Published online Jul 18, 2022. doi: 10.5312/wjo.v13.i7.662
Peer-review started: December 27, 2021
First decision: April 6, 2022
Revised: April 13, 2022
Accepted: July 11, 2022
Article in press: July 11, 2022
Published online: July 18, 2022
Processing time: 202 Days and 8.3 Hours
Anterior cruciate ligament (ACL) reconstruction has been a successful treatment for ACL rupture. However ongoing rotational instability can be an issue. Several surgical techniques have been recommended to overcome this including lateral extra-articular tenodesis (LET) and more recently anterolateral ligament reconstruction (ALLR).
To compare the clinical outcomes following ACL reconstruction (ACLR) alone or ACLR with either LET or ALLR.
A systematic review was conducted by means of four databases (MEDLINE, EMBASE, Cochrane and Clinical.Trials.Gov), and the Reference Citaion Analysis (https://www.referencecitationanalysis.com/) to identify all studies investigating either or both of LET and ALLR. The Critical Appraisal Skills Programme checklist for cohort studies was employed for critical appraisal and evaluation of all twenty-four studies which met the inclusion criteria.
Pooled meta-analyses illustrated that ACLR with additional LET or ALLR results in improved pivot shift test scores, compared to isolated ACLR. There was no statistically significant difference in International Knee Documentation Commi
This meta-analysis has found that use of either LET or ALLR in addition to ACLR results in improved mechanical outcomes suggesting surgeons should consider augmenting ACLR with an extra-articular procedure in patients with rotatory instability. Furthermore, both anterolateral extra articular procedures in addition to ACLR lead to reduced ACL re-rupture rates compared to isolated ACLR. Moreover, ALLR results in reduced ACL re-rupture rates, compared to LET. More research is needed to compare the two respective extra-articular procedures.
Core Tip: Either lateral extra-articular tenodesis (LET) or anterolateral ligament reconstruction (ALLR) should be utilized with anterior cruciate ligament (ACL) reconstruction (ACLR) in patients with rotational instability, to confer greater stability. Either technique, together with ACLR, leads to superior mechanical outcomes, in comparison to ACLR alone. Both techniques reduce risk of ACL re-rupture, compared to isolated ACLR, with ALLR having lower rates than LET.
- Citation: Agarwal N, Monketh J, Volpin A. Clinical and mechanical outcomes in isolated anterior cruciate ligament reconstruction vs additional lateral extra-articular tenodesis or anterolateral ligament reconstruction. World J Orthop 2022; 13(7): 662-675
- URL: https://www.wjgnet.com/2218-5836/full/v13/i7/662.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i7.662
Rupture of the anterior cruciate ligament (ACL) is one of the most common sporting injuries affecting the knee joint. In the United Kingdom, the National Ligament Registry has noted over 15304 cases of ACL rupture between 2012 and 2019[1].
Those with symptomatic instability have traditionally been treated with arthroscopic ACL reconstruction (ACLR). Numerous studies demonstrate excellent short term functional outcomes however some questions remain regarding this treatment[2,3]. ACLR has demonstrated to be effective in restoring translational stability, however the capacity to restore rotational stability is limited[4,5]. Patient reported outcome measures tend to correlate with improvements in translational rather than rotational stability. Moreover, rotational instability has been implicated in the development of knee osteoarthritis. Despite technical improvements, such as single or double bundle reconstructions and more accurate tunnel placement, the rates of positive pivot-shift test remain unacceptably high.
The role of the anterolateral soft tissue restraints (including the anterolateral ligament (ALL)) in rotational stability are increasingly being recognized[6,7]. Historically, several anterolateral extra articular procedures (AEAP) had been developed to tackle anterolateral instability, including lateral extra-articular tenodesis (LET), originally described by Lemaire[8]. There is conflicting evidence in the literature surrounding LET. Some studies have shown that LET provides no additional benefit when performed in combination with ACLR, compared to isolated ACLR[9,10]. Other studies have found that in high-risk patients, such as those with additional laxity, LET results in reduced graft rupture and reduces rotatory laxity[11,12]. More recently, with the newfound understanding of biomechanics and anatomy, another procedure, anterolateral ligament reconstruction (ALLR) has been developed. Biomechanical studies have shown variable restoration of knee kinematics in addition to concerns that the technique may lead to over constraint of the lateral compartment; thus, actually accelerating degenerative changes[13,14].
The aim of this systematic review and meta-analysis was to firstly compare the clinical effectiveness of ACLR combined with LET or ALLR, to ACLR alone. Secondly, to compare the clinical and mechanical outcomes of the two AEAPs discussed.
A systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRSIMA) was conducted[15]. Using the PICO model, inclusion and exclusion criteria were set[16]. Only randomized control trials (RCTs) cohort, cross-sectional studies and case control studies were included. Reviews, conference abstracts, case series, case reports and editorials were excluded. Only studies which investigated either ACL reconstruction with additional ALLR or LET were included. Studies which investigated revision ACLR were excluded. The references of the final studies were checked for any additional studies that would meet the inclusion criteria.
A literature search was carried out by A. N. Four databases were searched for studies which were relevant to this systematic review: MEDLINE (2000 to Week 4 November 2021), EMBASE (2000 to 29 November 2021), Cochrane library (2000 to November 2021) and clinical trials.gov (2000 to November 2021). The Reference Citaion Analysis (https://www.referencecitationanalysis.com/) software was also utilized to identify any additional studies.
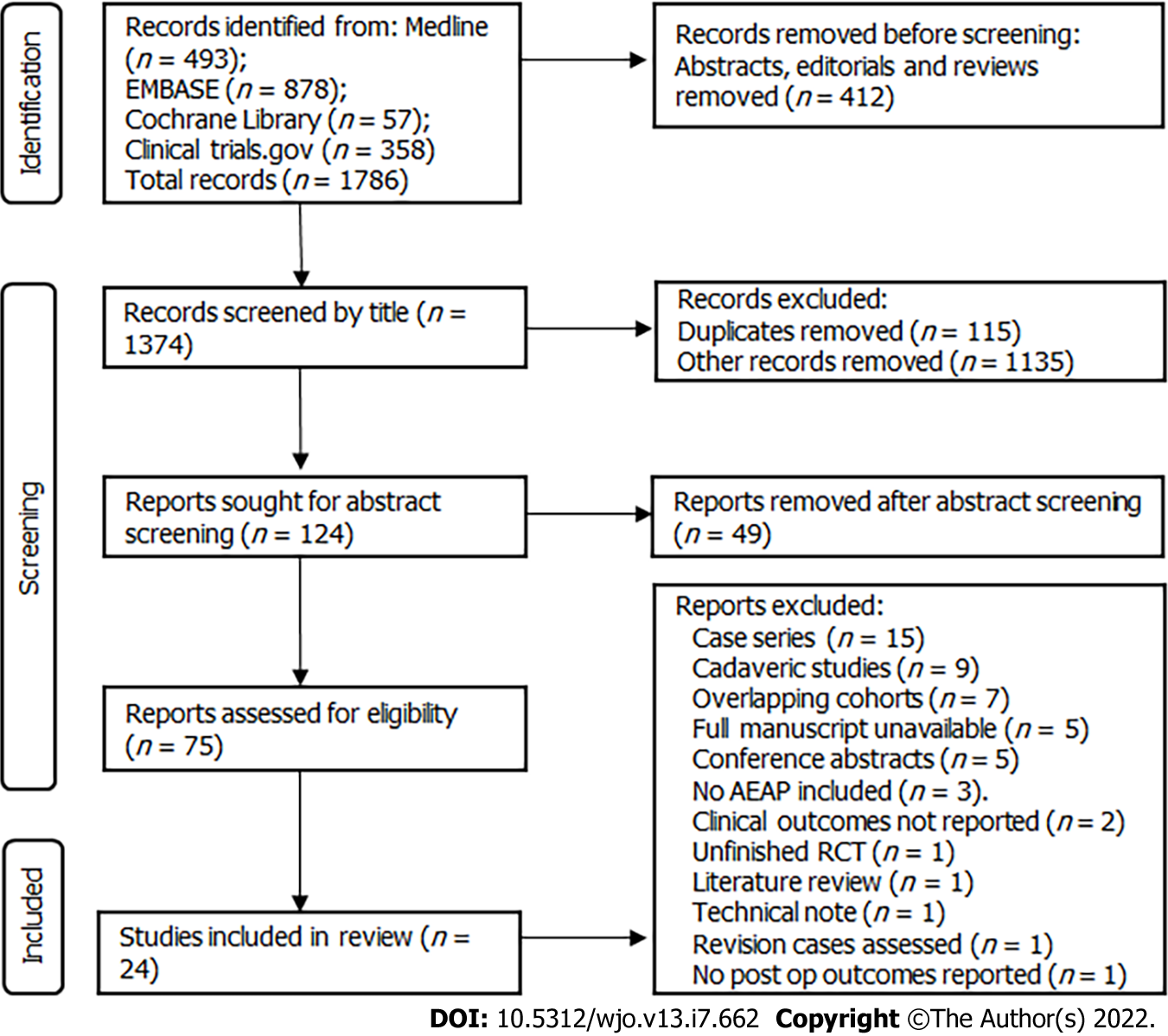
A comprehensive strategy was developed, upon which the databases were searched. This was designed on the basis of the guidelines provided by the Cochrane Highly Sensitive Search Strategy[17]. This included but was not restricted to the following MeSH terms: “Anterior Cruciate Ligament”, or “tenodesis” or “iliotibial band” or “extra articular” and “reconstruction” or “Anterior Cruciate Ligament Reconstruction”. Full MeSH terms used can be found in Appendix 1 (Supplementary material). Only in vivo studies were included. In addition, it was decided that only studies from 2000 onwards should be included, since studies before this time could be considered outdated, considering the novel developments in orthopaedic surgery. The authors only wanted to examine novel techniques which are currently in use in clinical practice. The overall results of the comprehensive search are shown in Figure 1. The structure of this table was incorporated from Page et al[18].
All studies included in this review were independently appraised by two authors A. N and J. M. The critical appraisal was conducted by the Critical Appraisal Skills Programme (CASP) checklists for randomized controlled trials, cohort studies and case control studies[19]. The appraisals for each RCT can be found in Table 1 and appraisals for cohort studies can be found in Table 2. One study was of case control study design. This was assessed accordingly by the CASP checklist for case control studies. The questions in each of the checklists are listed in Appendix 2 (Supplementary material). Any disagree
| Ref. | Q1 | Q2 | Q3 | Q4a | Q4b | Q4c | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 |
| Chiba et al[23] | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Getgood et al[12] | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hamido et al[39] | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Ibrahim et al[40] | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Mogoş et al[24] | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Porter et al[41] | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Sonnery-Cottet et al[25] | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Stensbirk et al[42] | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Trichine et al[43] | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Vadalà et al[44] | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Ref. | Q1 | Q2 | Q3 | Q4 | Q5a | Q5b | Q6a | Q6b | Q9 | Q10 | Q11 |
| Ahn et al[45] | Yes | Yes | Yes | Yes | No | Can’t tell | Yes | Yes | Yes | Yes | Yes |
| Dejour et al[46] | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | No | Yes | Yes | Yes |
| Erden et al[47] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Ferretti et al[33] | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Giraud et al[48] | Yes | Yes | Yes | Yes | No | Can’t tell | Yes | No | Yes | Yes | Yes |
| Goncharov et al[49] | Yes | Yes | Yes | Yes | No | No | Yes | No | Yes | Yes | Yes |
| Lee et al[50] | Yes | Yes | Yes | Yes | Yes | Can’t tell | Yes | No | Yes | Yes | Yes |
| Mahmoud et al[11] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Rowan et al[51] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Sonnery-Cottet et al[52] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Sonnery-Cottet et al[53] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Sonnery-Cottet et al[36] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Ventura et al[54] | Yes | Yes | Yes | Yes | No | Can’t tell | Yes | Yes | Yes | Yes | Yes |
The following study characteristics were extracted from each study after full text analysis: study design, number of patients included in the study, country of origin, mean follow up time, type of AEAP investigated, outcomes measured, and year published.
All statistical analysis was conducted using JASP (version 0.16, University of Amsterdam). A restricted maximum likelihood random effects model was used to generate a pooled estimate of the odds ratio of an “event” for analysis of post-operative pivot shift test and International Knee Documentation Committee (IKDC) score. I2 test was used as a measure of between study heterogeneity. The pivot shift test is a validated tool to assess rotatory instability, is highly sensitive and specific for ACL rupture and the presence of a positive results does correlate well with clinical outcomes[20]. The IKDC score has also been shown to have a high criterion validity in assessment of treatment outcome and is widely used[21]. As these two measures could be recorded as categorical variables they were selected for meta-analysis. For the purpose of the analysis and in line with previous published literature we considered a pivot shift test grades 1, 2 or 3 was defined as an event[22]. For the IKDC score an overall grade C (abnormal) or D (severely abnormal) was considered an event. Statistical analysis on categorical data was performed using cross tabulation and Chi squared testing for categorical data, or Fisher’s exact test if the sample size did not permit Chi Squared testing. A P value of < 0.05 was considered statistically significant.
Table 3 displays the study characteristics of all 24 studies encompassed in this review. Most studies were cohort studies, with 6 retrospective, 5 prospective and 2 matched cohort studies (n = 2). Ten studies were RCTs. One study was a case control study.
| Study characteristic | n(%) |
| Study design | |
| Randomised controlled trial | 10 (42) |
| Prospective cohort study | 5 (21) |
| Retrospective cohort study | 6 (25) |
| Matched cohort study | 2 (8) |
| Case control study | 1 (4) |
| Country of origin | |
| France | 6 (25) |
| Italy | 4 (17) |
| Australia | 2 (8) |
| South Korea | 2 (8) |
| United States | 1 (4) |
| Kuwait | 2 (8) |
| Turkey | 1 (4) |
| United Kingdom | 1 (4) |
| Brazil | 1 (4) |
| Russia | 1 (4) |
| Canada | 1 (4) |
| Denmark | 1 (4) |
| Algeria | 1 (4) |
| Year published | |
| 2006 | 1 (4) |
| 2012 | 1 (4) |
| 2013 | 1 (4) |
| 2014 | 2 (8) |
| 2016 | 1 (4) |
| 2017 | 2 (8) |
| 2018 | 1 (8) |
| 2019 | 4 (17) |
| 2020 | 4 (17) |
| 2021 | 7 (29) |
| Number of patients | |
| < 50 | 2 (8) |
| 50-100 | 10 (42) |
| 100-250 | 8 (33) |
| 250-500 | 2 (8) |
| > 500 | 2 (8) |
| Mean follow-up time | |
| 1-12 mo | 2 (8) |
| 13 -24 mo | 6 (25) |
| 25-36 mo | 4 (17) |
| 37-60 mo | 7 (29) |
| 61-120 mo | 4 (17) |
| > 120 mo | 1 (4) |
| Type of AEAP | |
| LET | 13 (54) |
| ALLR | 11 (46) |
Thirteen studies compared ACLR to ACLR + LET. The remaining 11 were studies which compared ACLR to ACLR + ALLR.
The most common range of follow up times was 37-60 mo (n = 7). Six studies had a follow up time between 13 and 24 mo. Only 5 of studies used follow up times greater than 60 mo. Thirteen of the studies included in this review, had a follow up duration time less than 37 mo.
Upon critical appraisal of the studies included in this review, using the appropriate CASP tools, it was established that very few RCTs included in this review were blinded. This was however, recognized by most studies, who considered it unfeasible to blind the patients, and impractical to blind the surgeons. Some of the cohort studies included in this review did not account for or did not mention confounding variables, which could have led to unforeseen biases. Three of the studies also were deemed to have short follow up (< 24 mo). While it was recognized the reliably of the meta-analysis would be improved by only including studies with longer follow up (> 24 mo), it was the consensus of the authors that the large number of patients and the overall quality of the studies meant the data present in these three studies would add robustness to the meta-analysis as such they were included[23-25]. Overall, the quality of all studies included in this review was high. Tables 1 and 2 demonstrate the full methodological quality assessment of the included studies.
Table 4 summarizes the main characteristics of all the studies included in this systematic review.
| Ref. | Design of study | AEAP used | Number of patients involved | Mean follow up | Outcome measures used | Technique favoured |
| Ahn et al[45] | Retrospective cohort study | LET | 171 | 49.7 ± 5.7 mo | IKDC, KL grade, graft maturation score and revision rates | ACLR with LET favoured over ACLR alone |
| Chiba et al[23] | RCT | LET | 18 | 12 mo | Anterior tibial translation, KOOS, tibial rotation relative to the femur | ACLR with LET is not superior to ACLR alone |
| Dejour et al[46] | Prospective cohort study | LET | 75 | 25 mo | Anterior tibial translation, IKDC, pivot shift grading | ACLR with LET favoured over ACLR alone |
| Erden et al[47] | Retrospective cohort study | ALLR | 63 | 24 mo | Cincinnati knee score, IKDC, Lysholm scores, graft rupture rate, anterior tibial translation, pivot shift test | ACLR with ALLR is not superior to ACLR alone |
| Ferretti et al[33] | Retrospective cohort study | LET | 140 | 120 mo | Lysholm score, IKDC, Tegner score, anterior tibial translation | ACLR with LET favoured over ACLR alone |
| Getgood et al[12] | RCT | LET | 618 | 24 mo | P4, KOOS, Marx Activity Rating scale, IKDC, ACL QOL | ACLR with LET favoured over ACLR alone |
| Giraud et al[48] | Prospective cohort study | LET | 63 | 84 mo | IKDC, anterior tibial translation, radiological medial and lateral compartment laxity | ACLR with LET is not superior to ACLR alone |
| Goncharov et al[49] | Prospective cohort study | ALLR | 50 | 24 mo | Tegner Lysholm score, IKDC, Lachmann test, Pivot shift test | ACLR with ALLR is not superior to ACLR alone |
| Hamido et al[39] | RCT | ALLR | 107 | 60 mo | IKDC, anterior tibial translation, Tegner score, Lysholm score | ACLR with ALLR favoured over ACLR alone |
| Helito et al[55] | Case control study | ALLR | 90 | 29.6 ± 6.2 mo for group 1; 28.1 ± mo for group 2 | Anterior tibial translation, IKDC, Lysholm, Tegner score Pivot shift test, rupture rates | ACLR with ALLR favoured over ACLR alone |
| Ibrahim et al[40] | RCT | ALLR | 103 | 27 mo | Anterior tibial translation, IKDC, Lysholm score, Tegner score, Pivot shift test | ACLR with ALLR is not superior to ACLR alone |
| Lee et al[50] | Retrospective cohort study | ALLR | 87 | 36 mo | ACL-RSI, Anterior tibial translation, IKDC, Lysholm score, Tegner score | ACLR with ALLR is not superior to ACLR alone |
| Mahmoud et al[11] | Matched cohort study | LET | 144 | 120 mo | IKDC, Lysholm score, OKS, Tegner score | ACLR with LET favoured over ACLR alone |
| Mogoş et al[24] | RCT | ALLR | 57 | 12 mo | IKDC, Lysholm score, Pivot shift test, Rolimeter test, Tegner score | ACLR with ALLR favoured over ACLR alone |
| Porter et al[41] | RCT | LET | 55 | 24 mo | IKDC, Lysholm score, KOOS, Tegner score | ACLR with LET favoured over ACLR alone |
| Rowan et al[51] | Prospective cohort study | LET | 273 | 52 mo | Lysholm score, Tegner score | ACLR with LET favoured over ACLR alone |
| Sonnery-Cottet et al[52] | Prospective cohort study | ALLR | 502 | 38.4 ± 8.5 mo | IKDC, Lysholm score, Side to side laxity, Tegner score | ACLR with ALLR favoured over ACLR alone |
| Sonnery-Cottet et al[53] | Retrospective cohort study | ALLR | 383 | 37.4 mo | Lysholm score, Side to side laxity, Tegner score | ACLR with ALLR favoured over ACLR alone |
| Sonnery-Cottet et al[25] | RCT | ALLR | 224 | 12.3 ± 1.9 mo | IKDC, Lysholm score, KOOS, Range of motion, Tegner score | ACLR with ALLR favoured over ACLR alone |
| Sonnery-Cottet et al[36] | Matched cohort study | ALLR | 172 | 104.33 ± 3.74 mo | IKDC, Lysholm score, KOOS, Side to side laxity, Tegner score | ACLR with ALLR favoured over ACLR alone |
| Stensbirk et al[42] | RCT | LET | 60 | 180 mo | AKP questionnaire, Lysholm score, Tegner score | ACLR with LET is not superior to ACLR alone |
| Trichine et al[43] | Single blinded RCT | LET | 120 | 24 mo | IKDC, Objective laxity | Inconclusive |
| Vadalà et al[44] | RCT | LET | 60 | 44.6 mo | Anterior tibial translation, IKDC, Lysholm score, Tegner score, VAS | ACLR with LET favoured over ACLR only |
| Ventura et al[54] | Retrospective cohort study | LET | 24 | 54 mo | Anterior tibial translation, IKDC, Lysholm score, Tegner score | ACLR with LET favoured over ACLR alone |
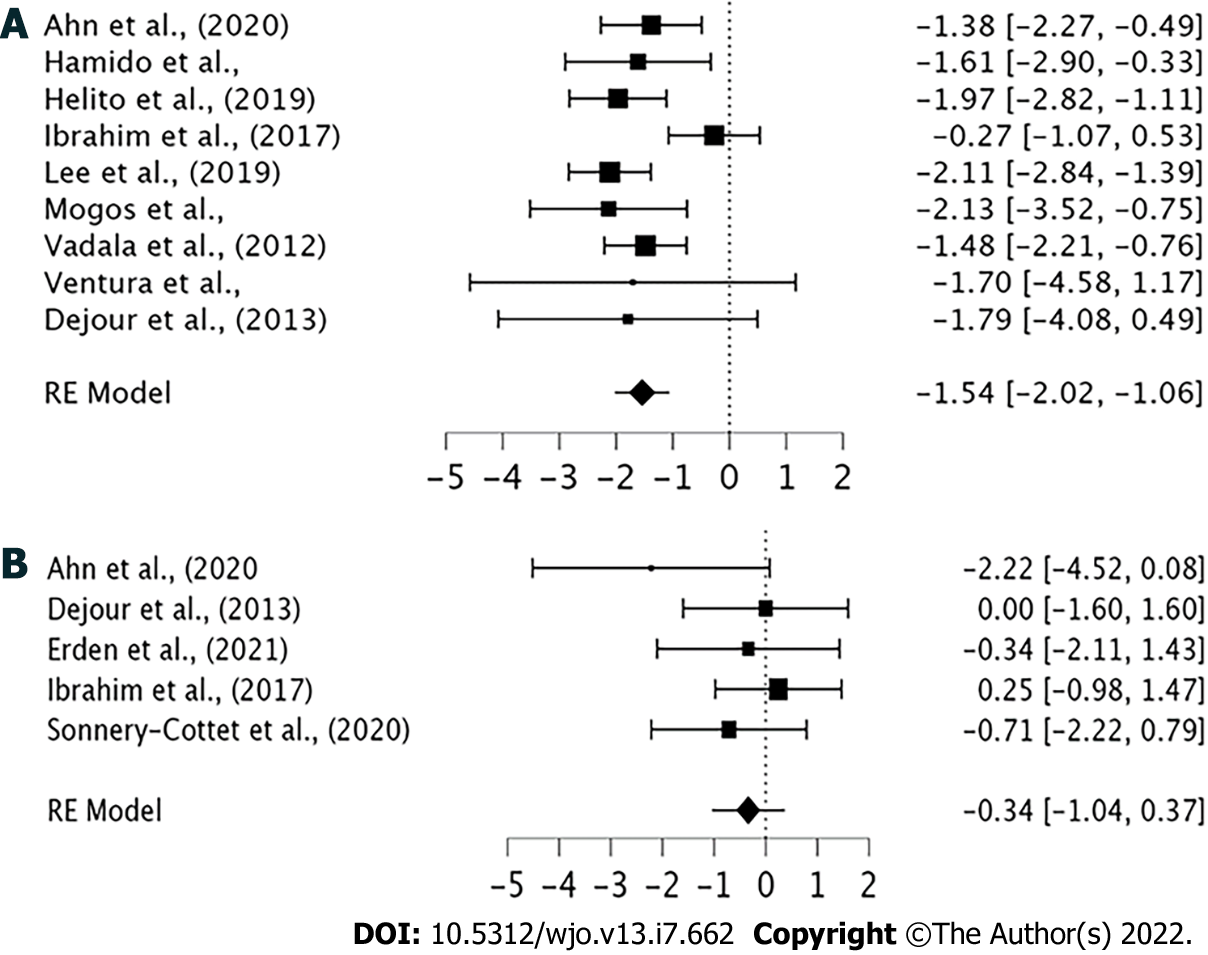
Forest plots were created to analyze clinical and mechanical outcomes most utilized by all studies in ACLR only patient groups vs ACLR + AEAP patient groups (Figure 2).
Figure 2A shows analysis of all nine studies which used pivot shift test scores to analyze mechanical outcomes in ACLR only patient groups vs ACLR + AEAP patient groups. The nine studies that could be used in analysis encompassed 961 knees. Six of the nine studies demonstrated a statistically significant difference in pivot shift test scores between ACLR only patient groups and ACLR + AEAP patient groups. The pooled estimates of odds ratio were -1.54 (95%CI -2.02 to -1.06, P < 0.001) in favor of ACLR + AEAP. This suggests that the addition of AEAP to ACLR results in statistically significantly better pivot shift test scores and therefore greater rotational stability.
Comparison of clinical outcomes between ACLR only and ACLR + AEAP patient groups was conducted using IKDC scores. Five studies were eligible for pooled analysis, which encompassed 878 knees (Figure 2B). There was no statistically significant difference in IKDC scores between the ACLR only and ACLR + AEAP patient groups in any of the five studies. The pooled estimates of log ratio were -0.34 (95%CI -1.04 to 0.37). This demonstrated that the addition of AEAP to ACLR did not result in any statistically significant improvement in IKDC clinical scores (Z = -0.938, P = 0.348).
Following statistical analysis of ACLR alone vs ACLR + AEAP, analysis was then conducted to determine whether there was a difference in clinical and mechanical outcomes between the two AEAPs included: LET and ALLR. The chi squared test was performed which demonstrated that there was no statistically significant difference in pivot shift tests between ACLR + LET and ACLR + ALLR groups (P = 0.39). The chi squared test also showed that there was no statistically significant difference in IKDC scores between ACLR + LET and ACLR + ALLR groups (P = 0.90). This indicates that there are no differences in rotational stability or clinical outcomes with regards to the specific AEAP (LET or ALLR) utilized with ACLR.
ACL re rupture rates were also compared between ACLR + LET and ACLR + ALLR techniques. There was a statistically significant difference between techniques, with a 1.14% re rupture rate in ACLR + ALLR, and 4.03% re rupture rate in ACLR + LET (P = 0.015). This indicated that ACL re-rupture rates were higher in ACLR + LET compared ACLR + ALLR. The re-rupture rate for ACLR alone across all studies was 12.59%, significantly higher than when augmented with either ALLR or LET (P < 0.0001 for both groups).
ACLR has shown excellent results in restoring translational stability. The capacity to restore rotational stability, however, remains an issue. This review has focused on the clinical and mechanical outcomes which follow treatment of primary ACL injuries with AEAPs, in addition to ACLR. The supplementation of an AEAP does appear to improve mechanical outcomes compared to ACLR alone. This suggests that patients with rotatory instability should be offered an AEAP with the ACLR reconstruction. However, there appears to be no difference in mechanical outcomes between AEAPs, which suggests that either LET or ALLR can be used with ACLR to reduce rotational instability. Our results did not show any benefits in clinical outcomes with the addition of AEAP to ACLR. An important consideration to note is that, since we have demonstrated there may not necessarily be direct clinical benefit in all patients, the challenge will be to identify patients where the risk-benefit analysis would favour AEAP. Both LET and ALLR can cause issue over constraint with poor graft placement which may worsen patient outcomes.
The most common mechanical outcome measured in the studies included in this review was the pivot shift test scores. Other mechanical outcomes investigated by studies included; KT 1000/-2000 arthrometry side to side laxity, anterior tibial translation, Lachmann test, Rolimeter test scores and radiological medial and lateral compartment laxities. Analysis of instability using the latter techniques mentioned was not conducted due to the inconsistent use of these scoring systems between studies, and the small number of studies which employed each. The combined analyses of pivot shift test scores demonstrated that use of AEAP in addition to ACLR results in better pivot shift test scores, compared to ACLR alone. However, upon comparison of the ACLR + LET vs ACLR + ALLR there is no statistically significant difference in mechanical outcomes between these two groups. This suggests that though ACLR + AEAPs confers greater rotational stability than ACLR alone, neither technique confers more rotational stability than the other.
Studies have shown that poorer pivot shift test scores correlate to poorer clinical outcomes and patient satisfaction following ACLR[26,27]. Moreover, recent cadaveric studies have demonstrated that ACLR alone does not restore normal knee kinematics, and that an AEAP is required to restore anterior tibial translation and tibiofemoral motion[28,29].
The most common clinical outcome utilized by studies was IKDC scores. Other clinical scores used were: Lysholm score, Tegner score, KOOS score and Cincinnati knee score. Analysis of clinical outcomes, using these latter scoring systems was not conducted due to the small number of studies which employed each one. The pooled analyses of the IKDC scores demonstrated that use of an AEAP with ACLR does not result in any statistical improvements in outcomes. There are several possibilities for this. There may be a ceiling effect to IKDC score making it insensitive in detecting improvements in rotatory stability. We also utilized overall scores and dichotomized the outcomes; this may have also reduced the sensitivity of the analysis.
When directly comparing ALLR with LET, re-rupture rates were higher with LET (1.14% vs 4.03%, P = 0.015). The re-rupture rate for ACLR alone across all studies was 12.59%, significantly higher than when augmented with either ALLR or LET (P < 0.0001 for both groups). Studies that evaluated ACLR + LET were then compared with studies which assessed ACLR + ALLR. Direct analysis shows that ACL re-rupture rates were higher in ACLR + LET than with ACLR + ALLR. This suggests that LET techniques have a higher ACL re rupture rate. However, existing literature suggests that ACL re-rupture rates are higher in ACLR alone compared with ACLR with AEAPs. A study conducted by Marom et al[30], found that the addition of LET to ACLR reduces stress on the graft, by transferring loads to the LET. In addition, this reduces anterior tibial translation when pivoting loads are applied[30]. The reduced strain on the graft would explain why AEAPs lead to reduced re-rupture rates.
There were no studies in the literature which directly compared LET with ALLR. This is understandable given the recent growing interest in ALLR. Certainly, randomized controlled trials are required to assess the two techniques. As ALLR becomes more common practice in the future this will likely become feasible. Ra et al[31] did compare the studies using ACLR + LET with ACLR + ALLR in 2020. Their meta-analysis of non-comparative could not demonstrate a significant difference in rotational stability between ALLR and LET.
There are risks associated with LET procedure. LET is a non-anatomical reconstructive procedure potentially giving it inherent disadvantages over ALLR. While there is evidence to suggest it does help restore normal knee kinematics following ACL injury, there are concerns in the literature that the knee may become over constrained[28,32]. Biomechanical studies have investigated the effects of over constraining[28,32]. Several studies reporting on LET have recommended the graft be fixed with the knee in extension. This could interfere with the “screw home” mechanism of the knee by acting as a restraint to tibial internal rotation[28]. Tibiofemoral contact pressures could increase, thus accelerating the development of osteoarthritis. In addition, this would increase tensile forces the knee is subjected to through the action of the extensor mechanism, potentially increasing the risk of graft rupture. This could explain why our date shows increased risk of graft rupture in LET compared to ALLR. However, these same studies have noted that if the graft is tensioned in neutral, risk of overstraining decreases and there is little risk of accelerated osteoarthritis[28,32]. The study by Ferretti et al[33] demonstrated that at a 10 year follow up, ACLR with LET did not result in increased osteoarthritic rates. This perhaps underscores the importance of sound surgical technique, as more experience is gained with LET, we may see improved outcomes with respect to over constraining of the lateral compartment. Longer term follow-up studies are needed to examine the risk of osteoarthritis further.
Similar concerns have been voiced for ALLR techniques. A recent cadaveric study demonstrated that over constraining is possible with ALLR[34]. A separate study by Neri et al[35] illustrated that ALLR does not lead to increased contact pressures in the lateral compartment. Sonnery-Cottet et al[36] commented that they considered the reason that ALLR avoids over constraint is because the grafts are fixed such that they behave an isometrically. In their technique they identify an isometric point close to the lateral femoral condyle. This point is drilled in an outside-in technique. The tunnel is used for both the ACL reconstruction and ALLR. Once the ACL reconstruction is completed the remaining strand of the graft is used to complete the ALLR by tunnelling it under the ilio-tibial band but superficial to the fibular collateral ligament. The graft is then passed though the tibial tunnel and then brought back proximally towards the femur. This creates an inverted Y shaped acting as a double bundle graft. Whether this behaves isometrically has yet to be proven.
LET is also associated with donor site cosmesis problems[37,38]. It is possible this can be overcome with new minimally invasive techniques which involve tunnelling the grafts deeper.
The strengths of this review include the breadth of studies included. Studies from 13 countries were included in this review. Multiple languages were included, meaning we were less likely to miss relevant datasets. To the best of our knowledge this first meta-analysis to include randomized control studies and case-control studies ALLR with ACLR and the largest to include ALLR.
There were limitations to this review. There was significant heterogeneity amongst the studies included in this review, and thus several studies could not be included in the pooled analysis. This is a common problem encountered when attempting to conduct a meta-analysis. Moreover, there was a wide variation in the techniques used for each procedure of ACLR, ALLR and LET. Regarding extra articular procedures, no consensus has been reached regarding the optimal graft type, location of fixation or the fixation angle.
Another limitation was that only studies conducted after 2000 were included in this review. The reason for this was we wanted to examine novel techniques that were currently in use. However, we acknowledge that this may bias the outcomes of this review. Moreover, this analysis did not search the grey literature, and so there are potentially other studies which are relevant but were not included in this review.
There were also limitations of the studies included in this review. The mean follow duration was 50.8 mo across all studies. The mean follow-up for LET studies was 62.2 mo, compared with 36.8 mo for ALLR. As a result, these studies could not effectively compare rates of osteoarthritis between techniques. Though as previously mentioned, Ferretti et al[33] which conducted a 10-year follow up study, found no increases in osteoarthritic rates with ACLR with LET. Since ALLR is a relatively new technique, it is possible that more studies with longer follow up times may be available over the coming years. While it was recognized the reliably of the meta-analysis would be improved by only including studies with longer follow up (> 24 mo). We did include three studies that had a mean follow up period of approximately 12 mo[23-25]. It was the consensus of the authors that the large number of patients and the overall quality of the studies meant the data present in these two studies would add robustness to the meta-analysis as such they were included. The authors also felt it would be of value to the reader for the review to be more comprehensive to make the reader aware of the breadth of evidence available on the subject matter. This strengthened the consensus for the inclusion of these studies.
The addition of AEAPs to primary ACLR appears to result in improved rates of rotatory stability when comparing pivot shift test results, however it remains unclear whether this translates to improved functional outcomes. Our results suggest that surgeons should consider offering AEAPs in patients with rotatory instability following ACL rupture. More work is needed to identify patients who would benefit most. Both techniques appear to result in reduced rates of graft failure, compared to isolated ACLR, though ALLR has lower re-rupture rates than LET. Mechanical outcomes appear equivocal between the two AEAPs. A randomized controlled trial comparing the two techniques would be of value.
Anterior cruciate ligament (ACL) reconstruction surgery has shown excellent outcomes, however the restoration of rotational stability remains limited. The role of the reconstruction of the lateral soft tissue restraints or the supplement of the ACL reconstruction with a lateral extra-articular tenodesis have gain popularity and they are now routinely procedures following an ACL reconstruction.
The research motivation of this systematic review and meta-analysis was to clarify how ACL reconstruction surgery combined with lateral extra-articular tenodesis (LET) or anterolateral ligament reconstruction (ALLR) can improve rotational stability and how this can prevent possible failure and instability symptoms.
The aim of this review article was to compare the clinical effectiveness of ACL reconstruction surgery combined with LET or ALLR to ACLR alone.
A systematic review to include all the studies investigation either or both of LET and ALLR was conducted. A literature search was carried out on 4 databases for studies from 2000 to November 2021. All studies included in this review were independently appraised by two authors. The critical appraisal was conducted by the Critical Appraisal Skills Programme. Statistical analysis was performed on the collected data.
Thirteen studies compared ACLR to ACLR + LET. The remaining eleven were studies which compared ACLR to ACLR + ALLR.The nine studies that could be used in analysis encompassed 961 knees. Six of the nine studies demonstrated a statistically significant difference in pivot shift test scores between ACLR only patient groups and ACLR + AEAP patient groups.
This systematic review has demonstrated that the use of either LET or ALLR in addition to ACLR results in improved mechanical outcomes suggesting surgeons should consider augmenting ACLR with an extra-articular procedure in patients with rotatory instability.
A randomized controlled trial comparing the two techniques would be of value for clarifying which technique would give the better outcomes regarding the rotational stability following an ACL reconstruction surgery.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Beyzadeoglu T, Turkey S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | National Ligament Registry. The Sixth Annual Report. 2020. Available from: https://www.uknlr.co.uk/. |
| 2. | Chouliaras V, Ristanis S, Moraiti C, Stergiou N, Georgoulis AD. Effectiveness of reconstruction of the anterior cruciate ligament with quadrupled hamstrings and bone-patellar tendon-bone autografts: an in vivo study comparing tibial internal-external rotation. Am J Sports Med. 2007;35:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 124] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 3. | Tashman S, Collon D, Anderson K, Kolowich P, Anderst W. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:975-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 567] [Cited by in RCA: 510] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 4. | Luc B, Gribble PA, Pietrosimone BG. Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train. 2014;49:806-819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 310] [Cited by in RCA: 286] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 5. | Lien-Iversen T, Morgan DB, Jensen C, Risberg MA, Engebretsen L, Viberg B. Does surgery reduce knee osteoarthritis, meniscal injury and subsequent complications compared with non-surgery after ACL rupture with at least 10 years follow-up? Br J Sports Med. 2020;54:592-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 6. | Caterine S, Litchfield R, Johnson M, Chronik B, Getgood A. A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc. 2015;23:3186-3195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 226] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 7. | Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 545] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 8. | Schindler OS. Surgery for anterior cruciate ligament deficiency: a historical perspective. Knee Surg Sports Traumatol Arthrosc. 2012;20:5-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 106] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 9. | Castoldi M, Magnussen RA, Gunst S, Batailler C, Neyret P, Lustig S, Servien E. A Randomized Controlled Trial of Bone-Patellar Tendon-Bone Anterior Cruciate Ligament Reconstruction With and Without Lateral Extra-articular Tenodesis: 19-Year Clinical and Radiological Follow-up. Am J Sports Med. 2020;48:1665-1672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 10. | Marcacci M, Zaffagnini S, Giordano G, Iacono F, Presti ML. Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: A prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med. 2009;37:707-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 164] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 11. | Mahmoud A, Torbey S, Honeywill C, Myers P. Lateral Extra-Articular Tenodesis Combined With Anterior Cruciate Ligament Reconstruction Is Effective in Knees With Additional Features of Lateral, Hyperextension, or Increased Rotational Laxity: A Matched Cohort Study. Arthroscopy. 2022;38:119-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 12. | Getgood AMJ, Bryant DM, Litchfield R, Heard M, McCormack RG, Rezansoff A, Peterson D, Bardana D, MacDonald PB, Verdonk PCM, Spalding T; STABILITY Study Group, Willits K, Birmingham T, Hewison C, Wanlin S, Firth A, Pinto R, Martindale A, O'Neill L, Jennings M, Daniluk M, Boyer D, Zomar M, Moon K, Pritchett R, Payne K, Fan B, Mohan B, Buchko GM, Hiemstra LA, Kerslake S, Tynedal J, Stranges G, Mcrae S, Gullett L, Brown H, Legary A, Longo A, Christian M, Ferguson C, Mohtadi N, Barber R, Chan D, Campbell C, Garven A, Pulsifer K, Mayer M, Simunovic N, Duong A, Robinson D, Levy D, Skelly M, Shanmugaraj A, Howells F, Tough M, Spalding T, Thompson P, Metcalfe A, Asplin L, Dube A, Clarkson L, Brown J, Bolsover A, Bradshaw C, Belgrove L, Millan F, Turner S, Verdugo S, Lowe J, Dunne D, McGowan K, Suddens CM, Declercq G, Vuylsteke K, Van Haver M. Lateral Extra-articular Tenodesis Reduces Failure of Hamstring Tendon Autograft Anterior Cruciate Ligament Reconstruction: 2-Year Outcomes From the STABILITY Study Randomized Clinical Trial. Am J Sports Med. 2020;48:285-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 446] [Article Influence: 89.2] [Reference Citation Analysis (0)] |
| 13. | Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, Claes S. Outcome of a Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Technique With a Minimum 2-Year Follow-up. Am J Sports Med. 2015;43:1598-1605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 347] [Article Influence: 34.7] [Reference Citation Analysis (1)] |
| 14. | Hopper GP, Aithie JMS, Jenkins JM, Wilson WT, Mackay GM. Combined Anterior Cruciate Ligament Repair and Anterolateral Ligament Internal Brace Augmentation: Minimum 2-Year Patient-Reported Outcome Measures. Orthop J Sports Med. 2020;8:2325967120968557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). 2015. Available from: http://www.prisma-statement.org/. |
| 16. | O’Connor D, Green S HJ. Defining the Review Question and Developing Criteria for Including Studies. In: Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series. 2008. Available from: https://training.cochrane.org/handbook. |
| 17. | Lefebvre C, Manheimer E, Glanville J. Searching for Studies. In: Cochrane Handbook for Systematic Reviews of Interventions. John Wiley and Sons; 2008; 95–150. [DOI] [Full Text] |
| 18. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 40131] [Article Influence: 10032.8] [Reference Citation Analysis (2)] |
| 19. | Critical Appraisal Skills Programme. CASP Cohort Study Checklist. 2018. Available from: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Cohort-Study-Checklist_2018.pdf. |
| 20. | Vaudreuil NJ, Rothrauff BB, de Sa D, Musahl V. The Pivot Shift: Current Experimental Methodology and Clinical Utility for Anterior Cruciate Ligament Rupture and Associated Injury. Curr Rev Musculoskelet Med. 2019;12:41-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 21. | Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:107-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 285] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 22. | Hewison CE, Tran MN, Kaniki N, Remtulla A, Bryant D, Getgood AM. Lateral Extra-articular Tenodesis Reduces Rotational Laxity When Combined With Anterior Cruciate Ligament Reconstruction: A Systematic Review of the Literature. Arthroscopy. 2015;31:2022-2034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 184] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 23. | Chiba D, Gale T, Nishida K, Suntaxi F, Lesniak BP, Fu FH, Anderst W, Musahl V. Lateral Extra-articular Tenodesis Contributes Little to Change In Vivo Kinematics After Anterior Cruciate Ligament Reconstruction: A Randomized Controlled Trial. Am J Sports Med. 2021;49:1803-1812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 24. | Mogoş Ş, D'Ambrosi R, Antonescu D, Stoica IC. Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Results in Superior Rotational Stability Compared with Isolated Anterior Cruciate Ligament Reconstruction in High Grade Pivoting Sport Patients: A Prospective Randomized Clinical Trial. J Knee Surg. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 25. | Sonnery-Cottet B, Pioger C, Vieira TD, Franck F, Kajetanek C, Fayard JM, Thaunat M, Saithna A. Combined ACL and Anterolateral Reconstruction Is Not Associated With a Higher Risk of Adverse Outcomes: Preliminary Results From the SANTI Randomized Controlled Trial. Orthop J Sports Med. 2020;8:2325967120918490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 26. | Ayeni OR, Chahal M, Tran MN, Sprague S. Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20:767-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 183] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 27. | Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84:1560-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 249] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 28. | Geeslin AG, Moatshe G, Chahla J, Kruckeberg BM, Muckenhirn KJ, Dornan GJ, Coggins A, Brady AW, Getgood AM, Godin JA, LaPrade RF. Anterolateral Knee Extra-articular Stabilizers: A Robotic Study Comparing Anterolateral Ligament Reconstruction and Modified Lemaire Lateral Extra-articular Tenodesis. Am J Sports Med. 2018;46:607-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 143] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 29. | Inderhaug E, Stephen JM, Williams A, Amis AA. Biomechanical Comparison of Anterolateral Procedures Combined With Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2017;45:347-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 204] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 30. | Marom N, Ouanezar H, Jahandar H, Zayyad ZA, Fraychineaud T, Hurwit D, Imhauser CW, Wickiewicz TL, Pearle AD, Nawabi DH. Lateral Extra-articular Tenodesis Reduces Anterior Cruciate Ligament Graft Force and Anterior Tibial Translation in Response to Applied Pivoting and Anterior Drawer Loads. Am J Sports Med. 2020;48:3183-3193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 79] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 31. | Ra HJ, Kim JH, Lee DH. Comparative clinical outcomes of anterolateral ligament reconstruction versus lateral extra-articular tenodesis in combination with anterior cruciate ligament reconstruction: systematic review and meta-analysis. Arch Orthop Trauma Surg. 2020;140:923-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 32. | Novaretti JV, Arner JW, Chan CK, Polamalu S, Harner CD, Debski RE, Lesniak BP. Does Lateral Extra-articular Tenodesis of the Knee Affect Anterior Cruciate Ligament Graft In Situ Forces and Tibiofemoral Contact Pressures? Arthroscopy. 2020;36:1365-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 33. | Ferretti A, Monaco E, Ponzo A, Basiglini L, Iorio R, Caperna L, Conteduca F. Combined Intra-articular and Extra-articular Reconstruction in Anterior Cruciate Ligament-Deficient Knee: 25 Years Later. Arthroscopy. 2016;32:2039-2047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 106] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 34. | Schon JM, Moatshe G, Brady AW, Cruz RS, Chahla J, Dornan GJ, Turnbull TL, Engebretsen L, LaPrade RF. Anatomic Anterolateral Ligament Reconstruction Leads to Overconstraint at Any Fixation Angle: Response. Am J Sports Med. 2016;44:NP58-NP59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | Neri T, Cadman J, Beach A, Grasso S, Dabirrahmani D, Putnis S, Oshima T, Devitt B, Coolican M, Fritsch B, Appleyard R, Parker D. Lateral tenodesis procedures increase lateral compartment pressures more than anterolateral ligament reconstruction, when performed in combination with ACL reconstruction: a pilot biomechanical study. J ISAKOS. 2021;6:66-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 36. | Sonnery-Cottet B, Haidar I, Rayes J, Fradin T, Ngbilo C, Vieira TD, Freychet B, Ouanezar H, Saithna A. Long-term Graft Rupture Rates After Combined ACL and Anterolateral Ligament Reconstruction Versus Isolated ACL Reconstruction: A Matched-Pair Analysis From the SANTI Study Group. Am J Sports Med. 2021;49:2889-2897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 87] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 37. | Roth JH, Kennedy JC, Lockstadt H, McCallum CL, Cunning LA. Intra-articular reconstruction of the anterior cruciate ligament with and without extra-articular supplementation by transfer of the biceps femoris tendon. J Bone Joint Surg Am. 1987;69:275-278. [PubMed] |
| 38. | Bylski-Austrow DI, Grood ES, Hefzy MS, Holden JP, Butler DL. Anterior cruciate ligament replacements: a mechanical study of femoral attachment location, flexion angle at tensioning, and initial tension. J Orthop Res. 1990;8:522-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 140] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 39. | Hamido F, Habiba AA, Marwan Y, Soliman ASI, Elkhadrawe TA, Morsi MG, Shoaeb W, Nagi A. Anterolateral ligament reconstruction improves the clinical and functional outcomes of anterior cruciate ligament reconstruction in athletes. Knee Surg Sports Traumatol Arthrosc. 2021;29:1173-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 40. | Ibrahim SA, Shohdy EM, Marwan Y, Ramadan SA, Almisfer AK, Mohammad MW, Abdulsattar WS, Khirat S. Anatomic Reconstruction of the Anterior Cruciate Ligament of the Knee With or Without Reconstruction of the Anterolateral Ligament: A Randomized Clinical Trial. Am J Sports Med. 2017;45:1558-1566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 95] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 41. | Porter M, Shadbolt B. Modified Iliotibial Band Tenodesis Is Indicated to Correct Intraoperative Residual Pivot Shift After Anterior Cruciate Ligament Reconstruction Using an Autologous Hamstring Tendon Graft: A Prospective Randomized Controlled Trial. Am J Sports Med. 2020;48:1069-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 42. | Stensbirk F, Thorborg K, Konradsen L, Jørgensen U, Hölmich P. Iliotibial band autograft versus bone-patella-tendon-bone autograft, a possible alternative for ACL reconstruction: a 15-year prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2014;22:2094-2101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 43. | Trichine F, Alsaati M, Chouteau J, Moyen B, Bouzitouna M, Maza R. Patellar tendon autograft reconstruction of the anterior cruciate ligament with and without lateral plasty in advanced-stage chronic laxity. A clinical, prospective, randomized, single-blind study using passive dynamic X-rays. Knee. 2014;21:58-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 44. | Vadalà AP, Iorio R, De Carli A, Bonifazi A, Iorio C, Gatti A, Rossi C, Ferretti A. An extra-articular procedure improves the clinical outcome in anterior cruciate ligament reconstruction with hamstrings in female athletes. Int Orthop. 2013;37:187-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 45. | Ahn JH, Kim J, Mun JW. A Retrospective Comparison of Single-Bundle Anterior Cruciate Ligament Reconstruction With Lateral Extra-Articular Tenodesis With Double-Bundle Anterior Cruciate Ligament Reconstruction. Arthroscopy. 2021;37:976-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 46. | Dejour D, Vanconcelos W, Bonin N, Saggin PR. Comparative study between mono-bundle bone-patellar tendon-bone, double-bundle hamstring and mono-bundle bone-patellar tendon-bone combined with a modified Lemaire extra-articular procedure in anterior cruciate ligament reconstruction. Int Orthop. 2013;37:193-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 47. | Erden T, Toker B, Toprak A, Taşer Ö. Comparison of the outcomes of isolated anterior cruciate ligament reconstruction and combined anterolateral ligament suture tape augmentation and anterior cruciate ligament reconstruction. Jt Dis Relat Surg. 2021;32:129-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 48. | Giraud B, Besse JL, Cladière F, Ecochard R, Moyen B, Lerat JL. [Intra-articular reconstruction of the anterior cruciate ligament with and without extra-articular supplementation by quadricipital tendon plasty: seven-year follow-up]. Rev Chir Orthop Reparatrice Appar Mot. 2006;92:788-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 49. | Goncharov EN, Koval OA, Dubrov VE, Bezuglov EN, Filimonova AM, Goncharov NG. Clinical experience with combined reconstruction of the anterior cruciate and anterolateral ligaments of the knee in sportsmen. Int Orthop. 2019;43:2781-2788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 50. | Lee DW, Kim JG, Cho SI, Kim DH. Clinical Outcomes of Isolated Revision Anterior Cruciate Ligament Reconstruction or in Combination With Anatomic Anterolateral Ligament Reconstruction. Am J Sports Med. 2019;47:324-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 112] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 51. | Rowan FE, Huq SS, Haddad FS. Lateral extra-articular tenodesis with ACL reconstruction demonstrates better patient-reported outcomes compared to ACL reconstruction alone at 2 years minimum follow-up. Arch Orthop Trauma Surg. 2019;139:1425-1433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 52. | Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M. Anterolateral Ligament Reconstruction Is Associated With Significantly Reduced ACL Graft Rupture Rates at a Minimum Follow-up of 2 Years: A Prospective Comparative Study of 502 Patients From the SANTI Study Group. Am J Sports Med. 2017;45:1547-1557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 361] [Article Influence: 45.1] [Reference Citation Analysis (0)] |
| 53. | Sonnery-Cottet B, Saithna A, Blakeney WG, Ouanezar H, Borade A, Daggett M, Thaunat M, Fayard JM, Delaloye JR. Anterolateral Ligament Reconstruction Protects the Repaired Medial Meniscus: A Comparative Study of 383 Anterior Cruciate Ligament Reconstructions From the SANTI Study Group With a Minimum Follow-up of 2 Years. Am J Sports Med. 2018;46:1819-1826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 97] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 54. | Ventura A, Legnani C, Boisio F, Borgo E, Peretti GM. The association of extra-articular tenodesis restores rotational stability more effectively compared to contralateral hamstring tendon autografts ACL reconstruction alone in patients undergoing ACL revision surgery. Orthop Traumatol Surg Res. 2021;107:102739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 55. | Helito CP, Sobrado MF, Giglio PN, Bonadio MB, Pécora JR, Camanho GL, Demange MK. Combined Reconstruction of the Anterolateral Ligament in Patients With Anterior Cruciate Ligament Injury and Ligamentous Hyperlaxity Leads to Better Clinical Stability and a Lower Failure Rate Than Isolated Anterior Cruciate Ligament Reconstruction. Arthroscopy. 2019;35:2648-2654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 108] [Article Influence: 18.0] [Reference Citation Analysis (0)] |