Published online Nov 18, 2023. doi: 10.5312/wjo.v14.i11.813
Peer-review started: August 16, 2023
First decision: September 19, 2023
Revised: September 21, 2023
Accepted: October 16, 2023
Article in press: October 16, 2023
Published online: November 18, 2023
Processing time: 91 Days and 21.6 Hours
Superior capsular reconstruction (SCR) with long head of biceps tendon (LHBT) transposition was developed to massive and irreparable rotator cuff tears (MIRCTs); however, the outcomes of this technique remain unclear.
To perform a systematic review of biomechanical outcomes and a meta-analysis of clinical outcomes after LHBT transposition for MIRCTs.
We performed a systematic electronic database search on PubMed, EMBASE, and Cochrane Library. Studies of SCR with LHBT transposition were included according to the inclusion and exclusion criteria. Biomechanical studies were assessed for main results and conclusions. Included clinical studies were evaluated for quality of methodology. Data including study characteristics, cohort demographics, and outcomes were extracted. A meta-analysis was conducted of the clinical outcomes.
According to our inclusion and exclusion criteria, a total of six biomechanical studies were identified and reported an overall improvement in subacromial contact pressures and prevention of superior humeral migration without limiting range of motion (ROM) after LHBT transposition for MIRCTs. A total of five clinical studies were included in the meta-analysis of LHBT transposition outcomes, consisting of 253 patients. The results indicated that compared to other surgical methods for MIRCTs, LHBT transposition had advantages of more significant improvement in ROM (forward flexion mean difference [MD] = 6.54, 95% confidence interval [CI]: 3.07-10.01; external rotation [MD = 5.15, 95%CI: 1.59-8.17]; the acromiohumeral distance [AHD] [MD = 0.90, 95%CI: 0.21-1.59]) and reducing retear rate (odds ratio = 0.27, 95%CI: 0.15-0.48). No significant difference in American Shoulder and Elbow Surgeons score, visual analogue scale score, and University of California at Los Angles score was demonstrated between these two groups for MIRCTs.
In general, SCR with LHBT transposition was a reliable and economical technique for treating MIRCTs, both in terms of biomechanical and clinical outcomes, with comparable clinical outcomes, improved ROM, AHD, and reduced the retear rates compared to conventional SCR and other established techniques. More high-quality randomized controlled studies on the long-term outcomes of SCR with LHBT transposition are required to further assess.
Core Tip: Superior capsular reconstruction (SCR) with long head of biceps tendon (LHBT) transposition was developed to massive and irreparable rotator cuff tears (MIRCTs). However, the outcomes of this technique remain unclear. SCR with LHBT transposition is a reliable and economical technique for treating MIRCTs, both in terms of biomechanical and clinical outcomes, with comparable clinical outcomes, improved range of motion, acromiohumeral distance, and reduced the retear rates compared to conventional SCR and other established techniques.
- Citation: Wan RW, Luo ZW, Yang YM, Zhang HL, Chen JN, Chen SY, Shang XL. Long head of biceps tendon transposition for massive and irreparable rotator cuff tears: A systematic review and meta-analysis. World J Orthop 2023; 14(11): 813-826
- URL: https://www.wjgnet.com/2218-5836/full/v14/i11/813.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i11.813
Rotator cuff tears are one of the most common musculoskeletal disorders, affecting between 15% and 50% of the population, and increasing in prevalence with age[1]. The prevalence of massive and irreparable rotator cuff tears (MIRCTs) is reportedly as high as 40% in rotator cuff tears[2,3]. The rotator cuff works as a dynamic stabilizer of the glenohumeral joint, and MIRCTs will cause the absence of this stabilizer, with the head migrating superiorly and anteriorly, leading to abnormal wear and tear of the head and glenohumeral joint[4,5]. If left untreated, the MIRCTs may lead to permanent pain and loss of function, eventually resulting in rotator cuff arthropathy.
The repair of MIRCTs still remains a surgical challenge due to muscle fat infiltration, tendon retraction, and tissue degeneration. Numerous surgical management options for MIRCTs are available, including debridement and sub
Superior capsular reconstruction (SCR) is considered a possible option for treating MIRCTs and restoring superior glenohumeral stability and shoulder function, which was first described by Mihata et al[18] in 2013. The graft used is a tensor fasciae lata (TFL) autograft that attaches medially to the superior glenoid and laterally to the greater tuberosity. Recently, the long head of biceps tendon (LHBT) has been proposed as an alternative to the standard SCR graft, which seems to overcome the problems of donor site morbidity, feasibility of grafting, and additional costs of allografting[19]. When performing the LHBT transposition technique, the native LHBT connection on the glenoid side was preserved. The proximal portion of the LHBT, was then transposed posteriorly and fixed on the supraspinatus tendon footprint as the SCR.
Currently, biomechanical studies have been carried out to observe the biomechanical effects of LHBT transposition for MIRCTs[20-22]. Meanwhile, few previous clinical studies have reported promising clinical outcomes after LHBT transposition for MIRCTs[23-25]; however, it remains unknown about the reliability of this technique. The purpose of this study was to perform a systematic review of biomechanical outcomes and a meta-analysis of clinical outcomes after LHBT transposition for MIRCTs. We hypothesized that LHBT transposition would effectively restore joint biomechanics compared with the unrepaired state and improve overall shoulder function, the acromiohumeral distance (AHD) and decrease the retear rate of repaired rotator cuff.
This meta-analysis and systematic review was written according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines[26].
Two independent authors (Wan RW and Luo ZW) performed an electronic search in three databases between their inception date and May 20, 2022: MEDLINE (PubMed), EMBASE (Ovid), and Cochrane Library. The Boolean search phrase was “(superior capsul* reconstruction OR superior capsul* repair OR superior labr* reconstruction OR superior labr* repair OR rotator cuff repair) AND (biceps).” The reference lists of correlational studies were also reviewed.
Inclusion criteria consisting of biomechanical studies were as follows: (1) Cadaveric shoulders with massive or irreparable rotator cuff tears; (2) LHBT transposition was used in cadaveric shoulders; and (3) articles written in English or with an English translation.
Inclusion criteria consisting of clinical studies were as follows: (1) LHBT transposition was used to treat rotator cuff tears; (2) Rotator cuff tears were large to massive or irreparable; (3) Postoperative functional outcomes were reported; and (4) Articles were written in English or had an English translation.
The exclusion criteria were as follows: (1) Computational-based or animal studies; (2) editorial letters or letters to the editor, case reports, technical notes, expert consensuses, systematic and narrative reviews, pilot studies, unpublished manuscripts, book chapters, lectures, meeting abstracts, conference proceedings, or dissertations; (4) superior labrum anterior and posterior (SLAP) injury or LHBT injury; (5) SCR without using LHBT transposition; and (6) clinical studies not reporting preoperative and postoperative outcomes or without enough information for data analyses.
After duplicates were removed, two independent authors (Wan RW and Luo ZW) evaluated all titles and abstracts for relative articles. If these data were inadequate, full texts were assessed to judge if studies met the inclusion criteria. If there was an objection concerning the inclusion of studies, studies were judged by the senior author (Shang XL) to make the final decision.
After assessing full-text articles for eligibility and applying the inclusion/exclusion criteria, the following information were extracted: study type, level of evidence, first author, publication year, country, number of patients, mean age, mean duration of follow-up, surgical technique, and postoperative clinical outcomes, and postoperative retear rates. The primary outcomes of interest were American Shoulder and Elbow Surgeons (ASES) score, visual analogue scale (VAS) score (0-10 [10 = severe pain]), University of California at Los Angles (UCLA) score, range of motion (ROM) including active external rotation at side (ER0; degrees), active forward flexion (FF; degrees), AHD, and retear rates. For studies with insufficient information, the reviewers contacted the primary authors, when possible, to acquire and verify the data.
Given the abundance of nonrandomized studies in the available literature, two independent reviewers (Wan RW and Luo ZW) critically appraised all eligible studies using Methodological Index for Nonrandomized Studies (MINORS) to evaluate their quality[27]. If a consensus was not achieved, a senior reviewer (Shang XL) made the final decision on the assessment. The MINORS instrument consists of 12 items: 4 for comparative studies only and 8 for noncomparative and comparative studies. A score of 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate) was suggested for each item, resulting in an ideal maximum score of 16 for noncomparative studies and 24 for comparative studies. For nonrandomized comparative studies, the methodologic quality was classified as follows: 0-12, low quality; 13-18, fair quality; and 19-24, good quality. The outcomes of the risk of bias and quality assessment offered context for the conclusions to be drawn from this review.
Statistical analyses were performed by using Review Manager, version 5.4 (Nordic Cochrane Centre, Cochrane Collaboration). The mean difference (MD) and odds ratio (OR) were used to compare continuous and dichotomous variables, respectively. All results were reported with 95% confidence intervals (CIs). P < 0.05 was considered statistically significant. I2 test was performed to assess the impact of study heterogeneity on the results of the meta-analysis. According to the Cochrane review guidelines, if severe heterogeneity was present at I2 > 50%, the random effect models were chosen. If I2 ≤ 50%, multiple similar studies were considered to be homogeneous, and the fixed effects model was used to combine the statistical values. The results are summarized in forest plots.
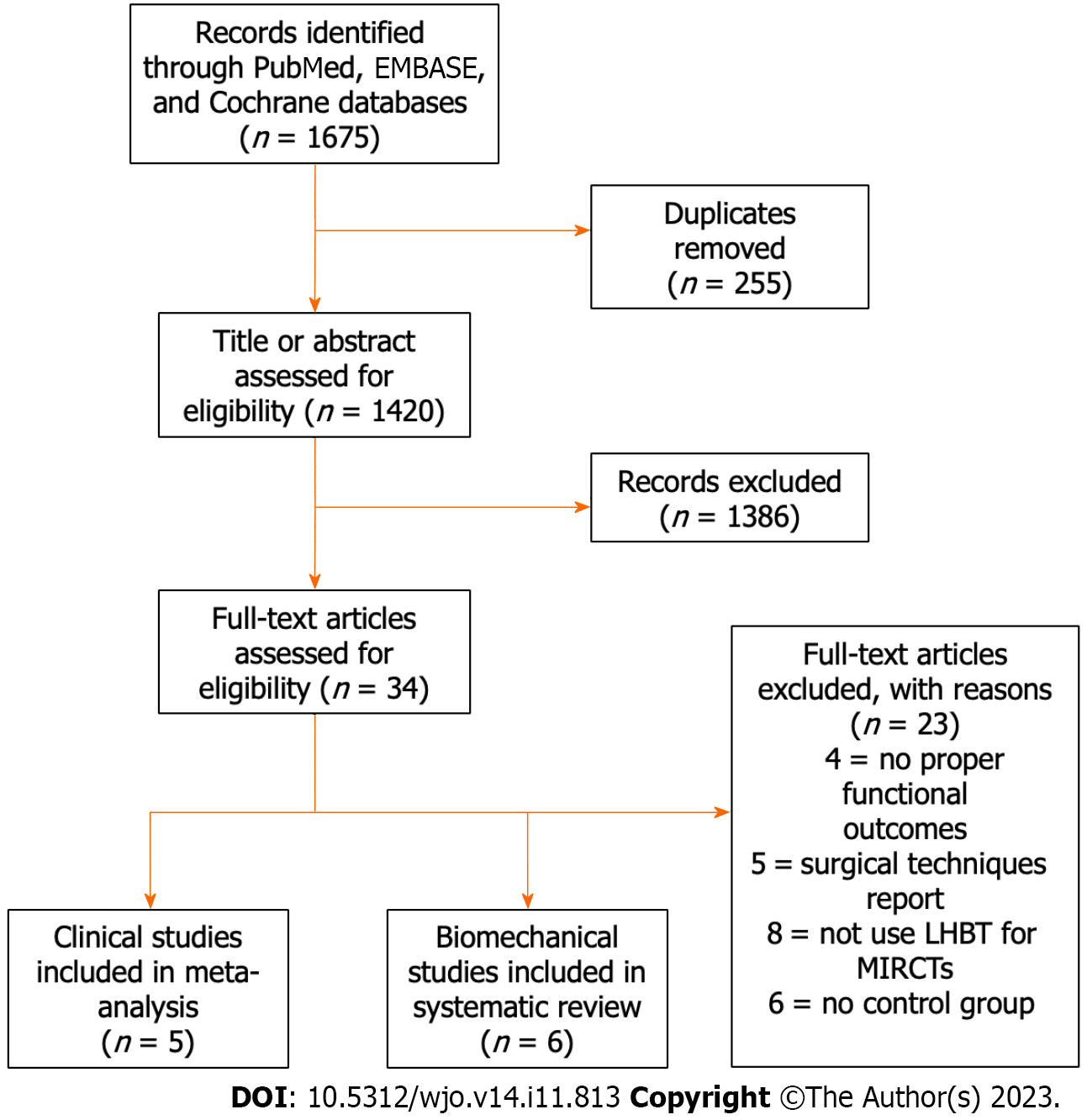
The initial literature search yielded 1675 articles (Figure 1). After removing duplicates, 1420 studies were screened for title and abstract, resulting in 34 full-text articles being assessed for eligibility. After the application of inclusion and exclusion criteria, six articles[21,28-32] reported biomechanical outcomes and five articles[33-37] reported clinical outcomes were identified for further analysis.
The MINORS scores of two retrospective control clinical studies[33,34] were ≥ 19 points, indicating good quality of evidence. The MINORS scores of three other retrospective control clinical studies[35-37] were > 13 points, indicating fair quality of evidence (Table 1).
| Ref. | Study type/LOE | A clearly stated aim | Inclusion of consecutive patients | Prospective collection of data | Endpoints appropriate to the aim of the study | Unbiased assessment of the study endpoint | Follow-up period appropriate to the aim of the study | Loss to follow up less than 5% | Prospective calculation of the study size | An adequate control group | Contemporary groups | Baseline equivalence of groups | Adequate statistical analyses | Score |
| Barth et al[37], 2020 | III, retrospective control study | 2 | 1 | 2 | 2 | 1 | 2 | 1 | 0 | 2 | 1 | 2 | 0 | 16 |
| Kocaoglu et al[34], 2020 | III, retrospective control study | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 20 |
| Rhee et al[33], 2021 | III, retrospective control study | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 19 |
| Chiang et al[36], 2021 | III, retrospective control study | 2 | 1 | 2 | 2 | 1 | 2 | 1 | 0 | 1 | 1 | 2 | 0 | 15 |
| Kawashima et al[35], 2022 | III, retrospective control study | 2 | 1 | 2 | 2 | 1 | 2 | 1 | 0 | 1 | 2 | 2 | 0 | 16 |
The characteristics and main results of included biomechanical studies are shown in Table 2. Because of the heterogeneity of testing conditions and outcome reporting, no meaningful statistical analyses could be performed. Overall, LHBT transposition for MIRCTs was reported to improve subacromial contact pressures and prevent superior humeral migration without limiting ROM.
| Ref. | Number of shoulders | Age, yr | Surgical technique | Testing conditions/groups | Testing method | Main results | Main conclusion |
| Park et al[22], 2018 | 9 | 58 (33-77) | ACR using autologous proximal biceps tendon for large to massive rotator cuff tears | (1) Intact; (2) Stage II tear (complete tear of the supraspinatus); (3) ACR for stage II tear; (4) Stage III tear (complete tear of the supraspinatus and anterior one-half of the infraspinatus); and (5) ACR for stage III tear | Range of motion, superior translation of the humeral head, and subacromial contact pressure were measured at 0°, 30°, 60°, and 90° of ER with 0°, 20°, and 40° of glenohumeral abduction | ACR for both stage II and stage III showed significantly higher total range of motion compared with intact at all angles. ACR significantly decreased superior translation for stage II tears at 0°, 30°, and 60° ER for both 0° and 20° abduction and for stage III tears at 0° and 30° ER for both 0° and 20° abduction. ACR for stage III tear significantly reduced peak subacromial contact pressure at 30° and 60° ER with 0° and 40° abduction and at 30° ER with 20° abduction | ACR using autologous biceps tendon biomechanically normalized superior migration and subacromial contact pressure, without limiting range of motion |
| El-shaar et al[21], 2018 | 10 (5 matched pairs) | 63 (59-67) | SCR utilizing a LHB autograft or TFL autograft | (1) After a massive RC tear without SCR; and (2) After SCR with either a TFL autograft or an LHB autograft | Cadaveric demographics, mean force required to superiorly translate the humerus, and change in mean force when normalized to the torn condition were recorded | SCR with an LHB autograft required 393.2% ± 87.9% of the force needed for superior humeral migration in the massive RC tear condition, while SCR with a TFL autograft required 194.0% ± 21.8%. The LHB reconstruction group trended toward a stronger reconstruction when normalized to the torn condition | SCR with an LHB autograft is a feasible procedure that is shown to be biomechanically equivalent and potentially even stronger than SCR with a TFL autograft in the prevention of superior humeral migration |
| Han et al[30], 2019 | 7 | 50-65 | SCR using the LHBT or using the LHBT with side-to-side repair | (1) Intact; (2) Simulated complete supraspinatus tendon tear; (3) Modified SCR using LHB; and (4) Modified SCR using LHB and side-to-side repair augmentation | Superior translation of the humerus, subacromial contact pressure and area, and glenohumeral range of motion were tested at 0°, 30°, and 60° of glenohumeral abduction | The complete cuff tear shifted the humeral head superiorly as compared to the intact shoulder. Subacromial peak contact pressure was also increased at 30° and 60° while contact area was increased at 0° and 30°. The modified SCR both with and without side-to-side repair shifted the humeral head inferiorly at 30° and 60°, with contact area further reduced at 60°. Both techniques had comparable results for contact pressure and total rotational range of motion | The LHB with appropriate distal insertion on the greater tuberosity restores shoulder stability in irreparable rotator cuff tears by re-centering the humeral head on the glenoid |
| Han et al[29], 2020 | 8 | 65 (56-69) | PR, BR and BRSS | (1) Intact; (2) IRCT; (3) PR; (4) BR; and (5) BRSS | Total rotational range of motion was measured at 40°, then 20°, and finally 0° of glenohumeral abduction. Superior humeral translation and subacromial contact pressure were measured at 0°, 30°, 6 0°, and 90° of external rotation at each abduction angle | Superior humeral translation was significantly decreased in the BR and BRSS conditions compared with the IRCT and PR conditions at 0° and 20° of GH abduction (P < 0.001). BR and BRSS significantly reduced subacromial contact pressure compared with IRCT and PR at 0° of GH abduction (P < 0.001). There was no significant decrease in total rotational range of motion after BR at any abduction angle | BR biomechanically restored shoulder stability without over constraining range of motion in an IRCT model |
| Berthold et al[32], 2021 | 8 | 53.4 ± 14.2 (20-64) | SCR with V- shaped LHBT reconstruction, box-shaped LHBT reconstruction or single-stranded LHBT reconstruction | (1) Intact; (2) Irreparable psRCT; (3) V-shaped LHBT reconstruction; (4) Box-shaped LHBT reconstruction; and (5) Single-stranded LHBT reconstruction | ghST, MAA, maximum cDF, and sCP were accessed and recorded in each condition | Each of the 3 LHBT techniques for reconstruction of the superior capsule significantly increased MAA while significantly decreasing ghST and cDF compared with the psRCT. Additionally, the V-shaped and box-shaped techniques significantly decreased sCP compared with the psRCT. The V-shaped technique further showed a significantly increased MAA and decreased cDF when compared with the box-shaped and single-stranded techniques, as well as a significantly decreased ghST when compared with the box-shaped technique | Using the LHBT for reconstruction of the superior capsule improved shoulder function by preventing superior humeral migration, decreasing deltoid forces and sCP |
| Denard et al[31], 2021 | 8 | 62 (46-70) | SCR with box-shaped LHBT reconstruction or single-limb LHBT reconstruction | (1) Intact state; (2) A stage III MCT model (complete supraspinatus and anterior one-half of the infraspinatus); (3) Box Biceps SCR; and (4) Single-limb biceps | A custom testing system used to evaluate range of motion, superior translation, and subacromial contact pressure at 0°, 20°, and 40° of abduction | Range of motion was not impaired with either repair construct (P > 0.05). The box SCR decreased superior translation by approximately 2 mm compared with the MCT at 0°, but translation remained greater compared with the intact state in nearly every testing position. The in situ tenodesis had no effect on superior translation. Peak subacromial contact pressure was increased in the MCT at 0° and 20°. Abduction compared with the native state but not different between the native and box SCR at the same positions | A box-shaped SCR using the native biceps tendon partially restores increased superior translation and peak subacromial contact pressure due to MCT. The technique may have a role in augmentation of an IMCT |
A total of five studies meeting inclusion criteria were included in the meta-analysis of LHBT transposition outcomes, consisting of 253 patients. The study characteristics are presented in Table 3. We considered LHBT transposition for MIRCTS as the intervention group and other surgical methods for MIRCTs, i.e. the double-row repair, the transosseous-equivalent technique with absorbable patch reinforcement, the traditional SCR with a fascia lata autograft, arthroscopic rotator cuff repair (ARCR) alone, ARCR and tenotomy of LHBT, as the control group.
| Ref. | Country | Journal | Level of evidence, study type | Groups | No. of shoulder in group | Male:female sex | Age, yr | Follow-up, mo | Outcomes |
| Barth et al[37], 2020 | France | Am J Sports Med | 3, retrospective study | DR vs TOE with absorbable patch reinforcement vs SCR with LHBT autograft | 28 vs 30 vs 24 | 15:13 vs 19:11 vs 16:8 | 63 ± 9 (48-83) vs 59 ± 7.6 (45-71) vs 60 ± 7 (47-81) | 25 ± 2 (24-29) vs 27 ± 5 (24-36) vs 25 ± 2 (24-29) | ASES score, VAS score, constant score, range of motion, simple shoulder test, subjective shoulder value, muscle strength, retear rate |
| Kocaoglu et al[34], 2020 | Turkey | Orthop J Sports Med | 3, retrospective study | SCR with LHBT autograft vs SCR with a tensor fasciae lata autograft | 14 vs 12 | N/A | 64.6 ± 8.4 vs 62.5 ± 6.5 | 28 vs 32 | ASES score, VAS score, QuickDASH, range of motion, AHD, retear rate |
| Rhee et al[33], 2021 | Korea | Arthroscopy | 3, retrospective study | ARCR + BR vs ARCR | 59 vs 52 | 32:27 vs 29:23 | 63.7 ± 6.5 vs 62.8 ± 6.9 | 15.1 ± 3.4 vs 25.1 ± 8.7 | ASES score, VAS score, constant score, UCLA score, range of motion, muscle strength, AHD, retear rate |
| Chiang et al[36], 2021 | China (Taiwan) | Arthroscopy | 3, retrospective study | ARCR and SCR with LHBT autograft vs ARCR and tenotomy of LHBT performed at the insertion site | 18 vs 22 | 7:11 vs 6:16 | 62.3 ± 7.5 vs 62.2 ± 6.1 | 26.6 ± 3.9 (24-38) vs 31.9 ± 6.4 (26-45) | ASES score, VAS score, UCLA score, rang of motion, AHD, retear rate |
| Kawashima et al[35], 2022 | Japan | Arthroscopy | 3, retrospective study | partial repair vs SCR with LHBT transposition | 10 vs 12 | 6:4 vs 7:5 | 71.9 ± 7.5 vs 67.8 ± 2.0 | 37.2 (24-72) vs 24.8 (24-30) | ASES score, UCLA score, rang of motion, AHD, retear rate |
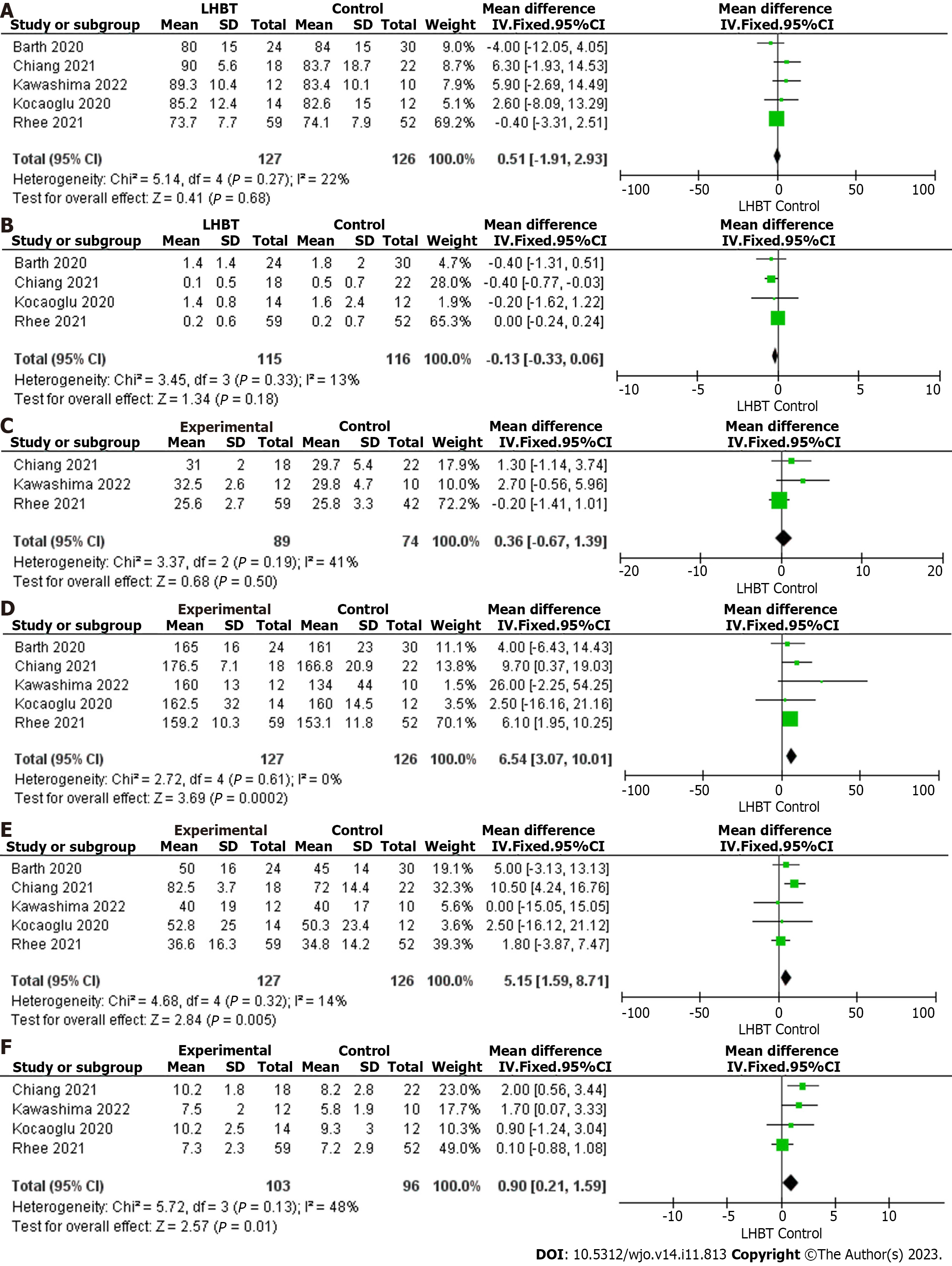
Patients were clinically assessed both preoperatively and postoperatively on a number of outcome-based scores that included ASES score, VAS score, UCLA score, ROM, AHD, and retear rates. ASES score was measured in five studies including a total of 253 patients: 127 in the LHBT transposition group and 126 in the control group. The results of the heterogeneity analysis indicated that these five studies had good homogeneity (P = 0.27, I2 = 22%). A mean difference of 0.51, 95%CI: -1.91 to 2.93 was calculated, with a P value of 0.68. No significant difference was observed between the two groups regarding the ASES score (Figure 2A).
VAS score was measured in four studies including a total of 231 patients: 115 in the LHBT transposition group and 116 in the control group. The results of the heterogeneity analysis indicated that these four studies had good homogeneity (P = 0.33, I2 = 13%). A mean difference of -0.13 (95%CI: -0.33 to 0.06) was calculated, with a P value of 0.18, indicating that no significant difference was found between the two cohorts (Figure 2B).
UCLA score was measured in three studies including a total of 163 patients: 89 in the LHBT transposition group and 74 in the control group. The results of the heterogeneity analysis indicated that these three studies had good homogeneity (P = 0.19, I2 = 41%). A mean difference of 0.36, 95%CI: -0.67 to 1.39 was calculated, with a P value of 0.50. This suggested that no significant difference was found between the two cohorts (Figure 2C).
ROM was evaluated in five studies including a total of 253 patients: 127 in the LHBT transposition group and 126 in the control group. The results of the heterogeneity analysis in FF and ER0 indicated that these five studies had good homogeneity (P = 0.61, I2 = 0%, P = 0.32, I2 = 14%). In terms of FF, a mean difference of 6.54, 95%CI: 3.07-10.01 was calculated, with a P value of 0.0002, indicating that the FF was significantly better in the LHBT transposition group (Figure 2D). Regarding ER0, a mean difference of 5.15, 95%CI: 1.59-8.17 was calculated, with a P value of 0.005, indicating that the ER0 was significantly better in the LHBT transposition group (Figure 2E).
AHD was measured in four studies including 199 patients: 103 in the LHBT transposition group and 96 in the control group. The results of the heterogeneity analysis indicated that these four studies had good homogeneity (P = 0.13, I2 = 48%). A mean difference of 0.90, 95%CI: 0.21-1.59 was calculated, with a P value of 0.01, indicating that LHBT trans
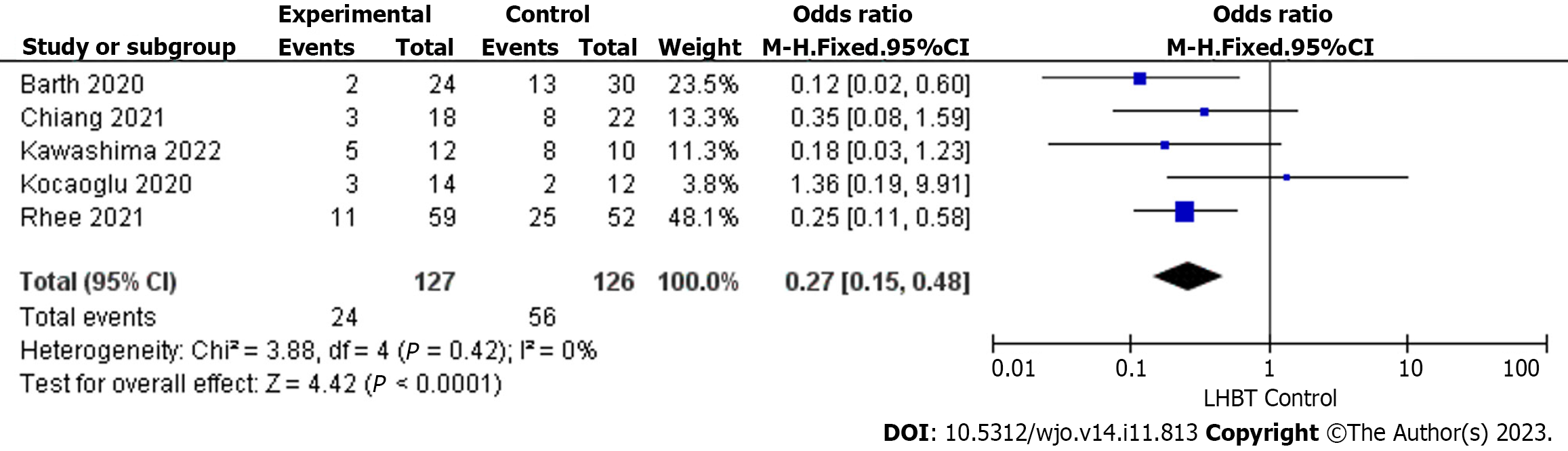
Retear rate was reported in five studies including a total of 253 patients: 127 in the LHBT transposition group and 126 in the control group. The results of the heterogeneity analysis indicated that these five studies had good homogeneity (P = 0.42, I2 = 0%). An odds ratio of 0.27, 95%CI: 0.15-0.48 was measured (P < 0.0001), thereby indicating that the retear rate in LHBT transposition group was lower (Figure 3).
The main finding of this investigation was that LHBT transposition for MIRCTs was generally reported to reduce subacromial contact pressures and prevent superior humeral migration without limiting ROM. On clinical outcomes, compared to other surgical methods for MIRCTs, LHBT transposition resulted in significant improvement in ROM, AHD, and reducing retear rate.
In the included biomechanical study, Park et al[22] reported that SCR with LHBT transposition significantly reduced the humeral head displacement caused by massive rotator cuff tears and decreased subacromial contact pressure. Meanwhile, El-shaar et al[21] found that SCR with LHBT transposition achieved equivalent and potentially even greater biomechanical stability than SCR using a TFL autograft in preventing humeral head migration. Han et al[30] found that SCR for LHBT transposition with or without side-to-side repair both shifted the humeral head downward and was a further reduction in the contact surface area of the acromion. Besides the results of both techniques were comparable in terms of contact pressure and total rotational ROM. A biomechanical study by Han et al[29] found that compared with partial repair after MIRCTs, LHBT transposition with or without side-to-side repair both significantly reduced the humeral head migration distance at 0° and 20° of glenohumeral abduction and effectively reduced the subacromial contact pressure at 0° of glenohumeral abduction. Three different SCR with LHBT transposition techniques were compared in the study of Berthold et al[32]: V-shaped, box-shaped, and single-stranded. Each of the techniques significantly increased maximum abduction angle while significantly decreasing glenohumeral superior translation and maximum cumulative deltoid force compared with the irreparable posterosuperior rotator cuff tear. The V-shaped technique further showed a significantly increased maximum abduction angle and decreased maximum cumulative deltoid force when compared with the box-shaped and single-stranded techniques, as well as a significantly decreased glenohumeral superior translation compared with the box-shaped technique. Meanwhile, Denard et al[31] found that ROM was not impaired with box-shaped and single-limb LHBT transposition and that there was no difference in subacromial contact pressure compared to an intact rotator cuff.
In the meta-analysis of the clinical study, compared to control group, LHBT transposition group improved FF, ER0, and AHD with a lower retear rate. No significant difference in ASES score, VAS score, and UCLA score was demonstrated between these two groups for MIRCTs. Two articles pioneered the treatment of MIRCTs with SCR using autologous broad fascia as the repair material, and the postoperative follow-up found that the patients’ function was significantly improved with satisfactory clinical outcomes[18,38]. However, the autologous broad fascia retrieval requires additional incisions, which not only increases the trauma but also makes the operation complicated and technically demanding. Besides, more anchors are used to fix the broad fascia, which leads to increased costs. Some authors have suggested replacing fascial autografts with human acellular dermal patch allografts to avoid any additional skin incisions and any donor site morbidity[39,40]. A recent study reported by Shin et al[41] showed satisfactory outcomes with SCR using acellular dermal allograft. However, a systematic review showed high retear rate on SCR using acellular dermal allograft compared with fascia lata[42]. The mechanical strength of acellular dermal materials remains controversial and expensive.
SCR with LHBT transposition was proposed by Boutsiadis et al[19] first, and the LHBT without significant tears or severe degeneration was fully utilized in the operation, with the superior glenoid labral is preserved. LHBT was transferred laterally to the supraspinatus tendon footprint area for fixation. Finally, the distal LHBT is chosen to be cut or preserved according to its distal LHBT quality in order to simulate SCR, while the partially repaired rotator cuff can be bridged. The main advantage of this method is to borrow the LHBT to provide a tension-reducing scaffold to strengthen the anterior rotator cuff tissue mechanics and anterosuperior blocking effect to assist the massive rotator cuff repair and reduce the tension on the repaired rotator cuff tissue, thereby reducing the rate of postoperative rotator cuff retears and improving the AHD. This is consistent with the results of our meta-analysis.
Other advantages of SCR with LHBT transposition are that it not only avoids the trauma at the extraction site caused by taking the autologous broad fascia for SCR but also reduces the amount of anchor nails used, thus greatly reducing the cost and time of the procedure and decrease of infection. In addition, it is technically easier and more reproducible than SCR using fascial autografts or dermal allografts, which require a long learning curve. Finally, another possible advantage is the biological aspect of using a local autograft attached to the upper glenoid so that its vasculature may be preserved.
There are several potential limitations of this technique. The main condition is the availability of a relatively good quality LHBT, and SCR with other grafts should be considered when there is LHBT severe degeneration, LHBT rupture or partial tearing involving more than 50%, SLAP lesions > II, and some rare cases of anatomic variation or absence of the tendon[43]. However, in the case of chronic MIRCTs, they are often accompanied by LHBT damage. In addition, the LHBT is reportedly a pain generator in patients with rotator cuff tears, and the use of the LHBT as an autograft for SCR may, in theory, increase postoperative pain[37]. However, the results of clinical studies showed no difference in postoperative pain between the various compared techniques for either tenotomy or rerouting of the LHBT, suggesting that it can be safely used as an autograft[25,37].
This study had several limitations. First, the available studies or data about LHBT transposition used for MIRCTs were limited, only five studies with 127 patients in LHBT transposition group and 126 patients in control group. Second, there was insufficient high-quality comparative evidence, as the five included studies were all retrospective studies with a level of evidence 3, which may create recall or selection bias. Although the MINORS scores of these studies indicate good or fair quality evidence, they still fall short of rigorous randomized controlled trial studies. Third, the surgical approaches in the control group, although all of them are commonly used to treat MIRCTs, may have influenced the comparison of outcomes. Additional comparative trials, or even randomized controlled trials, are necessary in the future to determine which treatments are more advantageous in treating MIRCTs, and which modifications of the technique provide better outcomes. Moreover, prior investigations have revealed that distinct rehabilitation modalities and durations exhibit diverse prognostic implications for individuals undergoing arthroscopic repair of rotator cuff tears[44]. In this regard, forthcoming studies could potentially prioritize the evaluation of the influence of diverse rehabilitation approaches on the utilization of LHBT transposition as a therapeutic intervention for the management of MIRCTs. In addition, high-quality studies are necessary to evaluate the long-term outcomes of SCR with LHBT transposition, including postoperative pain, function and structural integrity. High-resolution ultrasound investigation may play an important role in this regard[45]. In a word, future high-quality research of SCR using LHBT transposition for MIRCTs is necessary.
This systematic review and meta-analysis demonstrated that SCR with LHBT transposition was a reliable and economical technique for treating MIRCTs, both in terms of biomechanical and clinical outcomes, with comparable clinical outcomes, improved ROM, AHD and reduced the retear rates compared to conventional SCR and other established techniques. To further evaluate the long-term effects of SCR with LHBT transposition, more high-quality randomized controlled studies are needed.
Supracapsular reconstruction (SCR) combined with transposition of the biceps long head biceps tendon (LHBT) is an approach designed to meet the severe challenges posed by massive rotator cuff tears (MIRCT).
Although LHBT transposition has been adopted, its exact impact remains to be clearly elucidated.
There are gaps in our knowledge of the outcomes produced by this technique, and thus further research is needed to reveal its potential benefits and limitations.
We conducted a methodical search of electronic databases to identify relevant literature based on inclusion and exclusion criteria. We first conducted a systematic review of the main findings and conclusions of the biomechanical studies. Subsequently, we conducted a comprehensive meta-analysis of the clinical outcomes of the included studies.
Biomechanical studies have reported that after performing LHBT transposition in MIRCT, there was a comprehensive improvement in subacromial contact pressure and a prevention of proximal humeral migration, without any resultant limitation in range of motion. The meta-analysis of LHBT transposition outcomes has encompassed five clinical studies demonstrated that, compared to other surgical methods for MIRCTs, LHBT transposition exhibited significant advantages in enhancing patients’ ROM (forward flexion, mean difference [MD] = 6.54, 95% confidence interval [CI]: 3.00-8.08, external rotation [MD = 5.15, 95%CI: 1.59-8.17], acromiohumeral distance [AHD] [MD = 0.90, 95%CI: 0.21 to 1.59], and reducing the risk of retear [odds ratio = 0.27, 95%CI: 0.15-0.48]). There were no discernible differences between the two groups of patients in terms of American Shoulder and Elbow Surgeons scores, visual analogue scale scores, and University of California, Los Angeles scores.
In summary, the utilization of LHBT transposition in SCR proved to be a dependable and cost-effective approach for addressing MIRCTs. This technique demonstrated favorable results not only in terms of biomechanical factors but also in clinical outcomes. It exhibited comparable efficacy to conventional SCR and other established techniques, while presenting notable improvements in ROM, AHD, and a reduced incidence of retear. Nevertheless, it is essential to emphasize the necessity for additional high-quality randomized controlled trials focusing on the long-term effects of SCR with LHBT transposition to further evaluate its efficacy.
Future high-quality research of SCR using LHBT transposition for MIRCTs is necessary.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chang KV, Taiwan; Vyshka G, Albania S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Zhang XD
| 1. | Catapano M, de Sa D, Ekhtiari S, Lin A, Bedi A, Lesniak BP. Arthroscopic Superior Capsular Reconstruction for Massive, Irreparable Rotator Cuff Tears: A Systematic Review of Modern Literature. Arthroscopy. 2019;35:1243-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 61] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 2. | Rashid MS, Cooper C, Cook J, Cooper D, Dakin SG, Snelling S, Carr AJ. Increasing age and tear size reduce rotator cuff repair healing rate at 1 year. Acta Orthop. 2017;88:606-611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 121] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 3. | Sun Y, Lin J, Luo Z, Chen J. Preoperative Lymphocyte to Monocyte Ratio Can Be a Prognostic Factor in Arthroscopic Repair of Small to Large Rotator Cuff Tears. Am J Sports Med. 2020;48:3042-3050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Rugg CM, Gallo RA, Craig EV, Feeley BT. The pathogenesis and management of cuff tear arthropathy. J Shoulder Elbow Surg. 2018;27:2271-2283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Huang H, Xu F, Feng X, Luo Z, Wang Q. Comparative outcomes of extracorporeal shockwave therapy for shoulder tendinitis or partial tears of the rotator cuff in athletes and non-athletes. Int J Surg. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 6. | Aumiller WD, Kleuser TM. Diagnosis and treatment of cuff tear arthropathy. JAAPA. 2015;28:33-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Jeon YS, Lee J, Kim RG, Ko YW, Shin SJ. Does Additional Biceps Augmentation Improve Rotator Cuff Healing and Clinical Outcomes in Anterior L-Shaped Rotator Cuff Tears? Clinical Comparisons With Arthroscopic Partial Repair. Am J Sports Med. 2017;45:2982-2988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Noyes MP, Haidamous G, Spittle NE, Hartzler RU, Denard PJ. Surgical Management of Massive Irreparable Cuff Tears: Superior Capsular Reconstruction. Curr Rev Musculoskelet Med. 2020;13:717-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Luo Z, Lin J, Sun Y, Zhu K, Wang C, Chen J. Outcome Comparison of Latissimus Dorsi Transfer and Pectoralis Major Transfer for Irreparable Subscapularis Tendon Tear: A Systematic Review. Am J Sports Med. 2022;50:2032-2041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 10. | Park SR, Sun DH, Kim J, Lee HJ, Kim JB, Kim YS. Is augmentation with the long head of the biceps tendon helpful in arthroscopic treatment of irreparable rotator cuff tears? J Shoulder Elbow Surg. 2018;27:1969-1977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | Thorsness R, Romeo A. Massive Rotator Cuff Tears: Trends in Surgical Management. Orthopedics. 2016;39:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 60] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Veen EJD, Stevens M, Diercks RL. Biceps Autograft Augmentation for Rotator Cuff Repair: A Systematic Review. Arthroscopy. 2018;34:1297-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1579] [Cited by in RCA: 1537] [Article Influence: 73.2] [Reference Citation Analysis (0)] |
| 14. | Berth A, Neumann W, Awiszus F, Pap G. Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol. 2010;11:13-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 156] [Article Influence: 10.4] [Reference Citation Analysis (5)] |
| 15. | Mori D, Kizaki K, Funakoshi N, Yamashita F, Mizuno Y, Shirai T, Kobayashi M. Irreparable Large to Massive Rotator Cuff Tears With Low-Grade Fatty Degeneration of the Infraspinatus Tendon: Minimum 7-Year Follow-up of Fascia Autograft Patch Procedure and Partial Repair. Am J Sports Med. 2021;49:3656-3668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Lewington MR, Ferguson DP, Smith TD, Burks R, Coady C, Wong IH. Graft Utilization in the Bridging Reconstruction of Irreparable Rotator Cuff Tears: A Systematic Review. Am J Sports Med. 2017;45:3149-3157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 82] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 17. | Mulieri P, Dunning P, Klein S, Pupello D, Frankle M. Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am. 2010;92:2544-2556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 360] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 18. | Mihata T, Lee TQ, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Kinoshita M. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 551] [Cited by in RCA: 613] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 19. | Boutsiadis A, Chen S, Jiang C, Lenoir H, Delsol P, Barth J. Long Head of the Biceps as a Suitable Available Local Tissue Autograft for Superior Capsular Reconstruction: "The Chinese Way". Arthrosc Tech. 2017;6:e1559-e1566. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 20. | Denard PJ, Park MC, McGarry MH, Adamson G, Lee TQ. Biomechanical Assessment of a V-Shaped Semitendinosus Allograft Anterior Cable Reconstruction for Irreparable Rotator Cuff Tears. Arthroscopy. 2022;38:719-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 21. | El-Shaar R, Soin S, Nicandri G, Maloney M, Voloshin I. Superior Capsular Reconstruction With a Long Head of the Biceps Tendon Autograft: A Cadaveric Study. Orthop J Sports Med. 2018;6:2325967118785365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 22. | Park MC, Itami Y, Lin CC, Kantor A, McGarry MH, Park CJ, Lee TQ. Anterior Cable Reconstruction Using the Proximal Biceps Tendon for Large Rotator Cuff Defects Limits Superior Migration and Subacromial Contact Without Inhibiting Range of Motion: A Biomechanical Analysis. Arthroscopy. 2018;34:2590-2600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 23. | Kim JH, Lee HJ, Park TY, Lee JU, Kim YS. Preliminary outcomes of arthroscopic biceps rerouting for the treatment of large to massive rotator cuff tears. J Shoulder Elbow Surg. 2021;30:1384-1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 24. | Jeong JH, Yoon EJ, Kim BS, Ji JH. Biceps-incorporating rotator cuff repair with footprint medialization in large-to-massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2022;30:2113-2122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 25. | Chillemi C, Mantovani M, Gigante A. Superior capsular reconstruction of the shoulder: the ABC (Arthroscopic Biceps Chillemi) technique. Eur J Orthop Surg Traumatol. 2018;28:1215-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 26. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18665] [Cited by in RCA: 17498] [Article Influence: 1093.6] [Reference Citation Analysis (1)] |
| 27. | Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3743] [Cited by in RCA: 5611] [Article Influence: 255.0] [Reference Citation Analysis (0)] |
| 28. | Park MC, Detoc E, Lee TQ. Anterior Cable Reconstruction: Prioritize Rotator Cable and Tendon Cord When Considering Superior Capsular Reconstruction. Arthroscopy. 2022;38:1705-1713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | Han SY, Lee TQ, Wright DJ, Park IJ, Mauro M, McGarry MH, Lee HJ, Kim YS. Effect of biceps rerouting technique to restore glenohumeral joint stability for large irreparable rotator cuff tears: a cadaveric biomechanical study. J Shoulder Elbow Surg. 2020;29:1425-1434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 30. | Han F, Kong CH, Hasan MY, Ramruttun AK, Kumar VP. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: A biomechanical study on cadavers. Orthop Traumatol Surg Res. 2019;105:257-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 31. | Denard PJ, Chae S, Chalmers C, Choi JH, McGarry MH, Adamson G, Park M, Lee TQ. Biceps Box Configuration for Superior Capsule Reconstruction of the Glenohumeral Joint Decreases Superior Translation but Not to Native Levels in a Biomechanical Study. Arthrosc Sports Med Rehabil. 2021;3:e343-e350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 32. | Berthold DP, Muench LN, Dyrna F, Scheiderer B, Obopilwe E, Cote MP, Krifter MR, Milano G, Bell R, Voss A, Imhoff AB, Mazzocca AD, Beitzel K. Comparison of Different Fixation Techniques of the Long Head of the Biceps Tendon in Superior Capsule Reconstruction for Irreparable Posterosuperior Rotator Cuff Tears: A Dynamic Biomechanical Evaluation. Am J Sports Med. 2021;49:305-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 33. | Rhee SM, Youn SM, Park JH, Rhee YG. Biceps Rerouting for Semirigid Large-to-Massive Rotator Cuff Tears. Arthroscopy. 2021;37:2769-2779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 34. | Kocaoglu B, Firatli G, Ulku TK. Partial Rotator Cuff Repair With Superior Capsular Reconstruction Using the Biceps Tendon Is as Effective as Superior Capsular Reconstruction Using a Tensor Fasciae Latae Autograft in the Treatment of Irreparable Massive Rotator Cuff Tears. Orthop J Sports Med. 2020;8:2325967120922526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 35. | Kawashima K, Terabayashi N, Asano H, Akiyama H. Arthroscopic Long Head of the Biceps Transposition for Superior Capsular Augmentation Results in Comparable Clinical Outcomes to Arthroscopic Partial Repair for Irreparable Rotator Cuff Tears. Arthrosc Sports Med Rehabil. 2022;4:e425-e434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 36. | Chiang CH, Shaw L, Chih WH, Yeh ML, Ting HH, Lin CH, Chen CP, Su WR. Modified Superior Capsule Reconstruction Using the Long Head of the Biceps Tendon as Reinforcement to Rotator Cuff Repair Lowers Retear Rate in Large to Massive Reparable Rotator Cuff Tears. Arthroscopy. 2021;37:2420-2431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 37. | Barth J, Olmos MI, Swan J, Barthelemy R, Delsol P, Boutsiadis A. Superior Capsular Reconstruction With the Long Head of the Biceps Autograft Prevents Infraspinatus Retear in Massive Posterosuperior Retracted Rotator Cuff Tears. Am J Sports Med. 2020;48:1430-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 38. | Mihata T, Lee TQ, Fukunishi K, Itami Y, Fujisawa Y, Kawakami T, Ohue M, Neo M. Return to Sports and Physical Work After Arthroscopic Superior Capsule Reconstruction Among Patients With Irreparable Rotator Cuff Tears. Am J Sports Med. 2018;46:1077-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 153] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 39. | Hirahara AM, Adams CR. Arthroscopic Superior Capsular Reconstruction for Treatment of Massive Irreparable Rotator Cuff Tears. Arthrosc Tech. 2015;4:e637-e641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 155] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 40. | Petri M, Greenspoon JA, Millett PJ. Arthroscopic Superior Capsule Reconstruction for Irreparable Rotator Cuff Tears. Arthrosc Tech. 2015;4:e751-e755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 96] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 41. | Shin SJ, Lee S, Hwang JY, Lee W, Koh KH. Superior Capsular Reconstruction Using Acellular Dermal Allograft Combined With Remaining Rotator Cuff Augmentation Improved Shoulder Pain and Function at 1 Year After The Surgery. Arthroscopy. 2022;38:1089-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 42. | Abd Elrahman AA, Sobhy MH, Abdelazim H, Omar Haroun HK. Superior Capsular Reconstruction: Fascia Lata Versus Acellular Dermal Allograft: A Systematic Review. Arthrosc Sports Med Rehabil. 2020;2:e389-e397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 43. | Dierickx C, Ceccarelli E, Conti M, Vanlommel J, Castagna A. Variations of the intra-articular portion of the long head of the biceps tendon: a classification of embryologically explained variations. J Shoulder Elbow Surg. 2009;18:556-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 44. | Chang KV, Hung CY, Han DS, Chen WS, Wang TG, Chien KL. Early Versus Delayed Passive Range of Motion Exercise for Arthroscopic Rotator Cuff Repair: A Meta-analysis of Randomized Controlled Trials. Am J Sports Med. 2015;43:1265-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 45. | Chu PC, Chang CH, Lin CP, Wu WT, Chen LR, Chang KV, Özçakar L. The impact of shoulder pathologies on job discontinuation and return to work: a pilot ultrasonographic investigation. Eur J Phys Rehabil Med. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |