Published online Dec 18, 2023. doi: 10.5312/wjo.v14.i12.889
Peer-review started: August 29, 2023
First decision: October 9, 2023
Revised: October 15, 2023
Accepted: November 9, 2023
Article in press: November 9, 2023
Published online: December 18, 2023
Processing time: 101 Days and 13.3 Hours
Metallosis is the result of metallic wear debris in the soft tissues and is associated to both local and systemic inflammatory response. Metallosis has been reported after total hip and total knee arthroplasty (TKA), but rarely after a unicompartimental knee arthroplasty (UKA). In the context of UKA metallosis, surgeons often opt for revision using a TKA. However, in this paper, the authors successfully treated UKA revising the metal back only.
Prior to treat our patient we conducted a literature research through which we identified eleven cases of metallosis after UKA, ten (90.9%) were treated revising using though a TKA. Only one case was managed through a uni-on-uni revision, reporting high knee function. Our patient complained worsening pain and function after a snap occurred at 16 mo after UKA implantation. At 18 mo following surgical debridment and uni-on-uni revision surgery, our patient exhibited a relevant improvement in Oxford Knee Score and a reduction of metal ion levels in the blood.
Our study highlights that in case of metallosis after UKA, the treatment may be based on surgical debridement and just revising the mobilized components.
Core Tip: Metallosis is a rare but serious complication of unicompartimental knee arthroplasty. It is generally treated through surgical debridment and revision to a total knee arthroplasty. However, in case of absence of critical signs of implant malpositioning, soft tissue impairment or bone loss, it could be successfully resolved through surgical debridment and uni-on-uni revision.
- Citation: Toro G, Braile A, Conza G, De Cicco A, Abu Mukh A, Placella G, Salini V. Unicompartimental knee arthroplasty metallosis treated with uni-on-uni revision: A case report. World J Orthop 2023; 14(12): 889-896
- URL: https://www.wjgnet.com/2218-5836/full/v14/i12/889.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i12.889
Metallosis is a condition in which prosthetic metallic wear produces debris that could be observed in soft tissues, causing both local and systemic inflammation, and could be associated to malignant tumors and systemic toxicity[1,2]. Metallosis had been associated mainly with total hip arthroplasty (THA)[3]. In fact, it could be observed in 2%-5% of metal-on-metal THA implants, yet it was also described in the context of total knee arthroplasty (TKA) and less frequently unicompartimental knee arthroplasty (UKA)[4]. Metallosis treatment contemplates wide surgical debridement and revision surgery. Nevertheless, the authors noticed that the revision seems to differ from the damage entity. The rare cases of metallosis after an UKA are generally treated through a revision with TKA[5-15]. In this article, we review the literature and introduce a case of 77 years old man presenting an UKA metallosis treated with debridement and UKA tibial metalback revision.
This article reports the case of a 77 years old patient with a metallosis after a UKA.
13-mo before, the patient perceived a “snap”, that was initially conservatively treated, considering the complete and painless range of motion documented during outpatient evaluation.
Sixteen months prior to the metallosis diagnosis, the patient underwent to a medial UKA for unicompartimental knee osteoarthritis.
The patient had no other relevant co-morbidities.
In the three months after the “snap,” the patient started to report a constant worsening of knee pain and a substantial reduction of joint function [oxford knee score (OKS) of 27/48].
Baseline blood ion levels were in line with a diagnosis of metallosis (Chrome 1.26 µg/L, Cobalt 3.94 µg/L).
The imaging performed at that time confirmed tibial implant loosening (Figure 1) and revision surgery was necessary after excluding infection[16-18].
Prior to treat the patient, the research team decided to evaluate all the possible procedures. Therefore, a literature research was conducted through PubMed by two independent reviewers (Braile A and Conza G) using the following terms in their various combinations “Unicompartmental knee arthroplasty,” “metallosis,” “liner dislocation”, “fixed-bearing”, “mobile-bearing”. Studies compatible with our criteria were included and controversies between the two reviewers were analyzed by a third author for the inclusion decision (Salini V).
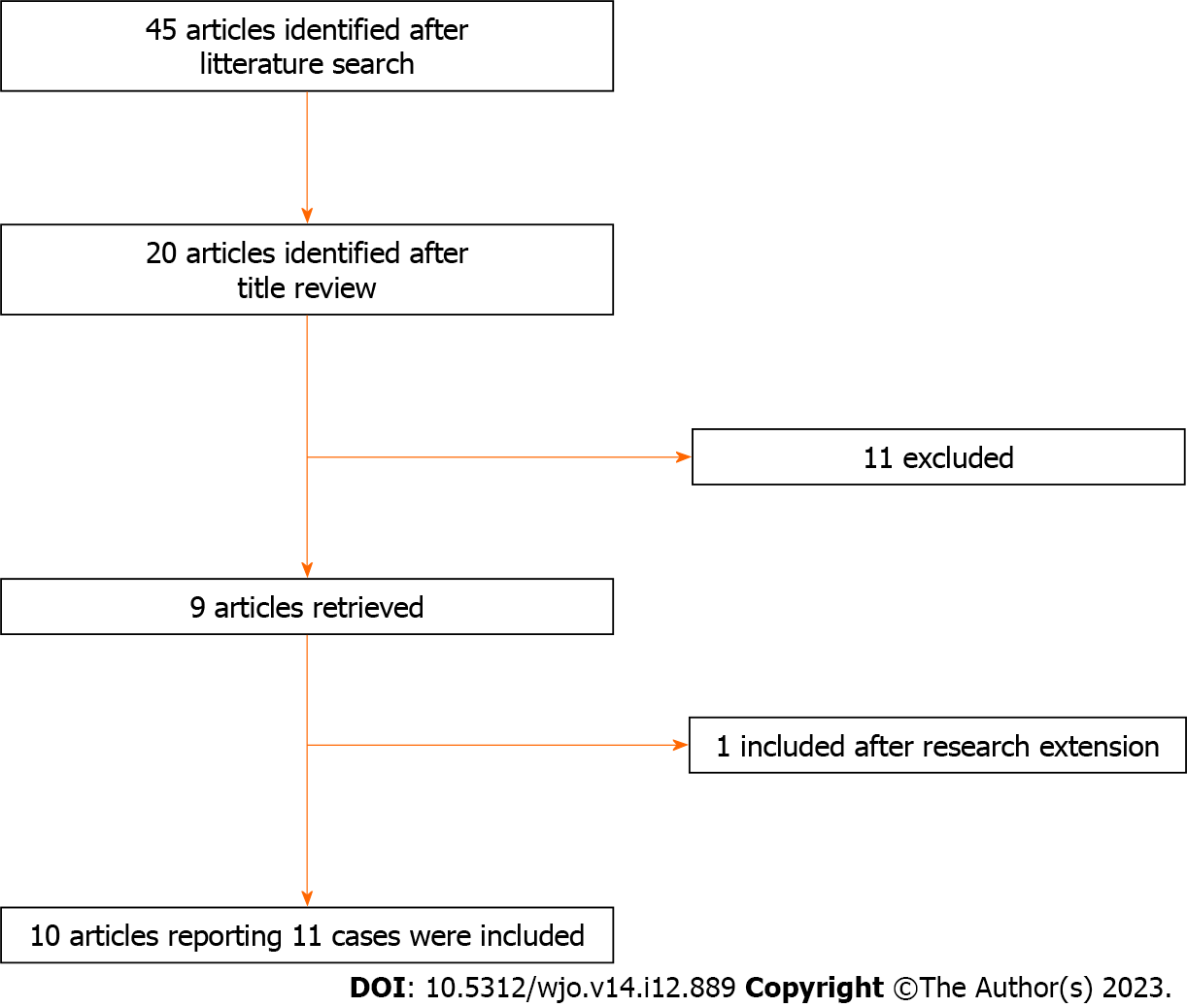
The literature search was conducted only in PubMed given that 90% of high-quality studies can be retrieved from this database, as reported by Rollin et al[19]. Therefore, to summarize the knowledge around a specific topic, PubMed research should be considered cost-effective as practitioners are able to easily retrieve most of the literature by using it[19,20]. All articles on metallosis after UKA in English, Spanish and Italian languages were included and analyzed in the present review. Articles with incomplete follow-up were excluded. The references cited in the included articles were also reviewed to identify further relevant studies. Data from each retrieved study were collected using a pre-arranged form. Out of 45 records identified, 20 presented criteria for further review. Eleven articles were then excluded after abstract review because did not meet the inclusion criteria. One further article was included after reviewing references cited in the included articles. Therefore, 10 articles, including 11 patients were retrieved and analyzed in the present study (Figure 2).
Patient age averaged 66.4 years (54-76 years), metallosis occurred at a mean time of 42.58 mo from the UKA. Out of 11 patients, 9 (81.8%) were treated through revision TKA. Two cases necessitated a second revision TKA at a mean of 39 mo. The functional outcome improved in all eleven cases (Table 1).
| Article info | Studied population | Outcomes | ||||||||||||||||||
| N. | Ref. | Year | Journal | Type | Population (n.) | Sex | Age (yr) | Implant type | Months elapsed between implantation and bearing dislocation | Metal ions (Cr/Cb) | Type of precedure | Function pre-op | Knee ROM pre-op | Metal ions (Cr/Cb) last follow-up | Function last follow-up | Knee ROM last follow-up | General complications | Infection | Fracture | Implant loosening (yes /months) |
| 1 | Sanchis-Alfonso et al[5] | 2007 | KSSTA | Case report | 1 | M | 54 | Fixed bearing | NA | Revision with TKA | NA | |||||||||
| 2 | Apostolopoulos et al[6] | 2014 | J Long Term Eff Med Implants | Case report | 1 | M | 67 | Mobile bearing | 54 | NA | NA | None | No | No | Yes /54 | |||||
| 3 | Vecchini et al[10] | 2019 | Acta Biomed | Case report | 1 | M | 71 | NA | NA | Revision with TKA | 10-110 | NA | 0-130 | None | No | No | ||||
| 4 | Greco et al[11] | 2018 | The knee | Case report | 1 | M | 72 | Fixed bearing | NA | Revision with TKA | NA | None | No | No | ||||||
| 5 | Rajgopal et al[13] | 2018 | Arthroplast today | Case report | 1 | M | 58 | NA | 24 | NA | Revision with TKA | KSS 48 OKS 19 UCLA 3 | 0-100 | NA | KSS 82 OKS 40 UCLA 7 | None | No | No | Yes /24 | |
| 6 | Vajapey et al[8] | 2021 | Arthroplasty | Case series | 2 | F | 76 | NA | 60 | NA | Revision with TKA | 30-120 | NA | None | No | No | ||||
| 7 | Kiran et al[14] | 2021 | JBJS Case connector | Case report | 1 | M | 61 | Fixed bearing | 60 | NA | Revision with TKA | NA | NA | OKS 39 | None | None | None | |||
| 8 | Foran et al[9] | 2013 | Clin Orthop Relat Res | Case series | 1 | NA | NA | NA | 56 | NA | Revision with TKA | NA | ||||||||
| 9 | Luyet et al[12] | 2015 | Acta Ortop. Belg. | Case report | 1 | F | 67 | NA | 1,5 | NA | Revision with UKA | ksk 59 KSF 60 | 0-90 | NA | Ksk 87 KSF 90 | 0-110 | No | No | ||
| 10 | Pescador et al[15] | 2016 | Reumatol Clin. | Case report | 1 | F | 72 | NA | NA | Revision with TKA | NA | |||||||||
| TOT. | 11 | 6 M /4 F | Mean: 66, 4 | 3 Fixed /1 Mobile | Mean: 42, 58 | 9 TKA /1 UKA | ||||||||||||||
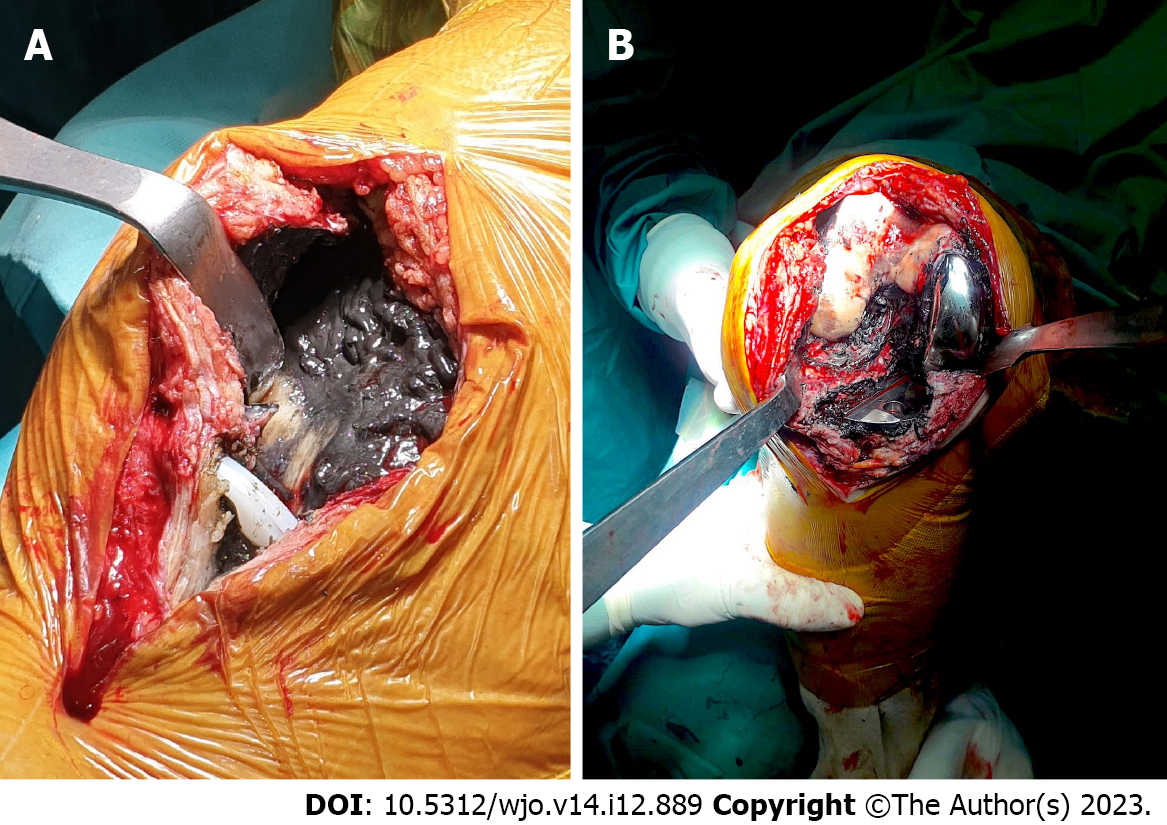
Intraoperatively, signs of soft tissue metallosis were evident (Figure 3). Following soft-tissue debridement and specimen collection, a component stability test confirmed isolated loosening of the tibial implant. Surgical specimen and baseline blood ion levels confirmed metallosis (Chrome 1.26 µg/L, Cobalt 3.94 µg/L).
The mobilized tibial component was revised using a larger Genus UNI Alderortho implant (Cormano, Italy).
We assessed the patient functional status through OKS and blood ion levels as previously recommended[21,22]. The patient presented a normal postoperative course. Complete range of motion, OKS score improvement (40/48), and good knee alignment were reported at 18 mo (Figure 4), while normalization of Ion blood levels (Chrome 0.95 µg/L, Cobalt 1.06 µg/L) were documented at 30 d after the uni-on-uni revision (Table 2).
| Pre-revision | Last follow-up | |
| OKS | 27 | 40 |
| Chrome (µg/L) | 126 | 106 |
| Cobalt (µg/L) | 334 | 95 |
Although UKA is an effective bone-preserving surgical option for unicompartmental symptomatic knee osteoarthritis in young and middle-aged patients[23], several complications may arise after its implantation. Due to the increasing number of arthroplasties performed yearly, optimizing the complication management is necessary.
In our case, we attributed metallosis and implant failure due to the progressive subclinical spinout of the polyethylene liner in an undersized tibial component which led to a posterior overload on the tibial implant. The surgeons performed UKA revision with a new UKA larger tibial implant against general recommendations because no tibial slope or coronal malalignment were present[24-27].
Very few cases of UKA revision with a new UKA implant were described in the available literature. Luyet et al[12] in a case of anterior dislocation of the polyethylene liner at 6 wk, presenting as a painful and swollen knee[13] furtherly complicated by metallosis decided to treat it through a uni-on-uni revision. Following the surgery, the patient presented good clinical and radiological outcomes in a 2 year follow-up[12]. Good clinical outcomes were reported after a Uni-on-uni revision also in an another a recent review about metallosis after knee replacement[4]. Epinette et al[27] in a retrospective study of 36 UKA-to-UKA revision surgery described this treatment as a reliable option, with lower morbidity and better functional outcomes compared with UKA-to-TKA revision. The authors suggested to reserve in patients with limited bone defects and no extension of the lesions[27].
Our review is limited by several factors including low patient number, the absence of a statistical analysis related to the nature of the review, and lack of literature on UKA metallosis. However, to the best of our knowledge, this is the first study reporting bloodstream ion changes while confirming clinical improvement following uni-on-uni revision in case of UKA metallosis. However, we believe that further analysis is necessary to confirm successful uni-on-uni revisions in case of metallosis.
In conclusion, we suggest that aseptic UKA metallosis without critical signs of malpositioning, soft tissue impairment or bone loss could be treated with surgical debridement and unicompartimental knee revision arthroplasty. This kind of approach could lead to a significant improvement of functional outcomes, and blood ion levels.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: OOMMEN AT, India S-Editor: Qu XL L-Editor: A P-Editor: Yuan YY
| 1. | Toro G, De Cicco A, Braile A, Landi G, Schiavone Panni A. New insights on metal allergy in total joint arthroplasty. J Biol Regul Homeost Agents. 2020;34:125-130. IORS Special Issue on Orthopedics. [PubMed] |
| 2. | Pesce V, Maccagnano G, Vicenti G, Notarnicola A, Lovreglio P, Soleo L, Pantalone A, Salini V, Moretti B. First case report of vanadium metallosis after ceramic-on-ceramic total hip arthroplasty. J Biol Regul Homeost Agents. 2013;27:1063-1068. [PubMed] |
| 3. | Goderecci R, Fidanza A, Necozione S, Francione V, Indelli PF, Calvisi V. Ultrasound-based decision making following metal-on-metal hip arthroplasty. J Clin Orthop Trauma. 2020;11:79-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Sahan I, Anagnostakos K. Metallosis after knee replacement: a review. Arch Orthop Trauma Surg. 2020;140:1791-1808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Sanchis-Alfonso V. Severe metallosis after unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2007;15:361-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Apostolopoulos AP, Katsougrakis I, Fanous R, Harrison A, Saavedra E. Severe metallosis following polyethylene dislocation in a mobile-bearing medial unicompartmental knee replacement. J Long Term Eff Med Implants. 2014;24:147-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Fujii T, Matsui Y, Noboru M, Inagaki Y, Kadoya Y, Tanaka Y. Meniscal Bearing Dislocation of Unicompartmental Knee Arthroplasty with Faint Symptom. Case Rep Orthop. 2015;2015:217842. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Vajapey SP, Alvarez PM, Chonko D. Bearing failure in a mobile bearing unicompartmental knee arthroplasty: an uncommon presentation of an implant-specific complication. Arthroplasty. 2021;3:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Foran JR, Brown NM, Della Valle CJ, Berger RA, Galante JO. Long-term survivorship and failure modes of unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2013;471:102-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 108] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 10. | Vecchini E, Ditta A, Gelmini M, Maluta T, Valentini R, Ricci M, Magnan B. Rupture of the femoral component and severe metallosis of the knee 10 years after unicompartmental knee arthroplasty (UKA): a case report. Acta Biomed. 2019;90:198-202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Greco N, Berend K. Polyethylene liner dislocation of fixed-bearing medial oxinium unicompartmental arthroplasty with severe metallosis. Knee. 2018;25:341-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Luyet A, Fischer JF, Jolles BM, Lunebourg A. Unexpected wear of an unicompartimental knee arthroplasty in oxidized zirconium. Acta Orthop Belg. 2015;81:790-795. [PubMed] |
| 13. | Rajgopal A, Panda I, Tyagi VC. Early failure with massive metallosis and posteromedial wear following atraumatic anterior cruciate ligament rupture after medial unicompartmental knee arthroplasty. Arthroplast Today. 2018;4:15-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Kiran M, Kho J, Hepburn E, Chakraverty J, Davies H. Chronic Wear-Induced Bearing Dislocation in a Fixed-Bearing Unicompartmental Knee Arthroplasty: A Case Report. JBJS Case Connect. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Pescador D, Calero-Paniagua I, Sánchez-González MD, Montilla C. Metallosis as a cause of pain and inflammation in a patient with a knee replacement: A case description. Reumatol Clin. 2016;12:112-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Toro G, Braile A, Zappulo E, Panni AS, Indelli PF. Does D-Dimer really help in the diagnosis of chronic periprosthetic joint infections (PJI)? A case-control study. Journal of Arthroscopy and Joint Surgery. 2020;7:189-193. [DOI] [Full Text] |
| 17. | Panni AS, Ascione F, Rossini M, Braile A, Corona K, Vasso M, Hirschmann MT. Tibial internal rotation negatively affects clinical outcomes in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26:1636-1644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 18. | Vasso M, Braile A, Ascione F, Toro G, De Cicco A, Lepore F, Schiavone Panni A. Two-stage reimplantation in periprosthetic knee infection. Eur Rev Med Pharmacol Sci. 2019;23:51-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 19. | Rollin L, Darmoni S, Caillard JF, Gehanno JF. Searching for high-quality articles about intervention studies in occupational health--what is really missed when using only the Medline database? Scand J Work Environ Health. 2010;36:484-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Pillastrini P, Vanti C, Curti S, Mattioli S, Ferrari S, Violante FS, Guccione A. Using PubMed search strings for efficient retrieval of manual therapy research literature. J Manipulative Physiol Ther. 2015;38:159-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Swiatkowska I, Martin N, Hart AJ. Blood titanium level as a biomarker of orthopaedic implant wear. J Trace Elem Med Biol. 2019;53:120-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 22. | Cobalt Blood Level. Science Direct Topics. Available from: https://www.sciencedirect.com/topics/nursing-and-health-professions/cobalt-blood-level. |
| 23. | Johal S, Nakano N, Baxter M, Hujazi I, Pandit H, Khanduja V. Unicompartmental Knee Arthroplasty: The Past, Current Controversies, and Future Perspectives. J Knee Surg. 2018;31:992-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 24. | Hernigou P, Deschamps G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am. 2004;86:506-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 227] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 25. | Crawford DA, Berend KR, Lombardi AV. Management of the Failed Medial Unicompartmental Knee Arthroplasty. J Am Acad Orthop Surg. 2018;26:e426-e433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 26. | Lombardi AV Jr, Kolich MT, Berend KR, Morris MJ, Crawford DA, Adams JB. Revision of Unicompartmental Knee Arthroplasty to Total Knee Arthroplasty: Is It as Good as a Primary Result? J Arthroplasty. 2018;33:S105-S108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 27. | Epinette JA, Leyder M, Saragaglia D, Pasquier G, Deschamps G; Société Française de la Hanche et du Genou. Is unicompartmental-to-unicompartmental revision knee arthroplasty a reliable option? Case-control study. Orthop Traumatol Surg Res. 2014;100:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |