Published online Dec 18, 2023. doi: 10.5312/wjo.v14.i12.868
Peer-review started: July 12, 2023
First decision: August 31, 2023
Revised: September 18, 2023
Accepted: October 16, 2023
Article in press: October 16, 2023
Published online: December 18, 2023
Processing time: 155 Days and 10.1 Hours
Ankle fractures are common lesions of the lower limbs. Approximately 40% of ankle fractures affect the posterior malleolus (PM). Historically, PM osteosynthesis was recommended when PM size in X-ray images was greater than 25% of the joint. Currently, computed tomography (CT) has been gaining traction in the preoperative evaluation of ankle fractures.
To elucidate the similarity in dimensions and to correlate PM size in X-ray images with the articular surface of the affected tibial plafond in the axial view on CT (AXCT) of a PM fracture.
Eighty-one patients (mean age: 39.4 ± 13.5 years) were evaluated (54.3% were male). Two independent examiners measured PM size in profile X-ray images (PMXR) and sagittal CT (SAGCT) slices. The correlation of the measurements between the examiners and the difference in the PM fragment sizes between the two images were compared. Next, the PM size in PMXR was compared with the surface of the tibial plafond involved in the fracture in AXCT according to the Haraguchi classification.
The correlation rates between the examiners were 0.93 and 0.94 for PMXR and SAGCT, respectively (P < 0.001). Fragments were 2.12% larger in SAGCT than in PMXR (P = 0.018). In PMXR, there were 56 cases < 25% and 25 cases ≥ 25%. When PMXR was < 25%, AXCT corresponded to 10.13% of the tibial plafond. When PMXR was ≥ 25%, AXCT was 24.52% (P < 0.001). According to the Haraguchi classification, fracture types I and II had similar PMXR measurements that were greater than those of type III. When analyzing AXCT, a significant difference was found between the three types, with II > I > III (P < 0.001).
PM fractures show different sizes using X-ray or CT images. CT showed a larger PM in the sagittal plane and allowed the visualization of the real dimensions of the tibial plafond surface.
Core Tip: The study showed fractures of the posterior malleolus (PM) were different sizes on X-ray and computed tomography (CT) images. It is possible to see that some PM patterns considered small on radiographs affected a significant joint area when CT scans were performed. CT scans also showed that the actual size of the PM fragment was larger than that seen on radiographs.
- Citation: De Marchi Neto N, Nesello PFT, Bergamasco JM, Costa MT, Christian RW, Severino NR. Importance of computed tomography in posterior malleolar fractures: Added information to preoperative X-ray studies. World J Orthop 2023; 14(12): 868-877
- URL: https://www.wjgnet.com/2218-5836/full/v14/i12/868.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i12.868
Ankle malleolar fractures are the most common fractures among those involving load-bearing joints[1]. Approximately 40% of ankle fractures are trimalleolar fractures[2], which affect the posterior edge of the tibia in addition to the lateral and medial malleoli, more specifically the portion known as Volkmann’s triangle or posterior malleolus (PM)[3]. Fractures involving the PM cause more incongruity, joint instability, and worse results than unimalleolar or bimalleolar fractures of the ankle[4-7].
Since the article by Nelson and Jensen[7] in 1940, the internal fixation of the PM has been recommended in ankle fractures, considering a size of one-third of the fragment relative to the articular surface of the tibia in lateral X-ray images. Other authors have stipulated a value of 25% of the articular surface as the determinant for the fixation of the posterior fragment to thereby restore ankle congruity[8-10]. PM fixation is currently controversial[11-14], and variable clinical results have been obtained in the treatment of trimalleolar fractures[15]. The classic recommendation to fix PM fractures with a radiological size ≥ 25% theoretically improves articular congruence and reduces the risk of post-traumatic arthritis[16,17]. On the other hand, some authors report fixing PM fractures of various sizes, including small fragments (< 25%), under the justification of providing more stability to the ankle joint and better functional results[18,19].
When diagnosing a PM in lateral ankle X-ray images, its visualization is frequently impaired by overlapping bone images, plaster immobilizations, or external fixators[20]. Moreover, measuring the size of a posterior fracture can be difficult, resulting in the underestimation of the size of the PM, which leads to an inaccurate interpretation, which in turn interferes with the treatment[20-22]. Thus, computed tomography (CT) is increasingly recommended in the treatment of ankle fractures, especially when the PM is affected[14,23]. CT allows a better interpretation of all joint fragments, particularly regarding PM morphology and size, and it also aids in preoperative planning[24,25]. Different PM fracture patterns are observed in CT studies, depending on the size of the bone fragment, its anatomical location, bone impaction, and the fragment’s relationship with other malleoli and the syndesmosis[15,23]. Specific PM classifications have been created, with associated recommendations for the best treatment for each type of fracture[2,26-28].
However, there is no clear relationship between the size of the PM in X-ray images and its actual size in CT slices or between the articular surface of the affected tibia and the fracture. Thus, the aim of the present study was to analyze PM size in X-ray and CT studies and to relate the size of the fragment obtained from X-ray images to the articular area of the tibial plafond.
Over a 5-year period from 2016 to 2021, 370 patients diagnosed with an ankle fracture were treated at our hospital (a level 1 trauma center). Of these fractures, 144 involved the PM. The study included patients aged 18 years or older with an ankle fracture or fracture-dislocation involving the PM [AO Foundation/Orthopedic Trauma Association (AO/OTA) classification 44-A3, 44-B3, and 44-C1/2]. Cases of tibial plafond fractures, cases of ankle fractures associated with other hindfoot fractures, and cases with incomplete data in the medical records, such as absence of appropriate X-ray and CT images, were excluded. A total of 81 patients met the study’s inclusion criteria. The study was approved by our Institutional Ethics Committee. The fractures were categorized according to the AO/OTA classification, and the Haraguchi CT classification was used specifically for the PM[26].
The Enterprise Imaging XERO Viewer software (Agfa HealthCare, Mortsel, Belgium) version 8.1.2 was used to select and analyze X-ray images, and the RadiAnt DICOM Viewer software (Medixant, Poznań, Poland) version 2.3 was used to analyze CT images. The PM fragments were measured on lateral X-ray images (PMXR) by two independent examiners (herein named X and Y), based on the relationship between fracture size and total articular surface (Figure 1). In sagittal CT (SAGCT) slices, the image with the largest PM was selected, and the latter was measured by the two examiners (X and Y). Similarly, to PMXR, PM size in SAGCT was measured using the proportion between the size of the fracture fragment and the total length of the joint (Figure 2). A second CT image was used in the axial plane to determine the size of the affected articular area in the tibial plafond. A point 5 mm above the highest point of the tibial articular surface was marked on the sagittal plane, and the corresponding axial (AXCT) slice was selected. The total tibial and PM areas were measured using the RadiAnt DICOM Viewer 2.3 software, and the fragment size relative to the total tibial plafond area on the AXCT was calculated (Figure 3).
Fractures were categorized into two groups based on the PMXR measurement: (1) PM < 25% of the joint; and (2) PM ≥ 25% of the joint. This cutoff value was used due to the consensus in the literature. Based on these groups, PM size was compared between PMXR and SAGCT, and the mean value of the examiners’ measurements was considered. A second evaluation was performed to determine the difference in PM size based on a classification of the fractures into smaller PMXR intervals, namely < 15%, 15%–19.9%, 20%–24.9%, 25%–29.9%, and ≥ 30% of the articular surface. For AXCT, the size of the affected articular surface was measured in both groups (A and B), and the size of the PM and the involvement of the articular surface were compared in the respective morphological categories using the classification proposed by Haraguchi et al[26].
The statistical analysis was performed using the SPSS Statistics software for Mac (IBM Corporation, Armonk, NY, United States), version 23, considering the mean of the values obtained by the examiners in PMXR and SAGCT. Data normality was tested for the quantitative variables using the Kolmogorov–Smirnov test. Interobserver reliability was assessed using the Kappa method for the qualitative variables and Pearson’s correlation for the quantitative variables. For direct comparison between X-ray and CT, the paired-sample t-test or the Wilcoxon, Mann–Whitney, and Kruskal–Wallis tests were used, depending on data normality, type of variable, and number of groups. The significance level was P < 0.05, with a 95% confidence interval.
A total of 81 patients participated in the study, of whom 44 were male (54.3%) and 37 were female (45.6%), with a mean age of 39.4 years (± 13.5). One ankle fracture (1.2%) was type A in the AO/OTA classification, 51 (62.9%) were type B, and 29 (35.8%) were type C. It was observed that the PM presented more than one fracture line in 22 cases (27.2%), which is described in the literature as a chondral or intercalary fragment at the center of the fracture, between the metaphysis and the posterior tibial cortex[29,30] (Table 1).
| Characteristic | Subcategory | n (%) |
| Agea | 39.48 (± 13.59) | |
| Sex | Male | 44 (54.32) |
| Female | 37 (45.67) | |
| Diagnosis | Fracture | 42 (51.85) |
| Fracture + dislocation | 39 (48.14) | |
| AO/OTA 44 | A | 1 (1.23) |
| B | 51 (62.96) | |
| C | 29 (35.80) | |
| Haraguchi | 1 | 29 (35.80) |
| 2 | 33 (40.74) | |
| 3 | 19 (23.45) | |
| Intermediate fragment | Yes | 22 (27.16) |
| No | 59 (72.83) |
The PMXR sizes measured by examiners X and Y were 21.15% and 20.46%, respectively, with a mean of 20.81% and Pearson’s correlation index of 0.93 (P < 0.001). With regard to SAGCT, the values obtained were 23.45% and 22.39%, with a mean of 22.92% and Pearson’s index of 0.94 (P < 0.001). This interobserver correlation was excellent both for PMXR and SAGCT (Table 2). Thus, regardless of the measured image, a good interobserver evaluation was obtained with the proposed measurement method. A significant difference was found in mean size between the images, with PM size in SAGCT being 2.12% (95% confidence interval: 0.3–3.8) greater than in X-ray images (P = 0.018).
| Examiner X | Examiner Y | Pearson’s | P value | |
| X-ray measurement | ||||
| Absolute size of the tibia | 5.28 (± 0.83) | 5.09 (± 0.82) | 0.88 | < 0.001 |
| Absolute size of the PM | 1.43 (± 0.75) | 1.32 (± 0.69) | 0.92 | < 0.001 |
| MP size (PMXR)a | 21.15 (± 10.20) | 20.46 (± 9.66) | 0.93 | < 0.001 |
| Mean PM sizea | 20.81 (± 9.70) | - | - | |
| CT measurement | ||||
| Absolute size of the tibia | 3.23 (± 0.65) | 3.13 (± 0.62) | 0.95 | < 0.001 |
| Absolute size of the PM | 0.97 (± 0.38) | 0.88 (± 0.37) | 0.89 | < 0.001 |
| PM size (SAGCT) | 23.45 (± 9.51) | 22.39 (± 9.96) | 0.94 | < 0.001 |
| Mean PM size | 22.92 (± 9.60) | |||
| Interobserver agreement | ||||
| PM < 25% in X-ray images | 56 | 58 | 0.88 | < 0.001 |
| PM ≥ 25% in X-ray imagesb | 25 | 23 | ||
| PM < 25% in CTb | 51 | 56 | 0.76 | < 0.001 |
| PM ≥ 25% in CTb | 30 | 25 | ||
When the sample was divided into two groups according to PMXR size, groups A (< 25%) and B (≥ 25%) had 56 and 25 patients, or 69.13% and 30.86% of the sample, respectively. When analyzing the AXCT of all fractures, the PM affected a mean 14.57% of the tibial plafond, but there was a difference between the groups, with 10.13% and 24.52% of the tibial plafond affected in group A (< 25%) and in group B (≥ 25%), respectively, (P < 0.001) (Table 3). The subdivision into the < 15.0%, 15.0%–19.9%, 20.0%–24.9%, 25.0%–29.9%, and ≥ 30.0% intervals and their respective AXCTs (Table 3) was performed to evaluate the gradual increase in the affected articular surface according to PMXR size. There were differences among all the evaluated subgroups, namely a gradual surface increase with the increase in PMXR; only the 20.0%–24.9% interval showed no statistical significance relative to the previous subgroup.
| Grouping according to PMXR < 25% and ≥ 25% (cases) | All cases | Group A, < 25% | Group B, ≥ 25% | P value | |
| 14.57% (81) (± 9.84) | 10.13% (56) (± 6.71) | 24.52% (25) (± 8.40) | < 0.001 | ||
| Subdivision of PMXR, % | < 14.9 | 15.0-19.9 | 20.0-24.9 | 25.0-29.9 | ≥ 30.0 |
| Affected articular surface % (cases) | 7.65 (26) (± 6.92) | 11.03a (18) (± 5.57) | 14.31 (11) (± 6.34) | 20.79a (14) (± 4.19) | 27.87a (12) (± 10.78) |
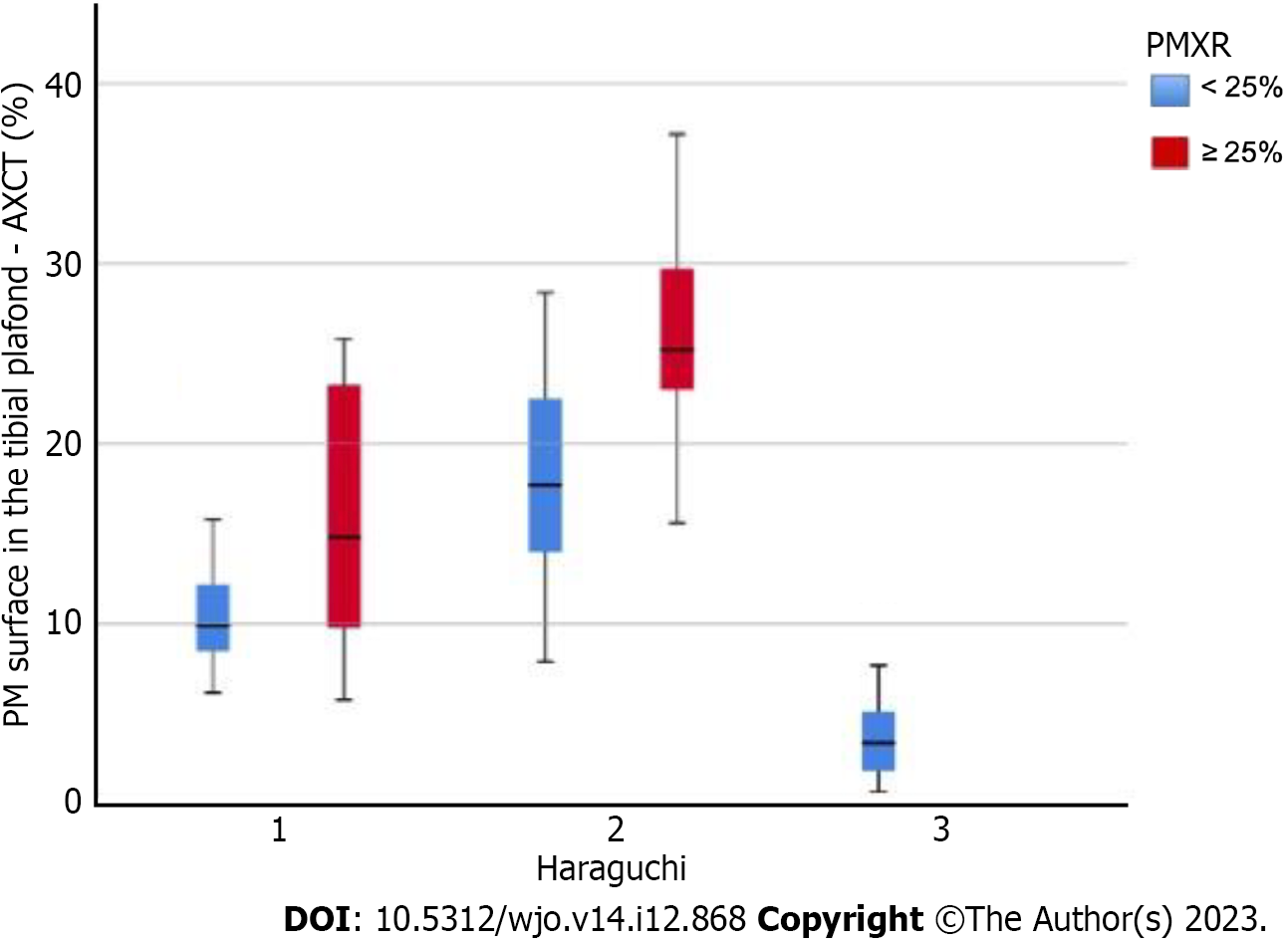
According to the Haraguchi classification, 29 fractures (35.8%) were type I, 33 (40.7%) were type II, and 19 (23.4%) were type III. In group A there were 21, 16, and 19 type I, type II, and type III fractures, respectively, whereas in group B there were 8 and 17 type I and type II fractures, respectively. The analysis of PM size in the X-ray images showed that type I and type II fractures had similar PMXR size (21.6% and 24.8%) and that both were larger than type III (small shell-shaped) fractures (P < 0.001).
In the overall evaluation of the articular surface, differences were found in AXCT among all Haraguchi CT categories, with PM fragments with mean values of 12.24%, 22.80%, and 3.84% of the tibial plafond surface, respectively, resulting in II > I > III (P < 0.001) (Table 4 and Figure 4). Differences in the articular surface of the tibial plafond (AXCT) for the Haraguchi subtypes were found in both groups, with P < 0.001 in group A and P = 0.002 in group B (Table 5 and Figure 5).
Historically, X-ray has been the most widely used imaging technique in the diagnosis of malleolar fractures and consequently of PM fractures. The indication for PM fixation is mostly associated with its size relative to the joint, although no consensus has emerged to date on the smallest articular fragment size that requires surgery[8,30,31].
The fact that there are different forms of measuring PM size should be considered. In addition, factors, such as image quality, immobilizations, and fixations, can interfere with PM measurement[20]. Several X-ray parameters have been studied to interpret ankle fractures, and PM size has good interexaminer reproducibility[21]. There is controversy regarding the best way of measuring PM size in lateral X-ray images; moreover, interobserver agreement shows variable results[22]. Currently, many authors consider CT essential for an adequate understanding of PM fractures due to the limitations of X-ray images and because CT aids in surgical planning by providing information on PM size and morphology and on its relationship with other malleoli and with the syndesmosis[20-22,32,33].
In the present study, considering only the X-ray images, the interobserver correlation for PM size was 0.93 (P < 0.001), which is excellent and higher than that obtained by Meijer et al[22] in an analysis with a larger number of examiners. This result suggests that good quality preoperative X-rays are fundamental for the adequate interpretation of the PM findings. A correlation of 0.94 (P < 0.001) was also achieved in the measurement performed in sagittal CT, which showed that an accurate measurement of the PM can be achieved using a simple method, regardless of the complementary exam that is used.
Most patients (56; 69.1%) had PM < 25% in PMXR. Therefore, if only the PM size was considered, the choice would be not to fix that fragment[13,16,34]. Stringfellow et al[35] compared X-ray and CT images and found that CT slices showed a larger PM than X-ray images in 92% of the cases. This result is similar to that obtained in the present study, in which the mean PM was found to be 2.12% larger (P = 0.018) in CT images. Thus, considering only the 25% cutoff value in PMXR as an indication for PM fixation, patients with fractures considered to be borderline, with PMXR values close to 25%, would probably fail to have the posterior fragment treated adequately if the diagnosis were based solely on X-ray images. For this reason, in recent decades, several authors started recommending the fixation of fragments < 25% because they feared that X-ray images could underestimate PM size when compared to CT[10,21].
Another concern is that X-ray images may not be adequate for the visualization of small osteochondral fragments and articular surface impaction[23,29,30,36]. The present case series supports this concern, as an osteochondral or intermediate fragment was found in 27.1% of CT images. Similarly, Büchler et al[21] reported that 23% of osteochondral fractures were not identified in X-ray images but were present in sagittal CT slices, thus suggesting that X-ray images have low sensitivity for diagnosing intermediate PM fragments, which could be a further hindrance for articular reduction[21,23,30].
By correlating X-ray images with axial CT slices, it is possible to determine the size of the articular surface affected by the PM fragment. In an initial evaluation considering groups < 25% and ≥ 25%, a significant difference in the percentage of affected articular surface was found: 10.13% vs 24.52% (P < 0.001). Previous studies have proposed random predetermined PM size intervals to evaluate the clinical results, articular congruity, and post-traumatic arthritis[35]. Similarly, by determining smaller PM intervals for X-ray images (< 15.0%, 15.0%-19.9%, 20.0%-24.9%, 25.0%-29.9%, and ≥ 30.0%), it was possible to evaluate the gradual increase in the percentage of affected articular surface in each interval relative to the previous interval. It should be noted that fragments in intervals 15.0%-19.9% and 20.0%-24.9% may have a similar articular surface. These results indicate that fragments considered small in X-ray images represent a relatively larger articular surface.
When the fractures were grouped according to their CT classification, type I and type II fractures had a similar size in X-ray images and could only be differentiated from type III (small shell) fractures; however, axial CT showed the difference between the articular surfaces of each CT type, as shown by the descriptive study of Haraguchi et al[26]. All the different CT types of fractures also showed differences in the size of the axial surface between groups A and B. We emphasize that the articular surfaces of the tibial plafond in type II fractures in group A and type I fractures in group B were of similar size (Figure 5). This means that although type II fragments in group A were deemed small in X-ray images (< 25%), the articular involvement was similar to that of a large fragment, such as one from group B. This information can only be obtained from the CT evaluation. Thus, the exclusive use of X-ray images for preoperative planning is associated with the risk of PMs with a larger area than expected being treated inadequately, which can interfere with the patient’s postoperative results.
The present study achieved a relevant sample, considering other studies on the same subject[26-28], and the study variables showed excellent correlation and interobserver agreement according to Landis and Koch[37], who demonstrated the applicability of the measuring method. However, the present study also had some limitations. The distribution of PM fractures among the three CT categories was satisfactory. However, there was a significant sample loss, and the distribution was based solely on 2D CT images, when some studies also used 3D images to evaluate PM[22,33]. Finally, the present findings add new information to the topic of articular involvement in PM fractures, which will hopefully aid the analysis of the clinical results of patients with PM fractures in future studies.
The size of PM fractures varies when evaluated by X-ray and CT. CT studies show a larger PM in the sagittal plane compared to PMXR images, and they also allow the identification of the presence of intermediate or chondral fracture fragments. Preoperative CT makes it possible to determine the real size of the articular surface of the tibial plafond, which can be underestimated if only X-ray is used.
For many decades when a posterior malleolus (PM) fracture was diagnosed, the size of the fragment on radiographs was always taken into consideration at the time of treatment. Therefore, fixation of the PM was recommended when greater than 25% of the tibial joint surface was involved.
This study aimed to see the real size of the PM fragment in ankle fractures and determine whether an X-ray image would be sufficient to show the real size of the fracture. It is also unknown if there is any correlation between PM size on X-rays and computed tomography (CT) scans.
To compare the PM size of the X-rays with the sagittal CT scans to see if they are similar and to evaluate the PM size compared with the axial CT scan and the articular surface of the tibial plafond involved in the ankle fracture.
Two foot and ankle specialists compared measurements of PM size on radiographs with CT scans. The PM size on the sagittal images and the joint surface area of the tibial plafond on the axial images were compared.
We found that PM fragments were 2.12% larger in sagittal CT than in X-rays. When analyzing axial CT scans, a significant difference was found between the three types of Haraguchi fractures.
PM fractures showed different sizes using X-ray or CT images. CT showed a larger PM in the sagittal plane and allowed the visualization of the real dimensions of the tibial plafond surface.
This study showed that CT is better to understand the size of the PM. Even small PM fractures on X-rays can affect a large portion of the articular surface. It would be recommended not to underestimate small PM fractures and always perform preoperative CT evaluation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ankrah AO, Netherlands; Khalifa AA, Egypt S-Editor: Liu JH L-Editor: Filipodia P-Editor: Zhang XD
| 1. | Palmanovich E, Brin YS, Laver L, Kish B, Nyska M, Hetsroni I. The effect of minimally displaced posterior malleolar fractures on decision making in minimally displaced lateral malleolus fractures. Int Orthop. 2014;38:1051-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Klammer G, Kadakia AR, Joos DA, Seybold JD, Espinosa N. Posterior pilon fractures: a retrospective case series and proposed classification system. Foot Ankle Int. 2013;34:189-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Volkmann R. Report on the disease cases treated at the halle surgical clinic in the year of 1873. Beitr Chir. 1875;104-109. In German. |
| 4. | Jaskulka RA, Ittner G, Schedl R. Fractures of the posterior tibial margin: their role in the prognosis of malleolar fractures. J Trauma. 1989;29:1565-1570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 205] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Irwin TA, Lien J, Kadakia AR. Posterior malleolus fracture. J Am Acad Orthop Surg. 2013;21:32-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 6. | Danford NC, Hellwinkel JE, Nocek MJ, Boddapati V, Greisberg JK, Trofa DP. Fractures of the posterior malleolus: a systematic review and analysis of patient-reported outcome scale selection. Eur J Orthop Surg Traumatol. 2023;33:1125-1131. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Nelson M, Jensen N. The treatment of trimalleolar fractures of the ankle. Surg Gynecol Obstet. 1940;71:509-514. |
| 8. | Heim D, Niederhauser K, Simbrey N. The Volkmann dogma: a retrospective, long-term, single-center study. Eur J Trauma Emerg Surg. 2010;36:515-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Evers J, Barz L, Wähnert D, Grüneweller N, Raschke MJ, Ochman S. Size matters: The influence of the posterior fragment on patient outcomes in trimalleolar ankle fractures. Injury. 2015;46 Suppl 4:S109-S113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 10. | Langenhuijsen JF, Heetveld MJ, Ultee JM, Steller EP, Butzelaar RM. Results of ankle fractures with involvement of the posterior tibial margin. J Trauma. 2002;53:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 131] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 11. | Bartoníček J, Rammelt S, Tuček M. Posterior Malleolar Fractures: Changing Concepts and Recent Developments. Foot Ankle Clin. 2017;22:125-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 112] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 12. | Carr D, Vannabouathong C, Petrisor BA, Parekh SG, Bhandari M. Posterior-Based Approaches to Open Reduction Internal Fixation of Bimalleolar and Trimalleolar Fractures: A Systematic Review and Meta-analysis. J Foot Ankle Surg. 2020;59:373-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | De Vries JS, Wijgman AJ, Sierevelt IN, Schaap GR. Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg. 2005;44:211-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 167] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 14. | Bergman C, Morin M, Lawson K. Anatomy, Classification, and Management of Ankle Fractures Involving the Posterior Malleolar Fragment: A Literature Review. Foot Ankle Orthop. 2019;4:2473011419887724. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Neumann AP, Rammelt S. Ankle fractures involving the posterior malleolus: patient characteristics and 7-year results in 100 cases. Arch Orthop Trauma Surg. 2022;142:1823-1834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 16. | McDaniel WJ, Wilson FC. Trimalleolar fractures of the ankle. An end result study. Clin Orthop Relat Res. 1977;37-45. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Verhage SM, Krijnen P, Schipper IB, Hoogendoorn JM. Persistent postoperative step-off of the posterior malleolus leads to higher incidence of post-traumatic osteoarthritis in trimalleolar fractures. Arch Orthop Trauma Surg. 2019;139:323-329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 74] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 18. | Mason LW, Marlow WJ, Widnall J, Molloy AP. Pathoanatomy and Associated Injuries of Posterior Malleolus Fracture of the Ankle. Foot Ankle Int. 2017;38:1229-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 113] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 19. | Evers J, Fischer M, Raschke M, Riesenbeck O, Milstrey A, Gehweiler D, Gueorguiev B, Ochman S. Leave it or fix it? How fixation of a small posterior malleolar fragment neutralizes rotational forces in trimalleolar fractures. Arch Orthop Trauma Surg. 2022;142:1031-1037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 20. | Ferries JS, DeCoster TA, Firoozbakhsh KK, Garcia JF, Miller RA. Plain radiographic interpretation in trimalleolar ankle fractures poorly assesses posterior fragment size. J Orthop Trauma. 1994;8:328-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 111] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Büchler L, Tannast M, Bonel HM, Weber M. Reliability of radiologic assessment of the fracture anatomy at the posterior tibial plafond in malleolar fractures. J Orthop Trauma. 2009;23:208-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 22. | Meijer DT, Doornberg JN, Sierevelt IN, Mallee WH, van Dijk CN, Kerkhoffs GM, Stufkens SA; Ankle Platform Study Collaborative – Science of Variation Group; Ankle Platform Study Collaborative - Science of Variation Group. Guesstimation of posterior malleolar fractures on lateral plain radiographs. Injury. 2015;46:2024-2029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 23. | Seo J, Yang KH, Shim DW, Cho H, Park YC. Marginal impaction associated with posterior malleolar fracture in rotational ankle injury. Injury. 2022;53:756-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Kumar A, Mishra P, Tandon A, Arora R, Chadha M. Effect of CT on Management Plan in Malleolar Ankle Fractures. Foot Ankle Int. 2018;39:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 25. | Bouche PA, Gaujac N, Corsia S, Leclerc P, Anract P, Auberger G. Ankle CT scan allows better management of posterior malleolus fractures than X-rays. Eur J Orthop Surg Traumatol. 2022;32:1301-1309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am. 2006;88:1085-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 193] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 27. | Bartoníček J, Rammelt S, Kostlivý K, Vaněček V, Klika D, Trešl I. Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg. 2015;135:505-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 180] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 28. | Mason LW, Kaye A, Widnall J, Redfern J, Molloy A. Posterior Malleolar Ankle Fractures: An Effort at Improving Outcomes. JB JS Open Access. 2019;4:e0058. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 29. | Sultan F, Zheng X, Pan Z, Zheng Q, Li H, Wang J. Characteristics of intercalary fragment in posterior malleolus fractures. Foot Ankle Surg. 2020;26:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 30. | Bartoníček J, Rammelt S, Tuček M, Naňka O. Posterior malleolar fractures of the ankle. Eur J Trauma Emerg Surg. 2015;41:587-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 31. | White TO. In defence of the posterior malleolus. Bone Joint J. 2018;100-B:566-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 32. | Donohoe S, Alluri RK, Hill JR, Fleming M, Tan E, Marecek G. Impact of Computed Tomography on Operative Planning for Ankle Fractures Involving the Posterior Malleolus. Foot Ankle Int. 2017;38:1337-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 33. | Zhang K, Jia X, Qiang M, Chen S, Wang S, Wang D, Chen Y. Quantitative Evaluation of Articular Involvement of Posterior Malleolus Associated with Operative Indication: A Comparative Study of Six Methods Based on Radiography and CT. Biomed Res Int. 2020;2020:6745626. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Tejwani NC, Pahk B, Egol KA. Effect of posterior malleolus fracture on outcome after unstable ankle fracture. J Trauma. 2010;69:666-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 35. | Stringfellow TD, Walters ST, Nash W, Ahluwalia R; Posterior Malleolus Study Group. Management of posterior malleolus fractures: A multicentre cohort study in the United Kingdom. Foot Ankle Surg. 2021;27:629-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Alluri RK, Hill JR, Donohoe S, Fleming M, Tan E, Marecek G. Radiographic Detection of Marginal Impaction in Supination-Adduction Ankle Fractures. Foot Ankle Int. 2017;38:1005-1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 37. | Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33:363-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2027] [Cited by in RCA: 2052] [Article Influence: 42.8] [Reference Citation Analysis (0)] |