Published online Nov 18, 2023. doi: 10.5312/wjo.v14.i11.836
Peer-review started: August 4, 2023
First decision: September 14, 2023
Revised: September 21, 2023
Accepted: October 25, 2023
Article in press: October 25, 2023
Published online: November 18, 2023
Processing time: 103 Days and 7 Hours
Cyclops lesions are a known complication of anterior cruciate ligament (ACL) reconstruction, with symptomatic cyclops syndrome occurring in up to 11% of surgeries. Recurrent cyclops lesions have been rarely documented; this case study documents the successful treatment of a recurrent cyclops lesion.
A 28-year-old female presented following a non-contact injury to the right knee. Workup and clinical exam revealed an ACL tear, and arthroscopic reconstruction was performed. Two years later a cyclops lesion was discovered and removed via arthroscopic synovectomy. Seven months postoperatively, the patient presented with pain, stiffness, and difficulty achieving terminal extension. A smaller re
To the best of our knowledge, this is the first documented case of recurrent cyclops lesion after bone-patellar tendon-bone allograft ACL reconstruction presenting as cyclops syndrome.
Core Tip: A 28-year-old female presented following a noncontact injury to the right knee. Workup and clinical exam revealed an anterior cruciate ligament tear, and arthroscopic reconstruction was performed. Two years later a cyclops lesion was discovered and removed via arthroscopic synovectomy. Seven months postoperatively, the patient presented with pain, stiffness, and difficulty achieving terminal extension. A smaller recurrent cyclops lesion was diagnosed, and a repeat synovectomy was performed. The patient recovered fully.
- Citation: Kelmer G, Johnson AH, Turcotte JJ, Redziniak DE. Recurrent cyclops lesion after primary anterior cruciate ligament reconstruction using bone tendon bone allograft: A case report. World J Orthop 2023; 14(11): 836-842
- URL: https://www.wjgnet.com/2218-5836/full/v14/i11/836.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i11.836
The cyclops lesion is a known complication following anterior cruciate ligament (ACL) reconstruction[1]. Initially described by Jackson and Schaefer[2] in 1990, a nodule of fibrous tissue with central granulation forms on the anterior aspect of the ACL graft and encroaches upon the intercondylar space. When this lesion is associated with a loss of terminal extension accompanied by symptoms such as pain, stiffness, or clunking with full extension, it is referred to as cyclops syndrome[2]. The incidence of cyclops lesions following ACL reconstruction is 25%-47%; however, many of these cases are asymptomatic, do not require surgical intervention, and are not associated with inferior clinical outcomes[3,4]. The rate of symptomatic cyclops lesions presenting as cyclops syndrome is much lower, at 0%-11%[5-8].
When a patient presents with an extension deficit following ACL reconstruction, magnetic resonance imaging (MRI) is the standard of diagnosis for cyclops lesions[3,5,8,9]. Physical therapy (PT) alone is not sufficient to restore full range of motion, arthroscopy with lesion excision is recommended[3,5,8]. Surgical management generally results in long-term resolution of the extension deficit[8-11]. In rare cases the cyclops lesion can recur. Only one such case was documented over two decades ago as part of a larger study on MRI of cyclops lesions[5]. In this report, we present the investigation of a recurrent cyclops lesion in a patient who sustained an ACL tear which was reconstructed using a bone-patellar tendon-bone allograft and ultimately underwent successful resection and rehabilitation.
A 28-year-old female patient presented to the clinic with a sports-related noncontact injury to her right knee.
The patient experienced a noncontact injury to her right knee while playing soccer nine days prior to presentation. She reports difficulty ambulating and instability in the knee.
No prior knee injuries.
Personal and family history was non-contributory.
Examination revealed a painful right knee with effusion, tenderness along the lateral joint line, and positive Lachman test.
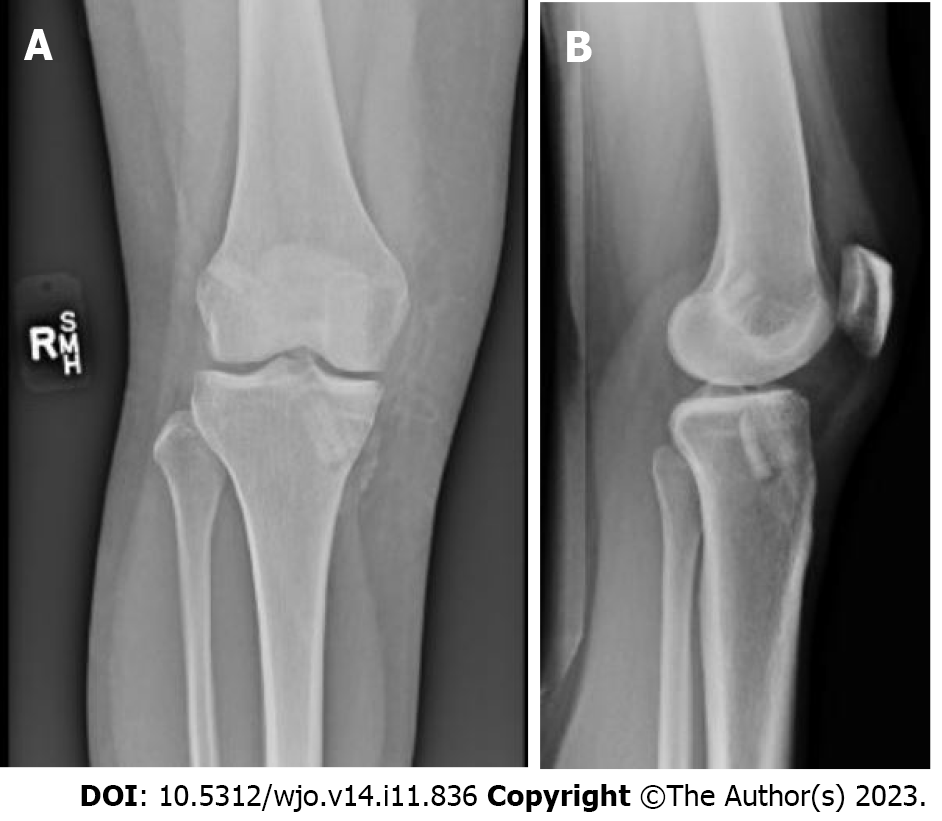
MRI demonstrated a complete tear of the ACL with associated bone contusions (Figure 1).
Recurrent cyclops lesion.
One week after initial presentation she was re-evaluated and arthroscopic ACL reconstruction was recommended, graft options were reviewed with the patient and a bone tendon bone allograft was selected as her graft of choice. She was provided a derotational brace, and referral to PT. Approximately 2.5 mo following the initial injury, reconstruction of the right ACL using bone-patellar tendon-bone allograft was performed. Body mass index (BMI) at the time of surgery was 29.9 kg/m2. The femoral tunnel was prepared using an anteromedial portal technique utilizing a limited notchplasty. Bioabsorbable interference screws were used for both femoral and tibial fixation. The knee was placed in extension with a posterior drawer applied to the proximal tibia for final fixation. Figure 2 shows postoperative X-rays indicating appropriate tunnel placement. There were no complications and recovery and PT progressed as expected. She returned to all activities without restrictions.
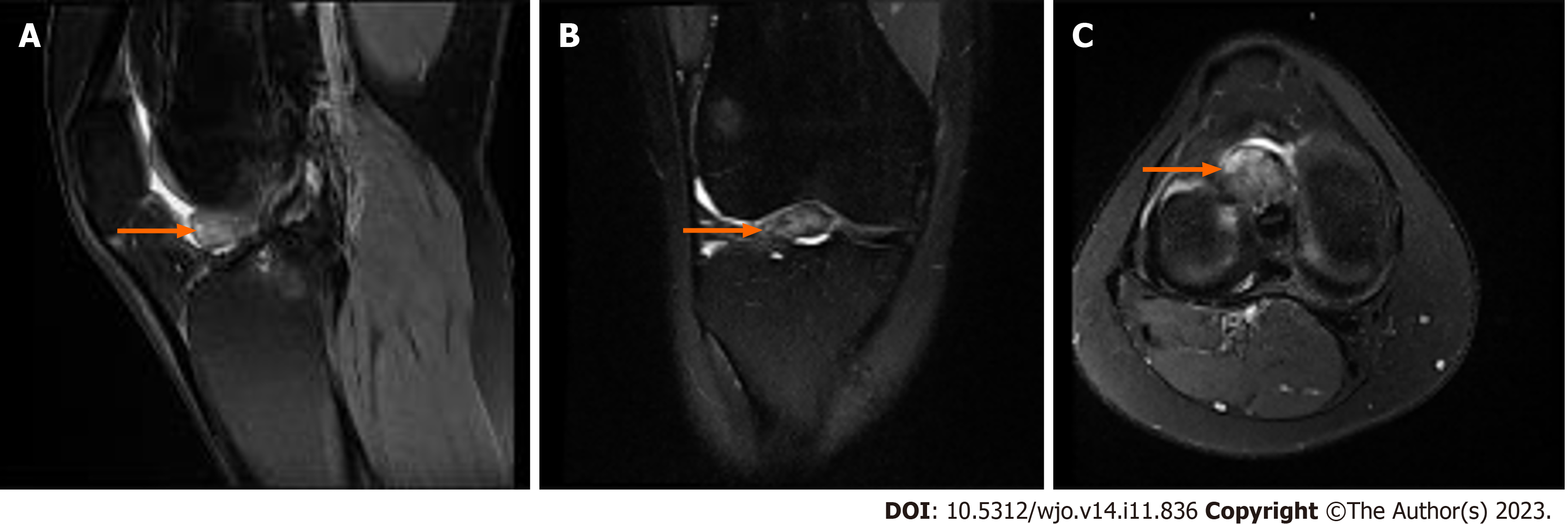
Two years after the ACL repair, the patient sustained a repeat injury to her right knee, presenting about a month after this incident. The patient reported feeling a pop and medial-sided knee pain. Physical examination revealed swelling, medial joint line tenderness, and positive McMurray test. Radiographs were unremarkable. MRI demonstrated an intact ACL graft with a moderate-sized cyclops lesion estimated at a size of 16 mm × 17 mm × 11 mm (Figure 3). After 8 wk of PT, she still complained of stiffness and moderate pain with knee extension. Right knee arthroscopic synovectomy was recommended, and the patient proceeded with surgery approximately 1 mo later. BMI at the time of surgery was 26.7 kg/m2.
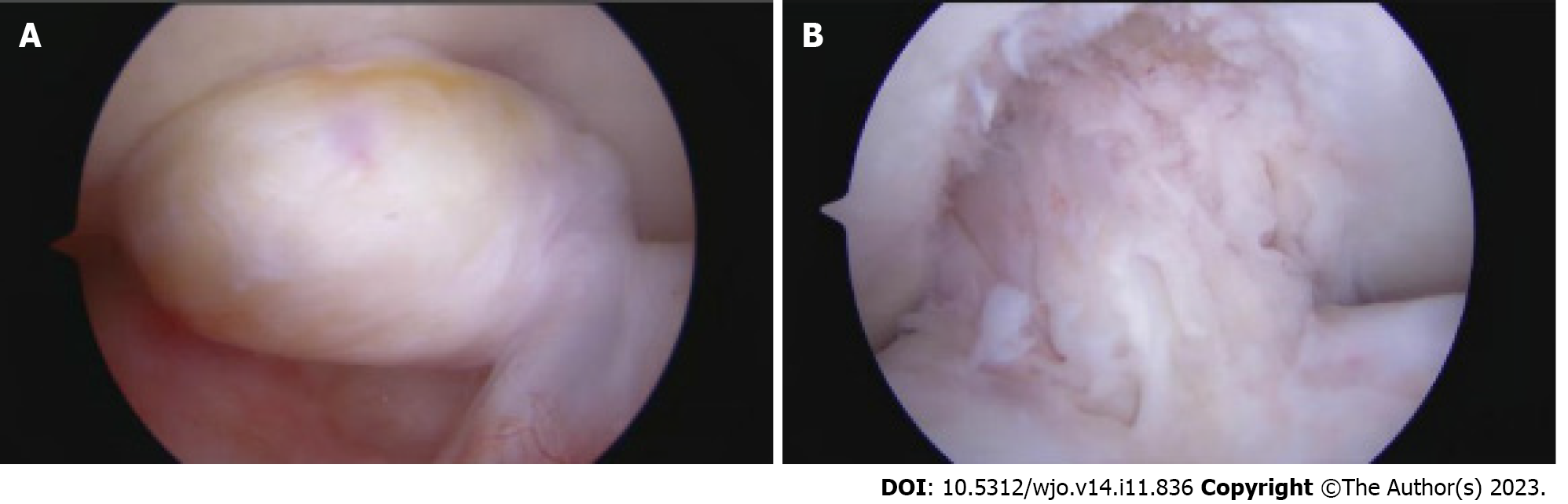
Intraoperatively, there was an isolated cyclops lesion appreciated at the insertion of the ACL on the proximal tibia, which impinged in the intercondylar notch with terminal extension (Figure 4). A biter and mechanical shaver were used to remove the lesion. Both the ACL and posterior cruciate ligament (PCL) were noted to be intact. Femoral and tibial tunnels were found to be in appropriate position without evidence of notch impingement. Arthroscopic images were taken of the intact cyclops lesion, pre and post arthroscopic debridement. The patient was found to have a stable knee on examination under anesthesia. There were no surgical complications. Postoperatively PT was started immediately, emphasizing obtaining terminal extension with unrestricted passive and active motion. Knee Injury and Osteoarthritis Outcome Score (KOOS) was 76.33 6 wk following surgery.
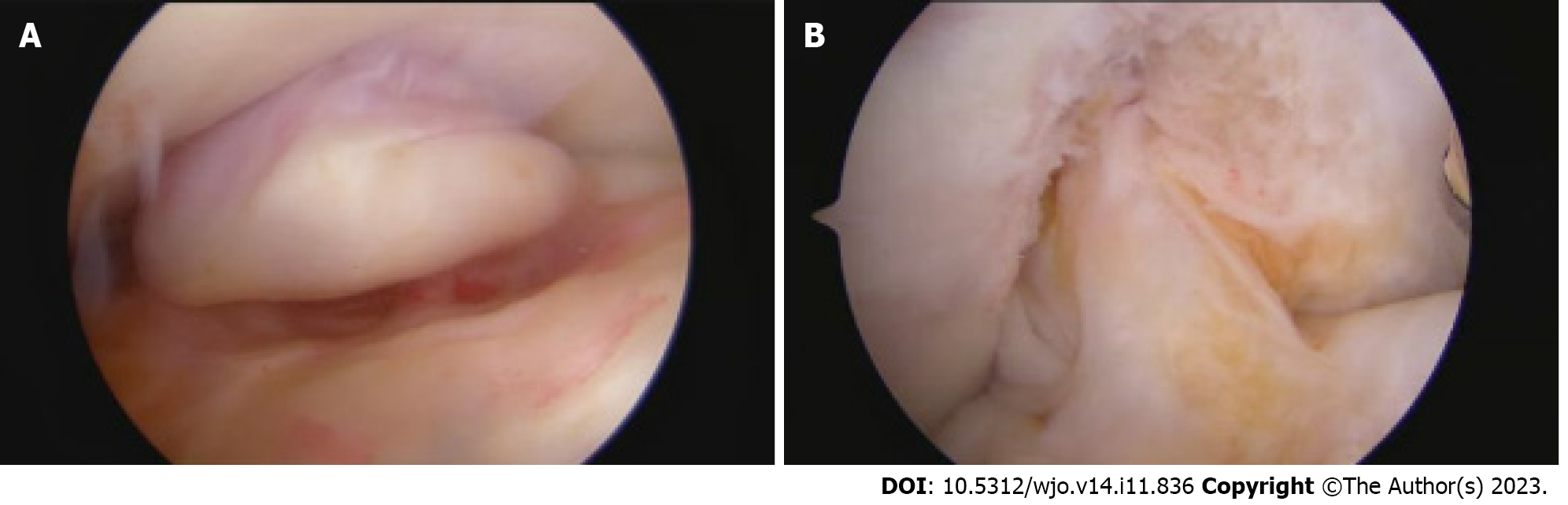
Seven months postoperatively, the patient presented with complaints of tightness and stiffness of her right knee, difficulty achieving terminal extension, and pain in the anteromedial aspect of her right tibia. An MRI was obtained, demonstrating intact ACL reconstruction with a smaller recurrent mass estimated at a size of 5 mm × 9 mm × 10 mm along the anterior margin of the distal ACL consistent with a recurrent cyclops lesion (Figure 5). Recurrent arthroscopic debridement was recommended after 8 wk of PT failed to improve her symptoms. Biopsy at the time of surgical intervention was also recommended to evaluate for recurrent synovial lesions such as pigmented villonodular synovitis. Two months later, the patient proceeded with a right arthroscopy and debridement of the right knee. BMI at the time of surgery was 27.1 kg/m2. KOOS one week prior to surgery was 44.91.
Repeat arthroscopy demonstrated a recurrent cyclops lesion adjacent to the anterior aspect of the ACL reconstruction (Figure 6). The ACL and PCL were intact. The medial and lateral compartments showed no meniscus tears or arthritis. A straight biter and grasper were used to obtain biopsies of the cyclops lesion. A mechanical shaver was then used to remove the cyclops lesion in its entirety from the intercondylar notch. Full range of motion with terminal flexion and extension was verified. Arthroscopic images were taken, and the recurrent cyclops lesion was sent for biopsy. Surgery was completed with no complications.
Pathologic analysis determined the excised mass was composed of synovial tissue with fibrosis and reactive fibrocartilage, consistent with a recurrent cyclops lesion. At 6 wk postoperatively, the patient was progressing through PT and was able to achieve terminal extension. The patient attended PT for 8 wk. By the end of PT, right knee active range of motion (ROM) reached 0-140 degrees, symmetric with the contralateral knee. Upon completion of PT she was able to resume all activities without restrictions.
Nineteen months after arthroscopy for recurrent cyclops lesion, the patient retained full function of the knee with no recurrent stiffness, full active and passive ROM, and able to perform all normal daily and athletic activities without pain; she denies any local recurrence to date. KOOS was 100 and Lysholm score was 100% at final follow up.
The mechanism of development and risk factors for cyclops lesions are still under investigation, and the incidence of recurrent cyclops lesions is sparsely documented. The commonly proposed origin of cyclops lesions is development as a result of an inflammatory reaction to remnants of the ruptured ACL[1,6]. Studies have found preservation of ACL remnants was not associated with cyclops lesions or cyclops syndrome, and minimal debridement during ACL repair did not increase incidence of cyclops lesions[4,6,8]. Tomihara et al[12] recently found that bone-patellar-tendon-bone autograft, female sex, and increased BMI were significant risk factors for cyclops lesions and syndrome. Conversely, Facchetti et al[3] reported no association of cyclops lesion incidence with factors such as graft type or sex but did find a positive correlation with lower patient BMI. Based on direct contradictions in the literature, it is difficult to theorize which demographic or surgical factors may have influenced the repeated development of cyclops lesions in our patient. Additional factors that have been associated with the development of cyclops lesions following ACL reconstruction include increased graft volume, double-bundle grafts, smaller femoral and tibial tunnel diameter and excessively anterior tibial tunnels, although none of these appear to be contributory in our patient[7,13,14].
It is suggested that early loss of extension following ACL reconstruction allows space for the cyclops lesion to form[4,6,15]. Gohil et al[4] found that multiple patients who experienced loss of extension 2 mo postoperatively did not demonstrate cyclops lesion on MRI, but they subsequently developed cyclops lesions with smaller extension deficits. At 3 and 6 wk postoperatively, Pinto et al[15] reported an extension deficit was associated with a significant increase in the incidence of cyclops lesions. The major risk factor for cyclops syndrome discovered by Delaloye et al[6] was an extension deficit at 3 and 6 wk following ACL reconstruction. The patient presented in our case progressed well through PT following both her ACL reconstruction and initial cyclops lesion excision and at no point in time did she have an extension deficit.
The only other known case of a recurrent cyclops lesion was reported by Bradley et al[5] in their investigation of the utility of MRI for diagnosis of cyclops lesions; four months following excision of the initial lesion, one patient demonstrated a recurrent cyclops lesion. The major difference between this case and our case lies in the presentation; the Bradley et al[5] lesion was discovered incidentally on postoperative MRI, whereas our patient returned 7 mo postoperatively with cyclops syndrome. Previous literature reports cyclops lesions are predominantly asymptomatic, do not confer poorer clinical outcomes, and do not show an association between lesion size and pain or other symptoms[3]. It is unclear to what extent our patient’s cyclops lesions contributed to her clinical presentation. A key aspect may have been the trauma of her repeated valgus injuries, the first causing her ACL tear and the second about two years after the repair. Both recurrent cyclops lesions were successfully managed with repeat arthroscopy and excision[5].
While cyclops lesions following ACL reconstruction are a common complication, recurrent cyclops lesions are minimally documented. Here, we describe what is, to the best of our knowledge, the first known case of a recurrent cyclops lesion presenting as cyclops syndrome. Future studies should be aimed at reconciling which demographic and surgical factors contribute to the development of cyclops lesions and syndrome.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Batta A, India S-Editor: Qu XL L-Editor: A P-Editor: Qu XL
| 1. | Kulczycka P, Larbi A, Malghem J, Thienpont E, Vande Berg B, Lecouvet F. Imaging ACL reconstructions and their complications. Diagn Interv Imaging. 2015;96:11-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Jackson DW, Schaefer RK. Cyclops syndrome: loss of extension following intra-articular anterior cruciate ligament reconstruction. Arthroscopy. 1990;6:171-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 205] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | Facchetti L, Schwaiger BJ, Gersing AS, Guimaraes JB, Nardo L, Majumdar S, Ma BC, Link TM, Li X; UCSF-P50-ACL Consortium; AF-ACL Consortium. Cyclops lesions detected by MRI are frequent findings after ACL surgical reconstruction but do not impact clinical outcome over 2 years. Eur Radiol. 2017;27:3499-3508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Gohil S, Falconer TM, Breidahl W, Annear PO. Serial MRI and clinical assessment of cyclops lesions. Knee Surg Sports Traumatol Arthrosc. 2014;22:1090-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Bradley DM, Bergman AG, Dillingham MF. MR imaging of cyclops lesions. AJR Am J Roentgenol. 2000;174:719-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 66] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Delaloye JR, Murar J, Vieira TD, Franck F, Pioger C, Helfer L, Saithna A, Sonnery-Cottet B. Knee Extension Deficit in the Early Postoperative Period Predisposes to Cyclops Syndrome After Anterior Cruciate Ligament Reconstruction: A Risk Factor Analysis in 3633 Patients From the SANTI Study Group Database. Am J Sports Med. 2020;48:565-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 7. | Noailles T, Chalopin A, Boissard M, Lopes R, Bouguennec N, Hardy A. Incidence and risk factors for cyclops syndrome after anterior cruciate ligament reconstruction: A systematic literature review. Orthop Traumatol Surg Res. 2019;105:1401-1405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Kambhampati SBS, Gollamudi S, Shanmugasundaram S, Josyula VVS. Cyclops Lesions of the Knee: A Narrative Review of the Literature. Orthop J Sports Med. 2020;8:2325967120945671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Wang J, Ao Y. Analysis of different kinds of cyclops lesions with or without extension loss. Arthroscopy. 2009;25:626-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Tonin M, Saciri V, Veselko M, Rotter A. Progressive loss of knee extension after injury. Cyclops syndrome due to a lesion of the anterior cruciate ligament. Am J Sports Med. 2001;29:545-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Mayr HO, Brandt CM, Weig T, Koehne M, Bernstein A, Suedkamp NP, Hube R, Stoehr A. Long-term Results of Arthroscopic Arthrolysis for Arthrofibrosis After Anterior Cruciate Ligament Reconstruction. Arthroscopy. 2017;33:408-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Tomihara T, Hashimoto Y, Nishino K, Taniuchi M, Takigami J, Tsumoto S, Katsuda H. Bone-patellar tendon-bone autograft and female sex are associated with the presence of cyclops lesions and syndrome after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2023;31:2762-2771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 13. | Moran TE, Taleghani ER, Ruland JR, Ignozzi AJ, Hart J, Diduch DR. An analysis of the incidence, risk factors, and timing of development of cyclops lesions after anterior cruciate ligament reconstruction. Knee. 2023;40:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 14. | Fujii M, Furumatsu T, Miyazawa S, Okada Y, Tanaka T, Ozaki T, Abe N. Intercondylar notch size influences cyclops formation after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23:1092-1099. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Pinto FG, Thaunat M, Daggett M, Kajetanek C, Marques T, Guimares T, Quelard B, Sonnery-Cottet B. Hamstring Contracture After ACL Reconstruction Is Associated With an Increased Risk of Cyclops Syndrome. Orthop J Sports Med. 2017;5:2325967116684121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |