Published online Nov 18, 2023. doi: 10.5312/wjo.v14.i11.791
Peer-review started: August 23, 2023
First decision: September 14, 2023
Revised: September 18, 2023
Accepted: October 8, 2023
Article in press: October 8, 2023
Published online: November 18, 2023
Processing time: 84 Days and 9.6 Hours
Supracondylar humerus fractures account for more than 60% of all elbow frac
To determine whether time of surgical intervention and/or surgeon level in
We retrospectively studied 155 pediatric patients presenting with a supracondylar humerus fracture in a level 1 trauma center from January 2006 to December 2019. The data extracted included demographic data, fracture characteristics, surgical data, and follow-up outcomes. The collected data was analyzed and P values of < 0.05 were considered statistically significant.
Of the cohort, 11% of patients had documented post-operative complications, of which the majority occurred in surgeries performed after day time working hours and in fractures requiring open reduction. While the lowest complication rate was found in surgeries performed by pediatric orthopaedic surgeons, this did not reach statistical significance.
In pediatric patients undergoing surgery for supracondylar fractures, we found a higher complication rate when surgeries were not performed during working hours. Surgeon level and training had no significant effect on the risk of post-operative complications.
Core Tip: In our pediatric cohort of surgically treated supracondylar humerus fractures we found a higher complication rate when surgeries were not performed during working hours. Surprisingly, surgeon level and training had no significant effect on the risk of post-operative complications.
- Citation: Albrahim IA, AlOmran AK, Bubshait DA, Tawfeeq Y, Alumran A, Alsayigh J, Abusultan A, Altalib A, Alzaid ZA, Alsubaie SS, Alzahrani MM. Time of surgery and surgeon level in supracondylar humerus fractures in pediatric patients: A retrospective study. World J Orthop 2023; 14(11): 791-799
- URL: https://www.wjgnet.com/2218-5836/full/v14/i11/791.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i11.791
Supracondylar humeral fractures (SCHF) account for 16% of all paediatric fractures and are commonly sustained by children younger than eight years of age[1-4]. These injuries commonly occur after a fall on an outstretched hand irrespective of forearm position[5-7]. The majority of these fractures require closed reduction and pinning, while open reduction is reserved for some complex patterns, delayed presentation or when closed reduction fails[8-10]. When compared to closed reduction and fixation, open reduction carries higher risk of complications, especially infection and loss of elbow range of motion[8,11-13].
Timing of surgical intervention for these injuries is an area of controversy, as proponents for emergent intervention prefer it before any surgical site swelling occurs to minimize complications including nerve injury and compartment syndrome. In addition, it is believed that early surgical management can improve the success of closed reduction in these patient[12]. Surgeons who prefer a more delayed but urgent approach believe that operating on these fractures with an experienced team and during the daytime hours will lead to a quicker and more efficient surgical experience and decrease the associated post-operative complications[14,15].
The purpose of our study was to explore outcomes of surgical management of SCHF in pediatric patients and to assess if timing of surgical intervention and/or surgeon level would influence the outcomes of these patients post-operatively.
This is a retrospective cohort study conducted in a level 1 trauma center from January 2006 to December 2019. After ethical approval was obtained from the institutional review board in our institute (IRB-UGS-2019-01-333), all pediatric patients 1 to 14 years old who sustained a SCHF and were treated surgically with a follow up period of at least 24 mo were included. Exclusion criteria were patients who were lost to follow up, had incomplete data points in their charts or had inadequate radiographs. In addition, Gartland type I fractures were excluded as these all were managed non-surgically in our institution.
All surgeries were performed by pediatric orthopaedic trained consultants, board certified orthopaedic consultants, fellows, or residents (with consultant supervision). Cases were booked in the dedicated emergency room by the admitting consultant and surgery is performed according to urgency level decided by the admitting consultant. Cases admitted after day time working hours by non-pediatric orthopaedic consultants are repatriated to a pediatric orthopaedic consultant the next morning if not done. Operative fixation was performed under general anaesthesia, with the patients in supine position. The operative extremity was prepped and draped in standard fashion and pre-operative weight appropriate prophylactic antibiotics were administered. A trial of closed reduction was performed and if adequate percutaneous fixation with k-wires was performed (configuration and number were left to surgeon discretion). If closed reduction was unsuccessful, an open reduction was performed. After fixation, a sterile dressing was applied to the pin sites and an above elbow back-slap was applied in neutral position. Patients were followed up in clinic at 2 wk post-operatively, then at the 6-week post-operative mark where pins were removed, and patients were allowed to start range of motion of the elbow. Patients were then seen at 3-, 6- and 12-mo post-surgery.
Data was extracted from the hospital electronic medical records, which included patient demographics data (age and gender), in addition to fracture characteristics and outcome variables. The collected variables included Gartland classification, time of surgery (during working hours “08:00-15:00” vs after day time working hours “15:00-8:00”), surgeon level (trainees “fellows or residents under supervision”, non-pediatric orthopedic surgeons, and pediatric orthopedic surgeons), nerve or vessel injury (both pre- and post-operative), associated complications (including compartment syndrome and pin site infection) and fixation construct. Post-operative radiographic alignment was assessed on plain antero-posterior and lateral elbow radiographs. Inadequate reduction was defined according to Flynn’s criteria (Baumann angle < 10˚, displacement > 4 mm and anterior humeral line not bisecting the capitellum)[16].
A power analysis was performed with data from Saarinen et al[17], using a power of 80% and α = 0.05, we estimated that we would require a sample size of 59 patients. Data was analyzed using Statistical Package for Social Sciences version 27 (IBM Corp, 2017). Categorical variables were described as frequencies and percentages, while continuous variables were described as mean and standard deviation. Bivariate analysis was tested using Chi-square test and ANOVA were applicable, with a P value of less than 0.05 considered as significant. Odds ratios with 95% confidence intervals were calculated to examine the association between the outcome variables and patient or fracture factors.
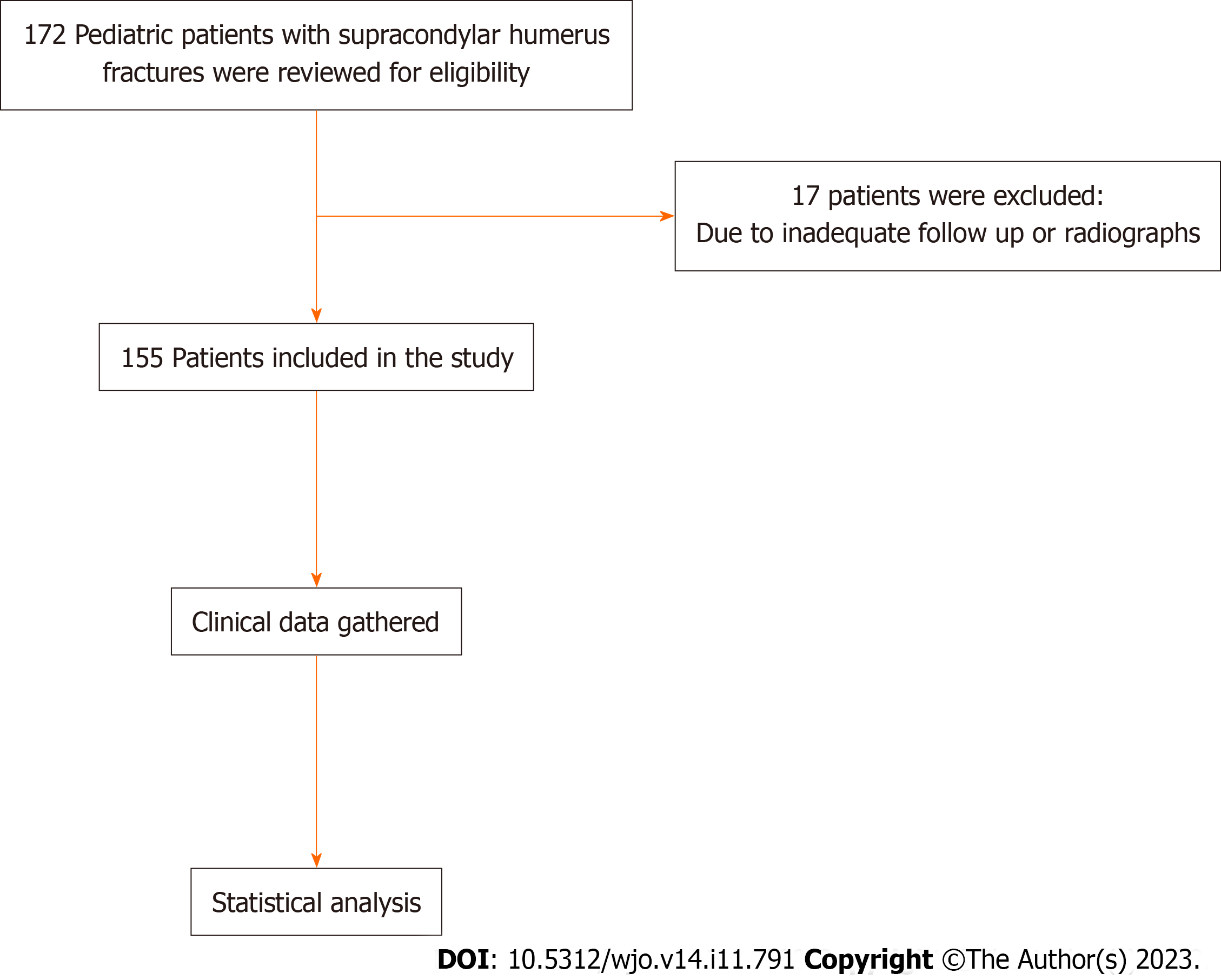
A total of 172 patients were reviewed and 155 were included in the study with a mean age of 5.36 years old (range 1-13 years old) (Figure 1). More than half of the patients were males 105 (67.7%). Of the patients included in the cohort, 2.6% had a documented nerve injury pre-operatively (half of which were managed during working hours), these injuries included two cases of median and two cases of radial nerve palsies. An absent radial pulse was found in 9% of patients (half of which were also managed during working hours), all patients regained pulses after manual reduction during the operative procedure (Table 1). More than half of patients (56.1%) were managed during working hours, while 43.9% were managed after day time working hours. The majority of fractures were managed by closed reduction and k-wire fixation (84.5%) and parallel K-wires were the most applied construct (48.4%) (Table 1).
| Variables, n (%) | ||
| Time of surgery | During working hours | 87 (56.1) |
| After working hours | 68 (43.9) | |
| Surgeon level | Pediatric orthopedic consultant | 44 (28.4) |
| Non-pediatric orthopedic consultant | 38 (24.5) | |
| Trainee | 73 (47.1) | |
| Gender | Male | 105 (67.7) |
| Female | 50 (32.3) | |
| Mechanism | Fall on outstretched hand | 112 (72.3) |
| Fall on flexed elbow | 17 (11) | |
| Direct | 15 (9.7) | |
| Motor vehicle accident | 8 (5.2) | |
| Others | 3 (1.9) | |
| Pre-operative nerve injury | Yes | 4 (2.6) |
| No | 151 (97.4) | |
| Pulse | Intact | 141 (91) |
| Absent | 14 (9) | |
| Classification | Gartland type 2 | 32 (20.6) |
| Gartland type 3 | 115 (74.2) | |
| Flexion type | 8 (5.2) | |
| Procedure | Open reduction | 24 (15.5) |
| Close reduction | 131 (84.5) | |
| K-wire arrangement | Parallel | 75 (48.4) |
| Medial & lateral | 35 (22.6) | |
| Two lateral & one medial | 34 (21.9) | |
| Others | 11 (7.1) | |
Twenty-four cases (15.5%) required an open reduction, 3 of which had an absent pulse pre-operatively which was regained after fracture reduction. More than half of the open reduction cases were performed by trainees with consultant supervision (58.3%), while 20.8% were performed by pediatric orthopaedic surgeons and 20.8% performed by non-pediatric orthopaedic surgeons.
Of the cohort, 17 patients (11%) had documented post-operative complications. These complications included four cases of nerve palsy post-operatively, three of which were fixed with two lateral and one medial k-wires (two had a median nerve injury and one ulnar nerve injury) and one fixed with two lateral parallel k-wires (sustained a median nerve injury). The remaining complications were 12 cases of unacceptable angular deformity post-fixation and one case of bony spur requiring operative management. Patients who were managed after day time working hours were associated with more complications when compared with daytime surgeries (5.7% vs 17.6%, P value < 0.05). Patients who had their surgeries done after day time working hours were nearly at a 3 times higher risk of developing complications (OR = 2.8, P value < 0.05) when compared to surgeries done during the daytime.
In addition, patient who required an open reduction had a higher rate of complications (33.3%) when compared to closed reduction (6.9%, P value < 0.001) (Table 2). Complications recorded with open reduction were 5 cases of angular deformity, one case of ulnar nerve palsy and one case of boney spur. The odds of a complication occurring was more than 6 times greater with an open reduction when compared to a closed reduction (OR = 6.8, P value < 0.005). We found no difference in rate of complication between Gartland type 2, type 3 and flexion type SCHFs.
| Variables | Complication, n (%), n = 155 | |||
| Yes, n = 16 (10.3) | No, n = 139 (89.7) | P value | ||
| Time of surgery | During working hours | 5 (5.7) | 82 (94.3) | 0.019 |
| After working hours | 12 (17.6) | 56 (82.4) | ||
| Surgeon level | Pediatric orthopaedic consultant | 4 (9.1) | 40 (90.9) | 0.841 |
| Non-pediatric orthopaedic consultant | 5 (13.2) | 33 (86.8) | ||
| Trainee | 8 (11) | 65 (89) | ||
| Gender | Male | 10 (9.5) | 95 (90.5) | 0.404 |
| Female | 7 (14) | 43 (86) | ||
| Classification | Gartland type 2 | 2 (6.3) | 30 (93.7) | 0.308 |
| Gartland type 3 | 13 (11.3) | 102 (88.7) | ||
| Flexion type | 2 (25) | 6 (75) | ||
| Procedure | Open reduction | 8 (33.3) | 16 (66.7) | 0.001 |
| Close reduction | 9 (6.9) | 122 (93.1) | ||
| K-wire arrangement | Parallel | 6 (8) | 69 (92) | 0.154 |
| Medial & lateral | 4 (11.4) | 31 (88.6) | ||
| Two lateral & one medial | 7 (20.6) | 27 (79.4) | ||
| Others | 0 (0) | 11 (100) | ||
Interestingly, although the lowest rate of complications was in surgeries performed by pediatric orthopaedic surgeons, this was not statistically significant (Table 2). There was no significant difference in Gartland classification, K-wire arrangement, pre-operative nerve injury and absent pulse between cases done by different levels of surgeons. Concerning timing of surgery and the surgeon performing the surgery, the majority (57.4%) of after day time working hours surgeries were performed by trainees, while only 25% were performed by non-pediatric orthopaedic surgeons and 17.6% by pediatric orthopaedic surgeons (P value < 0.05).
We also assessed the effect of surgeon level on complication rate in surgeries performed during working hours and surgeries performed after day time working hours, separately, and found no statistically significant difference.
The aim of this study was to investigate and analyze factors that could have an influence on outcomes of SCHF in pediatric patients, including time of surgery and surgeon level. In our cohort, we found that majority of complications occurred in cases performed after day time working hours, this may be attributed to that more severe injuries or cases with associated neurovascular compromise may be taken more urgently during the night. Aydoğmuş et al[18] reported inferior fixation of 91 pediatric patients with operatively managed SCHF during after-hours when compared to cases performed during the daytime. In their cohort, they found no difference operative time, requirement of open reduction nor patient outcomes. When comparing early (< 12 h) and delayed (> 12 h) surgical fixation of pediatric SCHF, Suganuma et al[19] and Gupta et al[20] found no difference in rate of open reduction, post-operative complications nor surgical time between the two groups. In addition, Mehlman et al[15] found no difference in rate of open reduction, pin tract infection nor iatrogenic nerve injury between pediatric SCHF performed within 8 h of injury and more than 8 h of injury. Multiple other studies explored differences in outcomes and complication rates when surgery is done early or in a delayed fashion for SCHF, with the majority finding no statistically significant differences (Table 3).
| Ref. | Sample size | Groups | Results |
| Suganuma et al[19], 2020 | 120 Gartland type II and III SCHF | Surgeries within 12 h of injury and > 12 h | No difference in: Operative time; Early complications; Post-operative radiographic parameters |
| Aydoğmuş et al[18], 2017 | 91 Gartland type III SCHF | Daytime vs after hours surgery | Poor fixation rate in after hour surgery; No difference in operative time or residual deformity |
| Schmid et al[25], 2015 | 343 Gartland type II and III SCHF | Surgeries within 6 h, 6-12 h, 12-24 h and > 24 h from injury | No difference in: Outcome; Complications; Requiring open reduction |
| Mayne et al[26], 2014 | 115 Gartland type II and III SCHF | Surgeries within 12 h of injury and > 12 h | No difference in: Infection rate; Iatrogenic nerve injury; Requiring open reduction |
| Larson et al[27], 2014 | 399 Gartland type II SCHF | Surgeries within 24 h of injury and > 24 h | No difference in complication rate |
| Yildirim et al[28], 2009 | 190 Gartland type III SCHF | Time from injury to surgery | 4 fold increase in requiring open reduction for each 5 hour delay |
| Walmsley et al[29], 2006 | 171 Gartland type III SCHF | Surgeries within 8 h of injury and > 8 h | No difference in complication rate; Higher risk of requiring open reduction in > 8 h group |
| Sibinski et al[30], 2006 | 77 Gartland type III SCHF | Surgeries within 12 h of injury and > 12 h | No difference in: Operative time; Outcome; Risk of open reduction |
| Gupta et al[20], 2004 | 150 operatively treated SCHF | Surgeries within 12 h of injury and > 12 h | No difference in: Pin tract infection; Iatrogenic nerve injury |
| Mehlman et al[15], 2001 | 198 operatively treated SCHF | Surgeries within 8 h of injury and > 8 h | No difference in: Pin tract infection; Iatrogenic nerve injury |
| Iyengar et al[31], 1999 | 58 Gartland type III SCHF | Surgeries within 8 h of injury and > 8 h | No difference in: Open reduction rate; Clinical outcomes |
Considering the higher complication rate in after day time working hours surgery and the lack of increased risk of adverse events in delayed fixation of SCHF, it seems clear that unless the extremity is pulseless with lack of perfusion, the fracture is open or there are signs of compartment syndrome, SCHF in pediatric patients should preferably be done during a reasonable time of day and not late after day time working hours.
While the majority of the complications in our cohort were in the surgeries that were conducted by trainees and non-pediatric orthopaedic surgeons, this was not statistically significant. When exploring the literature, we find that this is an area of controversy, as several studies have shown that the level and training of the surgeon has a significant effect on both outcome and complication rate of pediatric SCHF (Table 4). In addition, studies have also shown that when the procedure is supervised by a pediatric orthopedic surgeon, the outcomes are excellent with very low complication and revision rates irrespective of the level of the surgeon performing the surgery[21,22]. On the other hand, several studies have shown no difference in complication rate and risk of malreduction when the surgery is performed by a trained orthopaedic surgeon without pediatric fellowship training[17,23,24].
| Ref. | Sample size | Groups | Results |
| Fisher et al[23], 2021 | 231 patients who underwent CRPP for SCHF | Pediatric orthopaedic fellowship trained vs other orthopaedic surgeons | Shorter operative and fluoroscopy time; No difference in complications |
| Osateerakun et al[32], 2019 | 87 Gartland type II and III SCHF | Pediatric orthopaedic fellowship trained vs other orthopaedic surgeons | Higher risk of complications in Gartland type III when not performed by pediatric orthopaedic surgeon; Overall complication rate and acceptable alignment were similar |
| Saarinen et al[17], 2019 | 108 operatively treated SCHF | Residents, pediatric surgeons and orthopaedic surgeons | Orthopaedic surgeons had the least complications and inadequate reductions; Residents had less complications and inadequate reductions when compared to pediatric surgeons |
| Pesenti et al[33], 2018 | 236 Gartland type III SCHF | Surgeons with < 1 yr vs > 1 yr experience | Less experienced had longer operative time; No difference in complication and malalignment rate |
| Tuomilehto et al[34], 2018 | 210 operatively treated SCHF | Consultants vs registrars | Higher complications and poorer outcomes in surgeries done by registrars |
| Liu et al[22], 2011 | 654 operatively treated SCHF | Fellows progression through fellowship training | No difference in complications and malunions throughout the fellowship year; Spike of malreductions at case 7 which improves at case 15 |
| Padman et al[21], 2010 | 71 Gartland type II and III SCHF | Consultants vs trainees | Poorer outcome and more complications in surgeries performed by trainees without consultant supervision |
| Farley et al[24], 2008 | 444 operatively treated SCHF | Pediatric orthopaedic surgeon vs non-pediatric orthopaedic surgeon | No difference in complication rate and outcomes |
Limitations of the study include that it is a retrospective cohort, but we believe that we were successful in data collection from the patients’ medical records with good accuracy. Another possible limitation is the small sample size, but we believe that our study is adequately powered based on the sample size analysis using previous published studies. In addition, the number of complications in our study was relatively low, but the proportion of complications was similar in previously published studies.
In pediatric patients undergoing surgery for SCHF, we found a higher complication rate when surgeries were not performed during working hours, or when an open reduction is required. Although pediatric orthopaedic surgeons had the lowest rate of complications, this difference did not reach statistical significance. We believe the data presented in this study can help in reaching a better-informed decision about the timing of surgery for pediatric patients with SCHF.
Pediatric supracondylar humerus fractures can be associated with risk of complications including neurovascular injuries, malunions and limb deformities. Surgical timing and level of surgeon performing the surgery may have an effect on outcome of these fractures.
Explore the effect of time of surgery and level of surgeon on pediatric supracondylar humerus fractures.
The objective of this study was to determine whether time of surgical intervention and/or surgeon level influence the outcomes of surgically managed pediatric supracondylar humerus fractures.
We retrospectively studied 155 pediatric patients presenting with a supracondylar humerus fracture in a level 1 trauma center from January 2006 to December 2019. The data extracted included demographic data, fracture characteristics, surgical data, and follow-up outcomes. The collected data was analyzed and P values of < 0.05 were considered statistically significant.
Of the cohort, 11% patients had documented post-operative complications, of which the majority occurred in surgeries performed after day time working hours and in fractures requiring open reduction. While the lowest complication rate was found in surgeries performed by pediatric orthopaedic surgeons, this did not reach statistical significance.
In pediatric patients undergoing surgery for supracondylar fractures, we found a higher complication rate when surgeries were not performed during working hours. Surgeon level and training had no significant effect on the risk of post-operative complications.
We believe the data presented in this study can help in reaching a better-informed decision about the timing of surgery for pediatric patients with supracondylar humeral fractures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Zhang Y, China S-Editor: Liu JH L-Editor: A P-Editor: Xu ZH
| 1. | Cheng JC, Ng BK, Ying SY, Lam PK. A 10-year study of the changes in the pattern and treatment of 6,493 fractures. J Pediatr Orthop. 1999;19:344-350. [PubMed] [DOI] [Full Text] |
| 2. | Soldado F, Hodgson F, Barrera-Ochoa S, Diaz-Gallardo P, Garcia-Martinez MC, Ramirez-Carrasco TR, Domenech-Fernandez P, Knorr J. Gartland Type-IV Supracondylar Humeral Fractures: Preoperative Radiographic Features and a Hypothesis on Causation. Orthop Traumatol Surg Res. 2022;108:103049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 3. | Mangwani J, Nadarajah R, Paterson JM. Supracondylar humeral fractures in children: ten years' experience in a teaching hospital. J Bone Joint Surg Br. 2006;88:362-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Khoshbin A, Leroux T, Wasserstein D, Wolfstadt J, Law PW, Mahomed N, Wright JG. The epidemiology of paediatric supracondylar fracture fixation: a population-based study. Injury. 2014;45:701-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Otsuka NY, Kasser JR. Supracondylar Fractures of the Humerus in Children. J Am Acad Orthop Surg. 1997;5:19-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 201] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 6. | Cheng JC, Lam TP, Maffulli N. Epidemiological features of supracondylar fractures of the humerus in Chinese children. J Pediatr Orthop. 2001;10:63-7. [PubMed] [DOI] [Full Text] |
| 7. | Runtz A, Nallet J, Font V, Anriot M, Pechin C, Langlais J, de Billy B. Trampoline injuries in children: A prospective study. Orthop Traumatol Surg Res. 2022;108:103289. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Kzlay YO, Aktekin CN, Özsoy MH, Akşahin E, Sakaoğullar A, Pepe M, Kocadal O. Gartland Type 3 Supracondylar Humeral Fractures in Children: Which Open Reduction Approach Should Be Used After Failed Closed Reduction? J Orthop Trauma. 2017;31:e18-e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Thomas J, Rosello O, Oborocianu I, Solla F, Clement JL, Rampal V. Can Gartland II and III supracondylar humerus fractures be treated using Blount's method in the emergency room? Orthop Traumatol Surg Res. 2018;104:1079-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Abzug JM, Herman MJ. Management of supracondylar humerus fractures in children: current concepts. J Am Acad Orthop Surg. 2012;20:69-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Tomori Y, Nanno M, Takai S. Clinical results of closed versus mini-open reduction with percutaneous pinning for supracondylar fractures of the humerus in children: A retrospective case-control study. Medicine (Baltimore). 2018;97:e13162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Paci GM, Tileston KR, Vorhies JS, Bishop JA. Pediatric Supracondylar Humerus Fractures: Does After-Hours Treatment Influence Outcomes? J Orthop Trauma. 2018;32:e215-e220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Raux S, Madelaine A. Sequelae of childhood elbow fracture. Orthop Traumatol Surg Res. 2023;109:103454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 14. | Kwiatkowska M, Dhinsa BS, Mahapatra AN. Does the surgery time affect the final outcome of type III supracondylar humeral fractures? J Clin Orthop Trauma. 2018;9:S112-S115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Mehlman CT, Strub WM, Roy DR, Wall EJ, Crawford AH. The effect of surgical timing on the perioperative complications of treatment of supracondylar humeral fractures in children. J Bone Joint Surg Am. 2001;83:323-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 162] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 16. | Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years' experience with long-term follow-up. J Bone Joint Surg Am. 1974;56:263-72.. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 423] [Cited by in RCA: 364] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Saarinen AJ, Helenius I. Paediatric supracondylar humeral fractures: the effect of the surgical specialty on the outcomes. J Child Orthop. 2019;13:40-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Aydoğmuş S, Duymuş TM, Keçeci T, Adiyeke L, Kafadar AB. Comparison of daytime and after-hours surgical treatment of supracondylar humeral fractures in children. J Pediatr Orthop B. 2017;26:400-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Suganuma S, Tada K, Yasutake H, Horii T, Takata M, Shimanuki K, Tsuji D, Takagawa S, Asano Y, Tsuchiya H. Timing of Surgery for Pediatric Supracondylar Humerus Fractures and Early Postoperative Results. J Hand Surg Asian Pac Vol. 2020;25:226-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Gupta N, Kay RM, Leitch K, Femino JD, Tolo VT, Skaggs DL. Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J Pediatr Orthop. 2004;24:245-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 35] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Padman M, Warwick AM, Fernandes JA, Flowers MJ, Davies AG, Bell MJ. Closed reduction and stabilization of supracondylar fractures of the humerus in children: the crucial factor of surgical experience. J Pediatr Orthop B. 2010;19:298-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Liu RW, Roocroft J, Bastrom T, Yaszay B. Surgeon learning curve for pediatric supracondylar humerus fractures. J Pediatr Orthop. 2011;31:818-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Fisher BT, Chong ACM, Flick T, Forness M, Sauer BR, Peterson JB. Does Surgeon Subspecialty Training Affect Outcomes in the Treatment of Displaced Supracondylar Humerus Fractures in Children? J Am Acad Orthop Surg. 2021;29:e447-e457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Farley FA, Patel P, Craig CL, Blakemore LC, Hensinger RN, Zhang L, Caird MS. Pediatric supracondylar humerus fractures: treatment by type of orthopedic surgeon. J Child Orthop. 2008;2:91-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Schmid T, Joeris A, Slongo T, Ahmad SS, Ziebarth K. Displaced supracondylar humeral fractures: influence of delay of surgery on the incidence of open reduction, complications and outcome. Arch Orthop Trauma Surg. 2015;135:963-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Mayne AI, Perry DC, Bruce CE. Delayed surgery in displaced paediatric supracondylar fractures: a safe approach? Results from a large UK tertiary paediatric trauma centre. Eur J Orthop Surg Traumatol. 2014;24:1107-1110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Larson AN, Garg S, Weller A, Fletcher ND, Schiller JR, Kwon M, Browne R, Copley LA, Ho CA. Operative treatment of type II supracondylar humerus fractures: does time to surgery affect complications? J Pediatr Orthop. 2014;34:382-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Yildirim AO, Unal VS, Oken OF, Gulcek M, Ozsular M, Ucaner A. Timing of surgical treatment for type III supracondylar humerus fractures in pediatric patients. J Child Orthop. 2009;3:265-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Walmsley PJ, Kelly MB, Robb JE, Annan IH, Porter DE. Delay increases the need for open reduction of type-III supracondylar fractures of the humerus. J Bone Joint Surg Br. 2006;88:528-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 80] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 30. | Sibinski M, Sharma H, Bennet GC. Early versus delayed treatment of extension type-3 supracondylar fractures of the humerus in children. J Bone Joint Surg Br. 2006;88:380-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 70] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 31. | Iyengar SR, Hoffinger SA, Townsend DR. Early versus delayed reduction and pinning of type III displaced supracondylar fractures of the humerus in children: a comparative study. J Orthop Trauma. 1999;13:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 98] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 32. | Osateerakun P, Thara I, Limpaphayom N. Surgical treatment of pediatric supracondylar humerus fracture could be safely performed by general orthopedists. Musculoskelet Surg. 2019;103:199-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 33. | Pesenti S, Ecalle A, Peltier E, Choufani E, Blondel B, Jouve JL, Launay F. Experience and volume are determinantive factors for operative management of supracondylar humeral fractures in children. J Shoulder Elbow Surg. 2018;27:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 34. | Tuomilehto N, Sommarhem A, Nietosvaara AY. 9 years' follow-up of 168 pin-fixed supracondylar humerus fractures in children. Acta Orthop. 2018;89:351-356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |