hospital before (2017-2018) and after (2019-2021) the implementation of the AH-CH care bundle intervention. Patients were matched 1:1 based on their propensity scores and compared for AH LOS, CH LOS, hospitalization metrics, postoperative 30-d mortality, modified Barthel Index (MBI) scores, and costs.
Elderly patients transferred to CHs had a significantly shorter median AH LOS (7 d vs 9 d, P < 0.001), and the mean total AH inpatient cost per patient was 14.9% less for the elderly group transferred to CHs (S$24497.3 vs S$28772.8, P < 0.001). The overall AH U-turn rates for patients within the care bundle were low, with no mortality rate following orthopedic surgery. When elderly patients were discharged from CHs, their MBI scores improved significantly.
The AH-CH care bundle was found to be effective and cost-saving for elderly patients undergoing elective orthopedic surgery.
Collaboration between acute and community care providers can help to improve clinical service quality and achieve cost savings.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Health care sciences and services
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lin L, China; Primadhi RA, Indonesia S-Editor: Chen YL L-Editor: A P-Editor: Yuan YY
| 1. | Singapore S. Yearbook of statistics. Singapore: Department of Statistics, Ministry of Trade and Industry, 2009. [DOI] [Full Text] |
| 2. | Ministry of Community Development. Committee on Ageing Issues: Report on the Ageing Population. 2006. [cited 1 March 2023]. Available from: https://www.moh.gov.sg/docs/librariesprovider5/resources-statistics/reports/committee-on-ageing-issues-report-on-ageing-population.pdf. |
| 3. | Birrell F, Johnell O, Silman A. Projecting the need for hip replacement over the next three decades: influence of changing demography and threshold for surgery. Ann Rheum Dis. 1999;58:569-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 146] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 4. | Aynardi M, Pulido L, Parvizi J, Sharkey PF, Rothman RH. Early mortality after modern total hip arthroplasty. Clin Orthop Relat Res. 2009;467:213-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 68] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Gregory J, Starks I, Phillips S. Five-year survival of patients in their 90th year and beyond undergoing primary hip arthroplasty in the UK. J Bone Joint Surg. 2010;92-B:1227-1230. [RCA] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Berend ME, Thong AE, Faris GW, Newbern G, Pierson JL, Ritter MA. Total joint arthroplasty in the extremely elderly: hip and knee arthroplasty after entering the 89th year of life. J Arthroplasty. 2003;18:817-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Wurtz LD, Feinberg JR, Capello WN, Meldrum R, Kay PJ. Elective primary total hip arthroplasty in octogenarians. J Gerontol A Biol Sci Med Sci. 2003;58:M468-M471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Rahman N, Ng SH, Ramachandran S, Wang DD, Sridharan S, Tan CS, Khoo A, Tan XQ. Drivers of hospital expenditure and length of stay in an academic medical centre: a retrospective cross-sectional study. BMC Health Serv Res. 2019;19:442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Tan CC, Lam CSP, Matchar DB, Zee YK, Wong JEL. Singapore’s health-care system: key features, challenges, and shifts. Lancet. 2021;398:1091-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 105] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 10. | Zarain-Obrador L, Alonso-García M, Gil-Yonte P, Hijas-Gómez AI, Rodríguez-Villar D, Martínez-Amores B, Gil-de-Miguel Á, Ruiz-Tovar J, Rodríguez-Caravaca G, Durán-Poveda M. Effect of a Surgical Care Bundle on the Incidence of Surgical Site Infection in Colorectal Surgery: A Quasi-Experimental Intervention. Rev Invest Clin. 2021;73:251-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Weiser MR, Gonen M, Usiak S, Pottinger T, Samedy P, Patel D, Seo S, Smith JJ, Guillem JG, Temple L, Nash GM, Paty PB, Baldwin-Medsker A, Cheavers CE, Eagan J, Garcia-Aguilar J; Memorial Sloan Kettering Multidisciplinary Surgical-Site Infection Reduction Team. Effectiveness of a multidisciplinary patient care bundle for reducing surgical-site infections. Br J Surg. 2018;105:1680-1687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Bolshinsky V, Li MH, Ismail H, Burbury K, Riedel B, Heriot A. Multimodal Prehabilitation Programs as a Bundle of Care in Gastrointestinal Cancer Surgery: A Systematic Review. Dis Colon Rectum. 2018;61:124-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 98] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 13. | Gross PA, Neu HC, Aswapokee P, Van Antwerpen C, Aswapokee N. Deaths from nosocomial infections: experience in a university hospital and a community hospital. Am J Med. 1980;68:219-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 233] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 14. | Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, Caulley L, Chaiyakunapruk N, Greenberg D, Loder E, Mauskopf J, Mullins CD, Petrou S, Pwu RF, Staniszewska S; CHEERS 2022 ISPOR Good Research Practices Task Force. Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Int J Technol Assess Health Care. 2022;38:e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 132] [Article Influence: 44.0] [Reference Citation Analysis (0)] |
| 15. | Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud. 1988;10:61-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1642] [Cited by in RCA: 1821] [Article Influence: 49.2] [Reference Citation Analysis (0)] |
| 16. | Désiron HA, de Rijk A, Van Hoof E, Donceel P. Occupational therapy and return to work: a systematic literature review. BMC Public Health. 2011;11:615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | Buttigieg SC, Abela L, Pace A. Variables affecting hospital length of stay: a scoping review. J Health Organ Manag. 2018;32:463-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Schmidt R, Geisler S, Spreckelsen C. Decision support for hospital bed management using adaptable individual length of stay estimations and shared resources. BMC Med Inform Decis Mak. 2013;13:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Chia NC, Loh SP. Using the stochastic health state function to forecast healthcare demand and healthcare financing: Evidence from Singapore. Rev Dev Econ. 2018;22:1081-1104. [DOI] [Full Text] |