Published online Sep 18, 2022. doi: 10.5312/wjo.v13.i9.812
Peer-review started: January 4, 2022
First decision: February 21, 2022
Revised: May 4, 2022
Accepted: August 10, 2022
Article in press: August 10, 2022
Published online: September 18, 2022
Processing time: 262 Days and 11.6 Hours
Between 43% and 75% of patients who undergo primary anterior cruciate ligament (ACL) surgery return to sport activity. However, after a revision ACL reconstruction (ACLR) the rate of return to sports is variable. A few publications have reported returns to sports incidence between 56% to 100% after revision ACLR.
To determine return to sports and functional outcomes after a single-stage revision ACLR with a 5-year minimum follow-up at a single institution.
All patients operated between 2010 and 2016 with a minimum 5 years of follow-up were included. Type of sport, intensity, frequency, expectation, time to return to sport and failure rate were recorded. Lysholm, Tegner and International Knee Documentation Committee forms were evaluated prior to the first ACLR surgery, at 6 mo after primary surgery and after revision ACLR at 5 years minimum of follow-up. Objective stability was tested with the knee arthrometer test (KT-1000 knee arthrometer, Medmetric Corp).
A total of 41 patients who underwent revision ACLR during that period of time were contacted and available for follow-up. Median patient age at time of revision was 29 years old [interquartile range (IQR): 24.0-36.0], and 39 (95.0%) were male. The median time from revision procedure to follow-up was 70 mo (IQR: 58.0-81.0). Regarding return to sports, 16 (39.0%) were at the same level compared to preinjury period, and 25 patients (61.0%) returned at a lower level. Sixty-three percent categorized the sport as very important and 37.0% as important. One patient (2.4%) failed with a recurrent ACL torn. Mean preoperative Lysholm and subjective International Knee Documentation Committee scores were 58.8 [standard deviation (SD) 16] and 50 (SD 11), respectively. At follow-up, mean Lysholm and subjective International Knee Documentation Committee scores were 89 (SD 8) and 82 (SD 9) (P = 0.0001). Mean Tegner score prior to primary ACLR was 6.7 (SD 1.3), 5.1 (1.5 SD) prior to revision ACLR and 5.6 (1.6 SD) at follow-up (P = 0.0002). Overall, knee arthrometer test measurement showed an average of 6 mm (IQR: 4.0-6.0) side-to-side difference of displacement prior to revision ACLR and 3mm (IQR: 1.5-4.0) after revision.
Almost 40.0% of patients returned to preinjury sports level and 60.0% to a lower level. These may be useful when counseling a patient regarding sports expectations after a revision ACLR.
Core Tip: This was a retrospective case series with 41 patients seeking to evaluate return to sports and clinical outcomes after revision anterior cruciate ligament reconstruction at 5 years minimum of follow up. Retrospective analyzed data included physical examination, Tegner activity level, Lysholm, International Knee Documentation Committee, type of sport, intensity, frequency, expectation and time to return to sport. Objective stability was tested with the knee arthrometer test. All data were recorded at the base line and after a 5-year minimum follow-up.
- Citation: Ortiz E, Zicaro JP, Garcia Mansilla I, Yacuzzi C, Costa-Paz M. Revision anterior cruciate ligament reconstruction: Return to sports at a minimum 5-year follow-up. World J Orthop 2022; 13(9): 812-824
- URL: https://www.wjgnet.com/2218-5836/full/v13/i9/812.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i9.812
Consequent to a substantial increase in the incidence of anterior cruciate ligament (ACL) ruptures, revision ACL reconstruction (ACLR) has also suffered an increase[1]. The ACL re-rupture rate is between 4% to 6%, with the event occurring in the first 2 years in more than half of the cases[2-4]. The rate of one-third of ACL ruptures is around 13% to 19% according to different publications[5-7]. In addition, these patients also present an increased risk of developing early arthritis[8].
Historically, return to sports (RTS) is defined as the return to the pre-injury activity in one or two seasons, at the same sporting level[9]. A recently published consensus described continuous RTS in three stages: return to participation, RTS and return to previous performance. Thus, return to participation refers to the return to training or to a lower sporting level than the one practiced by the patient previously. RTS refers to the return to the sport previously performed, although not at the desired level. Return to previous performance refers to the return to the same level or a higher level than before the injury[10].
Between 43% and 75% of patients who undergo primary ACL surgery RTS[11-15]. However, after a revision ACLR the reported rates of RTS are very variable[16]. Causes of non-RTS are multifactorial and include age, sex, psychological factors, type of sport, number of previous surgeries, time lapse between surgeries and graft choice[11-26]. Few publications report sports return rates after revision ACLR, both in the medium and long term, and they vary from 56% to 100%[27-31]. The purpose of this study was to evaluate the rate of RTS in patients with revision ACLR after 5 years of surgery. The secondary purpose was to report the functional outcomes.
This study was approved by the Ethics Committee of our hospital. A retrospective study was performed including all patients who underwent a revision ACLR between 2010 and 2016. The inclusion criteria were patients with traumatic or atraumatic knee instability with a displacement equal to or larger than 5 mm anteroposterior compared to the contralateral knee measured with the KT-1000 arthrometer after primary ACL surgery and older than 18 years.
Patients with multiligament injuries (more than two ligaments injured at the same time), second ACL revision and patients with osteotomies at time of revision ACLR surgery were excluded (Table 1).
| Demographics | Results (N = 41) |
| Yr, median (IQR) | 29 (24-36) |
| Male, n (%) | 39 (95) |
| Follow up (mo) (IQR) | 70 (58-81) |
| Period (a) | 2010-2016 |
| Injury mechanism prior revision ACLR | |
| Traumatic | 26 (63.4%) |
| Atraumatic | 15 (36.6%) |
| Time between (mo) | |
| ACL Primary surgery and retear | 22 (22-39) |
| Revision ACLR and return to sport | 13 (11-15) |
| Failure | 1 (2.4%) |
A single stage revision ACLR was performed in the whole series. A diagnostic arthroscopy was performed in every case, and if necessary associated meniscal and cartilage lesions were treated. In 5 patients, allografts were used. The fixation technique was with 2 titanium screws for bone tendon bone, and in cases of hamstrings or anterior tibial allograft; fixation was performed with a cortical button in the femur and a biocomposite interferential screw in the tibia.
All patients entered the same rehabilitation protocol with rearrangements for individual needs. Partial loading was allowed for the first 3 wk. Passive flexion and extension range of motion were carried out. In special cases with complex meniscal sutures or cartilage treatment with mosaicoplasty, full loading was delayed until week 6. From the 4th month onwards, low impact workout exercises and progressive muscle strengthening were started. RTS was allowed after 10 mo depending on the sport practiced prior to the revision ACLR and based on an evaluation by our rehabilitation team.
Assessment was performed by a single evaluator in this study. Age, sex, follow-up time, injury mechanism prior to revision ACLR, time between primary surgery and re-rupture, time between revision ACLR and RTS, technique used in both primary surgery and revision ACLR and associated procedures were recorded.
All patients were asked about the type and level of sport practiced, the motivation to RTS and the expectation of returning to sport in three instances: prior to the first ACL reconstruction surgery, after primary surgery and after revision ACLR and RTS. RTS activity was considered to be the return to their sport prior to the last injury at the same level or below the previous level. Motivation was classified as: very important, important, moderately important, minimally important or not important. The expectation regarding RTS was classified as: return to the same sport level, return to a lower level or not returning to the same sport. The number of sports practices per week before and after the revision ACLR was recorded.
Using the Tegner score, the type of sport was classified into high impact, moderate and low impact, according to the classification published in 2015 by the American Heart Association[32]; high impact was considered those with Tegner greater or equal to 7, moderate impact with Tegner between 4 to 6 and low impact with Tegner between 1 to 3. Lysholm and International Knee Documentation Committee Knee (IKDC) scores were used prior to the revision ACLR and at the last follow-up. For an objective assessment, the KT-1000 arthrometer (Medmetric Corp) was used at the last follow-up.
We defined failure of revision ACLR surgery as ACL re-rupture, whether traumatic or atraumatic, associated with positive pivot shift and a difference in arthrometry with KT-1000 greater than or equal to 5 mm requiring new surgery.
Due to the small sample of patients non-sample size calculations were conducted. Continuous variables were described as median and interquartile ranges. Categorical variables were reported as proportions with their absolute frequency. Stata 14 software was used for the analysis. Statistical significance was considered to be P = 0.05.
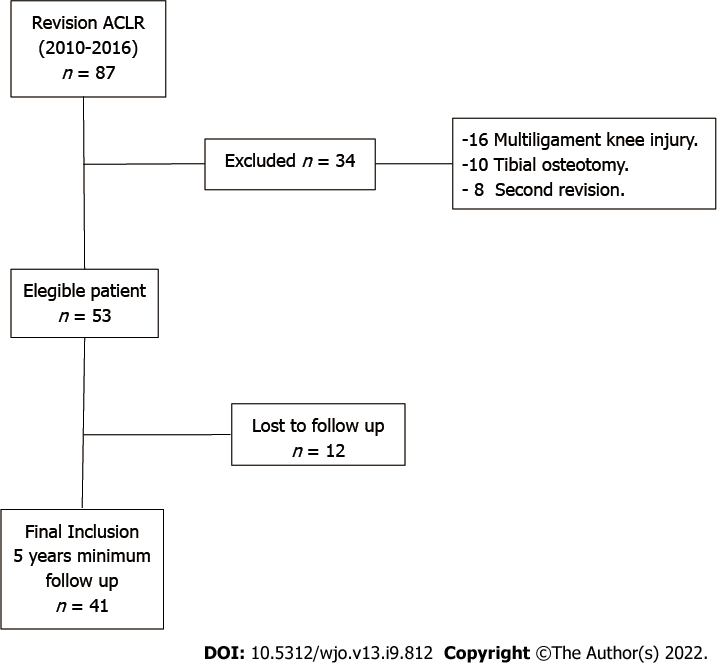
A total of 87 revision ACLR were performed in the study period: 16 were excluded because of multiligamentary lesions, 8 were second revisions, and 10 were associated with osteotomy. Of the 53 patients who met the inclusion criteria, 12 patients were lost during follow-up. The series consisted of 41 patients with a median follow-up of 70 mo (IQR: 58.0-81.0) (Figure 1). Thirty-nine patients were male with a median age of 29 years (IQR: 24.0-36.0). Table 1 shows the demographic data.
A total of 27 (65.8%) patients had concomitant meniscal lesions. The medial meniscus was more frequently injured (n = 26); 20 (77.0%) were treated with meniscectomy, 6 (19.0%) with repair and 1 (4.0%) with meniscal transplantation. Lateral meniscus was injured in 14 patients; all were treated with partial meniscectomy. Chondral lesions were found in 5 (12.0%) patients; 3 (60.0%) were treated with microfractures and 2 (40.0%) with chondroplasty (Table 2).
| Graft | n (%) | Surgical technique | n (%) | Augmentation | n (%) |
| Primary ACL | |||||
| Hamstring | 29 (70.7) | Monotunnel | 36 (87.0) | - | - |
| BPTB | 11(26.8) | Anatomic | 5 (12.0) | - | - |
| Allograft | 1 (2.4) | ||||
| Revision ACLR | |||||
| Hamstring | 10 (24.3) | Anatomic | 41 (100) | Lemaire | 15 (36.0) |
| BTB | 29 (70.3) | Allograft | 2 (4.8) | ||
| Allograft | 5 (2.0) | No Augmentation | 24 (58.0) | ||
| Concomitant lesions | |||||
| Both meniscus | 9 of 41 (21.0) | ||||
| Medial meniscus | 26 of 41 (66.0) | ||||
| Meniscectomy | 20 (77.0) | ||||
| Meniscal suture | 5 (19.0) | ||||
| Meniscal transplantation | 1 (4.0) | ||||
| Lateral meniscus | |||||
| Meniscectomy | 14 of 41 (34.0) | ||||
| Chondral lesions | 5 (12.0) |
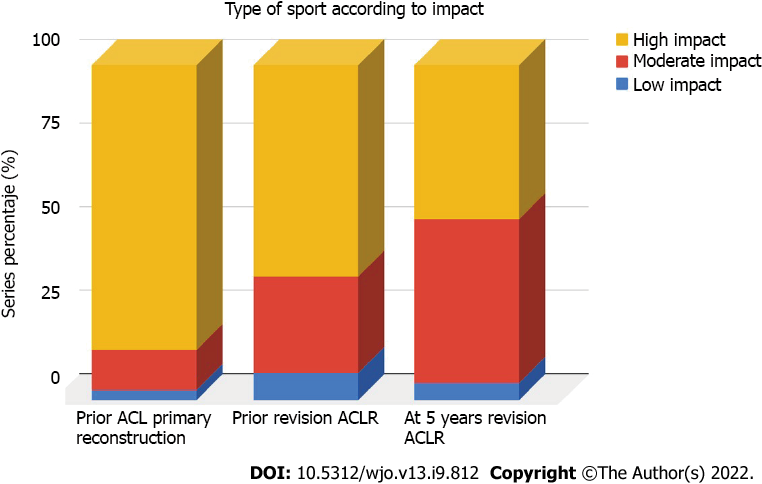
Prior to the first injury, 35 (85.0%) patients practiced high impact activities, 5 (12.0%) moderate and 1 (3.0%) low impact. After the first ACL surgery, 26 (63.0%) patients practiced high impact, 12 (29.0%) moderate and 3 (8.0%) low impact; 5 years after ACL revision, 19 (46.0%) continued to perform high impact, 20 (49.0%) moderate and 2 (5.0%) low impact (Figure 2). Prior to revision ACLR the patients practiced: soccer (24, 59.0%), running (9, 22.0%), gym (3, 7.0%), rugby (2, 5.0%), tennis (1, 2.0%), cycling (1, 2.0%) and other (1, 2.0%) other.
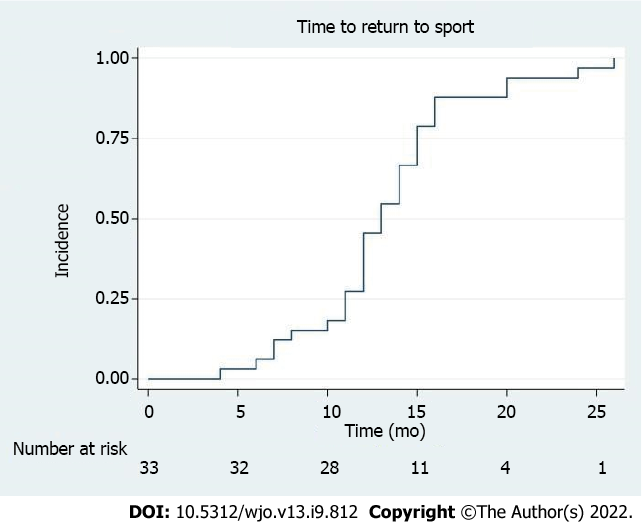
After primary ACL surgery, 13 (31.0%) returned to the same level of sport, 26 (64.0%) to a lower level and 2 (5.0%) did not RTS. The rate of RTS for revision ACLR was 16 (39.0%) returning to the same level of sport and 25 (61.0%) to a lower level (Table 3). The time to RTS for both post-primary surgery and revision ACLR was 13 mo (IQR 11.0-15.0) (Figure 3).
| Return to sports rate | ||
| Primary ACLR, % | Revision ACLR, % | |
| Total return | 95.0 | 100 |
| Same level | 31.7 | 39.0 |
| Lower level | 63.4 | 61.0 |
Eighty percent (12/15) of patients without associated procedures and 73.0% (19/26) of patients with associated procedures returned to the same sports level, with no statistically significant differences (P = 0.61). Similarly, we found no association (P > 0.44) between the associated procedures performed at the time of revision ACLR surgery and the type of sport.
Regarding impact activity after revision surgery, it is interesting to note that 13.0%[7] modified their sports practice. When classifying sports according to impact based on Tegner, we recorded a 40.0% decrease from high impact to moderate impact activity and a 2.2% decrease from moderate to low impact after 5 years of follow-up after revision ACLR (Table 4) (Figure 2). Of those who played soccer, 1 patient changed to tennis, 1 to functional training and 1 to running. Of those who performed running, 1 began to perform a pivoting activity (soccer) and the other 2 modified it to a low-impact activity (bicycle and yoga). This result was not modified for patients older than 40 years, in contrast to what it may be thought that in older patients (older than 40 years) the chances of modifying or abandoning sport is higher. The frequency with which they practiced sports in a week before and after the revision ACLR was maintained over time, being an average of twice a week (range 1-3); 26 (63.0%) patients practiced activities twice a week before the revision ACLR and 21 (51.0%) post-surgery.
| Impact sport and Tegner | Prior to primary ACLR, n (%) | At 5 yr revision ACLR, n (%) |
| Low | 1 (2.4) | 2 (4.8) |
| Moderate | 5 (12.2) | 20 (48.7) |
| High | 35 (85.3) | 19 (46.3) |
When assessing motivation, 26 (63.0%) classified it as very important and 15 (37.0%) as important. When the patients were asked about their expectations regarding the RTS after their primary ACL surgery, 33 (80.0%) patients described their intention to return to the same sports level and 8 (20.0%) to return to a lower level. Regarding their expectation after revision ACLR surgery, 16 (39.0%) patients intended to return to the same level and 25 (61.0%) to a lower level (Table 3).
According to the American Heart Association’s classification in relation to Tegner score, a 40.0% decrease in impact activities at 5 years postoperatively was registered. Tegner score prior to primary ACL surgery showed that 80.5% performed recreational physical activity, 9.8% performed their usual light work and 9.8% performed competitive sports activity. After primary ACL surgery, 58.5% performed their usual work, 36.6% performed recreational physical activity and 4.9% performed competitive sports activity. Post revision ACLR, 53.7% performed recreational physical activity, 41.5% performed their usual work/task and 4.9% performed competitive sports activity.
Prior to revision ACLR surgery the Lysholm score was good in 1.9% of the series, 35.8% were fair, and 62.3% were poor. For postoperative revision ACLR the score was excellent in 31.7% of the series, good in 56.1%, fair in 7.3% fair and poor in 4.9%. The Tegner, Lysholm and IKDC scores are summarized in Table 5. With the differential KT-1000 arthrometer the median values prior to ACL revision were 5 mm (IQR: 4.0-6.0) and at last follow-up 3 mm (IQR: 1.5-4.0). Finally, 1 patient had a failure after ACL revision surgery (2.4%) at 72 mo postoperatively.
| Preoperative | SD | 5 yr postoperative | SD | Delta | SD | 95%CI | P value | |
| Tegner | 6.7 | (1.3) | 5.6 | (1.6) | -1.170 | (1.8) | -1.739 to -0.602 | 0.002 |
| Lysholm | 58.8 | (16.0) | 89.0 | (8.0) | 30.121 | (17.0) | 24.736 to 35.507 | < 0.001 |
| IKDC | 50.0 | (11.0) | 82.0 | (9.0) | 31.475 | (15.0) | 26.649 to 36.300 | < 0.001 |
The main finding of this study was that all patients returned to their sports practice after revision ACLR, 61.0% at a lower level and 39.0% at the same level prior to revision ACLR surgery. The rate of return to full sport, according to a systematic review of 48 studies with 5770 patients, is 82% in patients with primary ACL surgery. Only 63% returned to the same pre-injury sport, but 44% were able to do so at a competitive level[19]. Although the literature is more limited for RTS in revision ACLR surgery, a systematic review of 23 studies with a total of 1090 patients indicated that 85% of patients returned to sport, 53% to their previous sport and 51% to a competitive level[16]. According to another systematic review, the rate of RTS in patients with revision ACLR surgery ranged from 56% to 100%[33], similar to our series.
There are several factors that influence RTS: social, psychological and demographic factors. Age and sex are important factors. Men have a 10% higher rate of return than women, and young people (< 25 years) have a rate higher than 30% compared to adult patients[19,20,31,33]. The longer the time between ACL re-rupture and revision surgery, the lower the rates of RTS as well as an increase in associated injuries as revision surgery is delayed[19]. In the same way, the graft choice could be a determining factor in the RTS; however, it has not been studied in depth[27].
In our series, the time to RTS was the same (13 mo) with no significant differences found when dividing the series into those older than 25 years and those younger than 25 years as well as when differentiating between sex. The median time between ACL re-rupture and revision ACLR was 21 mo (IQR: 3.0-24.0). For patients who took more than 1 year to undergo a revision ACLR, the RTS was also at 13 mo on average (7 to 26) with no significant differences with the overall rate of sports return (P = 0.64).
Focusing on the graft choice, according to a meta-analysis of 32 studies comparing hamstring and bone tendon bone for revision surgeries, an increase in the IKDC, Lysholm and Tegner scores and a decrease in complications and reoperations was observed in favor of hamstrings[40]. In contrast to this, the authors of the study recommended that the graft choice should be based on the circumstances of each patient, the technique preferred by each surgeon, the tunnel widening, the type of graft previously used and the possible availability of allografts and not on the rate of RTS according to the type of graft[40]. All patients in our series were treated with autografts with the exception of 5 patients where allografts were used. We did not find significant differences in the time to return in patients where an allograft was used, being 13 mo for both groups. The preference of the authors of this study is to use an autograft from the same injured knee. This is due to the fact that, according to literature, series of patients with revision surgeries in which an autograft was used showed faster rates of RTS in comparison with those in which allografts were used[38,39]. The use of contralateral hamstring tendons for revision ACLR surgeries presented similar subjective and objective rates at 5.2 years of follow-up compared to revision surgeries in which patellar or Achilles tendon allograft was used[39]. In our series we do not have patients operated with contralateral knee grafts.
Several authors recommend that when evaluating series to assess the RTS the Lysholm score should be used together with the Tegner score to be able to more effectively evaluate the sports activity[34]. In our series, Lysholm score after revision ACLR increased by 30.0% for excellent results considered as greater than 95 points (0% preoperative to 31% postoperative) and decreased by 50.0% for poor results (62% preoperative to 4.9% postoperative).
For the Tegner scale we observed a decrease of 1.7 points between preoperative primary ACL surgery and postoperative revision ACLR (P = 0.002) showing the decrease in impact activity between primary surgery and revision ACLR. When comparing our series with the literature for both the Lysholm, Tegner and IKDC scores we found results that are close to the mean (Table 6).
| Ref. | N | Years | F-up in yr | RTS | IKDC | Lysholm | Tegner | KT-1000, mm ± SD | KOOS |
| Battaglia et al[28], 2007 | 63 | 31 | 6.1 | 42 (66%) same level | G/E 36%; P 17%; F 11% | - | - | < 3 | - |
| Diamantopoulos et al[29], 2008 | 107 | 39 | 6 | 39 (36%) same level | G/E 57%; P 34%; F 7% | 88.5 ± 12.4 | 6.3 ± 1.8 | 0.93 ± 1.15 | - |
| Gifstad et al[30], 2013 | 56 | 26 | 7.5 | 7 (13%) same level | - | 80 ± 15 | 6 ± 4 | 3.3 ± 2.7 | 70 ± 21 |
| Shelbourne et al[31], 2014 | 259 | 22 | 7.2 | 178 (68%) same level | Subjective 76 ± 18.3 | - | - | 2.3 ± 1.7 | - |
| Ortiz et al, 2022 | 41 | 29 | 5.8 | 61% same level & 39% lower level | G/E 43%; P 53%; F 4% | 89 ± 8 | 5.6 ± 1.6 | 3 ± 1.2 | - |
When evaluating the expectation of patients regarding their intention to RTS after primary ACL surgery, 80.0% of our series intended to return to the same sport level, while 39.0% reported this intention prior to revision surgery (Tables 7-10 case examples). This 40.0% decrease in the expectation of RTS is consistent with the literature as shown by a study of 675 patients with a return expectation after primary surgery at 1 year of 84% and 63% for revision ACLR surgeries (P < 0.001 and P = 0.08, respectively). A multivariate logistic regression showed two determinant factors for abandoning sports practice, which were having suffered a revision ACLR (P < 0.0001) and being female (P = 0.02). In our series, all patients returned to sports, and we did not obtain representative casuistry to make a comparison between sexes[34].
| Case | Sex | Years | Time between in min | Graft choice | Augmentation at revision ACLR | Concomitant lesions | ||||
| Primary ACLR and retear | Revision ACLR and last evaluation, F-up | Return to sport | Primary | Revision | ||||||
| To Primary ACLR | To Revision ACLR | ACLR | ACLR | |||||||
| 1 | Male | 30 | 36 | 126 | 17 | 20 | Hamstring | BPTB | Lemaire | Medial meniscus tear |
| 2 | Male | 42 | 12 | 131 | 14 | 13 | Hamstring | BPTB | Lemaire | Medial meniscus tear |
| 3 | Male | 29 | 48 | 107 | 13 | 11 | Hamstring | BPTB | Lemaire | Chondral lesions |
| 4 | Male | 35 | 22 | 115 | 10 | 14 | Hamstring | BPTB | - | Chondral lesions |
| 5 | Female | 28 | 13 | 103 | 14 | 16 | Hamstring | BPTB | - | Medial meniscus tear |
| Case | Sex | Years | Return to sport | Type of Sports | Training frequency | ||||
| After | Days per week | ||||||||
| Primary ACLR | Revision ACLR | Prior ACLR | Prior revision ACLR | After revision ACLR | Prior revision ACLR | After revision ACLR | |||
| 1 | Male | 30 | Lower level | Lower level | Soccer | Running | Running | 2 | 1 |
| 2 | Male | 42 | Same level | Same level | Soccer | Soccer | Tennis | 2 | 1 |
| 3 | Male | 29 | Lower level | Same level | Soccer | Running | Soccer | 2 | 2 |
| 4 | Male | 35 | Lower level | Same level | Soccer | Soccer | Soccer | 2 | 2 |
| 5 | Female | 28 | Lower level | Same level | Martial arts | Tennis | Tennis | 2 | 2 |
| Case | Sex | Year | Motivation | Expectation | |
| After primary ACLR | After revision ACLR | ||||
| 1 | Male | 30 | Important | Same level | Lower level |
| 2 | Male | 42 | Very important | Same level | Same level |
| 3 | Male | 29 | Very important | Same level | Lower level |
| 4 | Male | 35 | Very important | Same level | Lower level |
| 5 | Female | 28 | Very important | Same level | Same level |
| Case | Sex | Year | Tegner | Lysholm | IKDC | |||
| Prior revision ACLR | At 5-yr F-up revision ACLR | Prior revision ACLR | At 5-yr F-up revision ACLR | Prior revision ACLR | At 5-yr F-up revision ACLR | |||
| 1 | Male | 30 | 7 | 4 | 47 | 65 | 62 | 71 |
| 2 | Male | 42 | 7 | 7 | 61 | 84 | 49 | 89 |
| 3 | Male | 29 | 7 | 4 | 39 | 86 | 59 | 90 |
| 4 | Male | 35 | 7 | 4 | 80 | 95 | 37 | 97 |
| 5 | Female | 28 | 7 | 6 | 38 | 86 | 49 | 86 |
The association between chondral and meniscal lesions showed poor functional results in patients with revision ACLR surgery; the association of chondral lesions at the time of revision surgery showed lower values according to the Lysholm score in comparison with patients who did not present it. In the same way, patients who presented this lesion modified their intensity in RTS[34-37]. Another study showed poor results in Marx, Knee Injury and Osteoarthritis Outcome Score-quality of life and IKDC activity scores after revision ACLR surgery in patients with chondral lesions and low scores for the Marx and Knee Injury and Osteoarthritis Outcome Score-quality of life scores in patients with medial meniscus lesions[29]. The level of RTS practice was equal or lower in patients who had associated injuries vs patients who did not have associated injuries at the time of revision ACLR surgery. Twelve patients returned to the same level; 3 patients returned to a lower level out of a total of 15 patients who underwent an associated procedure. In our series, 80.0% (12/15) of the patients without associated procedures and 73.0% (19/26) of the patients with associated procedures returned to the same sports level, with no statistically significant differences (P = 0.61).
Among the limitations of our retrospective study, there was no control group of patients with high sports performance nor a numerical scale detailing the level of RTS practice, being this a subjective response of patients. No pre- and postoperative strength or resistance test was performed to determine the “level of muscle strength at their return.” The series was a heterogeneous group of patients in terms of age and type of sport performed. Although the size of the series is close to those reported in international literature, the number is small. The strength of the study is that it is a case series operated in a single institution with a 5-year follow-up after revision ACLR.
Five years after a revision ACLR, 39.0% of patients returned to the same level of sport as before revision ACLR surgery and 61.0% to a lower level. The 13.2% (n = 7) of the series who changed their sports practice was a 40.0% decrease of high impact activity at the time of return. These data could be used to advise patients on the level and timing of sports return.
Between 43% and 75% of patients who undergo primary anterior cruciate ligament (ACL) surgery return to sport activity. However, after a revision ACL reconstruction (ACLR) rate of return to sport are variable. Few publications report return to sports incidence between 56% to 100% after revision ACLR. Five-year minimum follow-up after revision ACLR is a good mid/long-term period evaluation to report return to sport of a case series patients.
Return to sports is a frequent question from patients during the first consultation. We believe this research could help other knee surgeons answer these types of questions. Motivation and expectation must be asked by surgeons during the consultation so as to give the patient a more detailed and realistic response to that question.
The objective was to report functional clinical outcomes and return to sport at a mid/long-term period after revision ACLR.
A retrospective and observational study was performed to describe return to sport of an amateur case series of patients. The entire cohort was asked about motivation, expectation, intensity, frequency and level of return to sport after a 5-year follow-up after revision ACLR.
Thirty-nine percent of the cohort returned at the same level compared to the pre-injury period. Sixty-one percent returned at a lower level. Sixty-three percent categorized the sport as very important and 37.0% as important. One patient (2.4%) failed with a recurrent torn ACL.
Almost 40.0% of patients returned to their pre-injury sport level and 60.0% to a lower level after 5 years of follow-up after revision ACLR.
The direction of future research must be to compare return to sport of professional elite patients against amateur patients.
The authors thank Dr. Marciano S from the Research Department of the Hospital Italiano de Buenos Aires for his participation in the research protocol and statistical analysis.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Argentina
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ozden F, Turkey; Zeng Y, China S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ
| 1. | Liechti DJ, Chahla J, Dean CS, Mitchell JJ, Slette E, Menge TJ, LaPrade RF. Outcomes and Risk Factors of Rerevision Anterior Cruciate Ligament Reconstruction: A Systematic Review. Arthroscopy. 2016;32:2151-2159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of Second ACL Injuries 2 Years After Primary ACL Reconstruction and Return to Sport. Am J Sports Med. 2014;42:1567-1573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 572] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 3. | Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of Secondary Injury in Younger Athletes After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am J Sports Med. 2016;44:1861-1876. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 996] [Cited by in RCA: 871] [Article Influence: 96.8] [Reference Citation Analysis (0)] |
| 4. | Lewis PB, Parameswaran AD, Rue JP, Bach BR Jr. Systematic review of single-bundle anterior cruciate ligament reconstruction outcomes: a baseline assessment for consideration of double-bundle techniques. Am J Sports Med. 2008;36:2028-2036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 100] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | MARS Group. , Ding DY, Zhang AL, Allen CR, Anderson AF, Cooper DE, DeBerardino TM, Dunn WR, Haas AK, Huston LJ, Lantz BBA, Mann B, Spindler KP, Stuart MJ, Wright RW, Albright JP, Amendola AN, Andrish JT, Annunziata CC, Arciero RA, Bach BR Jr, Baker CL 3rd, Bartolozzi AR, Baumgarten KM, Bechler JR, Berg JH, Bernas GA, Brockmeier SF, Brophy RH, Bush-Joseph CA, Butler JB 5th, Campbell JD, Carey JL, Carpenter JE, Cole BJ, Cooper JM, Cox CL, Creighton RA, Dahm DL, David TS, Flanigan DC, Frederick RW, Ganley TJ, Garofoli EA, Gatt CJ Jr, Gecha SR, Giffin JR, Hame SL, Hannafin JA, Harner CD, Harris NL Jr, Hechtman KS, Hershman EB, Hoellrich RG, Hosea TM, Johnson DC, Johnson TS, Jones MH, Kaeding CC, Kamath GV, Klootwyk TE, Levy BA, Ma CB, Maiers GP 2nd, Marx RG, Matava MJ, Mathien GM, McAllister DR, McCarty EC, McCormack RG, Miller BS, Nissen CW, O'Neill DF, Owens BD, Parker RD, Purnell ML, Ramappa AJ, Rauh MA, Rettig AC, Sekiya JK, Shea KG, Sherman OH, Slauterbeck JR, Smith MV, Spang JT, Svoboda SJ, Taft TN, Tenuta JJ, Tingstad EM, Vidal AF, Viskontas DG, White RA, Williams JS Jr, Wolcott ML, Wolf BR, York JJ. Subsequent Surgery After Revision Anterior Cruciate Ligament Reconstruction: Rates and Risk Factors From a Multicenter Cohort. Am J Sports Med. 2017;45:2068-2076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22:116-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 325] [Cited by in RCA: 401] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 7. | Hettrich CM, Dunn WR, Reinke EK; MOON Group, Spindler KP. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41:1534-1540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 230] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 8. | Costa-Paz M, Garcia-Mansilla I, Marciano S, Ayerza MA, Muscolo DL. Knee-related quality of life, functional results and osteoarthritis at a minimum of 20 years' follow-up after anterior cruciate ligament reconstruction. Knee. 2019;26:666-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Lynch AD, Logerstedt DS, Grindem H, Eitzen I, Hicks GE, Axe MJ, Engebretsen L, Risberg MA, Snyder-Mackler L. Consensus criteria for defining 'successful outcome' after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2015;49:335-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 215] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 10. | Ardern CL, Glasgow P, Schneiders A, Witvrouw E, Clarsen B, Cools A, Gojanovic B, Griffin S, Khan KM, Moksnes H, Mutch SA, Phillips N, Reurink G, Sadler R, Silbernagel KG, Thorborg K, Wangensteen A, Wilk KE, Bizzini M. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med. 2016;50:853-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 517] [Article Influence: 57.4] [Reference Citation Analysis (0)] |
| 11. | Ardern CL, Österberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48:1613-1619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 286] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 12. | Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 274] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 13. | Brophy RH, Schmitz L, Wright RW, Dunn WR, Parker RD, Andrish JT, McCarty EC, Spindler KP. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40:2517-2522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 275] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 14. | Erickson BJ, Harris JD, Cvetanovich GL, Bach BR, Bush-Joseph CA, Abrams GD, Gupta AK, McCormick FM, Cole BJ. Performance and Return to Sport After Anterior Cruciate Ligament Reconstruction in Male Major League Soccer Players. Orthop J Sports Med. 2013;1:2325967113497189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Musahl V, Karlsson J, Krutsch W, Mandelbaum BR, Espregueira-Mendes J, d’Hooghe P. Return to Play in Football: An Evidence-based Approach. Springer; 2018. 987 p.. [DOI] [Full Text] |
| 16. | Grassi A, Zaffagnini S, Marcheggiani Muccioli GM, Neri MP, Della Villa S, Marcacci M. After revision anterior cruciate ligament reconstruction, who returns to sport? Br J Sports Med. 2015;49:1295-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | Feller J, Webster KE. Return to sport following anterior cruciate ligament reconstruction. Int Orthop. 2013;37:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 18. | Webster KE, Feller JA, Leigh WB, Richmond AK. Younger Patients Are at Increased Risk for Graft Rupture and Contralateral Injury After Anterior Cruciate Ligament Reconstruction. [RCA] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 373] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 19. | Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1016] [Cited by in RCA: 840] [Article Influence: 60.0] [Reference Citation Analysis (0)] |
| 20. | Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543-1552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1062] [Cited by in RCA: 915] [Article Influence: 83.2] [Reference Citation Analysis (0)] |
| 21. | Lai CCH, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52:128-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 342] [Article Influence: 42.8] [Reference Citation Analysis (0)] |
| 22. | Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41:1549-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 355] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 23. | Kvist J, Österberg A, Gauffin H, Tagesson S, Webster K, Ardern C. Translation and measurement properties of the Swedish version of ACL-Return to Sports after Injury questionnaire. Scand J Med Sci Sports. 2013;23:568-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9:9-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 448] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 25. | Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43:377-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 230] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 26. | Sonesson S, Kvist J, Ardern C, Österberg A, Silbernagel KG. Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: expect and motivate to satisfy. Knee Surg Sports Traumatol Arthrosc. 2017;25:1375-1384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 117] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 27. | Saper M, Pearce S, Shung J, Zondervan R, Ostrander R, Andrews JR. Outcomes and Return to Sport After Revision Anterior Cruciate Ligament Reconstruction in Adolescent Athletes. Orthop J Sports Med. 2018;6:2325967118764884. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 28. | Battaglia MJ 2nd, Cordasco FA, Hannafin JA, Rodeo SA, O'Brien SJ, Altchek DW, Cavanaugh J, Wickiewicz TL, Warren RF. Results of revision anterior cruciate ligament surgery. Am J Sports Med. 2007;35:2057-2066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | Diamantopoulos AP, Lorbach O, Paessler HH. Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med. 2008;36:851-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 113] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 30. | Gifstad T, Drogset JO, Viset A, Grøntvedt T, Hortemo GS. Inferior results after revision ACL reconstructions: a comparison with primary ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2013;21:2011-2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 31. | Shelbourne KD, Benner RW, Gray T. Return to Sports and Subsequent Injury Rates After Revision Anterior Cruciate Ligament Reconstruction With Patellar Tendon Autograft. Am J Sports Med. 2014;42:1395-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 32. | Levine BD, Baggish AL, Kovacs RJ, Link MS, Maron MS, Mitchell JH, et al Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 1: Classification of Sports: Dynamic, Static; and Impact: A Scientific Statement From the American Heart Association and American College of Cardiology. Circulation. 2015 Dec 1;132(22):e262–6.. [RCA] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 94] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 33. | Anand BS, Feller JA, Richmond AK, Webster KE. Return-to-Sport Outcomes After Revision Anterior Cruciate Ligament Reconstruction Surgery. Am J Sports Med. 2016;44:580-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 34. | Webster KE, Feller JA. Expectations for Return to Preinjury Sport Before and After Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2019;47:578-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 82] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 35. | Webster KE, Feller JA, Kimp A, Devitt BM. Medial meniscal and chondral pathology at the time of revision anterior cruciate ligament reconstruction results in inferior mid-term patient-reported outcomes. Knee Surg Sports Traumatol Arthrosc. 2018;26:1059-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 36. | MARS Group. Meniscal and Articular Cartilage Predictors of Clinical Outcome After Revision Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44:1671-1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 37. | MARS Group. , Wright RW, Huston LJ, Haas AK, Allen CR, Anderson AF, Cooper DE, DeBerardino TM, Dunn WR, Lantz BBA, Mann B, Spindler KP, Stuart MJ, Nwosu SK, Albright JP, Amendola AN, Andrish JT, Annunziata CC, Arciero RA, Bach BR Jr, Baker CL 3rd, Bartolozzi AR, Baumgarten KM, Bechler JR, Berg JH, Bernas GA, Brockmeier SF, Brophy RH, Bush-Joseph CA, Brad Butler V J, Campbell JD, Carey JL, Carpenter JE, Cole BJ, Cooper JM, Cox CL, Creighton RA, Dahm DL, David TS, Flanigan DC, Frederick RW, Ganley TJ, Garofoli EA, Gatt CJ Jr, Gecha SR, Giffin JR, Hame SL, Hannafin JA, Harner CD, Harris NL Jr, Hechtman KS, Hershman EB, Hoellrich RG, Hosea TM, Johnson DC, Johnson TS, Jones MH, Kaeding CC, Kamath GV, Klootwyk TE, Levy BA, Ma CB, Maiers GP 2nd, Marx RG, Matava MJ, Mathien GM, McAllister DR, McCarty EC, McCormack RG, Miller BS, Nissen CW, O'Neill DF, Owens BD, Parker RD, Purnell ML, Ramappa AJ, Rauh MA, Rettig AC, Sekiya JK, Shea KG, Sherman OH, Slauterbeck JR, Smith MV, Spang JT, Svoboda LSJ, Taft TN, Tenuta JJ, Tingstad EM, Vidal AF, Viskontas DG, White RA, Williams JS Jr, Wolcott ML, Wolf BR, York JJ. Predictors of Patient-Reported Outcomes at 2 Years After Revision Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2019;47:2394-2401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 38. | Group M; Mars Group; Wright RW. Effect of Graft Choice on the 6 Year Outcome of Revision Anterior Cruciate Ligament Reconstruction in the Multicenter ACL Revision Study (MARS) Cohort. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 39. | Legnani C, Zini S, Borgo E, Ventura A. Can graft choice affect return to sport following revision anterior cruciate ligament reconstruction surgery? Arch Orthop Trauma Surg. 2016;136:527-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 40. | Grassi A, Nitri M, Moulton SG, Marcheggiani Muccioli GM, Bondi A, Romagnoli M, Zaffagnini S. Does the type of graft affect the outcome of revision anterior cruciate ligament reconstruction? Bone Joint J. 2017;99-B:714-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 41. | Grassi A, Vascellari A, Combi A, Tomaello L, Canata GL, Zaffagnini S; SIGASCOT Sports Committee. Return to sport after ACL reconstruction: a survey between the Italian Society of Knee, Arthroscopy, Sport, Cartilage and Orthopaedic Technologies (SIGASCOT) members. Eur J Orthop Surg Traumatol. 2016;26:509-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |