Published online May 18, 2022. doi: 10.5312/wjo.v13.i5.528
Peer-review started: August 28, 2021
First decision: November 17, 2021
Revised: November 28, 2021
Accepted: April 25, 2022
Article in press: April 25, 2022
Published online: May 18, 2022
Processing time: 257 Days and 8 Hours
Femoral shaft fracture is a commonly encountered orthopedic injury that can be treated operatively with a low overall delayed/nonunion rate. In the case of delayed union after antegrade or retrograde intramedullary nail fixation, fracture dynamization is often attempted first. Nonunion after dynamization has been shown to occur due to infection and other aseptic etiologies. We present a unique case of diaphyseal femoral shaft fracture nonunion after dynamization due to intramedullary cortical bone pedestal formation at the distal tip of the nail.
A 37-year-old male experienced a high-energy trauma to his left thigh after coming down hard during a motocross jump. Evaluation was consistent with an isolated, closed, left mid-shaft femur fracture. He was initially managed with reamed antegrade intramedullary nail fixation but had continued thigh pain. Radiographs at four months demonstrated no evidence of fracture union and failure of the distal locking screw, and dynamization by distal locking screw removal was performed. The patient continued to have pain eight months after the initial procedure and 4 mo after dynamization with serial radiographs continuing to demonstrate no evidence of fracture healing. The decision was made to proceed with exchange nailing for aseptic fracture nonunion. During the exchange procedure, an obstruction was encountered at the distal tip of the failed nail and was confirmed on magnified fluoroscopy to be a pedestal of cortical bone in the canal. The obstruction required further distal reaming. A longer and larger diameter exchange nail was placed without difficulty and without a distal locking screw to allow for dynamization at the fracture site. Post-operative radiographs showed proper fracture and hardware alignment. There was subsequently radiographic evidence of callus formation at one year with subsequent fracture consolidation and resolution of thigh pain at eighteen months.
The risk of fracture nonunion caused by intramedullary bone pedestal formation can be mitigated with the use of maximum length and diameter nails and close follow up.
Core Tip: Femoral shaft fracture nonunion after surgical fixation is a rare complication known to be associated with infection, anatomic abnormalities, hardware failure, and other aseptic etiologies. It is now known that intramedullary bone pedestal formation can also be a cause of nonunion after fracture dynamization. In order to prevent this complication, surgeons should elect to use a maximal length intramedullary nail during initial fixation and follow up closely if the patient is showing signs of delayed union.
- Citation: Pasque CB, Pappas AJ, Cole Jr CA. Intramedullary bone pedestal formation contributing to femoral shaft fracture nonunion: A case report and review of the literature. World J Orthop 2022; 13(5): 528-537
- URL: https://www.wjgnet.com/2218-5836/full/v13/i5/528.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i5.528
Diaphyseal femur fractures treated with reamed intramedullary nail fixation have a low incidence of nonunion[1-5]. Nonunions have been found to occur secondary to infection and a variety of aseptic etiologies. Aseptic nonunions have been associated with fracture instability, distraction, malalignment, large bony defects, and open fractures. These procedure and fracture associated factors prevent adequate blood supply to the fracture site and impede the healing response. Patient factors have also been linked to nonunions in some series. These may be factors that lead to poor blood supply such as vascular disease, diabetes, and smoking. Others have a more direct effect on the healing process by impeding the immune response and preventing the proper balance of osteoblast/osteoclast activity. These include the use of non-steroidal anti-inflammatory drugs (NSAIDs), use of steroids, advancing age, malignancy, and diabetes mellitus[6-11].
When an aseptic fracture nonunion occurs after intramedullary nail fixation, there are multiple methods of revision that have been studied and proven to be effective. Such methods include, nail dynamization, exchange nailing, and augmentative plating[4,5]. Causes of non-union after revision have been found to be similar to that of non-union after initial fixation, though the rare incidence of repeat non-union has led to sparse data on the topic. We present a unique case of mid-shaft femur fracture nonunion after nail dynamization due to intramedullary bone pedestal formation.
A 37-year-old white male presented to our clinic with 5 mo of left thigh pain with activity.
The patient’s symptoms began when he was involved in a motocross accident in which he came down hard from a jump. He remarkably was able to hop to his car and drive himself to a nearby hospital where he was found to have an obvious deformity of the left thigh. Subsequent evaluation was consistent with an isolated, closed, left mid-shaft femur fracture.
The patient underwent reamed antegrade intramedullary nail fixation of his left femur fracture at an outside hospital. Post-operative recovery was unremarkable except that he continued to have problems with left thigh pain during activity. Four months after his initial surgery, he was found to have broken his single distal locking screw, and he underwent distal locking screw removal for nail dynamization at the outside hospital. Left thigh pain with activity persisted five months post-operatively prompting presentation to our clinic.
The patient had no relevant previous medical history.
The patient had no relevant personal or family medical history.
The patient had a well-healed incisions without evidence of infection. He had left thigh pain to palpation and with weight bearing.
Baseline laboratory studies including an erythrocyte sedimentation rate were unremarkable.
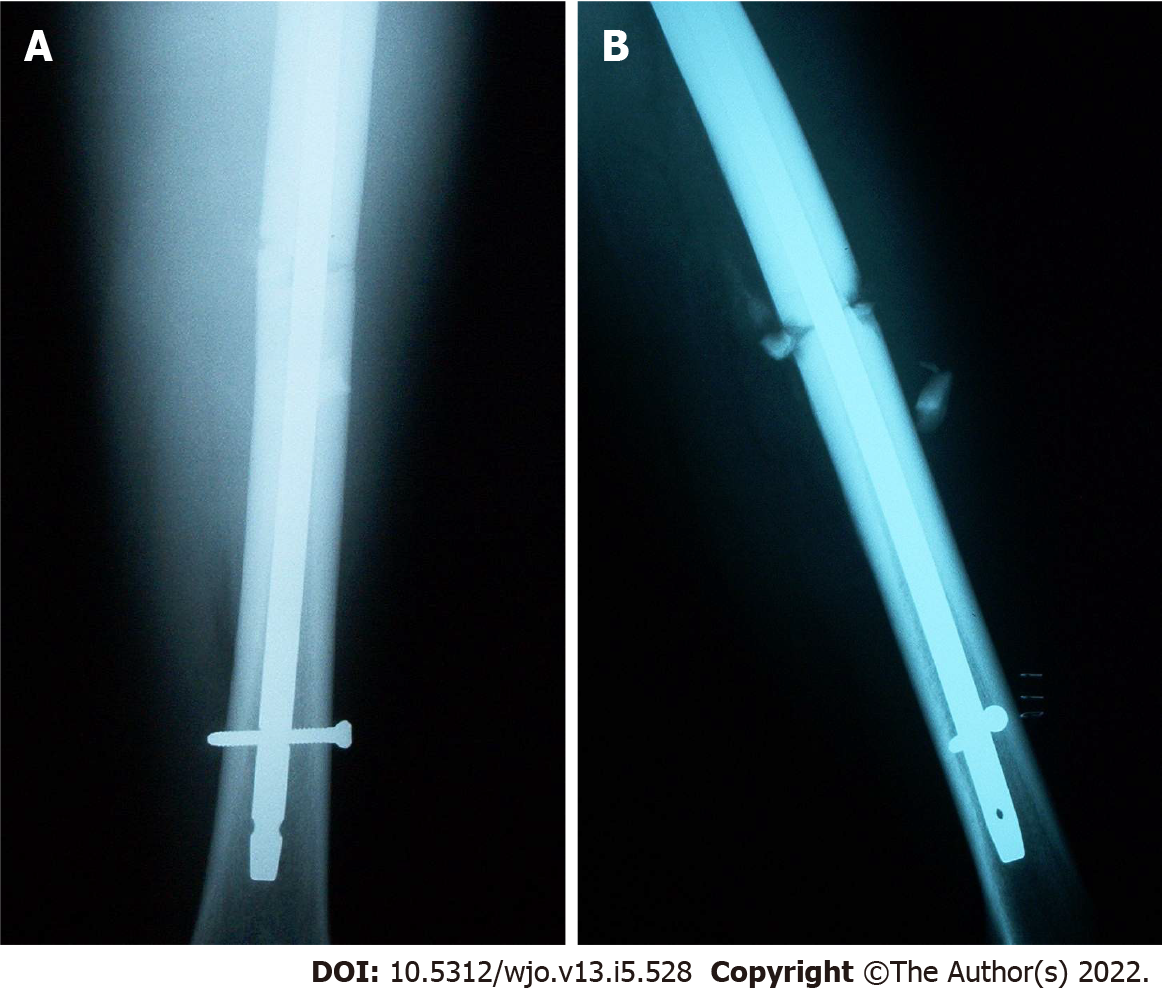
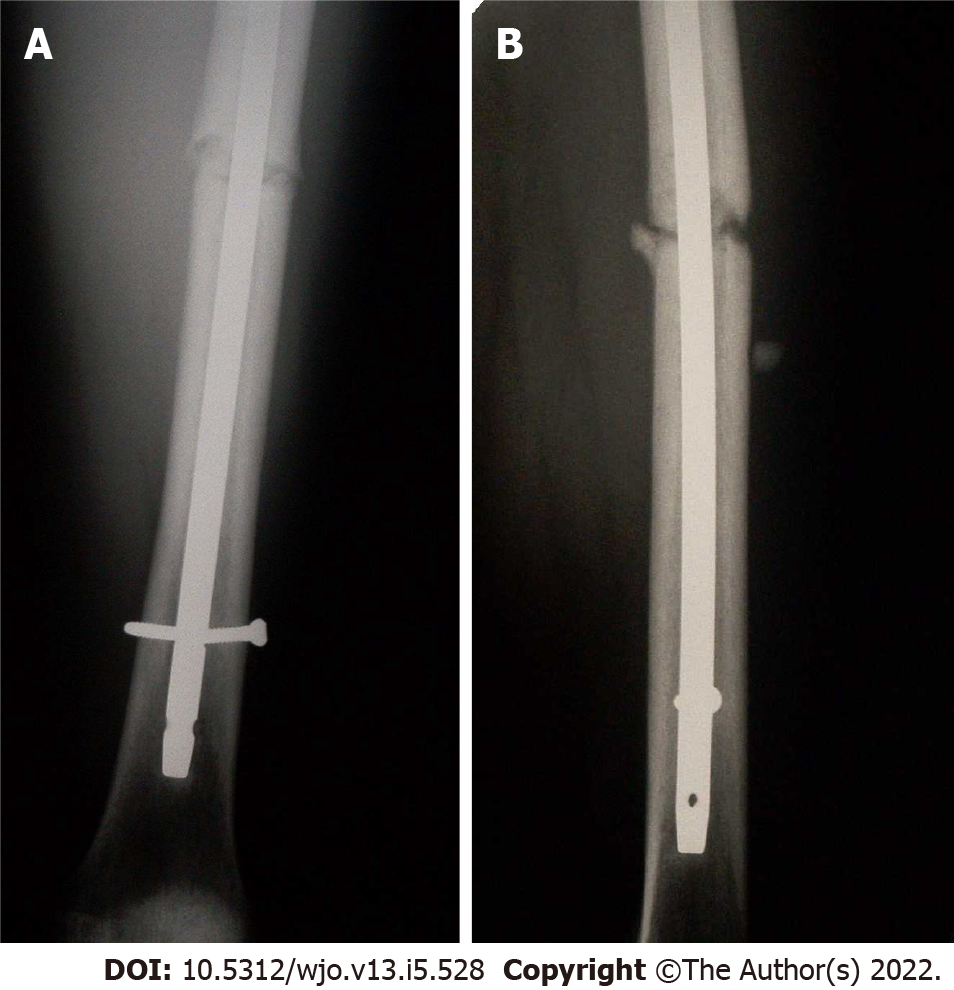
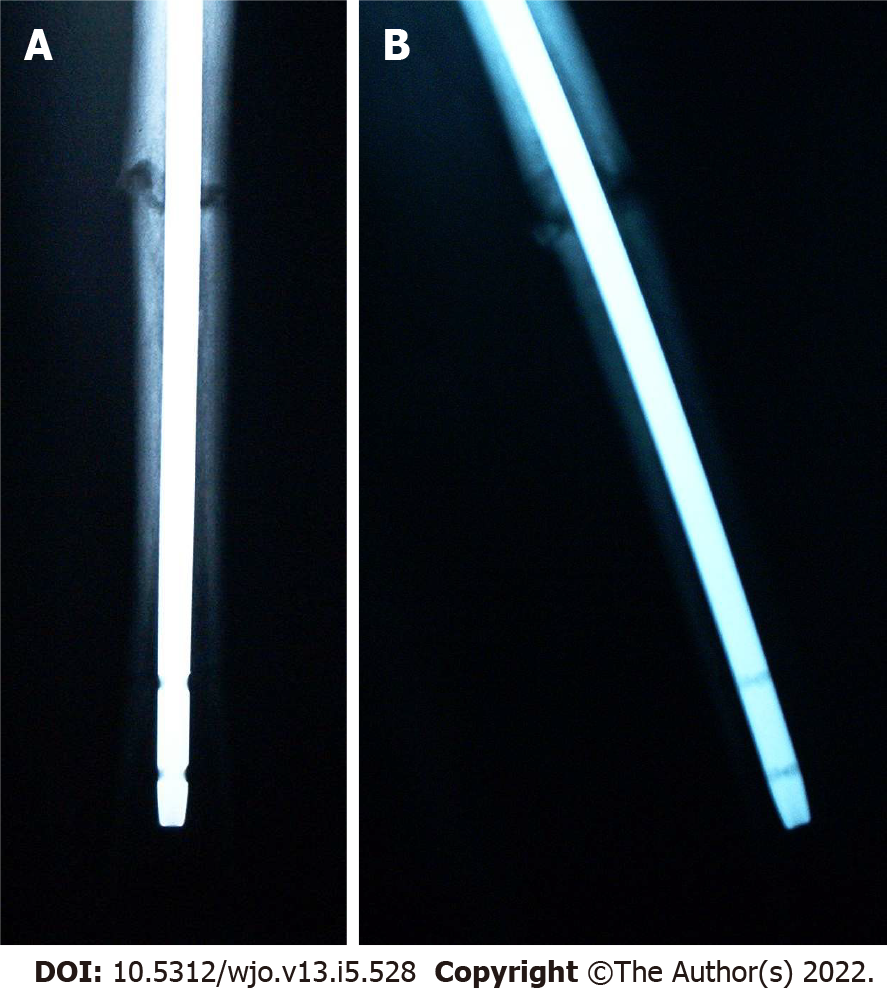
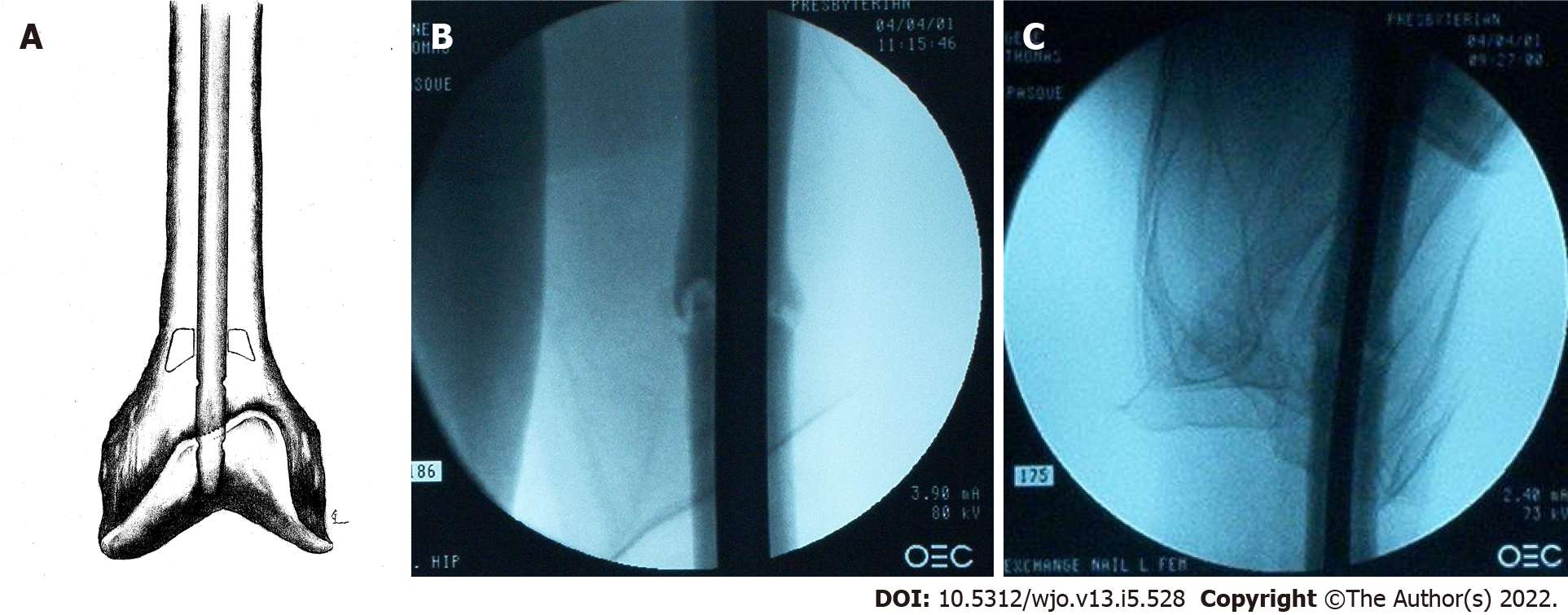
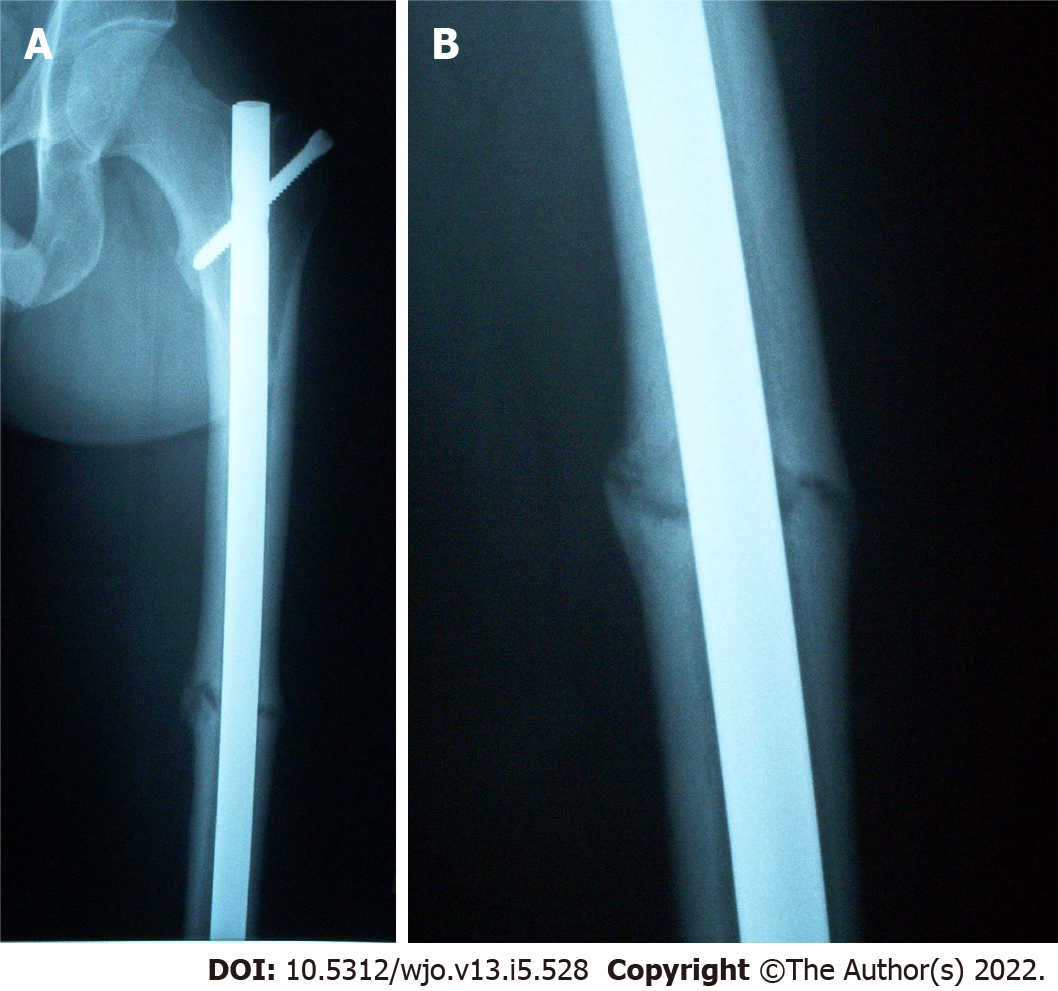
Post-operative radiographs from the outside hospital showed placement of 9 mm × 380 mm Russell-Taylor Delta II antegrade intramedullary nail through a left transverse mid-shaft femur fracture with single distal interlocking screw (Figure 1A and B). Radiographs obtained four months post-operatively at the outside hospital revealed breakage of the distal interlocking screw and no evidence of fracture union (Figure 2A and B). After presentation to our clinic, the decision was made to continue with normal weight bearing activity and obtain serial radiographs. Radiographs obtained 8 mo post-operatively continued to reveal no evidence of fracture union (Figure 3A and B).
Aseptic nonunion of left femoral shaft fracture.
The decision was made to proceed with exchange intramedullary nailing of the left femur.
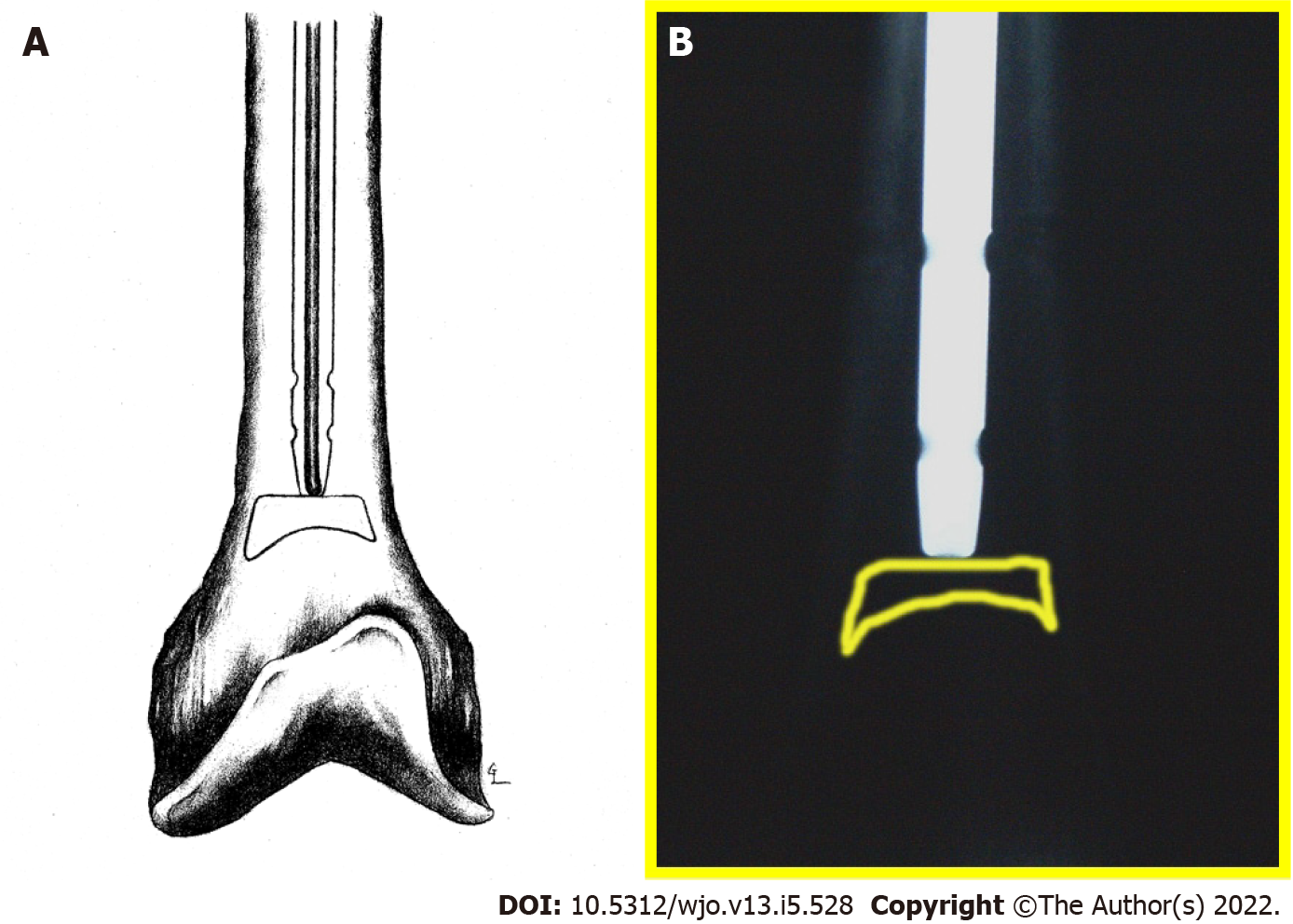
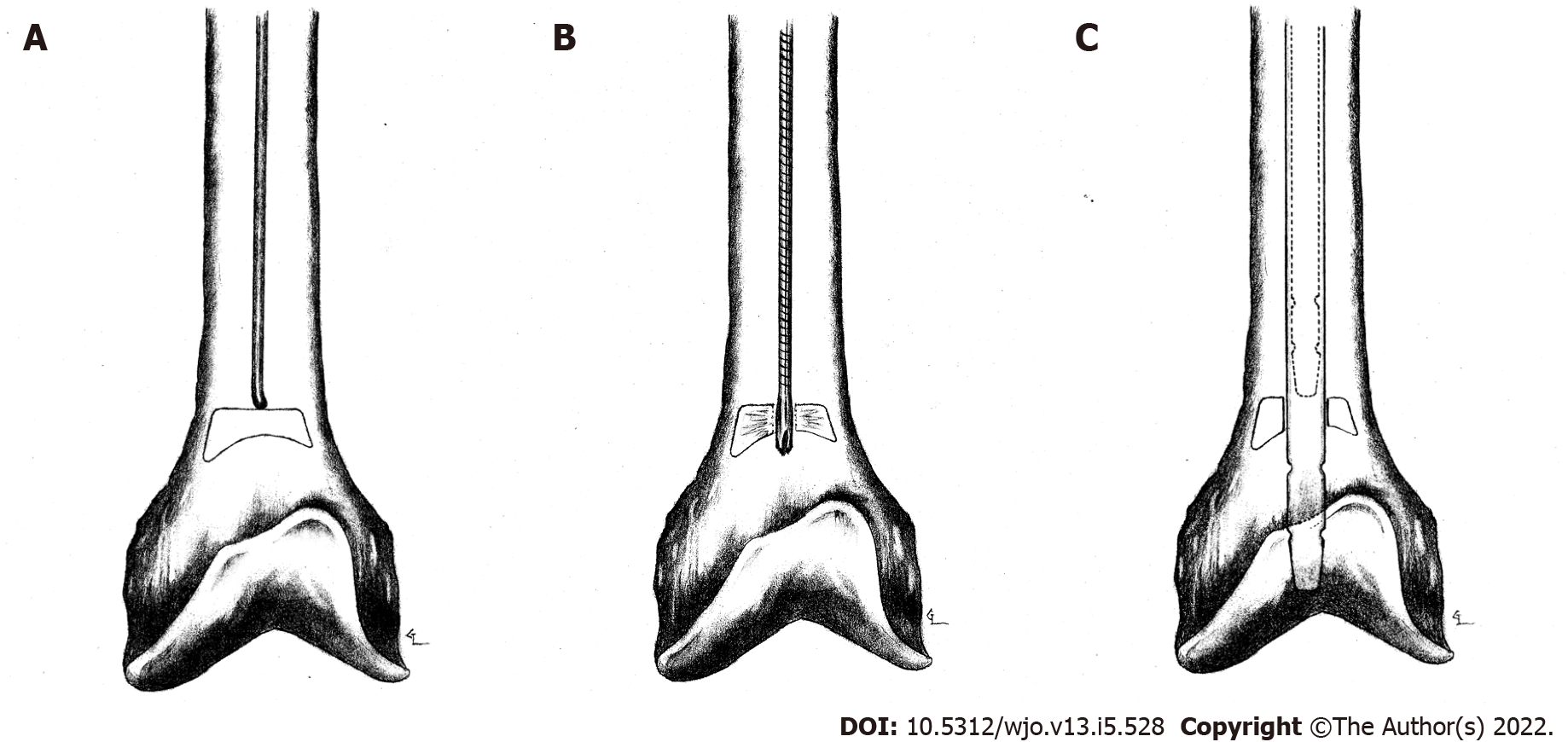
During nail extraction, attempts to pass a smooth-tip guide wire through the nail prior to removal were unsuccessful due to resistance at the nail tip (Figure 4A and B). The nail was subsequently removed with an appropriate nail extractor. Following nail removal, a standard guide wire was inserted into the canal without difficulty until it reached the point in the distal femur where the nail tip was previously seated. Again, the guide wire met resistance. Under magnified fluoroscopy, it appeared that there was a pedestal of cortical bone formation in the canal at this point (Figure 5A).
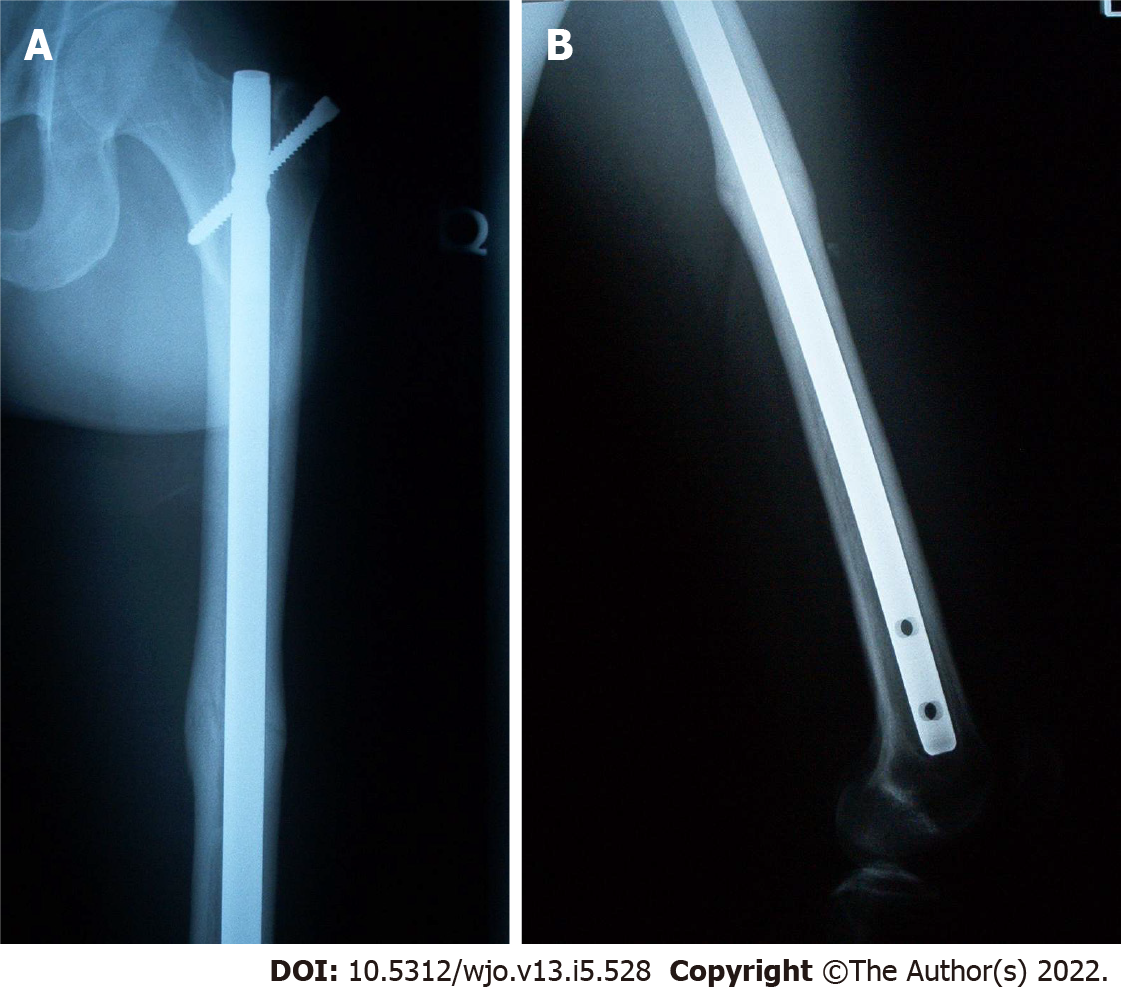
In order to breach the bony pedestal, the starting reamer was used to ream past the obstruction into the distal femoral meta-diaphyseal flare (Figure 5B). The ball-tip guide wire was then passed without difficulty to the physeal scar. The intramedullary canal was then reamed over the guide wire sequentially from 9 to 14 mm in 0.5 mm increments. The intramedullary reamings were saved for bone grafting and then inserted to the level of the fracture with the exchange tube. The bone graft was impacted using an 8 mm reamer at the fracture site. A 13 mm × 420 mm Russell-Taylor antegrade femoral nail was then inserted without difficulty. No distal locking screws were placed to allow fracture dynamization. Post-operative films showed adequate fracture reduction and placement of the intramedullary nail and proximal locking screw (Figure 6A-C). Figure 5C shows final nail placement (solid lines) compared to old, more proximal nail placement (dashed lines). Intra-operative cultures were subsequently negative.
At 1 year follow-up there was evidence of callus formation at the fracture site but not full cortical consolidation (Figure 7A and B). By 18 mo the fracture appeared well consolidated, and the patient had resolution of his thigh pain (Figure 8A and B).
Femoral shaft fracture nonunion is uncommon and is usually the result of aseptic etiologies. Nonunion following reamed antegrade intramedullary nail is a rare complication, occurring in 1%-2.2% of cases in early series[1-3]. In a recent systematic review of 38 studies involving 2829 femoral shaft fractures, Koso et al[4] found a 3.1% rate of nonunion after antegrade nail fixation and nonunion rates of 2.9% and 6.1% for reamed vs unreamed nail fixation, respectively.
There are numerous methods that may be used in the treatment of femur fracture nonunions. With infections, exchange intramedullary nailing should be performed after appropriate irrigation and debridement of the canal followed by an appropriate 4–6-wk course of parenteral or oral antibiotics. Some surgeons advocate a two-stage approach using antibiotic-impregnated beads or rods prior to final nail insertion. Aseptic nonunions may be treated with nail dynamization, exchange nailing (EN), or plate fixation. Several adjuncts may be employed in combination with these techniques, including bone-grafting, electrical stimulation, and bone morphogenetic protein or other bone growth supplements.
Fracture dynamization by distal locking screw removal is often attempted initially for delayed unions. This method provides the advantages of short procedure time with minimal soft-tissue dissection. Wu showed a 58% union rate with dynamization between 4 and 12 mo, but a high rate (21%) of femoral shortening of more than 2 cm[12]. In one meta-analysis, Vaughn et al[13] found a 66% (84/131) union rate with dynamization after nonunion though this rate increased to 82% (45/55) when treating delayed union. This provides evidence for the importance of close follow-up after intramedullary nailing as dynamization is most effective in the earlier windows of fracture healing. A review of the literature did not yield any reports of cases of post-dynamization union failure secondary to intramedullary bone pedestal formation.
The treatment of femoral diaphyseal fracture nonunion or delayed union of any etiology has been found to have a varied (53%-100%) rate of union following exchange reamed IM nail fixation (EN)[5,14-25]. Due to the infrequency of nonunion, most case series examining outcomes of EN are of relatively small cohorts (n < 105). The largest of these series showed rates of union from 86%-100%[14-21]. Some smaller (n = 19) series have shown lower rates of union from 53%-58%[22,23]. Of note, four studies (including three meta-analyses) comparing EN to other methods of treatment for nonunion found rates of union from 64%-86%[5,13,24,25]. Infected nonunions have been shown to have union rates up to 90%-100% with intramedullary nail fixation[26-28]. Despite some small studies reporting poor results, the majority of the literature supports EN as an effective and safe method of fixation.
Advantages of exchange intramedullary nailing include limited soft-tissue dissection and periosteal blood supply disruption, full post-operative weight-bearing, and early active rehabilitation. Complications include persistent nonunion, infection, and hardware failure[12,21,22,26]. Current recommendations call for over-reaming the canal 1-3 mm and replacing the extracted nail with one of a larger diameter[5,7,19-21,23].
Plating techniques are sometimes employed in treating nonunions when dynamization and/or exchange nailing have failed. When large bony defects are present and open bone-grafting techniques are employed, plating techniques are often preferred for stabilization. Union rates of 91%-100% are observed with various plating techniques after removal of the failed nail[29-31]. Several case series have shown excellent results in patients treated with augmentative plating (AP) with retained IM nail after femoral shaft fracture nonunion with mean union rate of 86%-100%[24,32-36]. Two recent meta-analyses have shown a significantly higher union rate following AP with retained IM nail when compared to EN alone. In a systematic review of 21 studies involving 448 cases of nonunion after IM nailing for femoral shaft fracture, Medlock et al[25] reports union rates of 99.8% (190/191) and 74% (190/257) for AP and EN, respectively. In another systematic review of 3 studies involving 232 nonunions, Luo et al[5] found union rates of 100% (113/113) and 86% (102/119) for AP and EN, respectively. Indications for AP include non-isthmic nonunion or isthmic nonunion with cortical defects or IM canal widening[37]. Advantages of AP over EN include lower rates of nonunion, shorter time to union, shorter operative time, and less intra-operative blood loss. Some of the disadvantages of plating include large soft tissue dissection, increased infection rate, and increased hardware failure.
Adjuncts to nonunion surgical interventions include bone-grafting, bone morphogenetic protein, electrical stimulation, and extracorporeal shock. When treating nonunion with AP, bone grafting is recommended and has been shown to produce excellent results with union rates of 88%-100%[24,29,32,35-37]. Bone grafting can be implemented through open or closed (intramedullary over-reaming) techniques with equivalent efficacy (100% union)[38]. Closed methods have a shorter time to union[12] . Open methods require harvest from the iliac crest or the tibial condyle. General indications for open grafting include atrophic nonunions, large bony defects (> 5 mm), and fracture malalignment[33,38].
Bai et al[39] obtained 16/17 fracture unions using plaster of Paris and bovine BMP composite implant at an average of 6 mo for femur fracture nonunion patients. In a systematic review comparing BMP and autologous grafting, Zhou et al[40] found BMP to have similar healing rates, improved limb function, and lower intraoperative blood loss, but with significantly higher hospitalization costs. While the literature on treatment of femoral nonunion with electrical stimulation is limited, electrical stimulation has shown some benefit for femur fractures[41], but is more commonly used and more successful with the treatment of tibia fracture nonunions[42].
There are several causes for the development of femoral shaft fracture nonunions following IM nail fixation and a number of methods to treat these complications. We propose a new etiology of delayed union or nonunion due to intramedullary cortical bone pedestal formation at the IM nail tip leading to failure of dynamization following distal locking screw removal. This complication may have been prevented with the use of a longer IM nail during the initial fixation or earlier dynamization. With the nail tip resting more distally in an area of increased intramedullary diameter, there would theoretically be a decreased opportunity for formation of an intramedullary pedestal of bone that could bridge the distance between the femoral cortices. Earlier dynamization would have also decreased the time available for bone pedestal consolidation within the femoral canal. If exchange intramedullary nailing is required, it is important to ream past the previous nail tip region to allow appropriate dynami
The strengths of this case report include radiographs of the clinical course, a detailed description of the surgical techniques with deviations required to overcome the encountered complication, a discussion of how to clinically manage and prevent such pathology, and a review of all available literature on clinical management of femoral shaft fracture nonunion after intramedullary nail fixation. Weaknesses include limited access to some of the patient files from the outside hospital.
This case presentation and literature review covers the most recent literature on causes of femur fracture nonunion and methods of revision after intramedullary nail fixation. We propose a new etiology for femur fracture nonunion caused by intramedullary bone pedestal formation leading to failure of dynamization after distal interlocking screw removal. Through the use of intramedullary nails of maximum length and close fracture follow-up with early intervention when delayed or nonunion of a fracture is suspected, this rare complication can be prevented.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hosseini MS, Iran; Wang YJ, China S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Karadimas EJ, Papadimitriou G, Theodoratos G, Papanikolaou A, Maris J. The effectiveness of the antegrade reamed technique: the experience and complications from 415 traumatic femoral shaft fractures. Strategies Trauma Limb Reconstr. 2009;4:113-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Winquist RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. 1984;66:529-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 637] [Cited by in RCA: 528] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 3. | Wolinsky PR, McCarty E, Shyr Y, Johnson K. Reamed intramedullary nailing of the femur: 551 cases. J Trauma. 1999;46:392-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 204] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 4. | Koso RE, Terhoeve C, Steen RG, Zura R. Healing, nonunion, and re-operation after internal fixation of diaphyseal and distal femoral fractures: a systematic review and meta-analysis. Int Orthop. 2018;42:2675-2683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 76] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 5. | Luo H, Su Y, Ding L, Xiao H, Wu M, Xue F. Exchange nailing versus augmentative plating in the treatment of femoral shaft nonunion after intramedullary nailing: a meta-analysis. EFORT Open Rev. 2019;4:513-518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Giannoudis PV, MacDonald DA, Matthews SJ, Smith RM, Furlong AJ, De Boer P. Nonunion of the femoral diaphysis. The influence of reaming and non-steroidal anti-inflammatory drugs. J Bone Joint Surg Br. 2000;82:655-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 198] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 7. | Hak DJ, Lee SS, Goulet JA. Success of exchange reamed intramedullary nailing for femoral shaft nonunion or delayed union. J Orthop Trauma. 2000;14:178-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 115] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Jeffcoach DR, Sams VG, Lawson CM, Enderson BL, Smith ST, Kline H, Barlow PB, Wylie DR, Krumenacker LA, McMillen JC, Pyda J, Daley BJ; University of Tennessee Medical Center, Department of Surgery. Nonsteroidal anti-inflammatory drugs' impact on nonunion and infection rates in long-bone fractures. J Trauma Acute Care Surg. 2014;76:779-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | Wheatley BM, Nappo KE, Christensen DL, Holman AM, Brooks DI, Potter BK. Effect of NSAIDs on Bone Healing Rates: A Meta-analysis. J Am Acad Orthop Surg. 2019;27:e330-e336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 118] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 10. | Taitsman LA, Lynch JR, Agel J, Barei DP, Nork SE. Risk factors for femoral nonunion after femoral shaft fracture. J Trauma. 2009;67:1389-1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Jiao H, Xiao E, Graves DT. Diabetes and Its Effect on Bone and Fracture Healing. Curr Osteoporos Rep. 2015;13:327-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 354] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 12. | Wu CC. The effect of dynamization on slowing the healing of femur shaft fractures after interlocking nailing. J Trauma. 1997;43:263-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 73] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Vaughn JE, Shah RV, Samman T, Stirton J, Liu J, Ebraheim NA. Systematic review of dynamization vs exchange nailing for delayed/non-union femoral fractures. World J Orthop. 2018;9:92-99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Furlong AJ, Giannoudis PV, DeBoer P, Matthews SJ, MacDonald DA, Smith RM. Exchange nailing for femoral shaft aseptic non-union. Injury. 1999;30:245-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 64] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Hierholzer C, Glowalla C, Herrler M, von Rüden C, Hungerer S, Bühren V, Friederichs J. Reamed intramedullary exchange nailing: treatment of choice of aseptic femoral shaft nonunion. J Orthop Surg Res. 2014;9:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Naeem-ur-Razaq M, Qasim M, Sultan S. Exchange nailing for non-union of femoral shaft fractures. J Ayub Med Coll Abbottabad. 2010;22:106-109. [PubMed] [DOI] [Full Text] |
| 17. | Oh I, Nahigian SH, Rascher JJ, Farrall JP. Closed intramedullary nailing for ununited femoral shaft fractures. Clin Orthop Relat Res. 1975;206-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Shroeder JE, Mosheiff R, Khoury A, Liebergall M, Weil YA. The outcome of closed, intramedullary exchange nailing with reamed insertion in the treatment of femoral shaft nonunions. J Orthop Trauma. 2009;23:653-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Webb LX, Winquist RA, Hansen ST. Intramedullary nailing and reaming for delayed union or nonunion of the femoral shaft. A report of 105 consecutive cases. Clin Orthop Relat Res. 1986;133-141. [PubMed] [DOI] [Full Text] |
| 20. | Wu CC, Chen WJ. Exchange nailing for aseptic nonunion of the femoral shaft. Int Orthop. 2002;26:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Swanson EA, Garrard EC, Bernstein DT, OʼConnor DP, Brinker MR. Results of a systematic approach to exchange nailing for the treatment of aseptic femoral nonunions. J Orthop Trauma. 2015;29:21-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Banaszkiewicz PA, Sabboubeh A, McLeod I, Maffulli N. Femoral exchange nailing for aseptic non-union: not the end to all problems. Injury. 2003;34:349-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Weresh MJ, Hakanson R, Stover MD, Sims SH, Kellam JF, Bosse MJ. Failure of exchange reamed intramedullary nails for ununited femoral shaft fractures. J Orthop Trauma. 2000;14:335-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 86] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Lai PJ, Hsu YH, Chou YC, Yeh WL, Ueng SWN, Yu YH. Augmentative antirotational plating provided a significantly higher union rate than exchanging reamed nailing in treatment for femoral shaft aseptic atrophic nonunion - retrospective cohort study. BMC Musculoskelet Disord. 2019;20:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | Medlock G, Stevenson IM, Johnstone AJ. Uniting the un-united: should established non-unions of femoral shaft fractures initially treated with IM nails be treated by plate augmentation instead of exchange IM nailing? Strategies Trauma Limb Reconstr. 2018;13:119-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 26. | Klemm KW. Treatment of infected pseudarthrosis of the femur and tibia with an interlocking nail. Clin Orthop Relat Res. 1986;174-181. [PubMed] [DOI] [Full Text] |
| 27. | Pradhan C, Patil A, Puram C, Attarde D, Sancheti P, Shyam A. Can antibiotic impregnated cement nail achieve both infection control and bony union in infected diaphyseal femoral non-unions? Injury. 2017;48 Suppl 2:S66-S71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Thonse R, Conway J. Antibiotic cement-coated interlocking nail for the treatment of infected nonunions and segmental bone defects. J Orthop Trauma. 2007;21:258-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 115] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 29. | Xing W, Pan Z, Sun L, Zhang C, Zhang Z, Feng W, Liu C. Sliding bone graft combined with double locking plate fixation for the treatment of femoral shaft nonunion. J Int Med Res. 2019;47:2034-2044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Peng Y, Ji X, Zhang L, Tang P. Double locking plate fixation for femoral shaft nonunion. Eur J Orthop Surg Traumatol. 2016;26:501-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 31. | Bellabarba C, Ricci WM, Bolhofner BR. Results of indirect reduction and plating of femoral shaft nonunions after intramedullary nailing. J Orthop Trauma. 2001;15:254-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 74] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 32. | Mittal KK, Gupta H, Kaushik N. Reunion of post nail aseptic non-union of diaphyseal femoral fractures by augmentation plating, decortication and bone grafting - Replacement for exchange nailing. Injury. 2021;52:1529-1533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (2)] |
| 33. | Ueng SW, Chao EK, Lee SS, Shih CH. Augmentative plate fixation for the management of femoral nonunion after intramedullary nailing. J Trauma. 1997;43:640-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 76] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 34. | Uliana CS, Bidolegui F, Kojima K, Giordano V. Augmentation plating leaving the nail in situ is an excellent option for treating femoral shaft nonunion after IM nailing: a multicentre study. Eur J Trauma Emerg Surg. 2021;47:1895-1901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 35. | Ru JY, Niu YF, Cong Y, Kang WB, Cang HB, Zhao JN. Exchanging reamed nailing versus augmentative compression plating with autogenous bone grafting for aseptic femoral shaft nonunion: a retrospective cohort study. Acta Orthop Traumatol Turc. 2015;49:668-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 36. | Choi YS, Kim KS. Plate augmentation leaving the nail in situ and bone grafting for non-union of femoral shaft fractures. Int Orthop. 2005;29:287-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 37. | Park J, Yang KH. Indications and outcomes of augmentation plating with decortication and autogenous bone grafting for femoral shaft nonunions. Injury. 2013;44:1820-1825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 38. | Wu CC, Chen WJ. Treatment of femoral shaft aseptic nonunions: comparison between closed and open bone-grafting techniques. J Trauma. 1997;43:112-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 40] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 39. | Kujala S, Raatikainen T, Ryhänen J, Kaarela O, Jalovaara P. Composite implant of native bovine bone morphogenetic protein (BMP) and biocoral in the treatment of scaphoid nonunions--a preliminary study. Scand J Surg. 2002;91:186-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 40. | Zhou YQ, Tu HL, Duan YJ, Chen X. Comparison of bone morphogenetic protein and autologous grafting in the treatment of limb long bone nonunion: a systematic review and meta-analysis. J Orthop Surg Res. 2020;15:288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 41. | Khalifeh JM, Zohny Z, MacEwan M, Stephen M, Johnston W, Gamble P, Zeng Y, Yan Y, Ray WZ. Electrical Stimulation and Bone Healing: A Review of Current Technology and Clinical Applications. IEEE Rev Biomed Eng. 2018;11:217-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 42. | Connolly JF. Selection, evaluation and indications for electrical stimulation of ununited fractures. Clin Orthop Relat Res. 1981;39-53. [PubMed] [DOI] [Full Text] |