Published online Aug 18, 2022. doi: 10.5312/wjo.v13.i8.714
Peer-review started: December 27, 2021
First decision: April 12, 2022
Revised: April 24, 2022
Accepted: July 26, 2022
Article in press: July 26, 2022
Published online: August 18, 2022
Processing time: 232 Days and 2.1 Hours
Ankylosing spondylitis at total hip arthroplasty (THA) has significant hip stiffness with flexion deformity, restricted mobility, and function. Range of movement (ROM) improvement with good functional outcome is seen following THA in these hips. The modified Hardinge approach without abductor compromise is helpful in these stiff hips with associated flexion deformity.
To assess improvement in ROM and functional outcomes with a modified lateral approach THA in ankylosing spondylitis with stiff hips.
A total of 69 hips that underwent THA with a modified Hardinge approach in 40 patients were evaluated at a mean follow-up of 38.33 mo. All individuals ambulated with weight-bearing as tolerated and ROM exercises from the 1st postoperative day. Modified Harris hip score and ROM were assessed during follow-up. Quality of life assessments using the 36-item and 12-item short form health surveys were done along with clinical and functional outcomes at follow-up. SPSS 22.0 was used for statistical analysis. The correlation of ROM and functional score change was performed using Pearson’s correlation coefficient.
Sixty-nine hips with a significant decrease in ROM preoperatively with 32 clinically fused hips showed significant improvement in flexion range. The mean flexion in 69 hips improved from 29.35 ± 31.38 degrees to 102.17 ± 10.48 degrees. The mean difference of 72.82 with a P value < 0.0001 was significant. In total, 45 out of 69 hips had flexion deformity, with 13 hips having a deformity above 30 degrees. The flexion during the follow-up was below 90 degrees in 3 hips. Eleven hips had flexion of 90 degrees at follow-up, while the remaining 55 hips had flexion above 100 degrees. Modified Harris hip score improved from 17.03 ± 6.02 to 90.66 ± 7.23 (P value < 0.0001). The 36-item short form health survey at the follow-up indicated health status in 40 patients as excellent in 11, very good in 20, good in 5, fair in 3, and poor in 1. The mean mental health score was 84.10 ± 11.58. Pain relief was good in all 69 hips. Altogether, 28/40 patients (70%) had no pain, 9 patients (22%) had occasional pain, and 3 patients (8%) had mild to moderate pain with unusual activity. Heterotopic ossification was seen in 21 hips with Brooker class 1 in 14 hips.
Modified Hardinge approach THA in ankylosing spondylitis with stiff hips with flexion deformity significantly improved ROM, Harris hip score, and quality of life indicated by the 36-item and 12-item short form health surveys.
Core Tip: Ankylosing spondylitis is characterized by significant hip stiffness with mobility restriction and decreased quality of life. Range of movement is reduced with coexistent flexion deformity. Total hip arthroplasty improves mobility by enhancing the quality of life. The modified Hardinge approach leaves the posterior two-thirds of the abductors intact. This approach is helpful in these hips with flexion deformity with good clinical and functional outcomes. Range of movement, Harris hip score, and quality of life indicated by the 36-item short form health survey score have shown promising results.
- Citation: Jacob MK, Reddy PK, Kuruvilla RS, John CV, Poonnoose PM, Oommen AT. Functional and clinical outcome with modified lateral approach total hip arthroplasty in stiff hips with ankylosing spondylitis. World J Orthop 2022; 13(8): 714-724
- URL: https://www.wjgnet.com/2218-5836/full/v13/i8/714.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i8.714
Ankylosing spondylitis (AS) belongs to the spondyloarthropathy group of disorders affecting the young with progressive stiffness of the spine and hip joints. The hip joint is involved in 25%-50% of patients[1], with bilateral hip disease seen in 50%-90% of AS[2-5]. Disability in these individuals is predominantly due to decreased movement resulting in stiffness restricting their activities. The hip involvement presents varying degrees of stiffness with bony ankylosis seen in about 40% at total hip arthroplasty (THA)[6]. The majority of these young patients have fixed deformities with loss of spinal mobility. THA improves the functional outcome in these patients with significant activity limitations and progressive stiffness in their spine and hips.
THA in these hips significantly improves the range of movement (ROM) and pain relief with marked improvement in function and mobility[4]. However, the associated risks are ectopic bone formation, reduced ROM, and re-ankylosis after THA in AS[6].
We aimed to assess the functional and clinical outcome in AS with stiff hips after THA with the modified lateral approach. ROM and functional outcomes using the modified Harris hip score (HHS), 36-item short-form health survey score (SF-36), and 12-item short form health survey (SF-12) scores were calculated for assessment.
A retrospective analysis of clinically stiff hips with AS who underwent THA in our unit between 2012 to 2018 were included. The criteria for inclusion were individuals over 18 years of age diagnosed with AS with decreased ROM with THA in our unit and had come for follow-up more than 6 mo after the procedure. Based on these criteria, 168 patients fulfilled the criteria for this study. In total, 69 hips in 40 patients who could be assessed clinically during the study period were included in this study. Sixty-two patients with AS were reviewed, and 22 patients had to be excluded due to insufficient data. The remaining were not available for a clinical evaluation during the study period. Data for the 40 patients were collected for clinical review. Information was also obtained from the medical records. Preoperative details regarding ROM, pain, and other data regarding the hip joint involvement were collected and compared with the data obtained at clinical follow-up. SPSS 22.0 was used for statistical analysis. The correlation of ROM and functional score change was done using Pearson’s correlation coefficient.
Data regarding medical management by the rheumatology department was also collected. Informed consent was obtained from all patients. Institutional Review Board approval was obtained for this study.
Sixty-nine hips were stiff, and 32 were clinically fused. Bilateral hip arthritis in 24 individuals had simultaneous THA in the same sitting. Five patients had staged THA for bilateral hip arthritis. Eleven individuals underwent unilateral THA. Two of the senior authors carried out all the THAs. The modified Hardinge approach was used for all the hips[7,8]. The Mallory modification with preservation of the posterior two-thirds of the abductors is the approach routinely utilized in our unit for all THAs except hips with a requirement for posterior or posterosuperior augmentation and reconstruction. The Mallory modification essentially preserves the posterior two-thirds of the gluteus medius rather than detaching the entire abductor in the classical Hardinge approach. The anterior one-third was cut at the musculotendinous junction to enable effective repair at the end of the procedure.
Templating was done preoperatively for all cases to assess the size of the acetabulum and femur. Lateral positioning for THA was challenging in the fused and stiff hips. Circumferential capsular release was done to enable mobilization of the proximal femur and provide complete exposure to the acetabulum. The capsule in these stiff hips was opened anterolateral and released from the entire bony acetabular margin. The capsular tissue was elevated, and the thickened fibrotic tissue interfering with the acetabular preparation was excised.
A femoral neck osteotomy was done in situ for 26 fused hips that could not be dislocated after defining the acetabular margins and the proximal femur with soft tissue release. Care was taken to support the limb on completion of the osteotomy to prevent additional propagation to the calcar region and the acetabular margins. Additional bony resection was done on the neck cut to leave enough calcar for stable femoral component implantation. Acetabulum reaming was done only after defining the margins. Sequential reaming onto the resected neck and head was done after ensuring to avoid eccentric reaming and maintaining the anterior and posterior wall thickness. The residual pulvinar identified the medial wall, and reaming continued gradually to obtain the best fit of the acetabular component.
The acetabulum was cementless in all our cases. Acetabular components in this series were Pinnacle (Depuy, United States) in 34 hips, R3 (Smith and Nephew, United States) in 29 hips, Trident (Stryker, United States) in 2 hips, and Latitud (Meril, India) in 4 hips. Screw fixation was used in 42 hips to augment fixation. The femur was prepared with the limb adducted and externally rotated to accommodate a cementless component in 61 hips, while 8 hips required a cemented fixation for Dorr type C femur. Cementless femur components were Corail (Depuy, United States) in 30 hips, Synergy (Smith and Nephew, United States) in 12 hips, Polarstem (Smith and Nephew, United States) in 13 hips, Latitud (Meril, India) in 4 hips, and Accolade (Stryker, United States) in 2 hips. The 8 cemented femoral implants were C stem (Depuy, United States) in 2 hips, CPCS (Smith and Nephew, United States) in 4 hips, and CPT (Zimmer, Warsaw, United States) in 2 hips. The head size depended on the acetabular component, with a mean head size of 32.92 mm (28 mm in 9 hips, 32 mm in 35 hips, 36 mm in 25 hips).
No constrained or dual mobility liners were used. Copious lavage with saline to remove all the bone debris was done before closure to reduce the chances of heterotopic ossification. A stable calcar cortical split was seen in the proximal femur in 2 hips at THA with the last broach size used, which required wiring for additional stability. Fracture of the greater trochanter was seen at the final reduction in 1 hip, which required stabilization with stainless steel wires.
All patients were given parenteral antibiotics for 48 h and ambulated with weight-bearing as tolerated by the next day after surgery. Deep vein thrombosis prophylaxis with aspirin was given for 6 wk. The patients with stiff hips were initially encouraged prolonged sitting as soon as tolerated to ensure spinal posture and muscle balance and then mobilized actively as mobility restriction was significant before surgery. The patients were ambulated as soon as tolerated with support, which was gradually weaned after 6 wk.
The preoperative and follow-up flexion and total ROM for each hip were compared. The ROM measurement was done with a goniometer. The total ROM for each hip was compared with the total ROM possible at the last follow-up. The improvement in flexion was compared for each hip. The SF-36 and SF-12 scores were calculated to assess the overall quality of life (QOL). Neuromuscular studies or magnetic resonance imaging were not used to assess hip abductors. The modified HHS, ROM, SF-36, and SF-12 scores were used to assess the overall outcome in these patients. The X-rays were evaluated for heterotopic ossification (HO), the presence of any radiolucent lines, lysis in the Charnley acetabular zones, and the Gruen femur zones with the implants.
The mean ± SD was analyzed based on the distribution of HHS and SF-12 and SF-36 scores. The distribution of the HHS, SF-12, and SF-36 were tabulated for all patients. SPSS 22.0 was used for statistical analysis. P value < 0.05 was considered as statistical significance.
There were 69 hips in 40 patients diagnosed as AS with stiff hips that underwent THA at our unit between January 2012 and December 2018 were included in this study. There were 36 males and 4 females with a mean age of 36.6 years (24 to 58). Sixty-nine hips were studied as 24/40 patients (60%) underwent simultaneous bilateral THA.
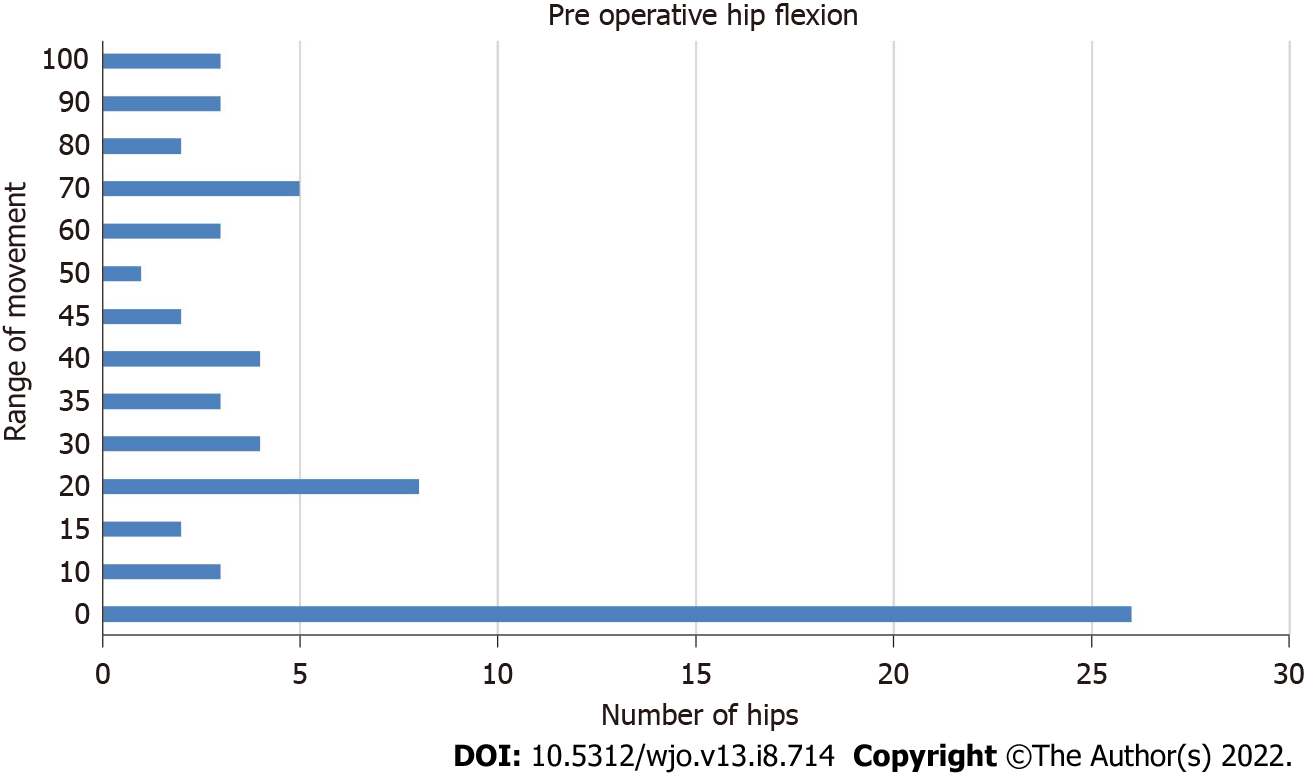
Forty-three hips were found to have preoperative flexion less than 30 degrees (Figure 1). In total, 45/69 hips had flexion deformity, with 13 hips having a deformity above 30 degrees. Three hips had preoperative flexion of 90 degrees, and two hips had preoperative flexion of 100 degrees. Five hips had external rotation deformity of 30 degrees. Significant internal and external rotation restriction was seen in the remaining 64 hips. All hips included had considerable restriction of daily activity with arthritis. The mean preoperative total ROM in 69 hips improved from 45.29 ± 47.20 to a mean of 223.59 ± 27.41. The mean flexion in 69 hips improved from 29.35 ± 31.38 degrees to 102.17 ± 10.48 degrees. The mean difference was 72.97, with a P value < 0.0001 being statistically significant. The total ROM in 32 clinically fused hips improved from a mean of 5.47 ± 9.22 to 223.59 ± 23.33 degrees at the last follow-up.
The flexion at follow-up was below 90 degrees in 3 hips. Eleven hips had flexion of 90 degrees at follow-up, while the remaining 55 hips had flexion above 100 degrees.
The modified HHS improved from 17.03 ± 6.02 to 90.66 ± 7.23 at follow-up. This improvement was found to be statistically significant (P < 0.001). At the follow-up, 30/40 patients had a modified HHS > 90 (Table 1).
| Movement | Preoperative | Follow-up | Mean difference (95%CI) | P value |
| Flexion | 29.35 | 102.17 | 65.76 ± 71.37 | < 0.0001 |
| ROM total | 45.29 | 220.65 | 132.97 ± 171.86 | < 0.0001 |
| ROM score | 1.71 | 4.95 | 3.33 ± 3.18 | < 0.0001 |
| MHHS | 17.03 | 90.66 | 53.84 ± 72.16 | < 0.0001 |
Pain scoring was done as part of the HHS assessment. All 40 patients had pain with restriction of movement for 31.08 ± 36 mo before THA. Pain relief was good in all 69 hips. Altogether, 28/40 patients (70%) had no pain, while 9 patients (22%) had occasional pain without any compromise in activity. Three patients (8%) had mild to moderate pain with unusual activity.
SF-36 is to date the most commonly used health-related QOL measure in research and has been used to assess the health status of AS patients and compared with normal individuals[9-11]. SF-36 focuses on eight domains with physical and mental components with outcome measures indicating the health-related QOL[12]. The responses are assessed in all domains, and the score is generated with higher scores indicating better health. This assessment has been used in the evaluation of patients after THA and total knee arthroplasty[12,13].
The SF-36 measures eight scales that include physical functioning, role limitations due to physical health, bodily pain, general health, vitality, social functioning, role limitations due to emotional problems, and mental health. This used extensively assessment tool is a reliable, detailed measure of overall physical and mental health. The mental health score of 84.10 ± 11.58, along with all other subscores, favored the assessment as an excellent overall outcome (Table 2). The SF-36 questionnaire scores calculated at the follow-up in 40 patients indicated general health as excellent or very good in 31 out of 40 patients (Table 3).
| SF-36 scores | ||
| Mental health | (n = 40) | 84.10 ±11.58 |
| Role limitations due to emotional problems | (n = 40) | 94.17 ± 19.81 |
| Social functioning | (n = 40) | 86.25 ± 16.70 |
| Energy fatigue/vitality | (n = 40) | 71.87 ± 16.63 |
| General health | (n = 40) | 63.12 ± 24.22 |
| Bodily pain | (n = 40) | 80.00 ± 19.23 |
| Physical functioning | (n = 40) | 69.63 ± 18.58 |
| Role limitations due to physical health | (n = 40) | 85.00 ± 33.87 |
| SF-36 scores | Our series | Bahardoust etal[10], 2012 | Dagfinrud etal[9], 2004 | van Tubergen etal[19], 2002 |
| Mental health | 84.10 (11.58) | 39.9 (28.2) | 70 (19) | 65.5 (18.1) |
| Role limitations due to emotional problems | 94.17 (19.81) | 79.1 (19.2) | 66 (42) | 68.5 (41.3) |
| Social functioning | 86.25 (16.70) | 28.5 (29.2) | 70 (27) | 64.6 (24.6) |
| Energy fatigue/vitality | 71.87 (16.63) | 56.2 (21.4) | 43 (23) | 42.6 (16.5) |
| General health | 63.12 (24.22) | 42.1 (26.3) | 51 (24) | 42.8 (20.2) |
| Bodily pain | 80.00 (19.23) | 48.2 (28.4) | 44 (22) | 48.3 (19.2) |
| Physical functioning | 69.63 (18.58) | 28.3 (11.1) | 71 (23) | 55.8 (23.4) |
| Role limitations due to physical health | 85.00 (33.87) | 31.2 (12.6) | 44 (41) | 35.6 (38.1) |
This short form survey instrument used in outcome assessment is quicker with fewer details and two components. The mean physical score of the physical component summary in 40 patients was 45.22 ± 8.94, and the mean score of the mental component summary was 57.63 ± 5.18.
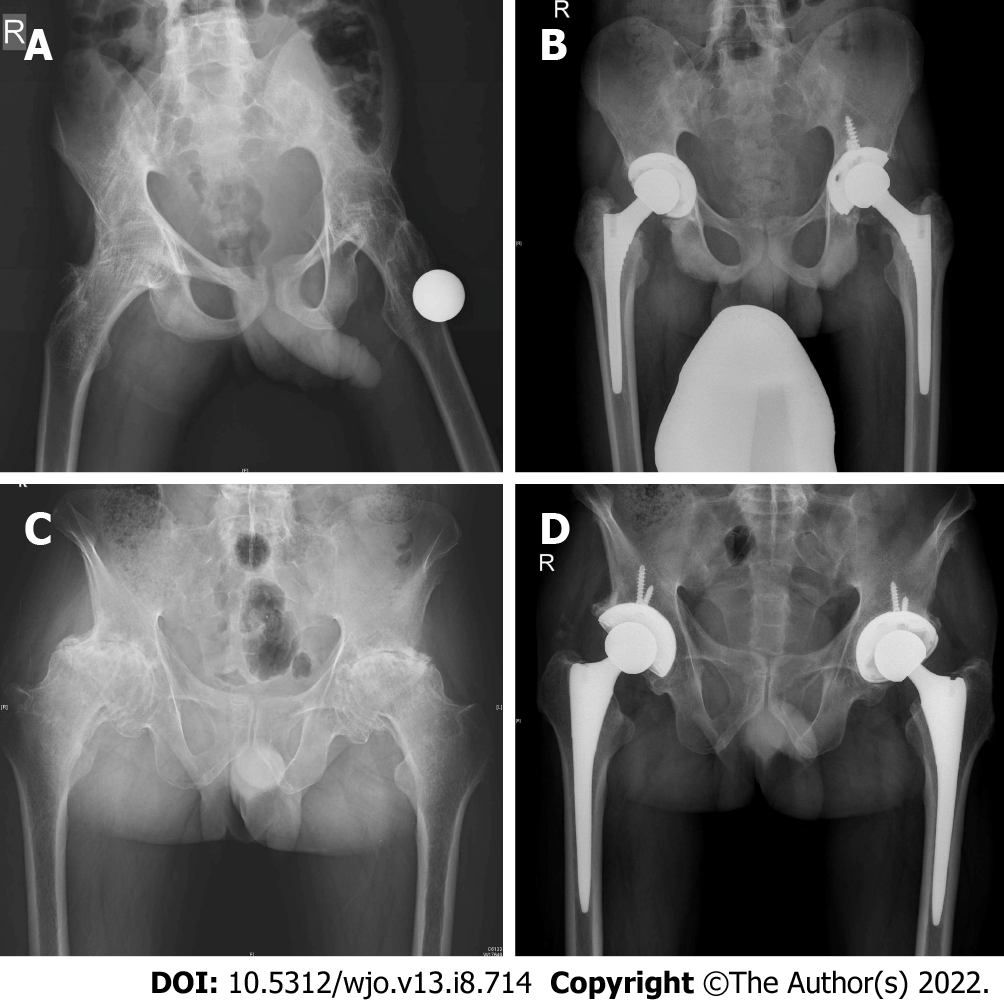
Preoperative assessment included spine as well as hip anteroposterior and lateral views. The anteroposterior view was done in all hips for immediate postoperative assessment. All 69 hips at follow-up showed implants with stable acetabular and femoral components. No radiolucent lines, lysis, or implant loosening was seen in all the Charnley and Gruen zones. HO was seen in 21 hips with Brooker class 1 in 14 hips, class 2 in 5 hips, and class 3 in 2 hips (Figure 2).
There were no dislocations or early infections in our series. One bilateral THA presented 73 mo postoperatively with symptoms suggestive of low-grade infection. He had been on irregular medical treatment and was also diagnosed with chronic venous insufficiency secondary to perforator incompetence in his lower limbs. He underwent a staged revision for his coagulase-negative Staphylococcus infection. There were no other early or delayed complications detected through the last follow-up.
THA effectively relieves pain and improves ROM and function in AS. Five percent of AS patients have been reported to need hip replacement surgery, and the overall rate of joint replacement surgery in AS has increased by 40%[14]. Previous studies have shown and established that AS has a higher male-to-female ratio of about 2:1 to 3:1, and it was evident in this series as 90% of patients were males.
Patients with stiff hips or bony ankylosis have significant functional disabilities. THA brings about dramatic changes in function and QOL in these young patients. The increased hip ROM and subsequent functional improvement in these individuals support THA in this condition.
The Mallory modification of the Hardinge approach is used routinely for THA in our unit. A lateral approach with trochanteric osteotomy has been described[3]. There is a lack of data regarding functional outcomes following THA in AS with fused hips with this approach. There has been a concern with the approach in AS fused hips related to abductor compromise. Hence the posterior approach has been advocated[4]. The modified lateral approach preserves the posterior two-thirds of the abductor and is helpful, especially in stiff hips with flexion deformity, as the approach facilitates the anterior capsular release.
Flexion deformity in the 45 hips was successfully corrected with this modified lateral approach’s extensive soft tissue release. The in situ neck resection in 26 fused hips was performed to prevent damage to the posterior acetabular wall during osteotomy[4]. Limb positioning with external rotation of the femur helps in posterior capsular release between the gluteus medius and the iliopsoas insertions. Femoral broaching and optimal sizing without damage to the residual abductor insertion is facilitated by external rotation of the limb with the modified lateral approach. Femoral anteversion assessment is enabled with proximal femur access provided through this approach. The posterior approach could be challenging for femoral neck osteotomy, especially in fused hips with external rotation deformity. Early mobilization after flexion deformity correction with extensive anterior release in these hips improves ROM and prevents stiffness.
The choice of implant for the acetabulum was based on the bone quality at the time of preparation. Gradual sequential reaming with information obtained from preoperative templating aided in cementless fixation with optimum fit and bone stock utilization in all 69 hips with additional screws when necessary. A cemented femur was used in 8 Dorr C femurs, and cementless components achieved stable fixation in the remaining 61 hips. Increased risk of intraoperative femur fracture would be high if uncemented fixation is attempted with larger sizes to achieve stable fixation in the larger canal with thin cortices. The proximal femur required wiring in 2 hips for medial femur calcar split seen at preparation. Cementless implants in AS have found favor with long-term survivorship in recent series[4] instead of cemented fixation, which was advocated earlier[5].
The average follow-up of patients in our series was 38.33 mo with no evidence of clinical or radiological signs of implant loosening. There were 21 hips with HO seen at follow-up with no functional limitations. Our protocol with copious lavage before closure to remove bone debris and active postoperative mobilization was to reduce the risk of HO. With rheumatology input, the patients were restarted on their disease-modifying antirheumatic drugs 1 wk after THA.
The mean flexion in 69 hips changed from 29.35 ± 31.38 to 102.17 ± 10.48 degrees, indicating a mean improvement of 72.82 degrees. The ROM in 43 hips with flexion less than 30 degrees and 23 fused hips also recorded significant improvement in their flexion at follow-up compared to patients who had preoperative ROM of more than 90 degrees. This significant improvement in ROM in the 69 hips resulted in considerable improvement in the hip function at follow-up.
Modified HHS improved from 17.03 ± 6.02 to 90.66 ± 7.23, which was statistically significant (P < 0.001) as 30/40 patients had a modified HHS > 90 at follow-up. This improvement in HHS is due to the significant increase in the activity levels achieved in these stiff hips. In this study, 92% of our patients had no pain or ignorable pain that did not compromise any activity, and 8% had moderate pain with unusual activity that required occasional analgesics for pain relief.
Thirty-one out of 40 patients showed excellent or good scores in SF-36 and SF-12 physical and mental component analysis, which was comparable with other QOL analyses done in spondyloarthropathy[15]. Improvement in ROM with HHS and SF-36 indicates an overall improvement in the hip joint function and the QOL. Data regarding the functional outcome and health-related QOL after THA in AS has been limited[4,15].
The functional scores and the QOL assessment have been reported in patients with AS[10]. The mental component did not significantly change, and the mean physical component score was significantly lower in the study group[10,16]. The SF-36 scores in this series did not have a preoperative value for comparison. AS patients have significantly impaired QOL, with most domains affected in the SF-36 assessment.
SF-36 at follow-up indicated significant improvement in the QOL after THA in this group of patients with AS. The overall QOL was good in all the domains assessed. The number of cases may have been too small (69 THAs) for analyzing the short-and mid-term effects of THA in AS. However, good scores were obtained in the physical and emotional quotient[17] (Table 3).
The SF-36 scores, which evaluate eight domains used as a functional outcome measure, have added value when used with the modified HHS and the ROM improvement in these stiff hips. SF-12 has a physical and mental component assessment and has fewer elements when compared to SF-36. The SF-36 used to assess functional outcomes in THA and total knee arthroplasty was found to significantly improve following THA[12]. Our series considered the improvement in ROM and the modified HHS. The modified HHS allows evaluation of the hip joints studied, as the HHS allows evaluation of the whole patient. The evaluation of the individual joint deformity and ROM, especially in the bilateral THAs, is possible with the modified HHS. These scores and the SF-36 showed a significant overall improvement in these patients with stiff hips in AS (Table 4).
| Ref. | Patients (hips) | Follow-up in mo | Pain relief, % | Final MHHS | ROM score/mean flexion | Approach | Complications, % |
| Bisla et al[20], 1976 | 23 (34) | 42.5 | 91 | NS | ROM-3 | NS | 5.88 |
| Resnick et al[21], 1976 | 11 (21) | 36 | NS | NS | NS | NS | 0 |
| Williams et al[22], 1977 | 56 (99) | 36 | NS | NS | NS | NS | 10 |
| Baldursson et al[23], 1977 | 10 (18) | 45.6 | 94 | NS | Flexion-90 | NS | 0 |
| Shanahan et al[24], 1982 | 12 (16) | 89 | 94 | NS | NS | NS | 6.25 |
| Finsterbush et al[25], 1988 | 23 (35) | 90 | NS | NS | Flexion-86 | NS | 14.28 |
| Walker et al[26], 1991 | 19 (29) | 58 | 97 | NS | ROM-4 | NS | 0 |
| Gualtieri et al[27], 1992 | 39 (73) | 90 | 89 | NS | NS | NS | 0 |
| Brinker et al[28], 1996 | 12 (20) | 75 | 90 | 89.1 | ROM-4 | Posterior, lateral | 0 |
| Sochart et al[29], 1997 | 24 (43) | 276 | 100 | NS | ROM-4 | NS | 27.9 |
| Lehtimäki et al[30], 2001 | 54 (76) | 240 | NS | NS | NS | NS | 3.94 |
| Joshi et al[31], 2002 | 103 (181) | 120 | 96 | NS | NS | Lateral, Hardinge | 10.5 |
| Kim et al[32], 2007 | 12 (24) | 132 | NS | 82.3 | NS | Lateral | 12.5 |
| Bhan et al[6], 2008 | 54 (92) | 102 | 62 | 82.6 | ROM-4 | Posterior | 14 |
| Li et al[33], 2009 | 24 (39) | 36 | NS | 91 | ROM-4 | Posterolateral | 2.5 |
| Tang et al[2], 2000 | 58 (95) | 135.4 | 94 | 88.8 | ROM-4.2 | Posterior | 20 |
| Bangjian et al[34], 2012 | 12 (24) | 50.4 | 100 | 86.25 | Flexion-84 | Posterolateral | 0 |
| Malhotra et al[35], 2012 | 23 (32) | 42 | NS | 87.1 | ROM-4 | Posterior | 4.7 |
| Siavashi et al[36], 2014 | 77 (NA) | 12 | NS | 88.22 | ROM-5 | Posterior, lateral | 20.8 |
| Xu et al[37], 2017 | 54 (81) | 42 | NS | 86.1 | Flexion-82.5 | Posterolateral | 0 |
| Our series | 40 (69) | 38.33 | 92 | 90.67 | Flexion-102.1739, ROM-4.9514 | Modified Hardinge | 1.4 |
The limitations of this study include a relatively short duration of follow-up and a small number of patients that could be included in this series. The retrospective nature of this study is another limitation. A 5-year follow-up with radiological and clinical outcomes would have been ideal for studying the various outcomes, while our study’s average follow-up was 38.33 mo (range 6-83 mo). We will continue to follow up on these patients to study the clinical, radiological, and overall outcomes. The risk of complications in THA with AS is associated with stiffness of the spine. The possibility of fractures and component loosening are a few complications that could be seen at longer follow-up times[18].
THA with a modified lateral approach in AS with stiff hips has significant improvement in the ROM, HHS, overall function, and QOL as indicated by functional outcome measures with SF-12 and SF-36 scores.
Total hip arthroplasty (THA) with modified lateral approach has been used routinely in our unit for arthritic hips not requiring posterior wall reconstruction. A good exposure of the acetabulum with preservation of the posterior abductors is optimal for hips with flexion deformities.
THA with modified lateral approach is not associated with abductor compromise and results in good functional outcome as seen in individuals coming back for follow-up.
The objective was to have a functional and overall assessment of hips with ankylosing spondylitis at follow-up after THA. Assessment of functional outcome with described tools such as the 36-item and 12-item short form health surveys with the hip scores would provide adequate information.
Patients with ankylosing spondylitis were assessed at follow-up after THA. Functional, clinical, and radiological assessment was done at the follow-up.
The results showed significant improvement in the functional scores in all domains with improvement in range of movement and quality of life.
Modified lateral approach THA in ankylosing spondylitis improves range of movement, function, and quality of life.
Long-term follow-up of 5 years to 10 years with comparison to other approaches would provide a better comparison of the efficacy of the lateral approach.
We would like to acknowledge Dr. Jayaseelan, Ms. Ambily, and Mr. Madhan from the Department of Biostatistics for their expert advice and contribution during the entire process.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhang Y, China S-Editor: Zhang H L-Editor: Filipodia P-Editor: Zhang H
| 1. | Burki V, Gossec L, Payet J, Durnez A, Elhai M, Fabreguet I, Koumakis E, Meyer M, Paternotte S, Roure F, Dougados M. Prevalence and characteristics of hip involvement in spondyloarthritis: a single-centre observational study of 275 patients. Clin Exp Rheumatol. 2012;30:481-486. [PubMed] |
| 2. | Tang WM, Chiu KY. Primary total hip arthroplasty in patients with ankylosing spondylitis. J Arthroplasty. 2000;15:52-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 112] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Hamadouche M, Kerboull L, Meunier A, Courpied JP, Kerboull M. Total hip arthroplasty for the treatment of ankylosed hips: a five to twenty-one-year follow-up study. J Bone Joint Surg Am. 2001;83:992-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 64] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Lin D, Charalambous A, Hanna SA. Bilateral total hip arthroplasty in ankylosing spondylitis: a systematic review. EFORT Open Rev. 2019;4:476-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 5. | Kubiak EN, Moskovich R, Errico TJ, Di Cesare PE. Orthopaedic management of ankylosing spondylitis. J Am Acad Orthop Surg. 2005;13:267-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 73] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Bhan S, Eachempati KK, Malhotra R. Primary cementless total hip arthroplasty for bony ankylosis in patients with ankylosing spondylitis. J Arthroplasty. 2008;23:859-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 83] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | Frndak PA, Mallory TH, Lombardi AV Jr. Translateral surgical approach to the hip. The abductor muscle "split". Clin Orthop Relat Res. 1993;135-141. [PubMed] |
| 8. | Mulliken BD, Rorabeck CH, Bourne RB, Nayak N. A modified direct lateral approach in total hip arthroplasty: a comprehensive review. J Arthroplasty. 1998;13:737-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 100] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Dagfinrud H, Mengshoel AM, Hagen KB, Loge JH, Kvien TK. Health status of patients with ankylosing spondylitis: a comparison with the general population. Ann Rheum Dis. 2004;63:1605-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 116] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 10. | Bahardoust M, Hajializade M, Amiri R, Mousazadeh F, Pisoudeh K. Evaluation of health-related quality of life after total hip arthroplasty: a case-control study in the Iranian population. BMC Musculoskelet Disord. 2019;20:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Yang X, Fan D, Xia Q, Wang M, Zhang X, Li X, Cai G, Wang L, Xin L, Xu S, Pan F. The health-related quality of life of ankylosing spondylitis patients assessed by SF-36: a systematic review and meta-analysis. Qual Life Res. 2016;25:2711-2723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 12. | Lindner M, Nosseir O, Keller-Pliessnig A, Teigelack P, Teufel M, Tagay S. Psychosocial predictors for outcome after total joint arthroplasty: a prospective comparison of hip and knee arthroplasty. BMC Musculoskelet Disord. 2018;19:159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 13. | Mariconda M, Galasso O, Costa GG, Recano P, Cerbasi S. Quality of life and functionality after total hip arthroplasty: a long-term follow-up study. BMC Musculoskelet Disord. 2011;12:222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 14. | Vander Cruyssen B, Muñoz-Gomariz E, Font P, Mulero J, de Vlam K, Boonen A, Vazquez-Mellado J, Flores D, Vastesaeger N, Collantes E; ASPECT-REGISPONSER-RESPONDIA working group. Hip involvement in ankylosing spondylitis: epidemiology and risk factors associated with hip replacement surgery. Rheumatology (Oxford). 2010;49:73-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 126] [Article Influence: 7.9] [Reference Citation Analysis (1)] |
| 15. | Rohde G, Berg KH, Pripp AH, Prøven A, Haugeberg G. No deterioration in health-related quality of life in patients with axial spondyloarthritis followed for 5 years in ordinary outpatient clinics in the biological treatment era. Qual Life Res. 2020;29:99-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Rojanasopondist P, Galea VP, Connelly JW, Matuszak SJ, Rolfson O, Bragdon CR, Malchau H. What Preoperative Factors are Associated With Not Achieving a Minimum Clinically Important Difference After THA? Clin Orthop Relat Res. 2019;477:1301-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 17. | Neuprez A, Neuprez AH, Kaux JF, Kurth W, Daniel C, Thirion T, Huskin JP, Gillet P, Bruyère O, Reginster JY. Total joint replacement improves pain, functional quality of life, and health utilities in patients with late-stage knee and hip osteoarthritis for up to 5 years. Clin Rheumatol. 2020;39:861-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 18. | Blizzard DJ, Penrose CT, Sheets CZ, Seyler TM, Bolognesi MP, Brown CR. Ankylosing Spondylitis Increases Perioperative and Postoperative Complications After Total Hip Arthroplasty. J Arthroplasty. 2017;32:2474-2479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | van Tubergen A, Coenen J, Landewé R, Spoorenberg A, Chorus A, Boonen A, van der Linden S, van der Heijde D. Assessment of fatigue in patients with ankylosing spondylitis: a psychometric analysis. Arthritis Rheum. 2002;47:8-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 125] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 20. | Bisla RS, Ranawat CS, Inglis AE. Total hip replacement in patients with ankylosing spondylitis with involvement of the hip. J Bone Joint Surg Am. 1976;58:233-238. [PubMed] |
| 21. | Resnick D, Dwosh IL, Goergen TG, Shapiro RF, D'Ambrosia R. Clinical and radiographic "reankylosis" following hip surgery in ankylosing spondylitis. AJR Am J Roentgenol. 1976;126:1181-1188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Williams E, Taylor AR, Arden GP, Edwards DH. Arthroplasty of the hip in ankylosing spondylitis. J Bone Joint Surg Br. 1977;59-B:393-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 25] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Baldursson H, Brattström H, Olsson T. Total hip replacement in ankylosing spondylitis. Acta Orthop Scand. 1977;48:499-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Shanahan WR, Kaprove RE, Major PA, Hunter T, Baragar FD. Assessment of longterm benefit of total hip replacement in patients with ankylosing spondylitis. J Rheumatol. 1982;9:101-104. [PubMed] |
| 25. | Finsterbush A, Amir D, Vatashki E, Husseini N. Joint surgery in severe ankylosing spondylitis. Acta Orthop Scand. 1988;59:491-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Walker LG, Sledge CB. Total hip arthroplasty in ankylosing spondylitis. Clin Orthop Relat Res. 1991;198-204. [PubMed] |
| 27. | Gualtieri G, Gualtieri I, Hendriks M, Gagliardi S. Comparison of cemented ceramic and metal-polyethylene coupling hip prostheses in ankylosing spondylitis. Clin Orthop Relat Res. 1992;81-85. [PubMed] |
| 28. | Brinker MR, Rosenberg AG, Kull L, Cox DD. Primary noncemented total hip arthroplasty in patients with ankylosing spondylitis. Clinical and radiographic results at an average follow-up period of 6 years. J Arthroplasty. 1996;11:802-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 43] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Sochart DH, Porter ML. Long-term results of total hip replacement in young patients who had ankylosing spondylitis. Eighteen to thirty-year results with survivorship analysis. J Bone Joint Surg Am. 1997;79:1181-1189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 84] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 30. | Lehtimäki MY, Lehto MU, Kautiainen H, Lehtinen K, Hämäläinen MM. Charnley total hip arthroplasty in ankylosing spondylitis: survivorship analysis of 76 patients followed for 8-28 years. Acta Orthop Scand. 2001;72:233-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 31. | Joshi AB, Markovic L, Hardinge K, Murphy JC. Total hip arthroplasty in ankylosing spondylitis: an analysis of 181 hips. J Arthroplasty. 2002;17:427-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 81] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 32. | Kim YL, Shin SI, Nam KW, Yoo JJ, Kim YM, Kim HJ. Total hip arthroplasty for bilaterally ankylosed hips. J Arthroplasty. 2007;22:1037-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Li J, Xu W, Xu L, Liang Z. Hip resurfacing arthroplasty for ankylosing spondylitis. J Arthroplasty. 2009;24:1285-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 34. | Bangjian H, Peijian T, Ju L. Bilateral synchronous total hip arthroplasty for ankylosed hips. Int Orthop. 2012;36:697-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 35. | Malhotra R, Kannan A, Kumar V, Nagaraj C, Marimuthu K, Khatri D. Hip resurfacing arthroplasty in inflammatory arthritis a 3- to 5-year follow-up study. J Arthroplasty. 2012;27:15-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Siavashi B, Mohseni N, Zehtab MJ, Ramim T. Clinical outcomes of total hip arthroplasty in patients with ankylosed hip. Arch Bone Jt Surg. 2014;2:25-30. [PubMed] |
| 37. | Xu J, Zeng M, Xie J, Wen T, Hu Y. Cementless total hip arthroplasty in patients with ankylosing spondylitis: A retrospective observational study. Medicine (Baltimore). 2017;96:e5813. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |