INTRODUCTION
Hip fracture is recognized as a worldwide health problem, and the incidence of hip fractures is on the rise due to the aging population[1]. Hip fractures are expected to increase from 258000 per year in 2010 to 458000 per year in 2050 in the United States. By 2050, the global number of hip fractures is expected to reach 4.5 million per year[2]. Older patients have more medical comorbidities, making it harder for them to recover from hip fractures[3]. Given that the global population of elderly individuals is expanding and the difficulty of recovery, hip fractures will be a huge challenge and a critical health issue for all of humanity. The new coronavirus disease-2019 (COVID-19) has posed a substantial threat to people’s social lives and medical health care worldwide. The Centers for Disease Control and Prevention in the United States reported 33.8 million confirmed COVID-19 cases and 605905 related fatalities as of July 2021. COVID-19 has had a significant impact on hospital and intensive care unit (ICU) expenditures as well as the length of stay[4]. The virus is transmitted by droplets and causes a flu-like upper respiratory infection with symptoms such as cough, fever, and dyspnea in severe cases[5]. However, to control the spread of the disease, the implementation of epidemic prevention policies, lockdown of social activities, and travel restrictions have reduced traumatic injury admissions to an all-time low. The mechanism of trauma-related fractures has shifted from high energy to low energy, for example, emergency admissions due to falls from a great height and vehicle accidents have declined[6]. Most of the cases seen are due to stumbles and falls from a standing position, particularly in elderly individuals with osteoporosis. Therefore, hip fractures in the elderly are still being seen generally at an unchanged rate, especially the fragility fractures around the hip such as neck of femur and intertrochanteric fractures[7,8]. In this vulnerable group, a significant number of patients are at risk of COVID-19, as the elderly have weaker immune systems, more chronic illness, and poorer tolerance[9]. The virus (acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which causes COVID-19 has been found to not only damage the respiratory system but affect multiple organ systems. Therefore, it is challenging for medical practitioners when two conditions exist in the same person, especially the elderly[10].
Hip fractures in patients defined as COVID-19 positive, whether preoperatively or postoperatively infected, have a multi-systemic impact that makes perioperative care, the course of surgery, and postoperative rehabilitation more difficult and complex. Compared to uninfected patients, they are exposed to more risks. Recent studies have identified that COVID-19 positive status is an independent predictor of mortality in hip fracture patients[11]. The data collected by Wang et al[12] demonstrated that the relative risk of postoperative mortality in COVID-19 positive patients compared to uninfected patients was 5.66 (95%CI: 4.01-7.98; P < 0.001). In a retrospective multicenter assessment, Oputa et al[13] discovered that the mortality of COVID-19 positive hip fracture patients at 120 d had also increased dramatically (63%:17%, P < 0.01). In addition, COVID-19 positive patients were associated with increased length of hospital stay, more admissions to the critical care unit, and a higher risk of perioperative complications compared with COVID negative hip fracture patients[14].
Although the prevention of COVID-19 has become a part of daily life for people all over the world and the virus does place a huge burden on both patient conditions and medical systems, the corresponding coping strategies are constantly being updated. To address these new challenges, increased attention to this comorbidity is necessary not only to gain a thorough understanding of the clinical condition of COVID-19 positive patients but also to provide optimal clinical treatment options for these patients. Here, we performed a narrative review to (1) Provide an overview of the clinical impact in COVID-19 positive hip fracture patients compared to those diagnosed as COVID-19 negative. Also to provide clinicians with predictability so that they can fully prepare in advance; and (2) Provide practical suggestions regarding existing diagnostic and care methods to overcome various difficulties caused by COVID-19.
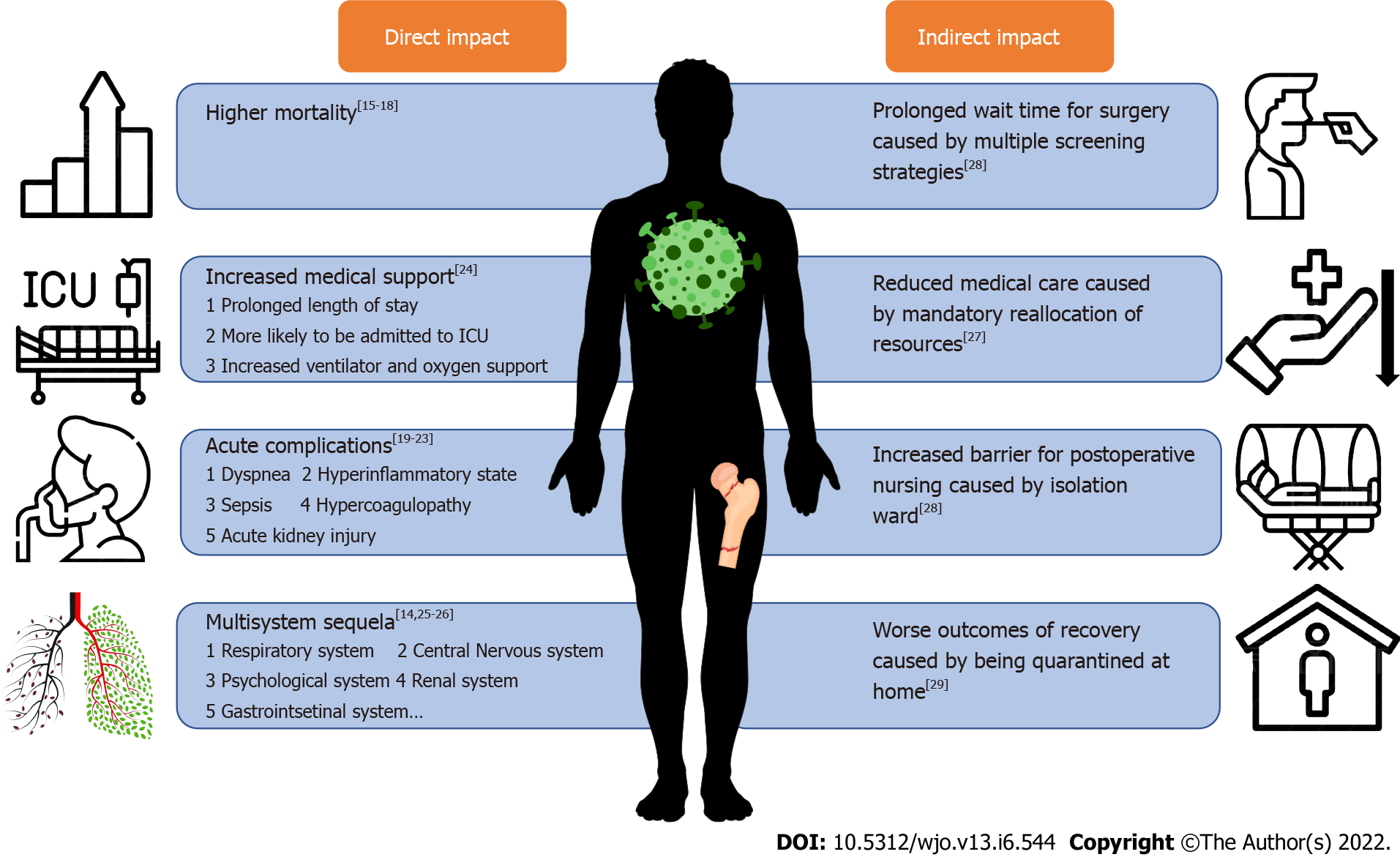
IMPACT OF COVID-19 ON PATIENTS WITH HIP FRACTURES
The direct impact of COVID-19 itself, as well as quarantine methods against COVID-19, both have a significant influence on the diagnosis and treatment of hip fracture patients. As the age distribution of patients with hip fractures is mainly over 60 years old, most patients will experience multiple complications and cannot completely reclaim their pre-injury physical function[15]. Therefore, if they are further infected with COVID-19, the underlying medical comorbidities, severity of COVID-19 complications, corresponding treatment measures and combined morbidity and mortality of the two conditions remain unclear.
Acute respiratory distress syndrome (ARDS) with widespread alveolar damage, diffuse thrombotic alveolar microvascular occlusion, and inflammatory mediator-associated airway inflammation are three ways the virus damages the lungs histologically. The patient can present with dyspnea, decreased oxygen saturation, and even pulmonary embolism[16]. A significant increase in mortality in patients with COVID-19 and hip fractures has been extensively documented[17-20]. According to recent research, patients with hip fractures who are COVID-19 positive are more vulnerable to complex perioperative complications, such as acute sarcopenia, sepsis, pneumonia, acute respiratory failure, cardiac arrest, and acute kidney injury than patients who are COVID-19 negative[21-23], and are more likely to experience life-threatening complications, such as acute respiratory failure, cardiac arrest, and serious infections[24,25]. These perioperative complications present challenges to surgery. Some complications in certain systems may affect the long-term recovery of hip fracture patients. For example, COVID-19 can cause muscle atrophy, which can then lead to a significant decline in physical function and an increased risk of falls[23]. Following surgery, the virus can introduce a widespread hyperinflammatory state (a cytokine storm), and this condition is further exacerbated by surgery and leads to widespread organ failure. In addition, both diseases can cause a procoagulant state and increase the rate of thromboembolic events[26]. Complex clinical symptoms require extra precise therapeutic intervention and support, as well as a longer length of stay[27]. Prolonged length of stay may be due to barriers to discharge planning, including waiting for COVID-19 positive patients to become negative. COVID-19 positive patients are also more likely to be admitted to the ICU, require ventilators and other medical support equipment after surgery. As COVID-19 mainly affects the lungs, causing symptoms such as dyspnea and decreased oxygen saturation, a ventilator is a necessary auxiliary therapeutic instrument for such patients.
In addition to the acute phase, COVID-19 also causes many long-term, multi-system sequelae, which could greatly delay the rehabilitation of hip fractures. As the COVID-19 pandemic has lasted for more than a year, it is difficult to identify and investigate its long-term sequelae. However, the follow-up of patients who recovered from severe acute respiratory syndrome coronavirus 1 (SARS-COV-1) infection in 2003 reported some results that may explain the long-term prognosis of SARS-COV-2 infection. According to a follow-up study of SARS-CoV-1 survivors, pulmonary ventilation performance in all patients was affected to varying degrees, and the pulmonary diffusion function in more than one-third of patients was considerably damaged[28,29], ultimately affecting the patient’s daily life. In addition to respiratory sequelae, disorders such as Alzheimer’s Disease, Parkinson’s Disease, and Multiple Sclerosis of the nervous system[16], acute sarcopenia of the muscular system, are all associated with COVID-19 and have detrimental effects on hip fractures.
Indirectly, the COVID-19 pandemic has led to a global surge in critically ill patients, hospitals have been forced to reallocate resources to virus screening for patients’ admission, setting up special isolation corridors, wards, and operating rooms (ORs), which potentially reduce patients’ access to emergency care[30]. For positive or suspected positive patients requiring emergency hip surgery, multiple admission screening, and evaluation, waiting for a designated negative pressure OR will inevitably delay operation time[31]. Post-operatively, as the patient is in an isolation ward, nurses, rehabilitation therapists and physicians have less access, resulting in the absence of routine in-hospital care. After discharge, it is suggested that the patients remain at home. In order to minimize the number of visits to the hospital and reduce the risk of re-infection, frequent follow-up visits are not recommended, which increases the difficulty of long-term postoperative recovery[32].
In conclusion, not only is the virus having a severe impact on patients, but some mandatory adoptions in response to COVID-19 are also potentially having an indirect impact on patients. The effects of COVID-19 on patients with hip fractures are presented in Figure 1.
Figure 1 Summary of the impact of coronavirus disease 2019 on patients with hip fractures.
ICU: Intensive care unit.
MANAGEMENT TO ADDRESS THE ISSUE
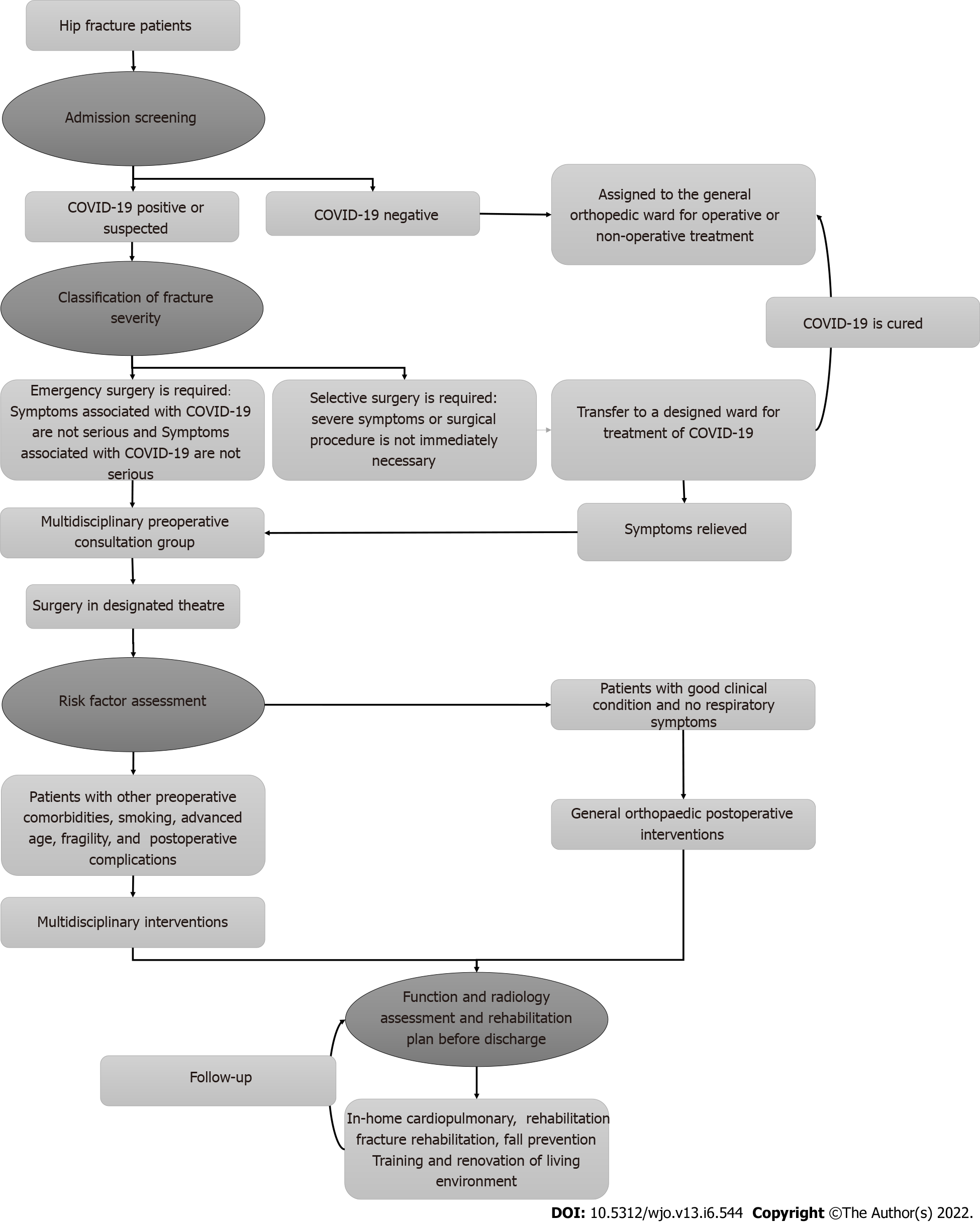
Admission screening
With no definitive treatment to date, prevention of COVID-19 is critical. To reduce infection between positive patients and other patients and hospital staff, patients admitted to the hospital and accompanying family members must be screened. Diagnosis in COVID-19 patients must be based on epidemiological history, clinical symptoms, imaging, and most importantly, a reverse-transcription PCR of nasopharyngeal and oropharyngeal swab samples[33]. An epidemiological inquiry should be made first to determine whether the patient has had close contact (someone who has clearly had contact with an infected person, possibly an asymptomatic carrier of the virus) with an infected person, or a high-risk community in the past 14 d.
Second, diagnostic evidence is further provided by the typical clinical features of COVID-19 infection, including fever, dry cough, and lung imaging features. Blood indicators can also be used as diagnostic indicators, such as white blood cell count, and platelet count[34].
However, 4%-18% of COVID-19 positive patients are asymptomatic carriers of the virus, and the incubation period for COVID-19 is 10 to 14 d, during which time the disease is highly contagious, but the patient may not show characteristics of systemic infection. Therefore, we strongly recommend nucleic acid testing for all hospitalized patients and multiple nucleic acid tests for patients with relevant clinical symptoms and patients with suspected epidemiology within 14 d.
Patient triage (determination of treatment)
It is widely known that early surgery should be performed in elderly patients with hip fractures[35]. If the condition does not allow surgery to be performed and the waiting time for surgery is prolonged, there are many complications associated with prolonged bed rest, such as respiratory failure, urinary and genital tract infection, stones, bedsores, body temperature disorders, deep vein thrombosis, which ultimately affect the recovery of physical functions[36]. However, COVID-19 patient status should play a role in determining the timing of surgery[37]. Recent studies have suggested that mortality in COVID-19 positive patients may be due to virus-driven high inflammation. Significantly elevated levels of multiple inflammatory markers can lead to widespread organ failure. In addition, inflammation due to acute fractures or fracture repair surgery may further exacerbate the status of patients with acute COVID-19. Therefore, surgical thresholds for positive patients should be higher than normal patients, particularly in the advanced-age group. Greater consideration should be given to the possibility of postponing non-emergency procedures and promoting non-surgical treatment. We recommend surgery only for patients with asymptomatic or mild COVID-19 symptoms. Although these patients may have temporary increased oxygen demands postoperatively, they can safely undergo early surgical intervention after appropriate medical optimization[38]. However, we still suggest that if an emergency operation is required, a comprehensive preoperative understanding of the patient’s multi-system clinical data and a multidisciplinary group of experts should be established to determine the optimum time of surgery[39]. Minimally invasive surgery, which requires less surgical time and minimizes blood loss, is also recommended for older patients with hip fractures. Conservative treatment with traction may be considered for high-risk COVID-19 patients with hip fractures.
Preoperative and intraoperative matters requiring attention
Rigorous quarantine measures should be immediately followed after the admission of COVID-19 positive patients. It is necessary to rationally design the hospital passage for infected and non-infected, as well as the isolation wards. To prevent cross-infection, COVID-19 positive patients are sent to an isolation ward, where separate teams should be appointed. A channel should be set up for the transfer of COVID-19 patients, but only if the transfer is minimal in the hospital. Those with suspected COVID-19 will be assigned to a separate room until multiple nucleic acid test results are obtained before further treatment. Medical institutions with limited medical technology and resources are advised to transfer patients to special hospitals equipped to treat COVID-19 patients.
The management of special passage, ORs, and isolation wards are strict during the pandemic, which leads to a delay in the operation start time, the extension of surgery duration, difficulty in prognosis observation, and difficulty in multi-disciplinary intervention such as postoperative rehabilitation intervention. Yu et al[31] found that the waiting time for surgery during the outbreak period was longer due to mandatory COVID-19 screening. Early surgical intervention can improve patient outcomes. On the contrary, prolonged operation time will increase the incidence of complications. Patients who are scheduled for emergency surgery should be prepared as quickly as possible to reduce the waiting time for patients who meet surgical criteria. With regard to the choice of anesthesia and surgical procedure, there are still no guidelines for patients with hip fractures and COVID-19 to help decide which procedure is the best option. Spinal anesthesia for hip fracture surgery in older adults was not found to be superior to general anesthesia with respect to survival and recovery of ambulation[40]. In addition, the type of surgery affects the length of hospital stay. Open reduction and internal fixation, and closed reduction and percutaneous pinning lead to fewer in-patient days than total hip arthroplasty and hemiarthroplasty, which should be taken into consideration in the anesthesia and surgical method[41].
Designated isolation ORs and surgical instruments should be prepared in advance, and cancellation of elective theatres can be advocated to offset increased waiting time for surgery[42]. In addition, there should be strict standards in the OR. The majority of ORs are under positive pressure. In these circumstances, a specialized OR should be set up with negative pressure. The number of people in the OR must be reduced to a strict minimum and entering and leaving the room should be avoided as much as possible during surgery. Disposable equipment is preferred[43]. When the surgery is complete, thorough disinfection of the OR is imperative before the next operation. Whether symptoms are present or not, all patients require interval testing with further swabs following surgery[44].
Efforts should be made to coordinate intra-departmental allocation and redeployment of human resources during the pandemic. The existing model should be updated to neutralize the impact of COVID-19.
Postoperative care
Postoperative care involves multiple dimensions. Supportive and nutritional treatment should be prioritized after surgery and individualized treatment should be tailored to each patient’s specific situation. A multicenter observational cohort study by Rasidovic demonstrated that male sex, smoking, and patients with two or more comorbidities (e.g. diabetes, dementia) were associated with higher mortality rates[45]. Extracapsular fractures are also an indicator of high mortality[46]. Smoking, alcohol consumption, and attitudes to COVID-19 may explain the higher prevalence in men than women[47]. Therefore, it is clinically meaningful to strengthen the post-operative care of males, smokers, drinkers, and patients with extracapsular fractures or multiple comorbidities. Multidisciplinary intervention in postoperative care should be provided by an expert team established preoperatively until the patient's clinical symptoms stabilize.
Despite being a respiratory illness, COVID-19 has been found to increase the risk of venous and arterial thromboembolic events[48]. The inflammatory changes in COVID-19 include a prothrombotic state with a high risk of venous thromboembolism[49]. Surgery for hip fractures may further aggravate this pathology. Therefore, postoperative use of anticoagulant drugs is necessary. Psychologically, patients under contact protection are visited less by family members and medical staff, which, together with the psychological impact of a hip fracture, leads to higher rates of anxiety, depression, and delirium[50].
Due to lockdown, people remain at home when they are discharged from the hospital. This highlights the importance of fall prevention strategies for the elderly at home. Patients at high risk of falling as indicated by the Morse Fall Scale or Berg Balance Scale before discharge are advised to wear a hip orthosis or explain the use of crutches. Indoor factors that may contribute to falls must also be corrected[51]. In addition, the unchanging living environment and facilities at home are not conducive to the progress of patients' physical function. The benefits of physical therapy should be explained to patients to avoid fragility fractures. Patients are advised to engage in low-intensity aerobic exercise (e.g. indoor walking for 30 min or more per day) to strengthen muscle and balance functions. Similarly, patients with muscle atrophy should be trained in a progressive manner, and patients with previous fragility fractures are at significantly increased risk of dysmotility syndrome and skeletal muscle function deficit that might presumably increase the risk of a new incident fracture[52]. Adequate daily calcium intake and regular calcium density checks should be emphasized in elderly female patients. As hospitals remain high-risk areas for COVID-19 infection, post-surgery follow-up and rehabilitation plan updates can be consulted via smartphone apps and telemedicine facilities, avoiding in-person visits and sudden suspension of medical institutions[53].
With the rapid spread of COVID-19, access to safe and effective vaccines is critical in ending the COVID-19 pandemic. Studies have shown that among hospitalized patients infected with COVID-19, despite receiving only one dose of the vaccine, mortality rates are significantly lower and hospital courses are simpler in the vaccinated group[54]. Although vaccination entails certain risks for the elderly population, especially those with underlying medical conditions and frailty, studies continue to show that the benefits of vaccination far outweigh the potential risks in frail elderly (e.g. long-term care facilities)[55]. Thus, we believe it is necessary to vaccinate patients with hip fractures.
CONCLUSION
COVID-19 can have significant adverse effects on patients with hip fractures, both directly and indirectly. However, the impact can be effectively reduced by monitoring all aspects of the post-admission process.
In this minireview, we outlined the direct physiological consequences introduced by COVID-19, as well as the practical issues that arise throughout the treatment and diagnosis procedure. By understanding these potential concerns in advance, staff in associated departments will be capable of making rational decisions and acquiring a comprehensive aspect of the progression of the disease. In the following section, we summarized the existing experimental evidence and offer a set of optimized suggestions to improve patient outcomes. The model consists of admission screening, patient triage (determination of treatment), preoperative and intraoperative matters requiring attention, and postoperative care (the clinical flowchart is presented in Figure 2). However, these recommendations are not the solution for all situations. As the prevalence of the epidemic varies across the nations, as does the medical capacity of hospitals, certain studies are required to reach a consensus that could suit more regions and circumstances. Notably, the suggested managements presented above apply not just to COVID-19 now, but also to any future highly contagious respiratory illnesses. Although the epidemic in China is now firmly under control, thanks to the government's attention, we should not be complacent, as the emergence of new and extremely contagious strains of COVID-19, such as Delta and Omicron, could make another outbreak possible. In addition, there are still certain countries in the world where suppression of COVID-19 is not ideal. Thus, research regarding COVID-19 co-morbidity in patients with hip fractures is expected to continue. In the context of COVID-19 ramping wildly, it is imperative to optimize treatment strategies to turn the tables globally.
Figure 2 Clinical flowchart of the treatment of patients with hip fractures who are coronavirus disease 2019 positive.
COVID-19: Coronavirus disease.
Fighting the COVID-19 pandemic has become a regular part of our lives, as well as a mountain that healthcare providers must overcome. Elderly people account for a large proportion of COVID-19 deaths[56,57] as they have more comorbidities and are more fragile. Prevention and care in this subgroup are essential, and when combined with a life-threatening trauma, this influences their clinical outcomes. We believe that it is necessary to form a multidisciplinary expert panel, which can not only comprehensively evaluate the timing of surgery for patients, but also provide a reasonable multidisciplinary treatment plan after surgery.
PERSPECTIVE
At present, there is limited information on the perioperative risk of increased mortality in patients who require urgent hip fracture surgery and are infected with COVID-19. Konda et al[58] utilized the Score for Trauma Triage in the Geriatric and Middle-Aged, which was originally a tool to predict postoperative in-hospital mortality in trauma patients, to create a research-based strategy for operative vs. nonoperative management of patients with hip fractures who were COVID-19 positive/suspected. For subsequent research, we strongly suggest that more experiments could further refine this risk assessment form into a more comprehensive and adaptable one. The assessment may include the patient's respiratory symptoms and fracture severity rating (which should be given primary weight), presence of complications, inflammatory indicators (such as C-reactive protein, procalcitonin, lactates), clinical scores (e.g., American Society of Anesthesiologists grade, Alvarado score, sequential organ failure assessment score), smoking status, etc. Use of this form could provide surgeons, physicians, and other healthcare practitioners with relevant clinical information, helping them make standardized therapeutic decisions by foreseeing potential outcomes. It has been reported that patients with asymptomatic infection or with only mild symptoms show a lower risk of perioperative morbidity and mortality associated with operations. Therefore, the surgical risk assessment for such patients should be reconsidered from that for patients with symptomatic infection[59]. However, there are no cohort studies to prove the effect of asymptomatic infection on surgical or prognostic recovery of hip fracture. Subsequent studies should identify the criteria for assessing surgical risk in these patients and whether asymptomatic infection has an impact on hip fracture outcomes, and if so, what impact.
In addition, as COVID-19 is a severe acute respiratory infection[60], most articles have placed an emphasis on the short-term clinical impact caused by the disease. However, it is well known that hip fracture patients require regular sustained rehabilitation[61]. Currently, available experimental data does not assist in comprehending the influence of COVID-19 on the long-term recovery of hip fracture. According to the report by McDonald[62], one of the sequelae that can occur in COVID-19 patients, especially in those who develop ARDS during infection, is pulmonary fibrosis. Pulmonary fibrosis results from excessive deposition of extracellular matrix molecules such as collagen, laminin, and fibronectin in the lung parenchyma. Eventually, the efficiency of gas exchange decreases due to thickened alveolar membrane. Patients will then suffer from decreased lung function and exercise intolerance, fatigue, and dyspnea, which severely delay the restoration process compared to those who possess fully functional lungs. It is critical to make early predictions of the possible long-term sequelae of COVID-19 and to formulate appropriate prevention and intervention strategies. Whether continuous low-intensity physical therapy combined with cardiopulmonary breathing training can better facilitate patients to restore prior functions deserves further investigation.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Rehabilitation
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Iida H, Japan; Moretti A, Italy S-Editor: Wang JL L-Editor: Webster JR P-Editor: Wang JL