Published online Apr 18, 2023. doi: 10.5312/wjo.v14.i4.207
Peer-review started: September 29, 2022
First decision: January 17, 2023
Revised: February 15, 2023
Accepted: March 24, 2023
Article in press: March 24, 2023
Published online: April 18, 2023
Processing time: 201 Days and 0.8 Hours
Radiocarpal dislocations are rare but potentially devastating injuries. Poorer outcomes are associated with inadequate or lost reduction, such as ulnar translocation, but no consensus exists on the ideal fixation technique. Dorsal bridge plate fixation has been described for various settings in the treatment of complex distal radius fractures and can be fixed distally to the second or third metacarpal, but its application for radiocarpal dislocations has not been established.
To determine whether distal fixation to the second or third metacarpal matters.
Using a cadaveric radiocarpal dislocation model, the effect of distal fixation was studied in two stages: (1) A pilot study that investigated the effect of distal fixation alone; and (2) a more refined study that investigated the effect of described techniques for distal and proximal fixation. Radiographs were measured in various parameters to determine the quality of the reduction achieved.
The pilot study found that focusing on distal fixation alone without changing proximal fixation results in ulnar translocation and volar subluxation when fixing distally to the second metacarpal compared with the third. The second iteration demonstrated that anatomic alignment in coronal and sagittal planes could be achieved with each technique.
In a cadaveric radiocarpal dislocation model, anatomic alignment can be maintained with bridge plate fixation to the second metacarpal or the third metacarpal if the described technique is followed. When considering dorsal bridge plate fixation for radiocarpal dislocations, the surgeon is encouraged to understand the nuances of different fixation techniques and how implant design features may influence proximal placement.
Core Tip: Radiocarpal dislocations are rare but potentially devastating injuries. Poorer outcomes are associated with inadequate or lost reduction, such as ulnar translocation, but no consensus exists on the ideal fixation technique. Dorsal bridge plate fixation has been described for various settings in the treatment of complex distal radius fractures and can be fixed distally to the second or third metacarpal, but its application for radiocarpal dislocations has not been established. In a cadaveric radiocarpal dislocation model, anatomic alignment can be maintained with bridge plate fixation to the second metacarpal or the third metacarpal if the described technique is followed. When considering dorsal bridge plate fixation for radiocarpal dislocations, the surgeon is encouraged to understand the nuances of different fixation techniques and how implant design features may influence proximal placement.
- Citation: Tabeayo E, Saucedo JM, Srinivasan RC, Shah AR, Karamanos E, Rockwood J, Rodriguez-Merchan EC. Bridge plating in the setting of radiocarpal instability: Does distal fixation to the second or third metacarpal matter? A cadaveric study. World J Orthop 2023; 14(4): 207-217
- URL: https://www.wjgnet.com/2218-5836/full/v14/i4/207.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i4.207
Radiocarpal dislocations are uncommon injuries, representing 0.2% of all dislocations[1] with the largest clinical series to date reporting only 27 cases[2]. They occur most frequently after high energy trauma, such as motor vehicle accidents or falls from height. Men in their fourth decade are at highest risk[3,4]. The proposed mechanism of injury is flexion or extension of the radiocarpal joint in combination with a rotational component[2].
Two classifications have been proposed, distinguishing between pure dislocations and those with associated fractures. The Dumontier[2] classification emphasizes the difference between pure radiocarpal dislocations, including those with an avulsion of the tip of the radial styloid (group 1), and those with an associated fracture of the styloid involving more than one third of the scaphoid fossa (group 2). Moneim et al[5] describes two types: Type I consists of a pure volar or dorsal dislocation, and type II describes a more complex injury, involving intracarpal fractures, dislocations and more severe ligamentous disruption.
Current published treatment options include pin fixation and external fixation, soft tissue reconstruction, and decompression of neurovascular structures when indicated[2-4]. The most common predictors for a poor outcome include pure ligamentous injuries (Dumontier Group 1 and Moneim Type I), persistent instability and non-anatomic reduction[2]. Primary or secondary ulnar shifting of the carpus after initial reduction has been reported as a frequent finding associated with poor range of motion and function, especially in Dumontier Group 1 radiocarpal dislocations[2,6] (pure ligamentous injuries). Anatomic reduction and stable fixation, then, are of paramount importance.
The use of dorsal bridge plate fixation for complex distal radius fractures has continued to gain traction in recent years. Relying in part on ligamentotaxis, bridge plate fixation has been advocated for high-energy distal radius fractures[7], those with intraarticular and/or metadiaphyseal comminution[8,9], multiply injured patients with lower extremity trauma who require immediate platform weight-bearing[10], the elderly[11], as well as those in extremis[12,13]. Bridge plate fixation has also been described for lower energy fractures in patients who have a baseline reliance on upper extremity weight bearing assist devices[14,15].
Two major techniques have been described and advocated[8,9,16,17], each with its advantages and disadvantages. Fixation to the third metacarpal may better centralize the distal fragment and carpus with respect to the radius and have certain biomechanical advantages[18] but may also place the extensor tendons at risk[19]. Fixation to the second metacarpal, however, may improve radial height and inclination in certain distal radius fractures and avoid tendon or nerve entrapment[19].
Bridge plate fixation for radiocarpal instability has received some attention recently. Wahl et al[20] reported good outcomes with the use of this technique in their retrospective review of 13 patients, using fixation to the third metacarpal in all their cases[20]. Azad et al[21] recently shared their results of a cadaveric study and suggested that fixation to the third metacarpal may result in more anatomic alignment. The senior authors of our study (RC Srinivasan and JM Saucedo), however, have routinely used both techniques (distal fixation to the second or third metacarpals) in treating complex distal radius fractures and radiocarpal dislocations, and both techniques appear capable of achieving anatomic reduction and satisfactory clinical results.
Given the rarity of radiocarpal dislocations in the community and in the literature, there appears to be little consensus on which fixation method allows for more anatomic reduction and stable fixation in the setting of radiocarpal instability. To help answer this question, we designed a study to compare distal fixation to the second metacarpal vs the third metacarpal in a cadaveric radiocarpal dislocation model. We hypothesized that in a cadaveric model for radiocarpal instability, distal fixation to the third metacarpal and the second metacarpal can equally achieve anatomic alignment.
Ten matched trans-humeral cadaveric arms were obtained, whose ages ranged from 25 to 65 years old (mean 48). Four were men and one female. None had a history of previous injury or surgery. Each was examined grossly and radiographically to confirm the absence of anatomic deformity.
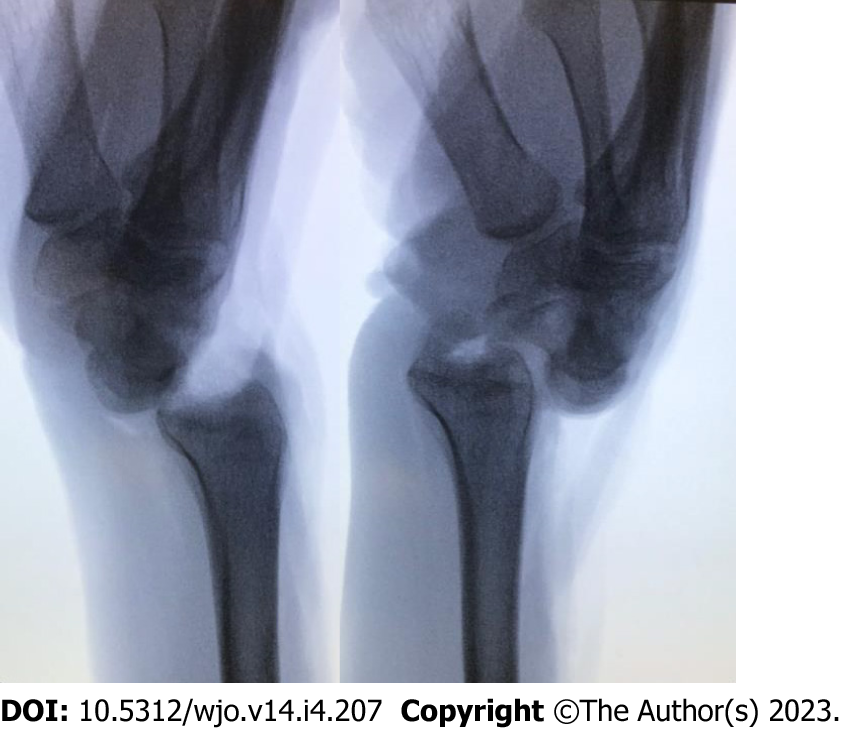
Cadaveric models were prepared through a standard dorsal approach to the radiocarpal joint. Under traction and through a dorsal incision over the radiocarpal joint, the dorsal and volar radiocarpal ligaments were transected until both dorsal and volar dislocation could be achieved with manipulation alone (defined by 100% translation of the carpus with respect to the radius on a standard lateral X-ray view) (Figure 1).
Each specimen was matched to itself to minimize confounding variables such as subtle differences in morphology. Each specimen had the plate fixed first to the radial shaft with a single screw through the fourth dorsal compartment. Then, all of the right-side specimens (group A) had the bridge plate fixed first to the second metacarpal. Once alignment was confirmed on fluoroscopy, an additional screw was placed distally and proximally. The plate was then removed from the second metacarpal and then fixed similarly to the third metacarpal with standardized X-rays obtained before and after each intervention. Group B included all of the left-sided specimens and underwent similar treatment except that distal fixation was made to the third metacarpal before the second.
The plate that was used is characterized by a widened center with a cluster of locking screw holes to facilitate fixation of fractures near the articular surface, as its primary design was meant to treat complex distal radius fractures.
Based on the results of the pilot study, a second study iteration was designed to more accurately reflect and evaluate the techniques as they were originally described. Two fixation techniques were studied: Distal fixation to the third metacarpal with the plate passed proximally through the floor of the fourth dorsal compartment (3M)[8] and distal fixation to the second metacarpal with the plate passed proximally through the second dorsal compartment (2M)[16]. Because the large cluster of screw holes in the previously used plate (the wide plate, WP) would not permit passage through the second dorsal compartment, a narrow plate (NP) design was used to facilitate passage through the second dorsal compartment.
Twelve fresh frozen cadaveric arms were obtained. The age of the specimens ranged from 37 to 85 (average 65.7 years old) and half of the specimens were male. Each was examined grossly and radiographically to confirm the absence of anatomic deformity. Each cadaver radiocarpal dislocation model was prepared in the manner described above.
For the 3M method, the WP is fixed to the third metacarpal distally and proximally to the radial shaft through the fourth dorsal compartment[17]. Our previous incision used to render the wrist unstable was used to expose the third and fourth dorsal compartments. The extensor pollicis longus was transposed, and the floor of the fourth dorsal compartment was elevated. A third incision over the dorsal shaft of the radius was made, and the WP was passed in retrograde fashion. While holding the radiocarpal joint reduced, the plate was secured under fluoroscopic guidance to the radius midshaft with 3.5 locking screws, and to the center of the third metacarpal with 2.7 locking screws. Fixation was obtained first with a single screw proximally and distally. Once reduction of the radiocarpal joint was confirmed by C-arm, a second screw was placed proximally and distally.
For the 2M method, the NP is fixed to the second metacarpal distally and proximally to the radial shaft through the second dorsal compartment[16]. The plate typically sits more radial on the proximal shaft than is seen with the 3M method. An incision was made over the second metacarpal, and the interval between the extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) tendon insertions was developed. A second incision was made proximal to the muscle bellies of the abductor pollicis longus and extensor pollicis brevis. The interval between the ECRL and ECRB was developed and the radial diaphysis exposed. The NP was passed from distal to proximal. While holding the radiocarpal joint reduced, the plate was secured to the second metacarpal with 2.7 mm screws and then to the radial diaphysis with 3.2 mm screws. Fixation was obtained first with a single screw proximally and distally. Once reduction of the radiocarpal joint was confirmed by C-arm, a second screw was placed proximally and distally.
The cadavers and the WP were provided through a research grant awarded by Acumed (Hillsborough, Oregon). The NP was provided on loan by TriMed (Valencia, California). Plates and screws were returned at the conclusion of the study. Surgical indications for bridge plating in the setting of radiocarpal dislocations were not included in the 510k for Acumed or TriMed at the time of this writing.
Radiographic imaging with standardized posterior-anterior (PA) and lateral radiographs were obtained prior to the dislocation procedure and after application of the plates. A true PA view of the distal radioulnar joint was obtained with the beam perpendicular to the distal radioulnar joint (DRUJ) and was defined by clear visualization of the ulnar head and sigmoid notch. Lateral views of the radiocarpal joint were standardized by using a 10 degree lateral tilt to optimize the lunate fossa and defined by overlap of the distal pole of the scaphoid over the pisiform[22].
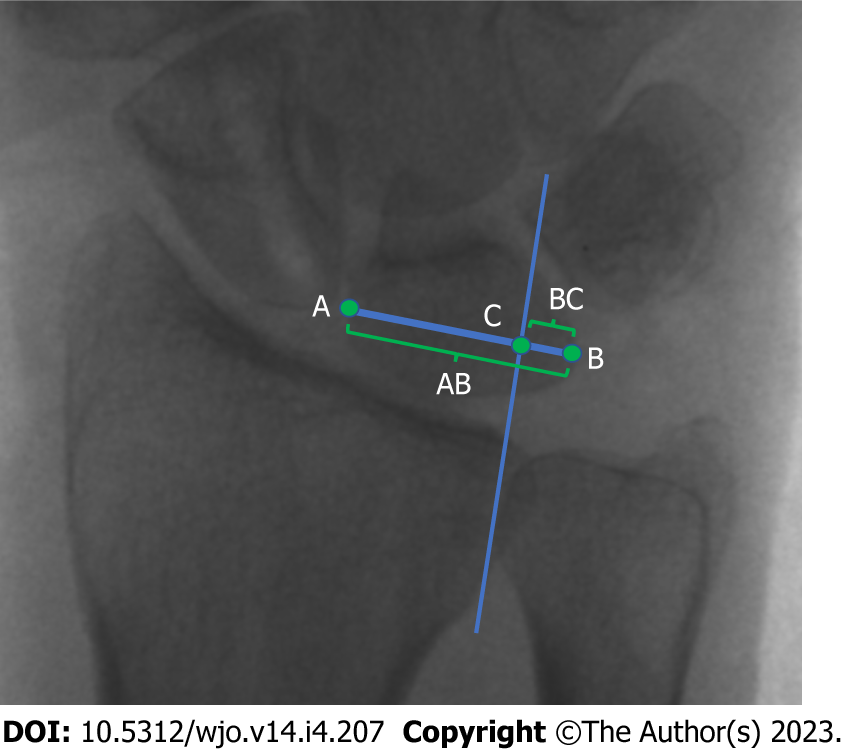
Specimens in the pilot study were measured before and after each intervention using two indices: Gilula’s lunate uncovering technique to measure the quality of radiocarpal reduction in the coronal plane (i.e., the amount of radio-ulnar translation) and the best-fit circle technique for sagittal alignment (i.e., volar-dorsal translation).
Gilula’s lunate uncovering has been proposed as the most sensitive method to measure ulnar translation of the carpus[23-25]. It measures the relationship between the total width of the lunate and the portion that is not covered by the radius lunate fossa. This calculation is demonstrated in Figure 2.
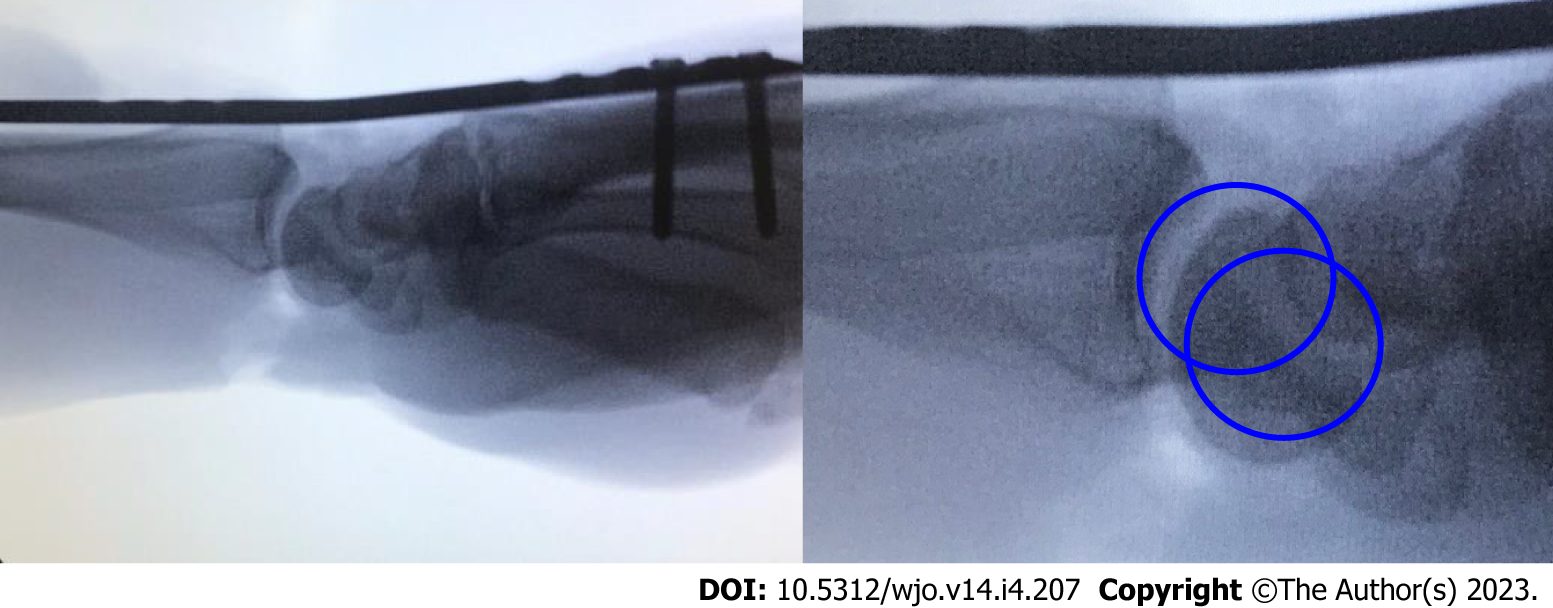
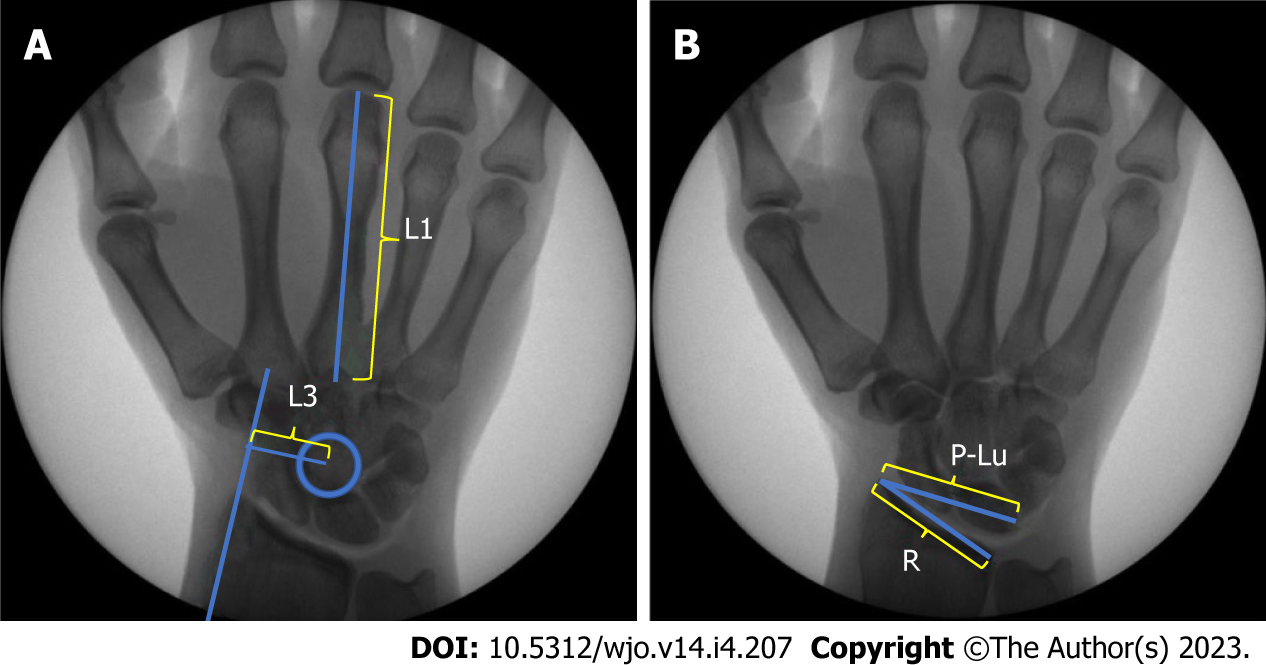
Lateral views were evaluated to assess radiocarpal reduction. Fitting a circle to the contour of the distal radius and next to the proximal pole of the lunate should result in concentric articular contours. If that relationship was altered, we considered the radiolunate joint noncongruent[26] and defined each state as either reduced or subluxated (Figure 3). Based on what was learned in the Pilot Study, two additional measurements (Chamay and Bouman) were made in the second iteration to further evaluate coronal alignment[23-25]. They are demonstrated and described in Figure 4.
Respective measurements were made before and after plate placement using OsiriX Lite (Pixmeo SARL, Switzerland).
Wollstein et al[23] found that the average physiologic lunate overhang with the wrist in neutral deviation ranged from 36% to 44% (radial shaft aligned with the third metacarpal). Lunate overhang greater than 50% was defined as pathologic. A power analysis showed that five patients in each group were needed to find a 6% difference between values with an 80% power and a 95% confidence level.
Comparison of lunate overhang was calculated for the Group A method and Group B method using the nonparametric Mann-Whitney U test, independent sample t-test, and parametric paired samples t-test. All analyses were done using SPSS (Chicago, IL) and significance assigned as P < 0.05.
The mean, median, range, minimum and maximum were calculated for each of the three scores (Chamay, Gilula, and Bouman) preoperatively and postoperatively for the 2M and 3M plating techniques. The Shapiro Wilk test was used to examine normality of distribution and all scores were found to have a normal distribution. Next, the paired sample t-test was used to compare the means of the preoperative and postoperatively scores for all subjects. Similarly, paired sample t-tests were used to compare the means of the postoperative scores of the 2M and 3M plating techniques. Lateral views were evaluated and described as either reduced or subluxated.
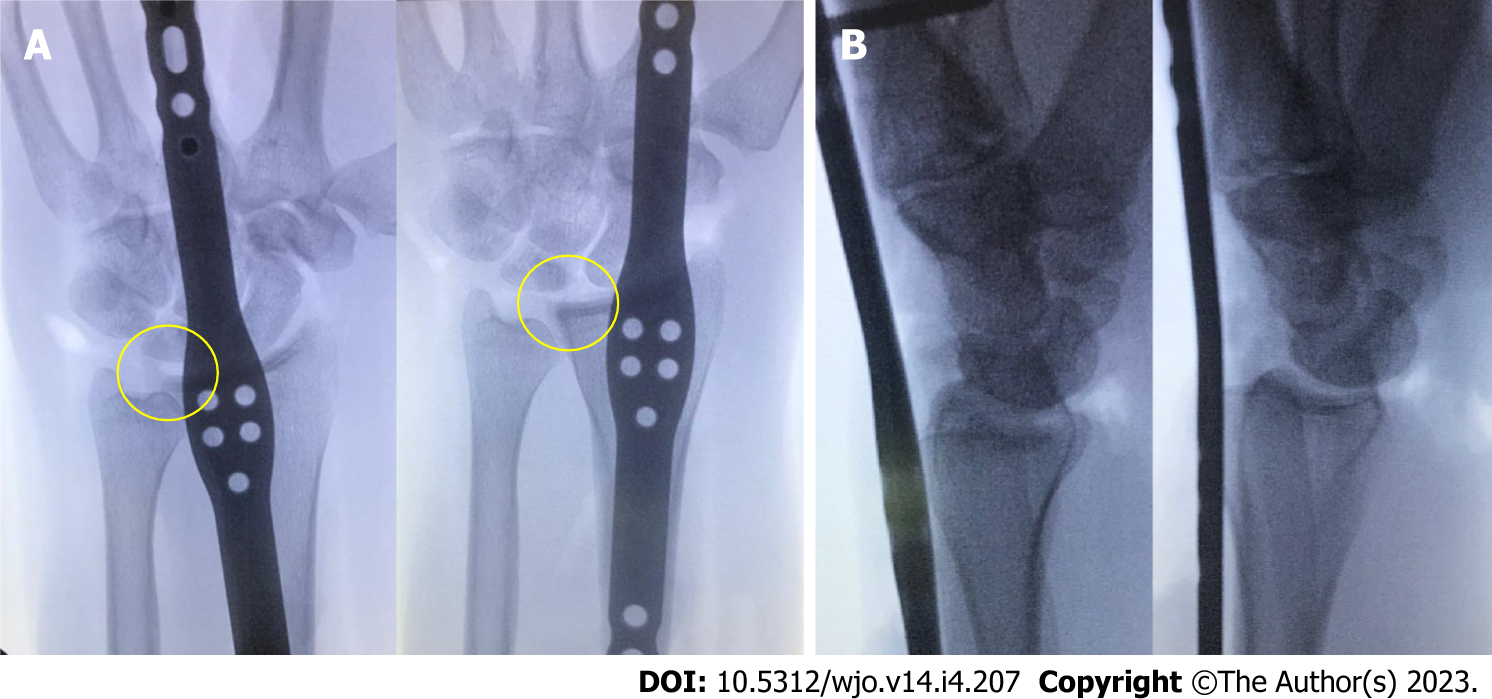
Lunate overhang (Gilula) was 0.29 ± 0.12 mm preoperatively, 0.78 ± 0.20 mm when fixed distally to the second metacarpal, and 0.44 ± 0.19 mm, when fixed distally to the third metacarpal. Paired samples t-test analysis demonstrated a significant difference (P = 0.001) between second and third metacarpal fixation for lunate overhang, with more anatomic alignment associated with third metacarpal plating (Figure 5A).
In addition, we found volar subluxation of the radiocarpal joint in 5 out of 10 specimens (Figure 5B). Each of those cases had the plate applied from the floor of the fourth dorsal compartment to the second metacarpal. None of the specimens that had been plated from the floor of the fourth dorsal compartment to the third metacarpal had volar subluxation of the lunate.
The pre-operative Gilula lunate overhang measurement was 0.32 ± 0.33 mm with a postoperative measurement of 0.4 ± 0.51 mm and 0.33 ± 0.49 mm for the 2M and 3M techniques, respectively. The preoperative Chamay measurement was 0.27 ± 0.11 mm. The postoperative Chamay measurement was 0.25 ± 0.07 mm and 0.27 ± 0.15 mm for the 2M and 3M techniques, respectively. The Bouman measurements were 0.98 ± 0.37 mm preoperatively and for the postoperative measurements for the 2M and 3M techniques, they were 1.02 ± 0.75 and 1.00 ± 0.44, respectively (Table 1).
| Variable | Mean | Median | Maximum | Minimum | Range |
| Preoperative Gilula score | 0.32 | 0.34 | 0.48 | 0.15 | 0.33 |
| 2M Gilula score | 0.4 | 0.38 | 0.68 | 0.17 | 0.51 |
| 3M Gilula score | 0.33 | 0.32 | 0.59 | 0.1 | 0.49 |
| Preoperative Chamay score | 0.27 | 0.28 | 0.32 | 0.21 | 0.11 |
| 2M Chamay score | 0.28 | 0.28 | 0.33 | 0.26 | 0.07 |
| 3M Chamay score | 0.27 | 0.27 | 0.34 | 0.19 | 0.15 |
| Preoperative Bouman score | 0.98 | 0.95 | 1.2 | 0.83 | 0.37 |
| 2M Bouman score | 1.02 | 1.04 | 1.39 | 0.64 | 0.75 |
| 3M Bouman score | 1.00 | 0.98 | 1.23 | 0.79 | 0.44 |
Bridge plating from the second dorsal compartment to the second metacarpal (2M) and from the fourth dorsal compartment to the third metacarpal (3M), resulted in no statistically significant differences in radiocarpal alignment compared to pre-dislocation status, according to the indices of Gilula, Chamay and Bouman, suggesting that each technique could achieve anatomic coronal alignment (Table 2 and Figure 6).
| Chamay | Gilula | Bouman | |
| 2M technique | 0.199 | 0.065 | 0.462 |
| 3M technique | 0.408 | 0.846 | 0.578 |
In all specimens (2M and 3M), lateral alignment was found to be anatomic using the best-fit circle technique.
While there is no consensus for the best fixation strategy for radiocarpal dislocations, it is generally understood that poorer outcomes are associated with inadequate or lost reduction, such as ulnar translocation. It stands to reason, then that anatomic reduction and stable fixation are essential, though not always sufficient, to obtaining a satisfactory clinical outcome. Bridge plating for distal radius fractures has been well-established through multiple biomechanical and clinical studies[26], but its use in radiocarpal dislocations is less understood.
The present study demonstrates that anatomic alignment is achievable with the two most commonly cited techniques for bridge plate fixation–distal fixation to the second metacarpal through the second dorsal compartment and distal fixation to the third metacarpal through the floor of the fourth dorsal compartment–if the techniques are followed carefully.
In addition to those findings, we believe that the Pilot Study results and subsequent analysis are just as relevant. The initial study exclusively used a plate that includes a cluster of screw holes designed to allow for supplemental periarticular fixation without compromising resistance to fatigability across the wrist joint. This design feature, however, results in a wider section of the plate that does not easily facilitate passage through the second dorsal compartment. In testing the concept of distal fixation to the second metacarpal, proximal fixation was essentially set at a single point, leading to mal-reduction of the radiocarpal joint when fixed to the second metacarpal vs the third metacarpal, which included ulnar translocation in nearly every specimen and volar subluxation at least 50 percent of the time. This is consistent with the results found by Azad et al[21] and may at least in part explain their findings. Another design feature, six degrees of dorsal bend, may have contributed to the volar subluxation, but this was found in only 50 percent of the Pilot Study specimens, so its significance is unclear.
The results of the pilot study were carefully studied and led the authors to realize that the second metacarpal fixation model did not accurately reflect the technique as it was originally described[16]. The 2M technique is known for its fixation to the second metacarpal, but it requires passage through the second dorsal compartment and more radial placement proximally on the radial shaft between the ECRB and ECRL tendons in order to maintain alignment. Fixation to the third metacarpal generally assumes passage through the floor of the fourth dorsal compartment and proximal fixation to the more central aspect of the radial shaft[8,17].
Comparing our methods to those of Azad et al[21] reveals that our models and techniques may have differed in significant ways and may explain the different results. Their model appears to have removed the extensor retinaculum in addition to the “dorsal radiocarpal capsuloligamentous structures.” Though they do not specify that the retinaculum was removed, the clinical photo in their article seems to suggest that this structure (and landmark) has been removed, which might obscure proper proximal placement of the plate when performing the 2M technique to the second extensor compartment. In addition, the authors do not specify the nuances of proximal positioning of the plate on the radius, which may introduce the opportunity for coronal and even sagittal malreduction, as we found in our pilot study.
There are advantages and disadvantages to each approach, and advocates have several studies to cite in support of their preferred technique, such as a potential protective advantage against tendon entrapment for the 2M technique[19] or a potential biomechanical advantage for the 3M technique[18].
Based on their collective experience and the results of this study, however, the senior authors encourage surgeons to be comfortable with both techniques, as each may offer different advantages and disadvantages in different scenarios. A larger patient with a heavier arm, for example, may fare better with a larger plate placed along the central axis of the radiocarpal joint and fixed to the third metacarpal. Similarly, in the setting of an unstable fracture pattern that requires multiple fragment-specific implants and supplemental bridge plate fixation, the surgeon may find it easier to pass the plate through the second dorsal compartment to the second metacarpal. And finally, anatomic variations among patients may at times require small changes in technique and bridge plate application.
Modification of the 3M technique in which we attempted to fix the wider plate to the second metacarpal from the floor of the fourth dorsal compartment consistently resulted in less anatomic reduction of the radiocarpal joint in our cadaveric model with observed ulnar translocation, relative supination of the carpus and volar subluxation, even when trying to translate the plate radially within the fourth dorsal compartment (Figure 5A). Such a finding may not be readily observed in the setting of a distal radius fracture in which the ligaments are intact, but our cadaveric model suggests that this modification of the 3M technique may result in non-anatomic alignment and would not be advised.
When choosing to bridge plate a distal radius fracture or radiocarpal dislocation, the treating surgeon is encouraged to carefully follow the technique as it is described by its proponents and understand the design features of their implant and the implications they may have for their chosen technique. Likewise, the surgeon must recognize that anatomic reduction is ultimately the surgeon’s responsibility and should maintain a critical eye for coronal and sagittal alignment, making adjustments as needed to match their patients’ normal anatomy. We suggest that obtaining preoperative contralateral images may help with this assessment, in addition to the various parameters that were used in this study (i.e., Gilula’s lunate uncovering and best-fit circles).
Limitations of this study include the use of an unvalidated cadaveric model of radiocarpal instability. Our model represents a completely unstable joint where the radiocarpal joint capsule and the ligaments have been transected completely. Though this may or may not accurately reflect the true nature of a radiocarpal dislocation in vivo, our model represents an extreme version of instability and demonstrates that in the setting of complete instability, both the 2M and 3M techniques appear to permit anatomic reduction. However, it is possible that in vivo, one technique may more easily facilitate anatomic reduction than the other, perhaps lending some credence to the findings of Azad et al[21], but without a consistent validated radiocarpal dislocation model or clinical studies, we cannot answer that question at this time.
Another potential limitation of this study is that the biomechanical strength of each technique was not tested. Therefore, we cannot comment on whether one technique is better than the other with regards to the stability of the construct; however, the aim of this study was to determine whether anatomic alignment could be achieved regardless of distal fixation, not biomechanical advantage. Compared to intramedullary wires and external fixator placement, bridge plating offers the advantage of maintaining an anatomic reduction throughout the postoperative course given that fixation is more robust and closer to the joint axis. While it has been well studied in biomechanical models of distal radius fractures[26], there is not enough data exploring its use in the setting of radiocarpal dislocations[20,21]. Biomechanical strength may either be extrapolated from the study by Alluri et al[18] or may represent an area of future research.
Further studies will be needed to advance in the understanding of the intricacies of these rare but devastating injuries. The creation of a validated cadaveric model would indeed enable us to compare the biomechanical advantages of one technique over another, as well as to test dorsal spanning plating vs other options such as external fixation or the use of Kirschner wires. Ultimately, in vivo studies will be necessary to evaluate the outcome in a real scenario.
In our cadaveric radiocarpal dislocation model, we found that bridge plating with distal fixation to the third metacarpal may facilitate more anatomic alignment if fixation to the radius through the fourth dorsal compartment is required. However, anatomic alignment and stable fixation can also be achieved with distal fixation to the second metacarpal through the floor of the second dorsal compartment if the technique is followed appropriately. When considering dorsal bridge plate fixation for radiocarpal dislocations, the surgeon is encouraged to understand the nuances of different fixation techniques and how implant design features may influence placement.
Dorsal bridge plate fixation has been described for various settings in the treatment of complex distal radius fractures and can be fixed distally to the second or third metacarpal, but its application for radiocarpal dislocations has not been established.
To determine whether distal fixation to the second or third metacarpal matters.
Using a cadaveric radiocarpal dislocation model, the effect of distal fixation was studied.
Two stages were considered: (1) a pilot study that investigated the effect of distal fixation alone; and (2) a more refined study that investigated the effect of described techniques for distal and proximal fixation. Radiographs were measured in various parameters to determine the quality of the reduction achieved.
The pilot study found that focusing on distal fixation alone without changing proximal fixation results in ulnar translocation and volar subluxation when fixing distally to the second metacarpal compared with the third. The second iteration demonstrated that anatomic alignment in coronal and sagittal planes could be achieved with each technique.
Anatomic alignment can be maintained with bridge plate fixation to the second metacarpal or the third metacarpal if the described technique is followed. When considering dorsal bridge plate fixation for radiocarpal dislocations, the surgeon is encouraged to understand the nuances of different fixation techniques and how implant design features may influence proximal placement.
Further studies will be needed to advance in the understanding of the intricacies of these rare but devastating injuries. The creation of a validated cadaveric model would indeed enable us to compare the biomechanical advantages of one technique over another, as well as to test dorsal spanning plating vs other options such as external fixation or the use of Kirschner wires. Ultimately, in vivo studies will be necessary to evaluate the outcome in a real scenario.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu L, China; Wahid M, United Kingdom S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | Dunn AW. Fractures and dislocations of the carpus. Surg Clin North Am. 1972;52:1513-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 155] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Dumontier C, Meyer zu Reckendorf G, Sautet A, Lenoble E, Saffar P, Allieu Y. Radiocarpal dislocations: classification and proposal for treatment. A review of twenty-seven cases. J Bone Joint Surg Am. 2001;83:212-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 76] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Yuan BJ, Dennison DG, Elhassan BT, Kakar S. Outcomes after radiocarpal dislocation: a retrospective review. Hand (N Y). 2015;10:367-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Singisetti K, Konstantinos M, Middleton A. Volar radiocarpal dislocation: case report and review of literature. Hand Surg. 2011;16:173-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Moneim MS, Bolger JT, Omer GE. Radiocarpal dislocation--classification and rationale for management. Clin Orthop Relat Res. 1985;199-209. [PubMed] [DOI] [Full Text] |
| 6. | Potter MQ, Haller JM, Tyser AR. Ligamentous radiocarpal fracture-dislocation treated with wrist-spanning plate and volar ligament repair. J Wrist Surg. 2014;3:265-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Burke EF, Singer RM. Treatment of comminuted distal radius with the use of an internal distraction plate. Tech Hand Up Extrem Surg. 1998;2:248-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 68] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Ruch DS, Ginn TA, Yang CC, Smith BP, Rushing J, Hanel DP. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. J Bone Joint Surg Am. 2005;87:945-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Ginn TA, Ruch DS, Yang CC, Hanel DP. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. Surgical technique. J Bone Joint Surg Am. 2006;88 Suppl 1 Pt 1:29-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Lauder A, Agnew S, Bakri K, Allan CH, Hanel DP, Huang JI. Functional Outcomes Following Bridge Plate Fixation for Distal Radius Fractures. J Hand Surg Am. 2015;40:1554-1562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Makhni EC, Ewald TJ, Kelly S, Day CS. Effect of patient age on the radiographic outcomes of distal radius fractures subject to nonoperative treatment. J Hand Surg Am. 2008;33:1301-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Ahmad AA, Yi LM, Ahmad AR. Plating of Distal Radius Fracture Using the Wide-Awake Anesthesia Technique. J Hand Surg Am. 2018;43:1045.e1-1045.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 13. | Jiang JJ, Phillips CS, Levitz SP, Benson LS. Risk factors for complications following open reduction internal fixation of distal radius fractures. J Hand Surg Am. 2014;39:2365-2372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 14. | Tinsley BA, Ilyas AM. Distal Radius Fractures in a Functional Quadruped: Spanning Bridge Plate Fixation of the Wrist. Hand Clin. 2018;34:113-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Hyatt BT, Hanel DP, Saucedo JM. Bridge Plating for Distal Radius Fractures in Low-Demand Patients With Assist Devices. J Hand Surg Am. 2019;44:507-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Hanel DP, Lu TS, Weil WM. Bridge plating of distal radius fractures: the Harborview method. Clin Orthop Relat Res. 2006;445:91-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 75] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Richard MJ, Katolik LI, Hanel DP, Wartinbee DA, Ruch DS. Distraction plating for the treatment of highly comminuted distal radius fractures in elderly patients. J Hand Surg Am. 2012;37:948-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Alluri RK, Bougioukli S, Stevanovic M, Ghiassi A. A Biomechanical Comparison of Distal Fixation for Bridge Plating in a Distal Radius Fracture Model. J Hand Surg Am. 2017;42:748.e1-748.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Lewis S, Mostofi A, Stevanovic M, Ghiassi A. Risk of tendon entrapment under a dorsal bridge plate in a distal radius fracture model. J Hand Surg Am. 2015;40:500-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Wahl EP, Lauder AS, Pidgeon TS, Guerrero EM, Ruch DS, Richard MJ. Dorsal Wrist Spanning Plate Fixation for Treatment of Radiocarpal Fracture-Dislocations. Hand (N Y). 2021;16:834-842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Azad A, Choi JT, Fisch R, Gipsman A, Nicholson LT, Ghiassi A. Wrist-Spanning Fixation of Radiocarpal Dislocation: A Cadaveric Assessment of Ulnar Translation. Hand (N Y). 2021;16:482-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Medoff RJ. Essential radiographic evaluation for distal radius fractures. Hand Clin. 2005;21:279-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 241] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 23. | Wollstein R, Wei C, Bilonick RA, Gilula LA. The radiographic measurement of ulnar translation. J Hand Surg Eur Vol. 2009;34:384-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Pirela-Cruz MA, Firoozbakhsh K, Moneim MS. Ulnar translation of the carpus in rheumatoid arthritis: an analysis of five determination methods. J Hand Surg Am. 1993;18:299-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Borisch N, Lerch K, Grifka J, Haussmann P. A comparison of two indices for ulnar translation and carpal height in the rheumatoid wrist. J Hand Surg Br. 2004;29:144-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Wolfe S. Distal Radius Fractures. In: Wolfe S, Pederson W, Kozin SH, eds. Green’s Operative Hand Surgery. 6th ed. Elsevier; 2010:567. |