Published online Oct 18, 2023. doi: 10.5312/wjo.v14.i10.733
Peer-review started: August 21, 2023
First decision: September 13, 2023
Revised: September 13, 2023
Accepted: October 8, 2023
Article in press: October 8, 2023
Published online: October 18, 2023
Processing time: 56 Days and 1.3 Hours
Triggering, locking, clicking, and crepitus of the fingers are common symptoms patients present with. Even though crepitus and triggering can occur as part of the same underlying diagnosis, it is important to differentiate between them, as they usually indicate different possible diagnoses. The differential diagnoses that should be considered include trigger finger, metacarpophalangeal joint (MCPJ) arthritis, fractures or dislocations, extensor digitorum communis subluxation or dislocation, locked MCPJ, avascular necrosis of the metacarpal head, and Dupuytren’s disease. A thorough clinical examination with appropriate special investigations can permit the clinician to make the correct diagnosis. Appropriate management of a confirmed diagnosis is successful in providing symptomatic improvement.
Core Tip: Despite trigger fingers being one of the most common causes of hand pain and disability, there are other possible causes of triggering, locking, clicking, and crepitus of the fingers. Failure to recognize and diagnose these other causes can lead to treatment errors and inappropriate management of patients.
- Citation: Jordaan PW, Klumpp R, Zeppieri M. Triggering, clicking, locking and crepitus of the finger: A comprehensive overview. World J Orthop 2023; 14(10): 733-740
- URL: https://www.wjgnet.com/2218-5836/full/v14/i10/733.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i10.733
Trigger fingers are one of the most common causes of pain and disability of the adult hand[1,2]. Even though a trigger finger is commonly associated with locking of the finger in flexion and a painful snapping (clicking) during extension[3,4], a mild trigger finger (Green 1)[5] may present with only pain, swelling and stiffness in the morning[6,7], whereas a severe one (Green 4)[5], may have a locked digit[7], presenting like a flexion contracture[7] which has to be distinguished from a Dupuytren’s contracture.
When associated with severe flexor synovitis, patients with trigger fingers may even have crepitus in the palm[7], but when crepitus is present, a clinician will tend to consider metacarpophalangeal joint (MCPJ) arthritis as a diagnosis. A well-known medical cliché is: “common things occur commonly.” This is important to remember, but at the same time, as clinicians, we have to keep in mind that “not all that glitters is gold.”
In this minireview, we provide a short summary of the broad differential diagnosis for triggering and crepitus of the finger and briefly discuss the clinical presentation, workup, and treatment of these different conditions.
In this modern day and age, many patients, after extensive internet research, will present to their doctor with a diagnosis. The majority of patients will still present with troublesome symptoms, which include the following.
Pain is probably the most common symptom. It is important to differentiate between pain in the mornings (inflammatory) and pain with motion (mechanical). A trigger finger will often be more painful in the mornings or evenings and will also experience pain with extension when triggering. Arthritis will generally cause pain with all motion of the joint and less pain when resting, except in cases of inflammatory arthritis, which can also present with morning and evening pain.
Stiffness is often associated with many conditions affecting the hand. It is important to determine whether there is a fixed decreased range of motion or just temporary stiffness or uneven motion.
Triggering can be reported in some individuals. Most patients will describe it as clicking or locking, depending on the severity of the disease.
Crepitus is a symptom that patients tend not to complain about; however, patients commonly describe it as grinding or they say it feels as though they have sand or gravel around the tendon when they try and move. In the case of a fracture, they may even describe a feeling of cracking.
The history is important as acute onset following trauma would guide the diagnosis more towards a fracture or sagittal band injury.
Several conditions need to be considered in the differential diagnosis of these symptoms. The most common conditions are listed below and reported in Table 1.
| Differential diagnoses |
| Trigger finger |
| Metacarpophalangeal joint arthritis |
| Fractures and dislocations |
| Extensor digitorum communis subluxation/dislocation |
| Locked metacarpophalangeal joint |
| Avascular necrosis of the metacarpal head |
| Dupuytren’s contracture |
Trigger finger remains the most common diagnosis[1]. It is caused by a discrepancy in the size of the flexor tendon and the A1 pulley[8], but in 1% of cases, the triggering can occur at the A2 pulley[5]. There is a bimodal distribution with pediatric trigger fingers presenting before the age of 8 and adult cases presenting in the 5th and 6th decade[1,3]. It is more common in females[3] and tends to affect the ring and middle fingers more commonly[1]. Many conditions are associated with trigger fingers including diabetes, inflammatory conditions, carpal tunnel syndrome, hypothyroidism, gout, storage diseases, De Quervain’s tenosynovitis, and Dupuytren’s contracture[7,8].
Arthritis causes pain, swelling, and a limited range of motion. Rheumatoid and other inflammatory arthritis used to be the most common causes of MCPJ arthritis. With improved medical control, this is seen less than it used to be. Osteoarthritis, posttraumatic arthritis, and crystalline deposition disorders should be included in the differential diagnosis.
This seems like an obvious diagnosis, but can be missed if not considered. There should be a clear trauma history with a painful, swollen, and bruised finger and crepitus and pain with motion. Consider metacarpal head and neck fractures and fractures at the base of the proximal phalanx as well as MCPJ dislocations.
In acute traumatic injury, Boxer’s Knuckle, there is a rupture of the sagittal band (most commonly the radial sagittal band), causing subluxation or dislocation of the extensor digitorum communis (EDC) tendon[10,11]. It can also occur due to attrition as seen in Rheumatoid Arthritis patients or occasionally in osteoarthritis[10]. The middle finger is most affected in a Boxer’s Knuckle[10-12]. The MCPJ is swollen and tender[11] and patients can complain of clicking with crepitus found during examination, which is called pseudo triggering[10]. In mild cases (Rayan and Murray grade 1)[13] the MCPJ is just swollen and tender, but in cases of complete EDC dislocation (Rayan and Murray grade 3)[13] active extension may not be possible[10,11] and can create the impression of a locked MCPJ or even an extensor tendon rupture.
A patient can present with a loss of active and passive MCPJ extension, without affecting interphalangeal joint motion and while maintaining full flexion[14,15]. This is caused by entrapment of the collateral ligament (usually the radial collateral ligament)[15] behind an osteophyte of the metacarpal head in flexion, which prevents extension. In certain cases, the ligament does not get stuck but just causes snapping as it passes over the osteophyte[16]. It can be caused by any condition that causes an abnormal shape of the metacarpal head, such as acromegaly or achondroplasia[15]. Impingement of a torn palmar plate can cause locking of the MCPJ[15,16], but in these cases, flexion can often be limited rather than extension[15].
Avascular necrosis (AVN) of the metacarpal head is very rare. It occurs more commonly in young men and more commonly in the middle finger[17,18]. Patients can present with pain and crepitus, very similar to arthritis, and it is associated with anatomical variations in blood flow, trauma, steroid use, systemic lupus erythematosus (SLE), hypercoagulability, alcoholism or it can be idiopathic[17,18].
Dupuytren’s disease is an idiopathic fibrosis of the palmar aponeurosis leading to contractures of the fingers[19]. It can be associated with trigger fingers, but should also be considered as a differential diagnosis for a locked finger. Even though the diagnosis may seem obvious, some patients can have subtle cords, making it less obvious. It should also be remembered that Dupuytren’s can be associated with trigger fingers and both diagnoses can co-exist on the same finger.
In many cases, the diagnosis can be made through history and clinical examination. In the case of a trigger finger, the patient will present with a typical history of temporary locking of the finger in flexion and painful snapping during extension[4]. Triggering may not be elicited in all cases, but there is generally mild swelling of the finger and tenderness over the A1 pulley[1,3].
In MCPJ arthritis, the patient will complain of pain with motion and a decreased range of motion. On examination, the joint will be swollen and tender, with a decreased range of active and passive motion[9] and a positive grind test. Crepitus may be felt.
Fractures and dislocations around the MCPJ should present with a typical trauma history with a painful swollen and bruised finger and hand. There can be a deformity and any motion will be extremely painful and may even produce crepitus. With a dislocation, the joint may seem locked in a certain position.
EDC subluxation may present with a trauma history[20] in cases of sagittal band rupture, but may also have a spontaneous onset[20] in cases of sagittal band attrition[10]. The MCPJ will generally be swollen and tender dorsally with clicking (pseudo triggering)[10] noted during motion[11]. In Rayan and Murray[13] grade 3 cases, there may be an extensive deficit during active motion, with normal passive extension. During full active MCPJ flexion, the EDC can be observed to sublux/dislocate out of its central position over the MCPJ.
A patient who presents with a locked MCPJ may suggest a trivial traumatic event as a cause of their condition. There may be signs of osteoarthritis of the other small joints in the hand and the MCPJ is often not swollen and non-tender. There will be decreased active and passive extension with normal interphalangeal joint motion and full active flexion of the finger[14,15].
AVN of the metacarpal head is a rare condition[17,18] and a diagnosis of exclusion[18]. There will be pain and possibly crepitus[17,18] and a decreased range of motion in a patient who is younger than would be normally expected to be seen in an arthritic joint. Conditions associated with AVN such as steroid use, alcoholism, SLE, and hypercoagulability[17,18] may be present.
In a patient with Dupuytren’s contracture, there will be a fixed contracture limiting full extension and there should be a visible and palpable cord and possible family history. A careful examination is mandatory as some patients can have very subtle cords and be aware that there may be a co-existing grade 1 trigger finger with a tender A1 pulley.
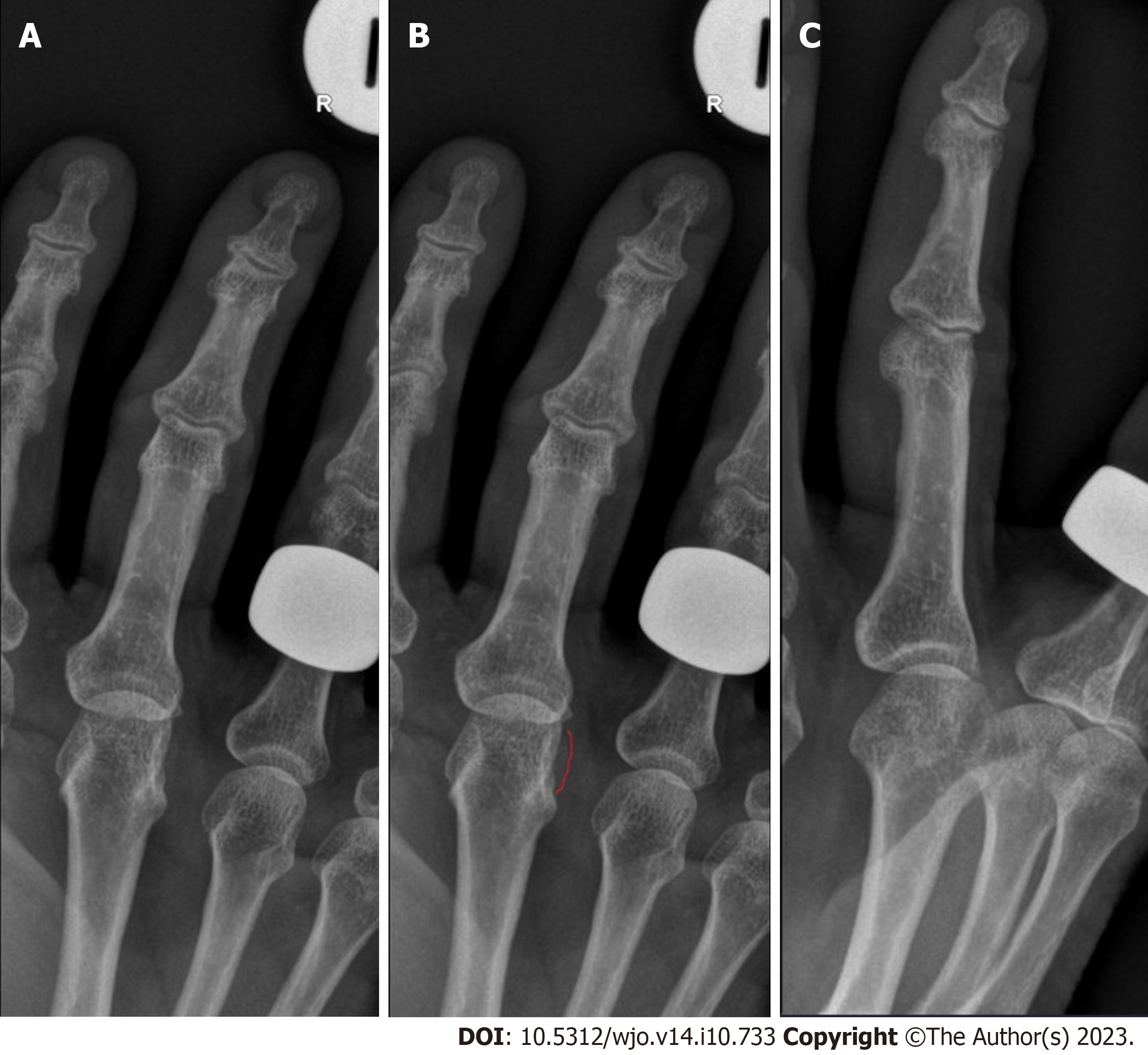
Where the diagnosis is not obvious on clinical examination, radiographs should be the first special investigation and will assist with the diagnosis of a fracture, dislocation, and arthritis (Figure 1). In sagittal band attrition, there may be signs of underlying arthritis and in a locked MCPJ an osteophyte may be visible (Figure 2). X-rays may be normal in early cases of AVN, but in more advanced cases collapse will be present.
Ultrasound can be used to confirm the diagnosis of a trigger finger if there is any doubt, and it will show a thickening of the A1 pulley and possibly the flexor tendon with or without signs of flexor synovitis. Dynamic scanning is possible for cases of suspected EDC subluxation/dislocation to assist with the diagnosis. Ultrasound can also be used in cases of a locked MCPJ to diagnose an entrapped collateral ligament or torn palmar plate. Even Dupuytren’s nodules and cords can be confirmed with ultrasound[21].
Blood tests will not help to differentiate between the diagnosis discussed here, but where a possible inflammatory or crystalline arthropathy is suspected or in cases of AVN it may be useful to determine the underlying cause.
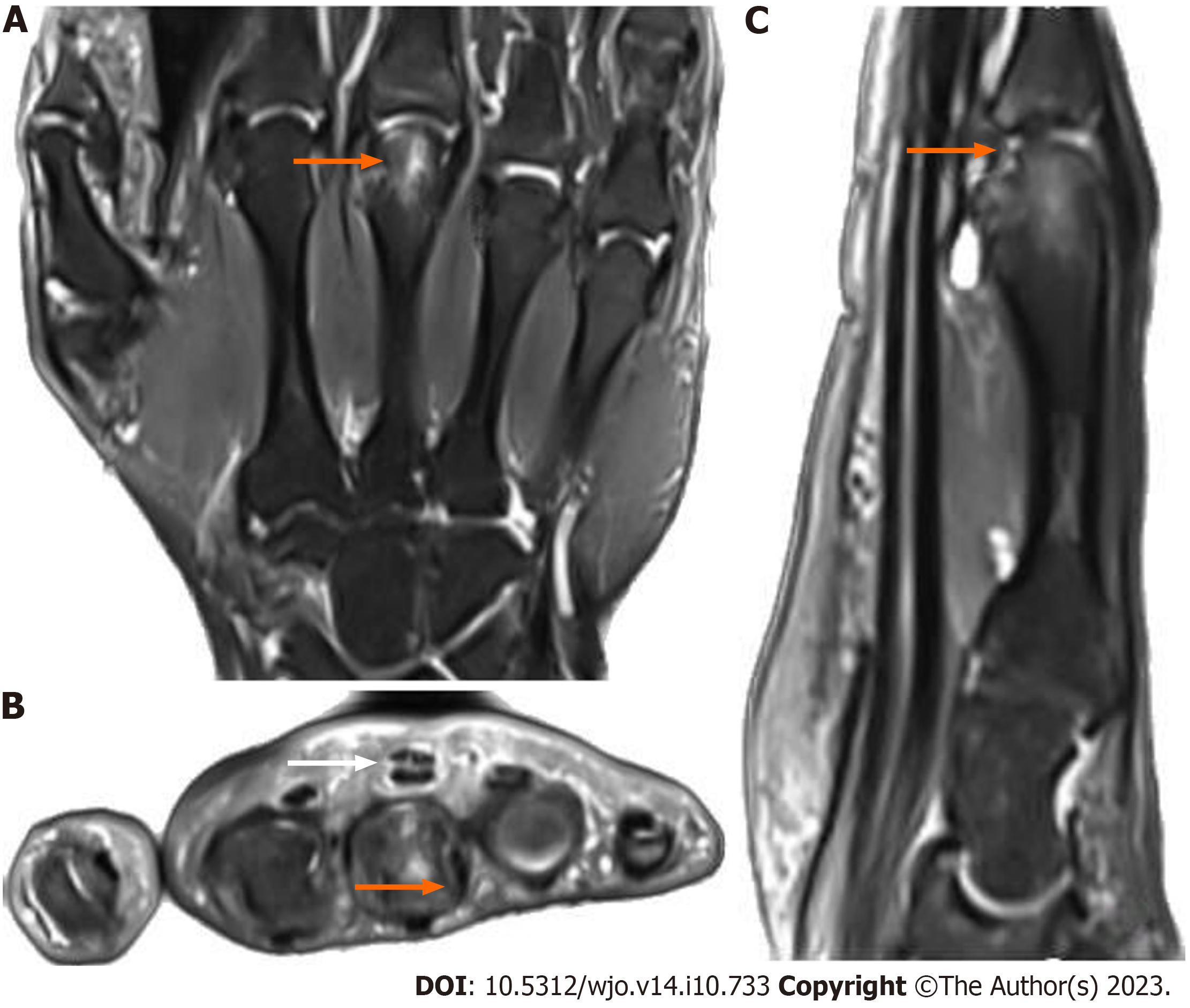
The main purpose of magnetic resonance imaging (MRI) is in the detection of early AVN[17] (Figure 3) where the x-ray is still normal and other diagnoses have been excluded and it can assist in the diagnosis of a locked MCPJ[15]. Even though MRI will pick up trigger fingers, arthritis, sagittal band attrition/rupture, fractures, and Dupuytren’s cords/nodules, it is not recommended as first-line investigation for any of these conditions.
An in-depth discussion of the treatment of all these conditions is outside the scope of this article, but we will discuss some general treatment principles and in brief discuss specific treatments for each condition.
Lifestyle modification and diet change is the simplest early treatment. As long as lifestyle modification does not affect quality of life, it can be very effective. Therapy with or without the use of splints is the next line of non-invasive therapy. A Prospective, Randomized, Double-Blind, Placebo-Controlled, Multicenter Clinical Trial showed that avocado/soybean unsaponifiables are more effective than placebo in providing symptomatic relief in hip and knee osteoarthritis[22]. Other medications such as non-steroidal anti-inflammatory medication can also be very effective in providing symptomatic relief. Cortisone injections, which in some cases only provide temporary symptomatic relief, can potentially be curable in for instance trigger fingers. Surgery is generally the last line of treatment, but in most cases is the most reliable solution for providing long-term relief.
It is important to remember that 52% of trigger fingers will resolve spontaneously without any intervention within 8 mo of the onset of symptoms[23]. Splints can be effective in up to 55% of cases in 1 year, but it is uncertain how many of these would have resolved spontaneously[1]. A single cortisone injection can be curative in 45%-80% of cases with repeat injections being effective in 30%-40% of cases[1]. There seems to be no difference between an injection into the flexor sheath vs an injection outside the flexor sheath[24]. Surgery can be performed as either open or percutaneous[7] and provides the best chance of a long-term symptom-free result.
When conservative management fails (see under general measures), arthroplasty is usually the surgical option of choice[9]. In cases of inflammatory or crystalline arthropathy, it is important to refer the patient to a Rheumatologist to adequately manage the underlying cause. It is worth remembering that hemochromatosis can cause arthritis of the index and middle finger MCPJs[25] and the patient should be worked up for this and referred for treatment if indicated.
Fractures should be managed according to the fracture type, displacement, angulation, rotation, and shortening. Most fractures can be managed conservatively in a splint, but if the position is not acceptable, may require a closed reduction with or without k-wires or an open reduction and internal fixation. Dislocations require reduction and this can mostly be achieved by closed means. In case of failed closed reduction or incongruent reduction, open surgery must be performed.
The majority of cases can be managed in a splint[10,12], especially within 3 wk of the injury[11,20]. Surgery is reserved for the professional athlete, chronic cases, or those who failed conservative treatment and can be either a direct repair or sagittal band reconstruction[10,11].
Closed reduction can be attempted by injecting local anesthetic into the joint and then applying gentle traction and rotation, but this does carry the risk of a potential fracture. Most cases are managed surgically by open reduction and excision of the osteophyte[14,15].
The first line of treatment should be rest and medication, but if this fails, then the surgical options are curettage and bone graft, osteotomy, osteochondral grafts, denervation, arthrodesis, or arthroplasty[17].
Once there is the progression of the contracture and it becomes functionally debilitating, surgery, either percutaneous needle aponeurotomy or fasciectomy (partial or segmental), becomes the treatment of choice[19].
The success of cortisone injections in trigger fingers has already been discussed. Surgery, whether open or percutaneous can have success rates of 90%-100%[1]. Arthroplasty for MCPJ arthritis is successful in improving pain and function and has patient satisfaction rates of up to 90% in certain studies, especially in osteoarthritis[9]. Conservative and surgical management, when indicated, is very effective in the treatment of EDC subluxation/dislocation in terms of symptom improvement[10]. In a case series of locked MCPJs, 13 of 14 patients (1 was lost to follow-up) had an excellent outcome with no pain and a normal range of motion[15]. AVN of the metacarpal head is rare and therefore little is known about the long-term prognosis[17]. Fractures, dislocations, and Dupuytren’s contractures have so many treatment options and are such vast topics in themselves, that the discussion of treatment specifics and prognosis falls outside the scope of this article.
With regards to what we currently know about this condition, triggering, clicking, locking, and crepitus of the finger are symptoms typically associated with a condition known as “trigger finger” or stenosing tenosynovitis. This condition primarily affects the flexor tendons of the fingers and is characterized by certain signs and symptoms. Triggering is a sensation where the finger gets stuck in a bent position and then suddenly releases with a “click” or “pop.” Clicking can be defined as an audible or palpable clicks or snaps during finger movement. Locking occurs when the finger becomes locked in a flexed position, requiring manual assistance to extend it. Crepitus can be described as the sensation or sound of grinding, popping, or crackling within the affected finger during movement.
Current knowledge suggests that these symptoms arise due to inflammation or thickening of the tendon sheath, obstructing the smooth gliding of the flexor tendon. The exact causes of the trigger finger are multifactorial, with risk factors including repetitive gripping activities, underlying medical conditions, and genetic predisposition.
The current theories that drive the clinical applications in the management include the inflammation within the tendon sheath plays a key role in trigger finger symptoms. Treatments often involve anti-inflammatory medications, corticosteroid injections, or physical therapy. The Structural Theory is thought that structural changes in the tendon, such as nodules or thickening, are responsible for the condition. Surgical interventions, such as tenosynovectomy or release, aim to address these structural issues. The Biomechanical Theory includes mechanical factors, like repetitive strain or improper hand ergonomics, which are thought to contribute to the development of trigger fingers. Occupational therapy and ergonomic modifications are employed to alleviate symptoms.
Further research on the trigger finger is essential for several reasons. Trigger finger is a common hand condition, and its prevalence is increasing, possibly due to changes in lifestyles and work habits. Understanding it better can help address this growing health concern. The condition can significantly impact an individual's quality of life, affecting their ability to perform daily activities and work. Improved management strategies can enhance patients' well-being. Trigger finger is associated with healthcare costs, including treatments, lost workdays, and rehabilitation. Better management approaches could reduce the economic burden.
Advancements in treatment are fundamental. As our understanding of the condition deepens, more targeted and effective treatment options can be developed, potentially reducing the need for surgery and minimizing recurrence rates. Research should focus on the long-term outcomes of different treatment modalities, including surgery, corticosteroid injections, and conservative therapies, to determine which provides the best-sustained relief.
Understanding the underlying pathophysiological mechanisms of the trigger finger can lead to more precise diagnostic tools and therapeutic targets. Identifying additional risk factors beyond those currently recognized can help with early detection and preventive measures. The efficacy of non-surgical treatments, such as physical therapy, occupational therapy, and ergonomic modifications, needs more extensive study to establish their role in managing the trigger finger.
Studies investigating the long-term outcomes of various treatment approaches, elucidating the precise patho
Triggering (locking, clicking) and crepitus of the fingers are symptoms that commonly occur. It can co-exist as part of the same pathology, but more often occur separately and point towards different pathologies. Even though trigger fingers are the most common cause of pain and disability in the hand, it is important to consider the other possible diagnoses. A thorough history and clinical examination with appropriate special investigations will aid in making the correct diagnosis. Adequate treatment has a high success rate in terms of resolution of symptoms and good functional recovery.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lee S, South Korea S-Editor: Lin C L-Editor: Filipodia P-Editor: Xu ZH
| 1. | Gil JA, Hresko AM, Weiss AC. Current Concepts in the Management of Trigger Finger in Adults. J Am Acad Orthop Surg. 2020;28:e642-e650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 2. | Merry SP, O'Grady JS, Boswell CL. Trigger Finger? Just Shoot! J Prim Care Community Health. 2020;11:2150132720943345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Vasiliadis AV, Itsiopoulos I. Trigger Finger: An Atraumatic Medical Phenomenon. J Hand Surg Asian Pac Vol. 2017;22:188-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Weng W. Symptoms, Diagnosis, and Treatments of Stenosing Tenosynovitis. Highlights in Science, Engineering and Technology. 2023;36:246-53. [DOI] [Full Text] |
| 5. | Wolfe SW, Pederson WC, Kozin SH, Cohen MS. Green’s Operative Hand Surgery. 8th ed. Amsterdam: Elsevier, 2021. |
| 6. | Blough C, Najdawi J, Kuschner S. Patient preference for trigger finger treatment. World J Orthop. 2022;13:1006-1014. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 7. | David M, Rangaraju M, Raine A. Acquired triggering of the fingers and thumb in adults. BMJ. 2017;359:j5285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Lunsford D, Valdes K, Hengy S. Conservative management of trigger finger: A systematic review. J Hand Ther. 2019;32:212-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 9. | Rizzo M. Metacarpophalangeal joint arthritis. J Hand Surg Am. 2011;36:345-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Kleinhenz BP, Adams BD. Closed Sagittal Band Injury of the Metacarpophalangeal Joint. J Am Acad Orthop Surg. 2015;23:415-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | James N, Farrell N, Mauck B, Calandruccio J. Sagittal Band Injury and Extensor Tendon Realignment. Orthop Clin North Am. 2022;53:319-325. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Hong IT, Oh CH, Sim YS, Han SH. Direct repair of the sagittal band for extensor tendon subluxation caused by finger flicking. Orthopade. 2017;46:755-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Rayan GM, Murray D. Classification and treatment of closed sagittal band injuries. J Hand Surg Am. 1994;19:590-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 69] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | VanHelmond TA, Kim MT, Wang ED. Middle Finger Metacarpophalangeal Joint Locked in Flexion Caused by Entrapped Ulnar Collateral Ligament. J Hand Surg Glob Online. 2022;4:379-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 15. | Thomsen L, Roulot E, Barbato B, Dumontier C. Locked metacarpophalangeal joint of long fingers: classification, definition and treatment based on 15 cases and literature review. Chir Main. 2011;30:269-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Cavalcanti Kußmaul A, Ayache A, Unglaub F. [Trigger finger-pitfalls and differential diagnosis]. Orthopadie (Heidelb). 2023;52:604-608. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Fan XL, Wang WT, Wang J, Xiao R. Current management of avascular necrosis of the metacarpal head: a comprehensive literature review. Int J Surg. 2023;109:1509-1517. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 18. | McGoldrick NP, McGoldrick FJ. Avascular necrosis of the metacarpal head: a case of Dietrich's disease and review of the literature. Am J Case Rep. 2015;16:12-15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Ruettermann M, Hermann RM, Khatib-Chahidi K, Werker PMN. Dupuytren's Disease-Etiology and Treatment. Dtsch Arztebl Int. 2021;118:781-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | Wu K, Masschelein G, Suh N. Treatment of Sagittal Band Injuries and Extensor Tendon Subluxation: A Systematic Review. Hand (N Y). 2021;16:854-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Molenkamp S, van Straalen RJM, Werker PMN, Broekstra DC. Imaging for Dupuytren disease: a systematic review of the literature. BMC Musculoskelet Disord. 2019;20:224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Maheu E, Mazières B, Valat JP, Loyau G, Le Loët X, Bourgeois P, Grouin JM, Rozenberg S. Symptomatic efficacy of avocado/soybean unsaponifiables in the treatment of osteoarthritis of the knee and hip: a prospective, randomized, double-blind, placebo-controlled, multicenter clinical trial with a six-month treatment period and a two-month followup demonstrating a persistent effect. Arthritis Rheum. 1998;41:81-91. [PubMed] [DOI] [Full Text] |
| 23. | McKee D, Lalonde J, Lalonde D. How Many Trigger Fingers Resolve Spontaneously Without Any Treatment? Plast Surg (Oakv). 2018;26:52-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Mardani-Kivi M, Karimi-Mobarakeh M, Babaei Jandaghi A, Keyhani S, Saheb-Ekhtiari K, Hashemi-Motlagh K. Intra-sheath versus extra-sheath ultrasound guided corticosteroid injection for trigger finger: a triple blinded randomized clinical trial. Phys Sportsmed. 2018;46:93-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Wimalawansa SM, Alsamkari R. Unusual presentation of hemochromatosis as isolated metacarpophalangeal joint osteoarthritis: a case report. Hand (N Y). 2011;6:329-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |