Published online Apr 18, 2023. doi: 10.5312/wjo.v14.i4.171
Peer-review started: December 11, 2022
First decision: January 9, 2023
Revised: January 22, 2023
Accepted: March 31, 2023
Article in press: March 31, 2023
Published online: April 18, 2023
Processing time: 127 Days and 15.8 Hours
Over the years, several studies demonstrated the crucial role of knee menisci in joint biomechanics. As a result, save the meniscus has become the new imperative nowadays, and more and more studies addressed this topic. The huge amount of data on this topic may create confusion in those who want to approach this surgery. The aim of this review is to provide a practical guide for treatment of meniscus tears, including an overview of technical aspects, outcomes in the literature and personal tips. Taking inspiration from a famous movie directed by Sergio Leone in 1966, the authors classified meniscus tears in three categories: The good, the bad and the ugly lesions. The inclusion in each group was determined by the lesion pattern, its biomechanical effects on knee joint, the technical challenge, and prognosis. This classification is not intended to substitute the currently proposed classifications on meniscus tears but aims at offering a reader-friendly narrative review of an otherwise difficult topic. Furthermore, the authors provide a concise premise to deal with some aspects of menisci phylogeny, anatomy and biomechanics.
Core Tip: Several studies investigated the effects of a meniscus tear and its optimal treatment. This review aims at providing a practical guide on this topic, including an overview of technical aspects, outcomes in the literature and personal tips.
- Citation: Simonetta R, Russo A, Palco M, Costa GG, Mariani PP. Meniscus tears treatment: The good, the bad and the ugly-patterns classification and practical guide. World J Orthop 2023; 14(4): 171-185
- URL: https://www.wjgnet.com/2218-5836/full/v14/i4/171.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i4.171
Meniscal tears are among the most common injuries of the knee, significantly impacting on the healthcare annual expense[1-4]. It has been estimated that the frequency of arthroscopic procedures for treating meniscus tears is increased by 49% during the 1990s and 2000s[5], but it could reasonably be further expanded in the last years.
Historically, menisci were considered as vestigial remnants, with no significant impact on knee biomechanics[6]. As a result, total meniscectomy was considered the most valuable option for a long time. McMurray[7] claimed insufficient meniscus removal was the main cause of failure of meniscectomy. In 1948, Fairbank[8] reported the clinical outcomes of 107 patients after total meniscectomies and found degenerative knee changes in most of them. From then, several other studies demonstrated the detrimental effects of total meniscectomies on knee joint[9-13]. These studies significantly changed the treatment approach of meniscus tears. Feeley and Lau[14] proposed an algorithm to approach arthroscopic partial meniscectomy starting from the concept of maintaining as much meniscal tissue as possible. The authors quantified as 60% as the maximum amount of meniscus tissue that can be sacrificed. However, this concept can be questioned, since not only the size of the tears but also the location was proved to significantly affect the outcomes[15]. Save the meniscus has become the new imperative nowadays[16,17]. Several studies addressed this topic over many years, but the huge amount of data may create confusion in those who want to approach this surgery.
The aim of this paper is to provide a practical guide for treatment of meniscus tears, including an overview of technical aspects, outcomes in the literature and personal tips. Furthermore, the authors provide a concise premise to deal with some aspects of menisci phylogeny, anatomy and biomechanics. This can be useful for the reader to fully understand the factors affecting the fate of a meniscus tear.
The knowledge of meniscus phylogeny and ontogeny can be useful to correlate meniscal gross anatomy to meniscal function.
Knee menisci are not unique to humans but can be found in several living tetrapods, including amphibians, reptiles, birds and mammals. In most of them, both menisci are massive structures fitted between the tibial and femoral surfaces and are connected anteriorly by an intermeniscal ligament. Only in mammals, regardless of the walking style or size, the menisci have the same semilunar shape[18]. The medial meniscus is very similar in all mammals, including primates. It is crescent shaped with two tibial insertions. By contrast, the lateral meniscus is more variable in shape and in the pattern of tibial insertions[19,20]. The presence of a double tibial insertion of the lateral meniscus is a particular feature of Homo sapiens, unique among living mammals. The second posterior insertion aids in preventing extreme anterior gliding of the lateral meniscus during frequent extension[21]. The presence of meniscofemoral ligaments reinforces the posterior fixation of the lateral meniscus, providing better stability. As a result, only humans are able to maintain a stable knee extension during bipedal stance. Other nonhuman primates cannot do likewise in bipedal walking, but only during quadrupedal gait. Therefore, humans’ menisci are not only simple load distributers, but provide a fundamental contribution to knee stability during bipedal stance.
In humans, the meniscus is identifiable after about 8 wk[21,22], assuming its characteristic shape already at this stage. At no time the lateral meniscus takes a discoid shape. In the prenatal stage, the meniscus is highly cellular with a large nuclear/cytoplasmic ratio. Blood vessels are numerous throughout the substance of the foetal meniscus, mostly along the capsular attachment sites. The main postnatal change is the progressively decreasing vascularity and cellularity, with concomitant increase in collagen content[22].
The menisci are two fibrocartilaginous structures mainly composed of water (65%-75%), type I collagen (22%) and glycosaminoglycans (approximately 1%)[23]. The collagen bundles are combined in different orientations to oppose compressive, radial, and shear stresses. Specifically, radial bundles are more frequent in the inner part, which is more resistant to compression forces. Conversely circumferential bundles are mainly located in the outer two-thirds part of the meniscus, counteracting to radial tension forces. This may explain why radial tears typically start from the inner portion, whereas longitudinal tears are more frequent in the most peripheral zones of the meniscus[24]. Furthermore, fiber orientation affects the tensile properties of suture configurations. Vertical sutures showed a significantly higher pull-out strength than horizontal sutures[25-27]. It was assumed that vertical sutures captured more circumferential collagen fiber, thus providing higher failure strength. A third group of collagen fiber are located among the circumferential bundles and are called “tie fibers”. These fibers are radially orientated, thus opposing to longitudinal splitting forces[24].
The medial meniscus has a stable fixation to the tibia due to the anterior and posterior root attachments, the meniscotibial (coronary) ligament around the entire perimeter of the meniscus and the deep medial collateral ligament. In 1998, Berlet and Fowler[28] described four distinct insertion patterns of the anterior horns of the medial meniscus. The type I insertion is the most common and seems to provide a very strong fixation to the tibia into the flat area called crista areae intercondylaris anterior by Jacobsen[29]. The type II insertion also provide a firm fixation, but more medially and closer to the articular surface. Type III insertion is very anterior and, even if firm, provides little resistance to anterior motion of the meniscus. The last one, type IV, has no firm fixation on the tibia, and the displacement of the anterior horn of the meniscus is controlled by coronary fibers. The superior part of the medial meniscus body is attached to the synovial tissue. In the posterior horn of the medial meniscus, the superior edge does not attach to the joint capsule, while the inferior part attaches to the tibia through the meniscotibial ligament. This ligament, together with the posterior joint capsule, forms the posteromedial femoral recess, defined as ramp area. The semimembranosus attachment to the posterior capsule seems to have a role on the pathogenesis of meniscus tears in this area. A fixation of the medial posterior horn to the capsule may potentially have an influence on the mobility of the medial meniscus, which subsequently might be responsible for poor long-term follow-up. A strictly anatomic medial meniscus repair with reconstruction only of meniscotibial attachment should be to be considered.
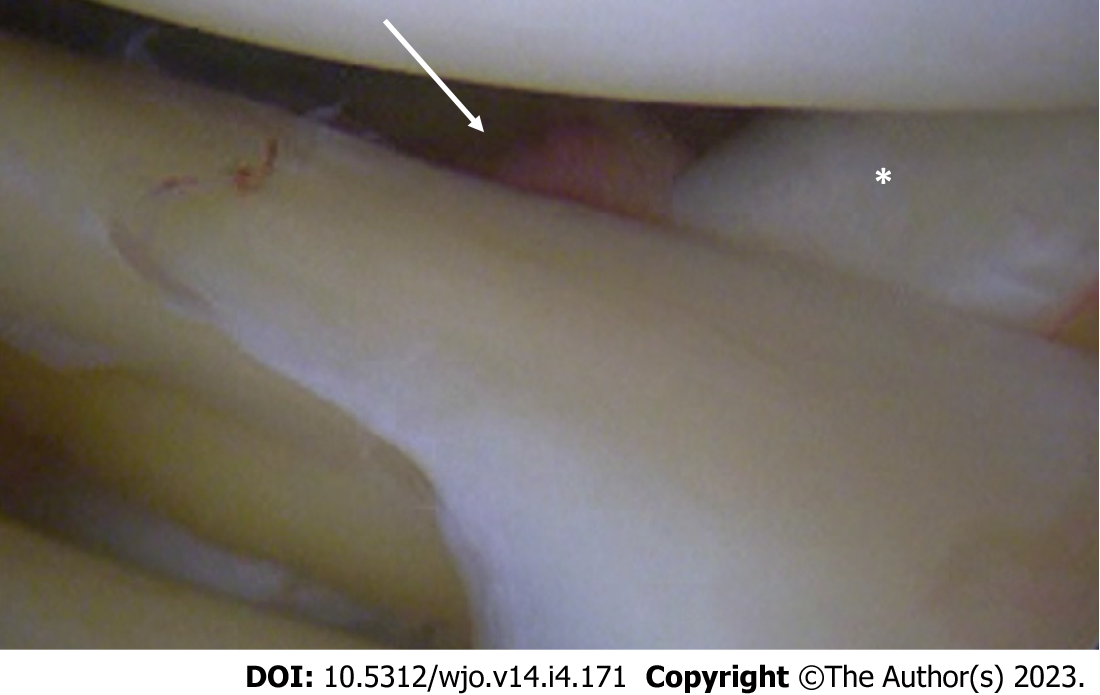
The lateral meniscus has a looser attachment to the tibia and joint capsule, because of the presence of the hiatus popliteus. In this zone, the popliteomeniscal fascicules connect the lateral meniscus to the popliteus tendon and the joint capsule. An injury or the absence of such fascicules in discoid meniscus variations may produce an unstable tear causing a symptomatic meniscus hypermobility[30] (Figure 1). Posteriorly, lateral meniscus root attachment is reinforced by one or two meniscofemoral ligaments. These ligaments seem to have a significant contribution in preventing lateral meniscus extrusion[31].
Menisci vascularization is another important factor affecting the healing process. The major vascular support to the meniscus comes from the branches of superior and inferior geniculate arteries that make a subsynovial and perimeniscal capillary network infiltrating the periphery of the meniscus. Vascular supply is limited to the peripheral 10%–25% for the lateral meniscus and 10%–30% for the medial meniscus[32], but it seems to be wider in younger individuals[33]. Vascular penetration is fairly homogeneous in the lateral meniscus, whereas there is more variation within the medial meniscus, with the medial posterior horn having a significantly smaller vascularization[33]. According to the vascular supply, three different zones can be detected within the menisci: The red-red zone (the most peripheral and vascularized zone), the red-white zone (at the inner border of the vascularized zone) and the white-white zone (the inner and avascular zone)[32]. Evidently, tears in the most vascularized zones have higher healing potential and are amenable for repair, while tears in the inner portion are frequently subject to meniscectomy.
Nerve fibers follow closely the blood vessels in their course, with the vascular outer third of the menisci being the most innervated portion[34].
Menisci play a critical role in load distribution, protecting the smooth hyaline cartilage on both the distal femur and proximal tibia. The medial meniscus covers up to 50%–60% of the medial tibial plateau[35], and it is responsive of about 50% of load transmission in the medial tibiofemoral compartment[36]. The lateral compartment is less congruent, since the lateral tibial plateau has a more convex morphology when compared to the medial compartment. For that reason, the lateral meniscus has a higher contribute to ensure joint congruency, transferring up to 70% of load in its compartments[37]. Indeed, lateral meniscectomy result in worse clinical and radiological outcomes than medial meniscectomy[38].
Menisci also provide a fundamental contribute to joint stability. Specifically, the medial meniscus has been shown to be a secondary restraint to anterior translation of the tibia[39], while the lateral meniscus notably restrains tibial rotation and the pivot-shift mechanism[40]. Both medial and lateral menisci translate posteriorly on the tibial plateau during deep knee flexion. The posterior translation of the lateral meniscus (8.2 ± 3.2 mm) is greater than that of the medial one (3.3 ± 1.5 mm)[41]. This asymmetry of kinematics between the medial and lateral compartment is an established characteristic of human knees, resulting in an internal rotation of the tibia relative to the femur with increasing flexion.
At last, menisci are also thought to play roles in knee joint lubrication and nutrient distribution as well as knee proprioception[42,43].
An ideal classification system should be simple, all-inclusive, reliable, reproducible, and treated-oriented[44]. Actually, numerous classifications of meniscus tears have been described, but the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine classification is most widely adopted[45,46]. It is based on tear depth, pattern, length, location and rim width, as well as quality of meniscal tissue. However, some important factors are missing, including prognosis of the lesion pattern.
Taking inspiration from a famous movie directed by Leone and Tigani[44], the authors classified the meniscus tears in three categories: The good, the bad and the ugly lesions. The inclusion in each group was determined by the type of injury, its biomechanical effects on knee joint, the technical challenge, and the prognosis. The meniscus tear patterns included in each cluster and the related treatment proposed by the authors are resumed in Table 1. This classification is not intended to substitute the currently proposed classifications on meniscus tears but aims at offering a reader-friendly narrative review of an otherwise difficult topic.
| Suggested treatment | Secondary treatment | |
| Good lesions | ||
| Stable longitudinal tears | Repair of peripheral tears | Peripheric small tears of the lateral meniscus can be left in situ because of the low risk of subsequent meniscectomy |
| Small flap tears | Partial meniscectomy of small lesions in the avascular zone of the meniscus | |
| Bad lesions | ||
| Bucket handle tears | Repair with dedicated technique according to the lesion features | Meniscectomy of isolated medial bucket handle tears must be discussed with patients |
| Ramp lesions | Conservative treatment should be considered as first-line for degenerative tears | Surgical treatment of degenerative tears should be considered when conservative approach failed or in presence of mechanical symptoms |
| Lateral posterior root tears | ||
| Degenerative tears (big flap tears, horizontal tears, complex tears) | ||
| Ugly lesions | ||
| Radial tears | Repair must be attempted aiming at preserving meniscus function | Valgus or varus osteotomy needs to be considered in case of limb malalignment |
| Medial posterior root tears | ||
| Anterior root tears |
Small stable longitudinal tears (both partial and full thickness tears), as well as small oblique/flap tears can be classified as good lesions. This is mainly due to the poor impact on knee biomechanics[10], both in terms of maximum contact pressure and tibial contact area changes. However, if the tear is more than 15 mm and involves the posterior horn of the meniscus, a significant change of knee biomechanics has been reported[47]. Moreover, longitudinal tears were found to decrease the in-situ meniscus force[48], thus potentially impacting on meniscus function. In addition to this, longitudinal tears of medial meniscus were significantly correlated with meniscus extrusion[49], especially if the tear size increases. Probably, the same traumatic force causing longitudinal meniscus tears may produce a concomitant meniscotibial ligament lesion, which has been closely related to meniscus extrusion[50]. As a result, such lesions should not be overlooked because if they become larger, the knee functionality may be irreversibly impaired.
Either partial meniscectomy or arthroscopic repair can be performed, depending on the tear location and according to the vascular zones of the meniscus. A meta-analysis comparing meniscus repair and meniscectomy found better functional scores in the first group, but meniscectomy for unstable lesions in the white-white zone offered better short-term outcomes and a lower revision surgery rate[15]. The indication for surgical repair of small stable lesions in the peripheric zone of the medial meniscus is almost mandatory, due to the high risk of secondary meniscectomy if left alone[51]. On the other hand, for the lateral meniscus with peripheric small stable lesions, “leave the meniscus alone” can be the preferred approach given the low risk of subsequent meniscectomy[52].
Recent systematic reviews confirmed the good healing potential, regardless of the surgical technique[53,54]. Meniscal zones and timing from trauma have been reported as predictors of meniscal repairs outcomes[55,56]. Even arthroscopic repair of the meniscus tear in the red-white zone of the meniscus showed low failure rates[57]. Biological enhancements like platelet-rich plasma and bone marrow mesenchymal stem cells were found to improve the healing process in the white-white zone in canine models[58], but these data need to be confirmed in clinical setting. Once again, location would seem to affect outcomes, since lateral meniscus repairs showed lower failure rate than medial repairs[15]. There is still controversy regarding the influence of patients’ age on failure rate[59]. This is probably because cartilage status as well as activity level may play a more significant role[60].
The bad lesions are defined as tears causing a significant loss of meniscus function and significantly altering knee biomechanics. However, prognosis can be good when promptly treated. Big longitudinal tears, bucket-handle tears, ramp lesions, posterior lateral root tears and complex degenerative tears can be included in this group.
Large longitudinal tears worth being counted among bad lesions for the biomechanical reasons stated above[47-49]. Arthroscopic repair of such lesions is to be attempted, since meniscectomy would result in great loss of meniscus function[14]. Bucket-handle tears are peculiar longitudinal tears with unstable fragment causing pain and mechanical symptoms. A particular variant is the ‘‘hypermobile lateral meniscus’’, that is a very peripheral longitudinal tear causing the detachment of the lateral meniscus from the capsule in the region of the popliteus tendon hiatus. Traumatic or microtraumatic rupture of the meniscopopliteal fascicles is called upon, allowing excessive meniscal mobility[30,61]. High index of suspicion is needed because diagnosis can be easily misled with the magnetic resonance imaging (MRI).
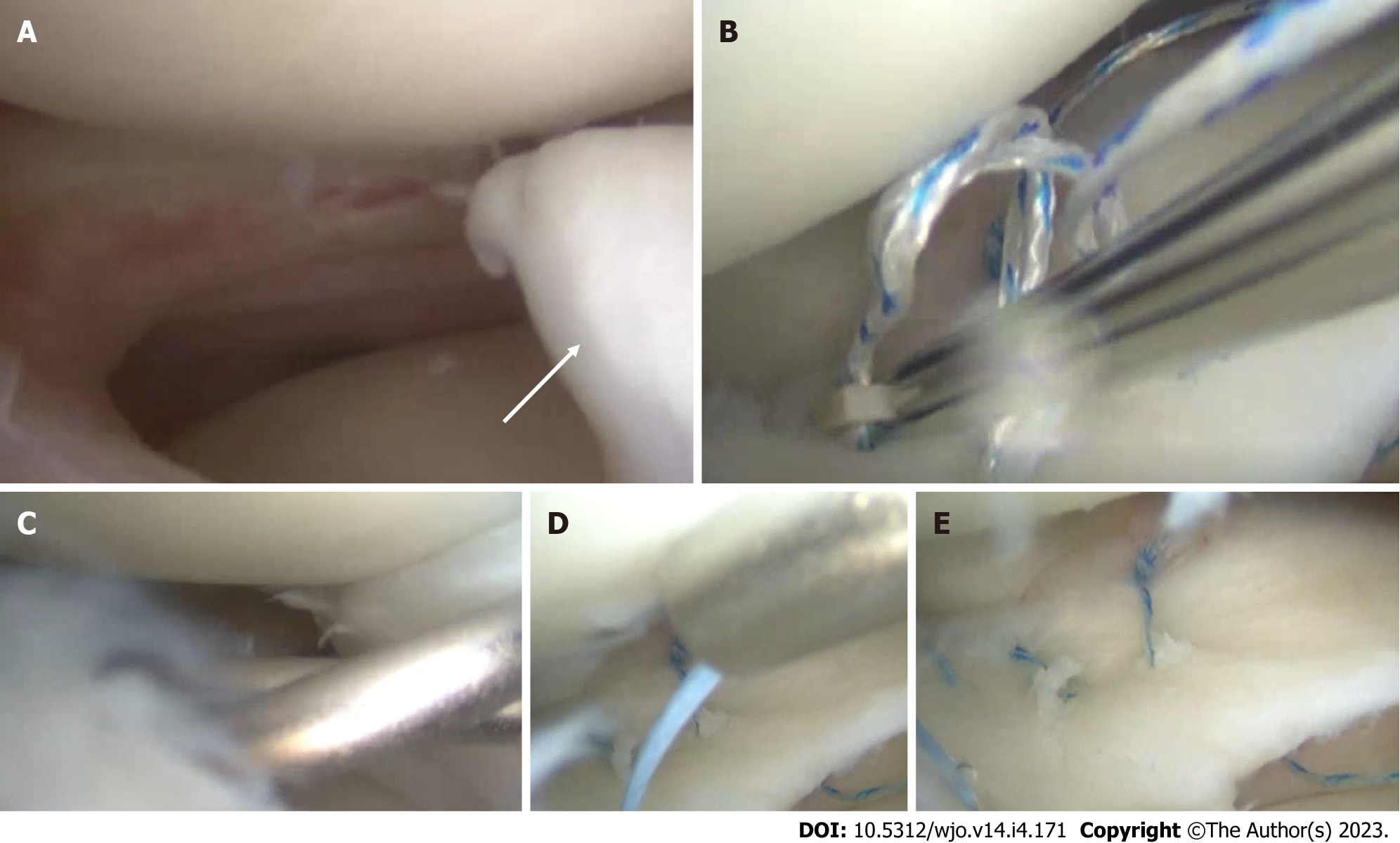
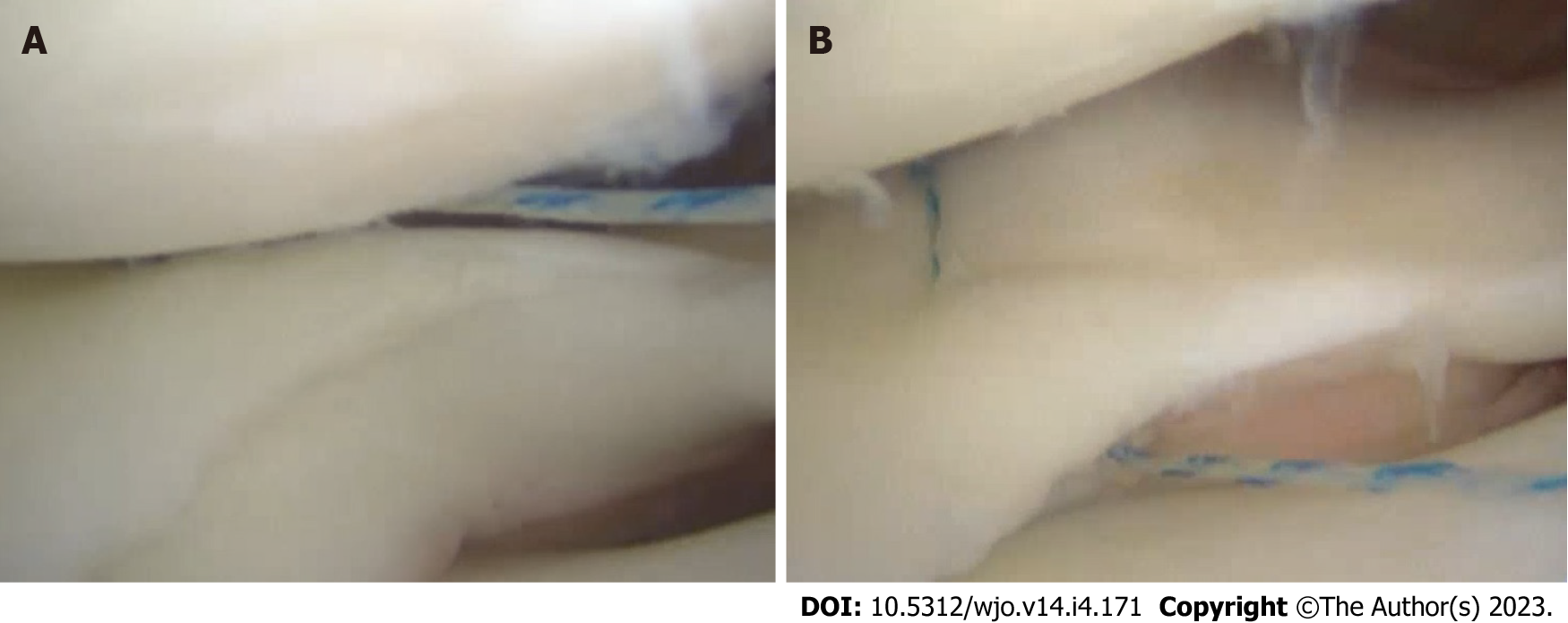
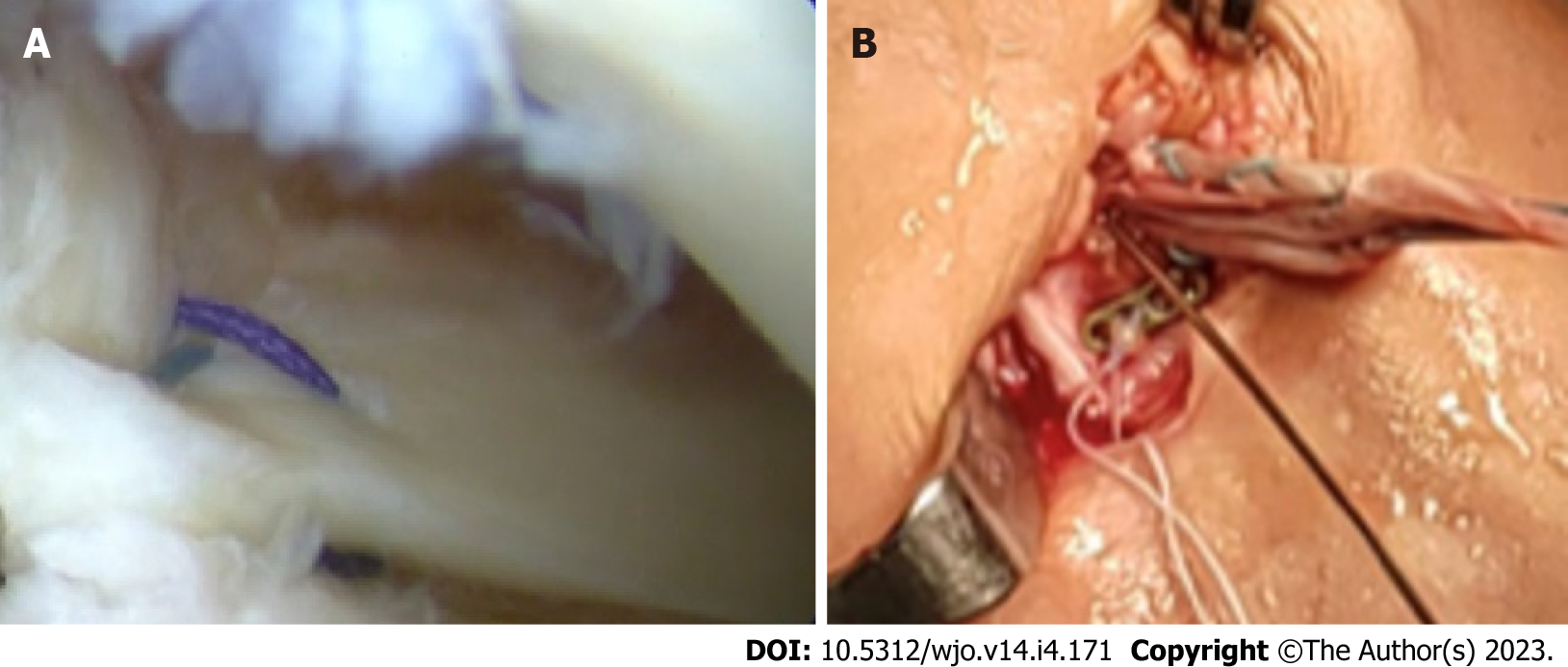
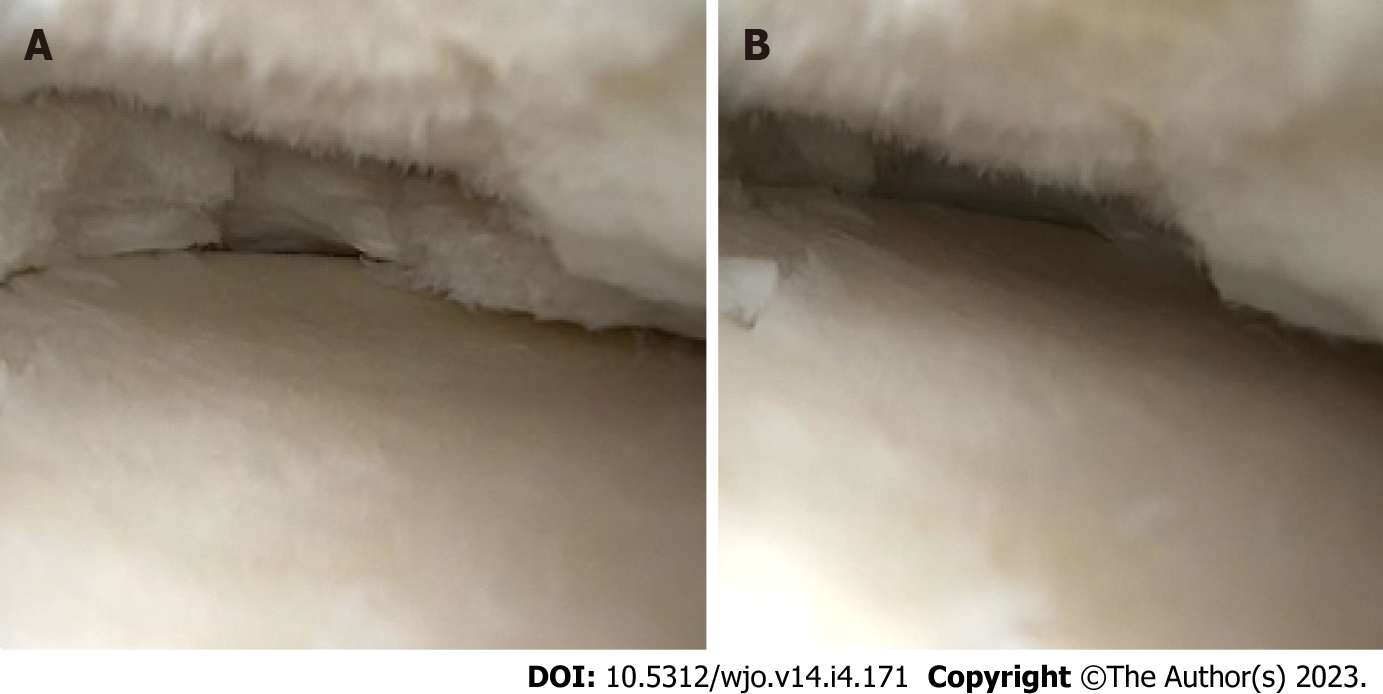
Preservation of the meniscal tissue is of utmost importance in this setting. Resection of bucket-handle tears drastically increases the mean and peak contact pressures in both medial and lateral tibiofemoral compartments, whereas arthroscopic repair of a bucket-handle tear more closely restores native tibiofemoral biomechanics[62]. However, the healing process of bucket-handle tears can be challenging because of the size and the complexity of the lesion[15]. A recent meta-analysis[63] showed that failure rate after arthroscopic bucket-handle meniscus tears repair ranges between 11.3%-18.3%, that is significantly higher than longitudinal tears. Medial tears and isolated tears are found to significantly increase the risk of failure within 2 years[63]. On the other hand, higher is the number of stitches, lower is the risk of failure[63]. Literature supports arthroscopic repair of such lesions, especially the bucket-handle tears of the lateral meniscus and during concomitant anterior cruciate ligament (ACL) reconstruction[16,17]. A combination of all suture techniques (all-inside, inside-outside and outside-inside) is desirable to improve the mechanical strength of the repair (Figure 2). The use of vertical sutures every 5 to 7 mm is preferred, because horizontal sutures are placed parallel to the meniscus collagen fibers and can easily pull out by separating such fibers. Either circumferential compression sutures[64] with dedicated devices or double-sided all-inside suture repair[65] (both in the superior and in the inferior surface of the meniscus) can produce overall compression of the tear, thus promoting complete healing (Figure 3). Isolated medial meniscus bucket-handle tears pose a treatment dilemma with no easy solution[66]. The good short-term outcomes as well as the high return-to-play rates after partial meniscectomy must be balanced against the long-term degenerative consequences. Patient’s age and activity level need to be taken into consideration. The decision to perform either a meniscectomy or a repair must be made in agreements with the patient, discussing risks and benefits of each option.
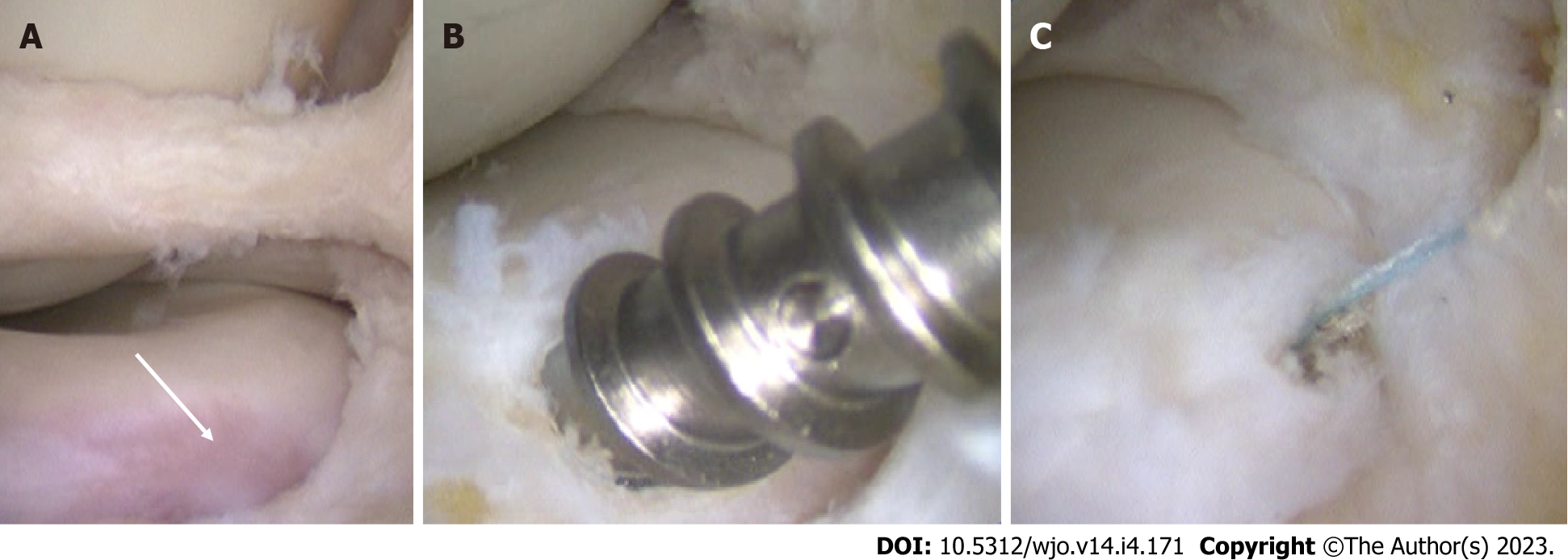
Ramp lesions represent a further variant of bad lesion. These longitudinal peripheral tears of the posterior horn of medial meniscus produce a meniscocapsular or meniscotibial disruption, increasing the anterior tibial translation, internal and external rotation, and the pivot shift in ACL-deficient knees[67]. An isolated ACL reconstruction cannot adequately restore native tibiofemoral biomechanics but requires concomitant meniscocapsular and meniscotibial repair[67]. Furthermore, it has been reported that unrepaired ramp lesions may evolve in medial bucket handle meniscus tears at long-term follow-up[68]. As a result, a proper diagnosis and treatment of such lesion is fundamental. However, this type of injury can be often missed, both during MRI reading and due to its "blind" point of arthroscopic vision. It is crucial to perform a systematic exploration of the posteromedial compartment of the knee using a specific trans-notch approach. As these lesions occur in a well-vascularized zone of the meniscus, small (less than 10 mm) and stable tears may be amenable to trephination alone[69]. For unstable tears, arthroscopic repair is recommended. Reported failure rates range between 2.6% and 12.0%[70]. Several surgical techniques have been proposed, including inside-outside technique[71], all-inside[72] technique with standard devices introduced from the anterior portals, and all-inside technique using a suture hook[73] introduced from a posteromedial portal (Figure 4). The type of suture would seem associated with failure of the ramp lesion repair, with a significantly higher risk with the all-inside device than with suture hook repair sutures[74]. A hybrid repair is recommended in large lesions involving the most medial part of the ramp area in order to enhance structural stability[75]. Even the suture material has been called into question, and an absorbable monofilament suture is advocated for such repair to reduce the risk of failure[70].
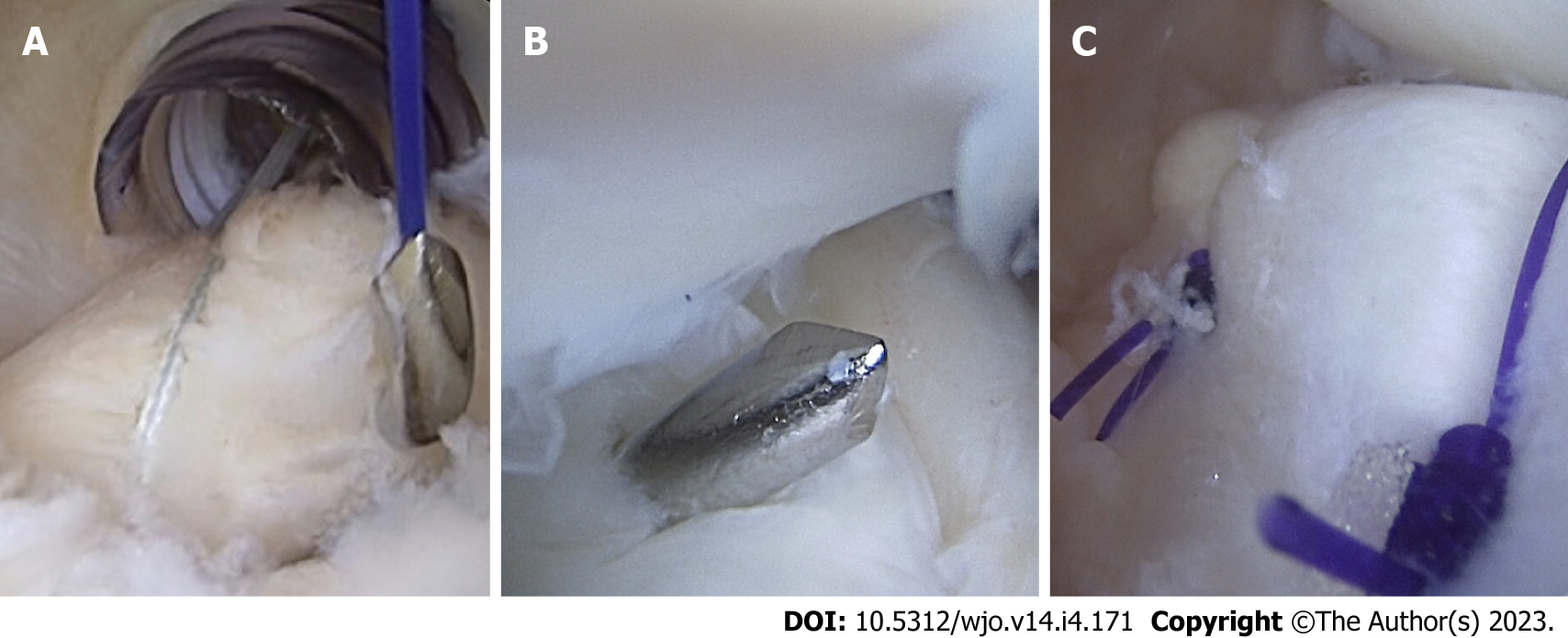
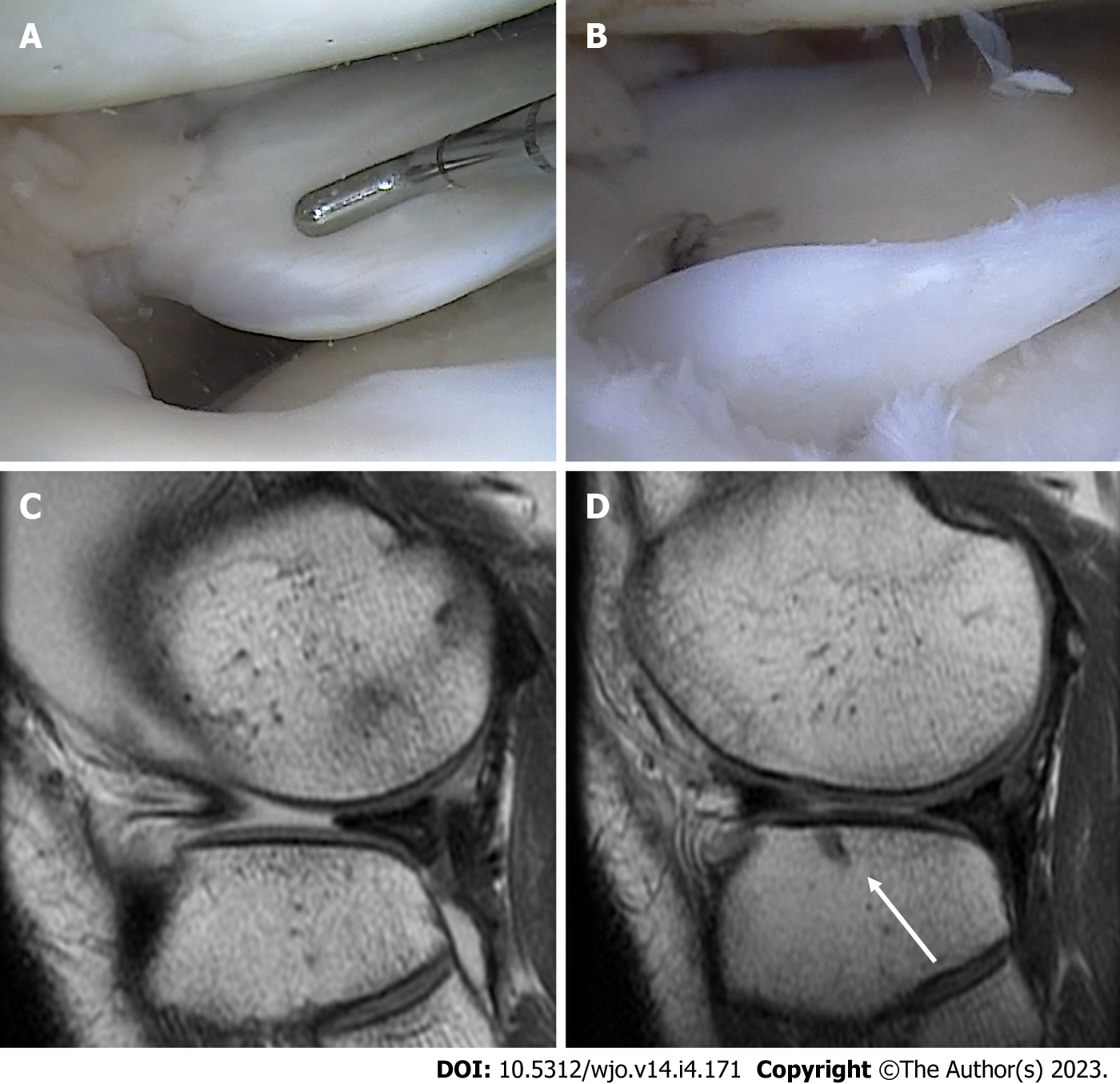
Lateral meniscus posterior root tear (LMPRT) is a further bad lesion typically occurring in ACL-deficient knees. Such lesions create altered load distribution and transmission functions[76], also contributing to increase anterior tibial subluxation of the lateral compartment[77]. Compared with the medial ones, LMPRTs occur in younger male patients with lower body mass index, less cartilage degeneration and less extrusion on MRI. The better functional outcomes after LMPRTs repair than medial root repair suggest that differences in injury and patient characteristics may contribute to differences in these results[78,79]. Repair of LMPRT can be performed with a side-to-side reconstruction or a trans-tibial pull-out technique, according to the type of the lesion. If the repair occurs during concomitant ACL reconstruction, the risk of convergence of the posterior root tunnel and the tibial ACL tunnel is high. Some authors recommend drilling the meniscal root tunnel from the anterolateral tibia[80]. Other authors suggest using the ACL tunnel to fix the meniscus suture[31] (Figure 5). A personalized technique using a suture anchor[81] was previously described, in order to eliminate this risk in selected cases.
The list of the bad lesions is completed with complex tears, that are a combination of different degenerative tear patterns including oblique tears, big flaps and horizontal cleavage of the meniscus. These lesions are counted among this group because they can be indicators of early-stages osteoarthritis. Knee malalignment, obesity and functional overloading may be responsive for degenerative meniscal matrix changes, thus leading to meniscal fatigue, loss of function and extrusion. Such lesions in their turn further undermine knee joint, by increasing peak compressive and shear stress of both cartilages and menisci[82]. Degenerative tears of the medial meniscus seem to have a greater impact on knee biomechanics, by inducing larger stress and extrusion than the lateral meniscal tears[82]. There is a consensus in the literature promoting conservative treatment as the first-line approach for such lesions[83,84]. This should include activity modification, intra-articular injections, physical therapy with specific rehabilitation, gait analysis and supportive orthoses[85-87]. Surgical treatment is recommended only in case of pain no longer responsive to medical therapy or in presence of mechanical symptoms, such as clicking or briefly locking knees. Surgical indication must be confirmed with radiographic and MRI investigation, to rule out signs of advanced osteoarthritis, meniscal extrusion, extensive cartilage damage or bone marrow lesions, which may negatively impact on arthroscopy outcomes. Due to the degenerative nature of the lesion and the poor biological potential of healing, arthroscopic partial meniscectomy has been recommended as the main surgical option. Partial meniscectomy should be limited to the unstable fragments but preserving as much healthy meniscal tissue as possible. A complete resection of such tears would subsequently result in a subtotal meniscectomy, further accelerating the joint degenerative process[82]. This also applies in case of degenerative horizontal tears. In a biomechanical study on 10 cadaveric knees, both single leaflet and double leaflet resection was found to significantly reduce contact area and increase contact pressure in the knee[88]. Only a suture repair of such horizontal cleavage tears returns the contact area and contact pressure to nearly normal[88]. As a result, the repair of such lesions is recommended using a vertical mattress stitch configuration following minimum edge resection, if the quality of the meniscal tissue is adequate[89]. Biological augmentation has been proposed in the literature to enhance healing potential of such degenerative lesions[90,91], but further studies with higher methodologic quality are needed to confirm this option.
The ugly lesions represent the worst scenario for knees, since this group include meniscus tears with the poorest prognosis. All meniscus injuries causing a damage of the meniscus ring are considered ugly lesions, because the interruption of this structure means a complete loss of meniscal function.
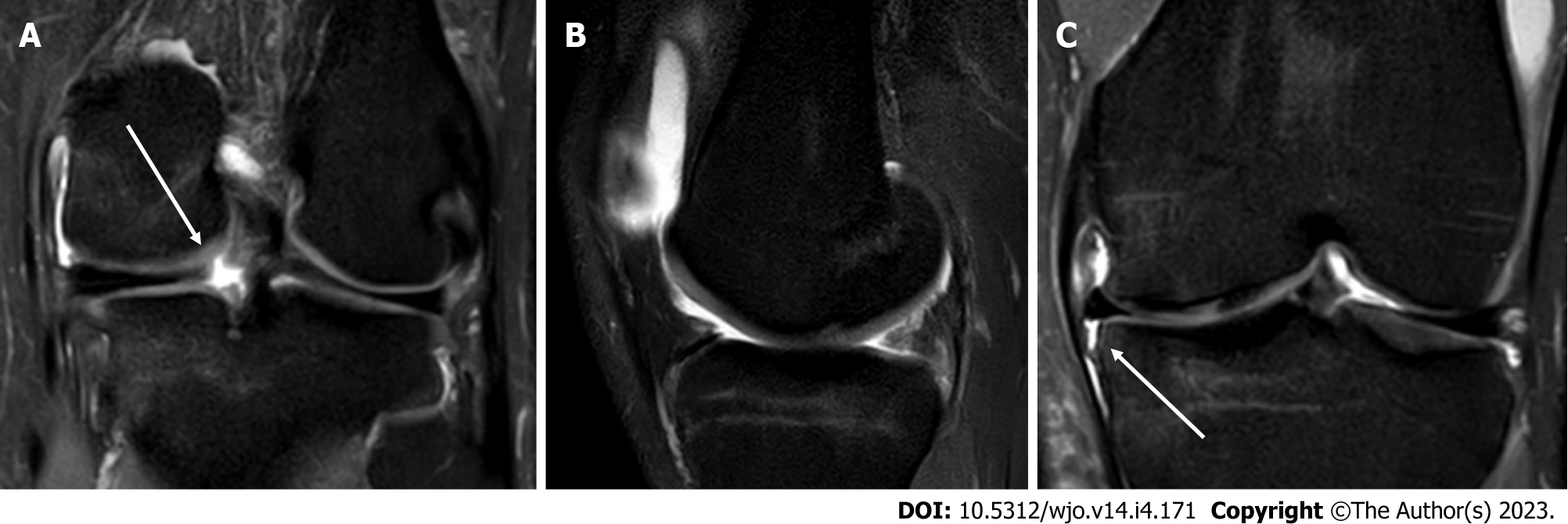
Radial tears represent the first type of ugly lesions, because create unfavourable knee dynamic contact mechanics that are not significantly different from those resulting from meniscectomy[11,76] (Figure 6 and Video 1). Such lesions seem to have a lower potential for healing than longitudinal tears[92]. Despite this, the focus on preservation of meniscal tissue has become increasingly imperative even in this context. This has led to the emergence of several arthroscopic repair techniques. Inside-outside or outside-inside horizontal repairs have been considered for long time as the gold standard. However, a recent systematic review demonstrated that a combination of all-inside horizontal or crossed stitches reinforced with suture parallel to the tear as ripstop (defined as hashtag or crosstag technique, respectively) may improve the repair strength[93]. Radial meniscus tear repairs can be further strengthen by creating a transtibial tunnel augmentation[93]. Even a suture anchor can be used to reinforce the radial meniscus repair (Figure 7), but biomechanical data are needed to confirm the validity of this technique.
Medial meniscus posterior root tears (MMPRTs) represent a further variant of ugly lesions. This is because creates an interruption of the meniscus ring with subsequent effects on knee kinematics, load transmission and stability[94-96]. In addition, this injury can be responsive of meniscus extrusion[94] (Figure 8), thus leading to a complete meniscus loss of function. Differently to LMRTs, the medial tears are typically associated with high-grade chondral lesions and severe varus knee alignment, which are well-recognized risk factors for poor outcomes[78,97]. According to the current literature, MMPRT repairs result in favourable clinical improvements, but meniscus extrusion seems not to be significantly reduced[98]. Furthermore, the progression of joint degeneration seems to not be completely prevented[98]. The arthroscopic meniscus centralization associated with MMPRT repair has been proposed (Figure 9), resulting in good short terms outcomes and significant reduction of extrusion distance[99]. However, the beneficial long-term effects have yet to be demonstrated. In such circumstances, surgeons’ efforts should not only focus on the meniscus tear, but also on limb alignment. A concomitant valgus osteotomy needs to be considered in cases of severe varus knees. This has been demonstrated to improve meniscus healing process, although clinical and radiological outcomes seem not to significantly differ from isolated valgus osteotomies[100].
Medial and lateral anterior root tears need a separate mention. Injuries to the anterior root of the menisci are less common and frequently iatrogenic, such as during arthroscopic portals creation, ACL tibial tunnel reaming or tibial nailing for traumatic fractures[96]. In the authors’ experience, medial anterior root tear can be associated with medial bucket-handle tear (Figure 10). As a result, the biomechanical effect of such lesions remains unclear. Although most of the reported literature refers to posterior meniscal root tears, it would stand to reason that anterior root tears will have the same fate if not anatomically repaired. Repair of such lesions can be extremely challenging. Anatomical tibial tunnel positioning or the use of suture anchor can be needed. The creation of accessory portals and the use of dedicated devices can make the procedure easier.
This review aims at representing a practical and updated guide for treatment of meniscus tears. Several factors should be considered when approaching meniscus surgery. Biomechanical aspects, technical challenges and long-term outcomes need to be considered before deciding the most appropriate therapeutic approach. Further biomechanical studies as well as rigorous clinical research with high methodologic quality are welcome to improve the current knowledge on this fascinating but challenging topic.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Itthipanichpong T, Thailand; Tang G, China S-Editor: Fan JR L-Editor: A P-Editor: Yuan YY
| 1. | Baker BE, Peckham AC, Pupparo F, Sanborn JC. Review of meniscal injury and associated sports. Am J Sports Med. 1985;13:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 197] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39:1338-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 486] [Cited by in RCA: 482] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 3. | Mather RC 3rd, Garrett WE, Cole BJ, Hussey K, Bolognesi MP, Lassiter T, Orlando LA. Cost-effectiveness analysis of the diagnosis of meniscus tears. Am J Sports Med. 2015;43:128-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Small NC. Complications in arthroscopic meniscal surgery. Clin Sports Med. 1990;9:609-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Garrett WE Jr, Swiontkowski MF, Weinstein JN, Callaghan J, Rosier RN, Berry DJ, Harrast J, Derosa GP. American Board of Orthopaedic Surgery Practice of the Orthopaedic Surgeon: Part-II, certification examination case mix. J Bone Joint Surg Am. 2006;88:660-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 159] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 6. | McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88:1549-1556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 379] [Article Influence: 21.1] [Reference Citation Analysis (1)] |
| 7. | McMurray TP. The semilunar cartilages. J Br Surg. 1942;29:407-414. [RCA] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 95] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30B:664-670. [PubMed] [DOI] [Full Text] |
| 9. | Petty CA, Lubowitz JH. Does arthroscopic partial meniscectomy result in knee osteoarthritis? Arthroscopy. 2011;27:419-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 146] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 10. | Goyal KS, Pan TJ, Tran D, Dumpe SC, Zhang X, Harner CD. Vertical Tears of the Lateral Meniscus: Effects on In Vitro Tibiofemoral Joint Mechanics. Orthop J Sports Med. 2014;2:2325967114541237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Bedi A, Kelly N, Baad M, Fox AJ, Ma Y, Warren RF, Maher SA. Dynamic contact mechanics of radial tears of the lateral meniscus: implications for treatment. Arthroscopy. 2012;28:372-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 107] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 12. | Sturnieks DL, Besier TF, Mills PM, Ackland TR, Maguire KF, Stachowiak GW, Podsiadlo P, Lloyd DG. Knee joint biomechanics following arthroscopic partial meniscectomy. J Orthop Res. 2008;26:1075-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Hall M, Wrigley TV, Metcalf BR, Hinman RS, Cicuttini FM, Dempsey AR, Mills PM, Lloyd DG, Bennell KL. Mechanisms underpinning the peak knee flexion moment increase over 2-years following arthroscopic partial meniscectomy. Clin Biomech (Bristol, Avon). 2015;30:1060-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Feeley BT, Lau BC. Biomechanics and Clinical Outcomes of Partial Meniscectomy. J Am Acad Orthop Surg. 2018;26:853-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 15. | Xu C, Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2015;23:164-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 149] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 16. | Beaufils P, Pujol N. Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res. 2017;103:S237-S244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 109] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 17. | Seil R, Becker R. Time for a paradigm change in meniscal repair: save the meniscus! Knee Surg Sports Traumatol Arthrosc. 2016;24:1421-1423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 18. | Parsons FG. The Joints of Mammals compared with those of Man: A Course of Lectures delivered at the Royal College of Surgeons of England: Part II. J Anat Physiol. 1900;34:301-323. [PubMed] |
| 19. | Tardieu C. The knee joint in three hominoid primates: application to Plio-Pleistocene hominids and evolutionary implications. In: Taub D, King F. Current perspectives in primate biology. New York: Van Nostrand Reinold, 1986: 182-190. |
| 20. | Tardieu C. Ontogeny and phylogeny of femoro-tibial characters in humans and hominid fossils: functional influence and genetic determinism. Am J Phys Anthropol. 1999;110:365-377. [PubMed] [DOI] [Full Text] |
| 21. | Tardieu C. Evolution of the knee intra-articular menisci in primates and some fossil hominids. In: Else JG, Lee PC. Primate Evolution. proceeding of the 10th congress of the international primatological society. Cambridge: Cambridge University Press, 1986; 1: 183–190. |
| 22. | Gardner E, O'Rahilly R. The early development of the knee joint in staged human embryos. J Anat. 1968;102:289-299. [PubMed] |
| 23. | Herwig J, Egner E, Buddecke E. Chemical changes of human knee joint menisci in various stages of degeneration. Ann Rheum Dis. 1984;43:635-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 179] [Reference Citation Analysis (0)] |
| 24. | Bullough PG, Munuera L, Murphy J, Weinstein AM. The strength of the menisci of the knee as it relates to their fine structure. J Bone Joint Surg Br. 1970;52:564-567. [PubMed] |
| 25. | Kohn D, Siebert W. Meniscus suture techniques: a comparative biomechanical cadaver study. Arthroscopy. 1989;5:324-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 89] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | Bellemans J, Vandenneucker H, Labey L, Van Audekercke R. Fixation strength of meniscal repair devices. Knee. 2002;9:11-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Post WR, Akers SR, Kish V. Load to failure of common meniscal repair techniques: effects of suture technique and suture material. Arthroscopy. 1997;13:731-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 114] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 28. | Berlet GC, Fowler PJ. The anterior horn of the medical meniscus. An anatomic study of its insertion. Am J Sports Med. 1998;26:540-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 74] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 29. | Jacobsen K. Area intercondylaris tibiae: Osseous surface structure and its relation to soft tissue structures and applications to radiography. J Anat. 1974;117:605-618. [PubMed] |
| 30. | Papalia R, Simonetta R, Di Vico G, Torre G, Saccone L, Espregueira-Mendes J, Denaro V. Tears of popliteomeniscal fascicles, diagnostic and clinical implications. A review of the evidence. J Biol Regul Homeost Agents. 2016;30:99-106. [PubMed] |
| 31. | Forkel P, Herbort M, Sprenker F, Metzlaff S, Raschke M, Petersen W. The biomechanical effect of a lateral meniscus posterior root tear with and without damage to the meniscofemoral ligament: efficacy of different repair techniques. Arthroscopy. 2014;30:833-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 32. | Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10:90-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 892] [Cited by in RCA: 719] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 33. | Crawford MD, Hellwinkel JE, Aman Z, Akamefula R, Singleton JT, Bahney C, LaPrade RF. Microvascular Anatomy and Intrinsic Gene Expression of Menisci From Young Adults. Am J Sports Med. 2020;48:3147-3153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 34. | Lin Y, Zhang K, Li Q, Li J, Xu B. Innervation of nociceptors in intact human menisci along the longitudinal axis: semi-quantitative histological evaluation and clinical implications. BMC Musculoskelet Disord. 2019;20:338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Śmigielski R, Becker R, Zdanowicz U, Ciszek B. Medial meniscus anatomy-from basic science to treatment. Knee Surg Sports Traumatol Arthrosc. 2015;23:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 36. | Bourne RB, Finlay JB, Papadopoulos P, Andreae P. The effect of medial meniscectomy on strain distribution in the proximal part of the tibia. J Bone Joint Surg Am. 1984;66:1431-1437. [PubMed] |
| 37. | Seedhom BB, Dowson D, Wright V. Proceedings: Functions of the menisci. A preliminary study. Ann Rheum Dis. 1974;33:111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 118] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 38. | Chatain F, Adeleine P, Chambat P, Neyret P; Société Française d'Arthroscopie. A comparative study of medial versus lateral arthroscopic partial meniscectomy on stable knees: 10-year minimum follow-up. Arthroscopy. 2003;19:842-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 183] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 39. | Arno S, Hadley S, Campbell KA, Bell CP, Hall M, Beltran LS, Recht MP, Sherman OH, Walker PS. The effect of arthroscopic partial medial meniscectomy on tibiofemoral stability. Am J Sports Med. 2013;41:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (1)] |
| 40. | Novaretti JV, Lian J, Patel NK, Chan CK, Cohen M, Musahl V, Debski RE. Partial Lateral Meniscectomy Affects Knee Stability Even in Anterior Cruciate Ligament-Intact Knees. J Bone Joint Surg Am. 2020;102:567-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 41. | Yao J, Lancianese SL, Hovinga KR, Lee J, Lerner AL. Magnetic resonance image analysis of meniscal translation and tibio-menisco-femoral contact in deep knee flexion. J Orthop Res. 2008;26:673-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 42. | Musumeci G, Loreto C, Carnazza ML, Cardile V, Leonardi R. Acute injury affects lubricin expression in knee menisci: an immunohistochemical study. Ann Anat. 2013;195:151-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 43. | Karahan M, Kocaoglu B, Cabukoglu C, Akgun U, Nuran R. Effect of partial medial meniscectomy on the proprioceptive function of the knee. Arch Orthop Trauma Surg. 2010;130:427-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 44. | Leonetti D, Tigani D. Pilon fractures: A new classification system based on CT-scan. Injury. 2017;48:2311-2317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 45. | Anderson AF, Irrgang JJ, Dunn W, Beaufils P, Cohen M, Cole BJ, Coolican M, Ferretti M, Glenn RE Jr, Johnson R, Neyret P, Ochi M, Panarella L, Siebold R, Spindler KP, Ait Si Selmi T, Verdonk P, Verdonk R, Yasuda K, Kowalchuk DA. Interobserver reliability of the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) classification of meniscal tears. Am J Sports Med. 2011;39:926-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 132] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 46. | Wadhwa V, Omar H, Coyner K, Khazzam M, Robertson W, Chhabra A. ISAKOS classification of meniscal tears-illustration on 2D and 3D isotropic spin echo MR imaging. Eur J Radiol. 2016;85:15-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 47. | Muriuki MG, Tuason DA, Tucker BG, Harner CD. Changes in tibiofemoral contact mechanics following radial split and vertical tears of the medial meniscus an in vitro investigation of the efficacy of arthroscopic repair. J Bone Joint Surg Am. 2011;93:1089-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 48. | Tachibana Y, Mae T, Shino K, Ohori T, Fujie H, Yoshikawa H, Nakata K. A longitudinal tear in the medial meniscal body decreased the in situ meniscus force under an axial load. Knee Surg Sports Traumatol Arthrosc. 2020;28:3457-3465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 49. | Katagiri H, Miyatake K, Nakagawa Y, Otabe K, Ohara T, Shioda M, Sekiya I, Koga H. The effect of a longitudinal tear of the medial meniscus on medial meniscal extrusion in anterior cruciate ligament injury patients. Knee. 2019;26:1292-1298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 50. | Mariani PP, Torre G, Battaglia MJ. The post-traumatic meniscal extrusion, sign of meniscotibial ligament injury. A case series. Orthop Traumatol Surg Res. 2022;108:103226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 51. | Pujol N, Beaufils P. Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2009;17:396-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 52. | Beaufils P, Hulet C, Dhénain M, Nizard R, Nourissat G, Pujol N. Clinical practice guidelines for the management of meniscal lesions and isolated lesions of the anterior cruciate ligament of the knee in adults. Orthop Traumatol Surg Res. 2009;95:437-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 53. | Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012;94:2222-2227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 305] [Cited by in RCA: 246] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 54. | Elmallah R, Jones LC, Malloch L, Barrett GR. A Meta-Analysis of Arthroscopic Meniscal Repair: Inside-Out versus Outside-In versus All-Inside Techniques. J Knee Surg. 2019;32:750-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 55. | Gerritsen LM, van der Lelij TJN, van Schie P, Fiocco M, van Arkel ERA, Zuurmond RG, Keereweer S, van Driel PBAA. Higher healing rate after meniscal repair with concomitant ACL reconstruction for tears located in vascular zone 1 compared to zone 2: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30:1976-1989. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 56. | Cinque ME, DePhillipo NN, Moatshe G, Chahla J, Kennedy MI, Dornan GJ, LaPrade RF. Clinical Outcomes of Inside-Out Meniscal Repair According to Anatomic Zone of the Meniscal Tear. Orthop J Sports Med. 2019;7:2325967119860806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 57. | Barber-Westin SD, Noyes FR. Clinical healing rates of meniscus repairs of tears in the central-third (red-white) zone. Arthroscopy. 2014;30:134-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 58. | Xiao WF, Yang YT, Xie WQ, He M, Liu D, Cai ZJ, Yu DJ, Li YS, Wei LC. Effects of Platelet-Rich Plasma and Bone Marrow Mesenchymal Stem Cells on Meniscal Repair in the White-White Zone of the Meniscus. Orthop Surg. 2021;13:2423-2432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 59. | Rothermel SD, Smuin D, Dhawan A. Are Outcomes After Meniscal Repair Age Dependent? Arthroscopy. 2018;34:979-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 60. | Everhart JS, Magnussen RA, Poland S, DiBartola AC, Blackwell R, Kim W, Kaeding CC, Flanigan DC. Meniscus repair five-year results are influenced by patient pre-injury activity level but not age group. Knee. 2020;27:157-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Grassi A, Pizza N, Andrea Lucidi G, Macchiarola L, Mosca M, Zaffagnini S. Anatomy, magnetic resonance and arthroscopy of the popliteal hiatus of the knee: normal aspect and pathological conditions. EFORT Open Rev. 2021;6:61-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 62. | Logan CA, Aman ZS, Kemler BR, Storaci HW, Dornan GJ, LaPrade RF. Influence of Medial Meniscus Bucket-Handle Repair in Setting of Anterior Cruciate Ligament Reconstruction on Tibiofemoral Contact Mechanics: A Biomechanical Study. Arthroscopy. 2019;35:2412-2420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 63. | Costa GG, Grassi A, Zocco G, Graceffa A, Lauria M, Fanzone G, Zaffagnini S, Russo A. What Is the Failure Rate After Arthroscopic Repair of Bucket-Handle Meniscal Tears? Am J Sports Med. 2022;50:1742-1752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 64. | Saliman JD. The circumferential compression stitch for meniscus repair. Arthrosc Tech. 2013;2:e257-e264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 65. | Foissey C, Thaunat M, Fayard JM. All-Inside Double-Sided Suture Repair for Longitudinal Meniscal Tears. Arthrosc Tech. 2021;10:e2043-e2048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 66. | Borque KA, Jones M, Cohen M, Johnson D, Williams A. Evidence-based rationale for treatment of meniscal lesions in athletes. Knee Surg Sports Traumatol Arthrosc. 2022;30:1511-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 67. | DePhillipo NN, Moatshe G, Brady A, Chahla J, Aman ZS, Dornan GJ, Nakama GY, Engebretsen L, LaPrade RF. Effect of Meniscocapsular and Meniscotibial Lesions in ACL-Deficient and ACL-Reconstructed Knees: A Biomechanical Study. Am J Sports Med. 2018;46:2422-2431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 146] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 68. | Tuphé P, Foissey C, Unal P, Vieira TD, Chambat P, Fayard JM, Thaunat M. Long-term Natural History of Unrepaired Stable Ramp Lesions: A Retrospective Analysis of 28 Patients With a Minimum Follow-up of 20 Years. Am J Sports Med. 2022;50:3273-3279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 69. | Liu X, Zhang H, Feng H, Hong L, Wang XS, Song GY. Is It Necessary to Repair Stable Ramp Lesions of the Medial Meniscus During Anterior Cruciate Ligament Reconstruction? Am J Sports Med. 2017;45:1004-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 100] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 70. | Sonnery-Cottet B, Serra Cruz R, Vieira TD, Goes RA, Saithna A. Ramp Lesions: An Unrecognized Posteromedial Instability? Clin Sports Med. 2020;39:69-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 71. | DePhillipo NN, Cinque ME, Kennedy NI, Chahla J, Geeslin AG, Moatshe G, Engebretsen L, LaPrade RF. Inside-Out Repair of Meniscal Ramp Lesions. Arthrosc Tech. 2017;6:e1315-e1320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 72. | Li WP, Chen Z, Song B, Yang R, Tan W. The FasT-Fix Repair Technique for Ramp Lesion of the Medial Meniscus. Knee Surg Relat Res. 2015;27:56-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 73. | Thaunat M, Fayard JM, Guimaraes TM, Jan N, Murphy CG, Sonnery-Cottet B. Classification and Surgical Repair of Ramp Lesions of the Medial Meniscus. Arthrosc Tech. 2016;5:e871-e875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 127] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 74. | Thaunat M, Foissey C, Ingale P, Haidar I, Bauwens PH, Penet A, Kacem S, Fayard JM. Survival and Risk Factor Analysis of Arthroscopic Ramp Lesion Repair During Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2022;50:637-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 75. | Qalib YO, Tang Y, Wang D, Xing B, Xu X, Lu H. Ramp lesion of the medial meniscus. EFORT Open Rev. 2021;6:372-379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 76. | Ohori T, Mae T, Shino K, Fujie H, Hirose T, Tachibana Y, Yoshikawa H, Nakata K. Different effects of the lateral meniscus complete radial tear on the load distribution and transmission functions depending on the tear site. Knee Surg Sports Traumatol Arthrosc. 2021;29:342-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 77. | Zheng T, Song GY, Feng H, Zhang H, Li Y, Li X, Zhang ZJ, Ni QK, Feng Z. Lateral Meniscus Posterior Root Lesion Influences Anterior Tibial Subluxation of the Lateral Compartment in Extension After Anterior Cruciate Ligament Injury. Am J Sports Med. 2020;48:838-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 78. | Krych AJ, Bernard CD, Kennedy NI, Tagliero AJ, Camp CL, Levy BA, Stuart MJ. Medial Versus Lateral Meniscus Root Tears: Is There a Difference in Injury Presentation, Treatment Decisions, and Surgical Repair Outcomes? Arthroscopy. 2020;36:1135-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 79. | Zheng T, Song G, Li Y, Zhang Z, Ni Q, Cao Y, Feng Z, Zhang H, Feng H. Clinical, Radiographic, and Arthroscopic Outcomes of Surgical Repair for Radial and Avulsed Lesions on the Lateral Meniscus Posterior Root During ACL Reconstruction: A Systematic Review. Orthop J Sports Med. 2021;9:2325967121989678. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 80. | Campbell A, Narvaez M, Caldwell JM, Banffy M. Stay Ipsilateral: An Analysis of Tibial Tunnel Distance Between Cruciate Ligament Reconstruction and Posterior Meniscal Root Repair. Arthrosc Sports Med Rehabil. 2021;3:e1031-e1035. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 81. | Familiari F, Palco M, Russo R, Moatshe G, Simonetta R. Arthroscopic Repair of Posterior Root Tears of the Lateral Meniscus with All-Suture Anchor. Arthrosc Tech. 2022;11:e781-e787. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 82. | Zhang K, Li L, Yang L, Shi J, Zhu L, Liang H, Wang X, Yang X, Jiang Q. Effect of degenerative and radial tears of the meniscus and resultant meniscectomy on the knee joint: a finite element analysis. J Orthop Translat. 2019;18:20-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 83. | Beaufils P, Becker R, Kopf S, Englund M, Verdonk R, Ollivier M, Seil R. Surgical management of degenerative meniscus lesions: the 2016 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2017;25:335-346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 182] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 84. | Hohmann E, Angelo R, Arciero R, Bach BR, Cole B, Cote M, Farr J, Feller J, Gelbart B, Gomoll A, Imhoff A, LaPrade R, Mandelbaum BR, Marx RG, Monllau JC, Noyes F, Parker D, Rodeo S, Sgaglione N, Shea K, Shelbourne DK, Yoshiya S, Glatt V, Tetsworth K. Degenerative Meniscus Lesions: An Expert Consensus Statement Using the Modified Delphi Technique. Arthroscopy. 2020;36:501-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 85. | Giuffrida A, Di Bari A, Falzone E, Iacono F, Kon E, Marcacci M, Gatti R, Di Matteo B. Conservative vs. surgical approach for degenerative meniscal injuries: a systematic review of clinical evidence. Eur Rev Med Pharmacol Sci. 2020;24:2874-2885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 86. | Hussain SM, Neilly DW, Baliga S, Patil S, Meek R. Knee osteoarthritis: a review of management options. Scott Med J. 2016;61:7-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 108] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 87. | Palco M, Fenga D, Basile GC, Rizzo P, Cavalieri B, Leonetti D, Alito A, Bruschetta A, Traina F. Platelet-Rich Plasma Combined with Hyaluronic Acid versus Leucocyte and Platelet-Rich Plasma in the Conservative Treatment of Knee Osteoarthritis. A Retrospective Study. Medicina (Kaunas). 2021;57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 88. | Beamer BS, Walley KC, Okajima S, Manoukian OS, Perez-Viloria M, DeAngelis JP, Ramappa AJ, Nazarian A. Changes in Contact Area in Meniscus Horizontal Cleavage Tears Subjected to Repair and Resection. Arthroscopy. 2017;33:617-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 89. | Kurzweil PR, Lynch NM, Coleman S, Kearney B. Repair of horizontal meniscus tears: a systematic review. Arthroscopy. 2014;30:1513-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 90. | Kamimura T, Kimura M. Repair of a Chronic Large Meniscal Defect With Implantation of Autogenous Meniscal Fragments Using a Tubular-Shaped Fibrin Clot. Arthrosc Tech. 2018;7:e257-e263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 91. | Ciemniewska-Gorzela K, Bąkowski P, Naczk J, Jakob R, Piontek T. Complex Meniscus Tears Treated with Collagen Matrix Wrapping and Bone Marrow Blood Injection: Clinical Effectiveness and Survivorship after a Minimum of 5 Years' Follow-Up. Cartilage. 2021;13:228S-238S. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 92. | Milliron EM, Magnussen RA, A Cavendish P, P Quinn J, DiBartola AC, Flanigan DC. Repair of Radial Meniscus Tears Results in Improved Patient-Reported Outcome Scores: A Systematic Review. Arthrosc Sports Med Rehabil. 2021;3:e967-e980. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 93. | Oosten J, Yoder R, DiBartola A, Bowler J, Sparks A, Duerr R, Magnussen R, Kaeding C, Flanigan D. Several Techniques Exist With Favorable Biomechanical Outcomes in Radial Meniscus Tear Repair-A Systematic Review. Arthroscopy. 2022;38:2557-2578.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 94. | Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922-1931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 628] [Cited by in RCA: 705] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 95. | Gajjar SM, Solanki KP, Shanmugasundaram S, Kambhampati SBS. Meniscal Extrusion: A Narrative Review. Orthop J Sports Med. 2021;9:23259671211043797. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 96. | Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, LaPrade RF. Meniscal Root Tears: Current Concepts Review. Arch Bone Jt Surg. 2018;6:250-259. [PubMed] |
| 97. | Jiang EX, Abouljoud MM, Everhart JS, DiBartola AC, Kaeding CC, Magnussen RA, Flanigan DC. Clinical factors associated with successful meniscal root repairs: A systematic review. Knee. 2019;26:285-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 98. | Chung KS, Ha JK, Ra HJ, Kim JG. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24:1455-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 135] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 99. | Mochizuki Y, Kawahara K, Samejima Y, Kaneko T, Ikegami H, Musha Y. Short-term results and surgical technique of arthroscopic centralization as an augmentation for medial meniscus extrusion caused by medial meniscus posterior root tear. Eur J Orthop Surg Traumatol. 2021;31:1235-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 100. | Kyun-Ho S, Hyun-Jae R, Ki-Mo J, Seung-Beom H. Effect of concurrent repair of medial meniscal posterior root tears during high tibial osteotomy for medial osteoarthritis during short-term follow-up: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2021;22:623. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |