Published online May 18, 2022. doi: 10.5312/wjo.v13.i5.444
Peer-review started: October 8, 2021
First decision: January 12, 2022
Revised: January 25, 2022
Accepted: April 29, 2022
Article in press: April 29, 2022
Published online: May 18, 2022
Processing time: 216 Days and 23.2 Hours
Subsidence is one of the concerning early complications in cementless femoral stem. Few publications have studied the influencing factors for subsidence in short cementless stems, due to their metaphyseal anchoring without diaphyseal invasion, they might demonstrate different subsidence patterns than with the conventional stems.
To analyze the factors associated with significant subsidence in short stems, including any radiographic parameters.
The digitized radiographs of 274 consecutive short stem total hip arthroplasties were retrospectively reviewed. Subsidence, neck-filling ratio (NFR), seating height and lateral stem contact were evaluated after a minimum of two years follow-up. A threshold of subsidence > 3 mm was considered a clinically significant migration.
For the entire cohort, subsidence occurred in 75 cases (27.4%) with the mean stem subsidence of 0.5 mm. (0-12.7, 1.68). Twelve hips (4.4%) had significant subsidence (> 3 mm). The univariate regression analysis demonstrated that age, diagnosis, BMI, Dorr’s type B, NFR, and seating height had no significant influence on significant subsidence, whereas insufficient lateral stem contact (≥ 1 mm) did have a statistically significant influence [Odds ratio (OR) = 5.02; 95%CI: 1.3-18.9; P = 0.017]. The multivariate regression analysis also demonstrated that insufficient lateral stem contact was a statistically significant influencing factor (OR = 5.5; 95%CI: 1.4-21.4; P = 0.014). There was no femoral stem revision for aseptic loosening in our cohort.
This study demonstrated that insufficient lateral stem contact was a statistically significant influencing factor on significant subsidence. Therefore, it is a particularly important step to create proper lateral cortical contact when performing the short stem total hip arthroplasty.
Core Tip: Short stem total hip arthroplasties (THAs) are commonly used in young and active patients. The advantages of these stems include more proximal load transfer which reduces stress shielding and, thigh pain, and they provide better options should revision surgery become necessary. Subsidence is one of the concerning complications in cementless femoral fixation. It is particularly important to identify the key intraoperative decision criteria to predict post-implantation subsidence of the short stem, which should be useful for choosing the proper size and position of the short stem and for allowance of early weight bearing post-operatively. This study demonstrated that insufficient lateral stem contact was a statistically significant influencing factor on significant subsidence. Therefore, it is a particularly important step to create proper lateral cortical contact when performing the short stem THA.
- Citation: Suksathien Y, Chuvanichanon P, Tippimanchai T, Sueajui J. Insufficient lateral stem contact is an influencing factor for significant subsidence in cementless short stem total hip arthroplasty. World J Orthop 2022; 13(5): 444-453
- URL: https://www.wjgnet.com/2218-5836/full/v13/i5/444.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i5.444
Cementless femoral stem in total hip arthroplasty (THA) is one of the most successful procedures in orthopaedic surgery[1]. Short stem THAs are commonly used in young and active patients. The advantages of these stems include more proximal load transfer which reduces stress shielding and, thigh pain, and they provide better options should revision surgery become necessary[2]. Short stem THA has shown excellent results in patients with primary osteoarthritis[3-5], osteonecrosis of the femoral head (ONFH)[6-9] and developmental dysplasia of the hip (DDH)[10,11] in many previous studies.
Subsidence is one of the concerning complications in cementless femoral fixation. It can lead to limb length discrepancy, decreased hip stability, or even implant failure. In conventional cementless stems, several previous studies have revealed the relationship between subsidence and stem survivorship[12,13], and some studies demonstrated the relationship between percentage of canal fill and subsidence[14,15]. However, few publications have studied the influencing factors for subsidence in short cementless stems, due to their metaphyseal anchoring without diaphyseal invasion, they might demonstrate different subsidence patterns than with the conventional stems. The purpose of this study is to analyze the factors associated with subsidence in short stems, including any radiographic parameters after a minimum of two years follow-up.
This research has been approved by the IRB of the authors’ affiliated institutions. The digitized radiographs of patients who had undergone short stem THA in our institute between January 2011 and December 2018 were retrospectively reviewed. According to previous study showed that the short stem subsided at the initial phase of about 3-6 mo after implantation and then no further subsidence was observed at two years follow-up[16]. Therefore, the inclusion criteria in this study were patients aged > 18 years with complete radiographic data at a minimum of two years follow-up. Because the Metha stem was designed for metaphyseal fitting without diaphyseal anchorage which suitable for patients with good bone quality, therefore, we excluded patients with osteoporotic bone. Patients with history of previous surgical treatment on the hip was also excluded.
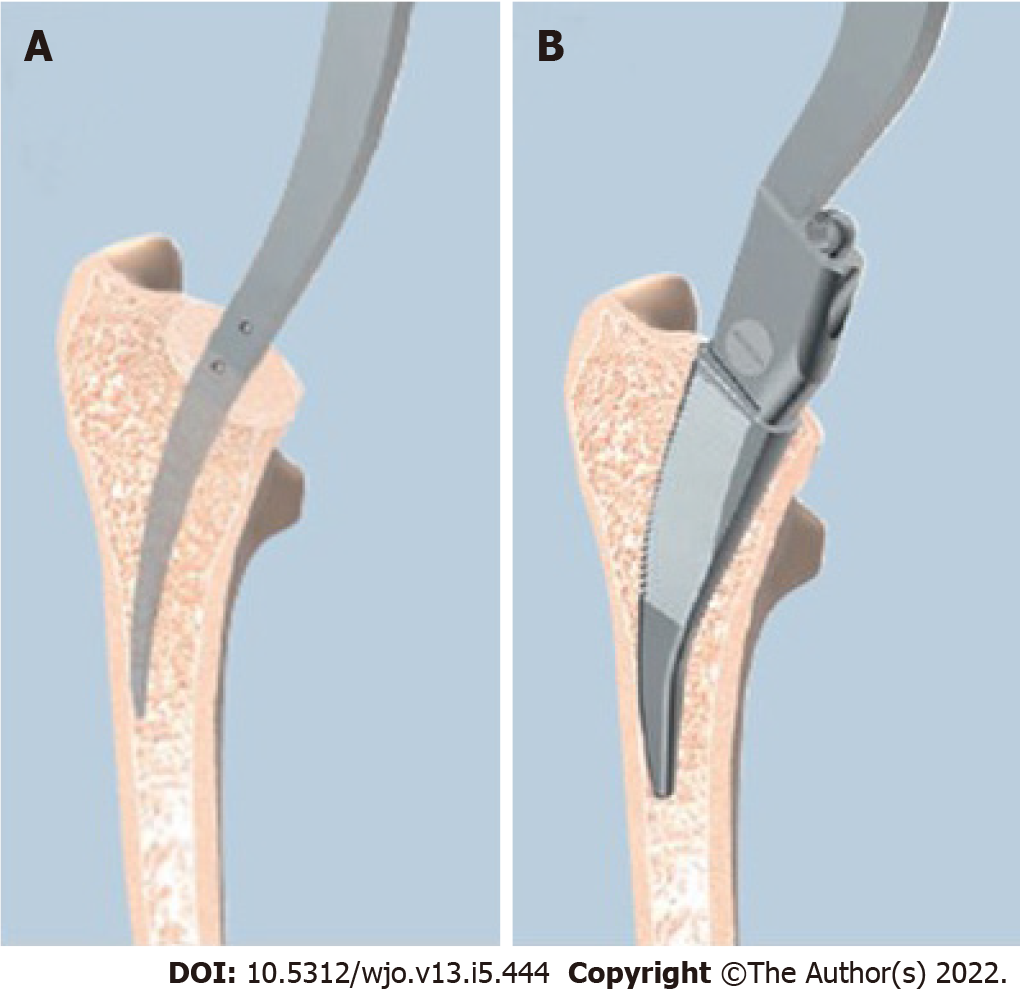
All THAs in this study were performed using Metha short stem by two experienced surgeons (Suksathien Y, Sueajui J), through a modified Hardinge approach. The Metha short stem is cementless, tapered, collarless, and made of titanium forged alloy (Ti6A14V) with suggested metaphyseal anchorage within the closed ring of the femoral neck. This stem is available in 5 sizes (0, 1, 2, 3 and 4) and 3 caput-column-diaphysis angles (120o, 130 o and 135 o). The Metha short stem is round coated with Plasmapore, a calcium phosphate layer, for osseointegration (Figure 1). In all cases the femoral neck was cut above the notch of the femoral neck at an angle of 50o to the femoral axis to create a closed cortical ring[17]. Intra-operative calcar cracks that occurred incidentally were routinely treated with cerclage wire. The Metha short stem was classified as type IIA according to Khanuja et al[18]; type I is femoral neck only, type II is calcar loading, type III is calcar loading with lateral flare, and type IV is shortened tapered stem. Additionally, type 2 stems are categorized into 4 subtypes: A, trapezoidal; B, round; C, threaded; and D, thrust plate. The cementless acetabular cup (Plasmafit, B.Braun Aesculap, Tuttlingen, Germany) with polyethelene liner (Vitelene, Vit E Stabilized Highly Crosslinked Polyethelene, B.Braun Aesculap, Tuttlingen, Germany) and metal head was used in all cases with the target angles for acetabular cup abduction and anteversion were 40° and 15° respectively. The femoral head diameter depended on cup size, 32 mm for cup diameter 50 mm or less, and 36 mm for cup diameter 52 mm or more.
Patients were allowed to stand and progress to full weight-bearing using crutches on the second post-operative day. The standard protocol for anteroposterior (AP) digital radiograph of both hips with both legs at 15° internal rotation and lateral cross-table, to control femoral stem rotation, was taken on the first post-operative day and at each follow-up radiograph. Patients were routinely contacted every three months in the first post-operative year and then every six months thereafter.
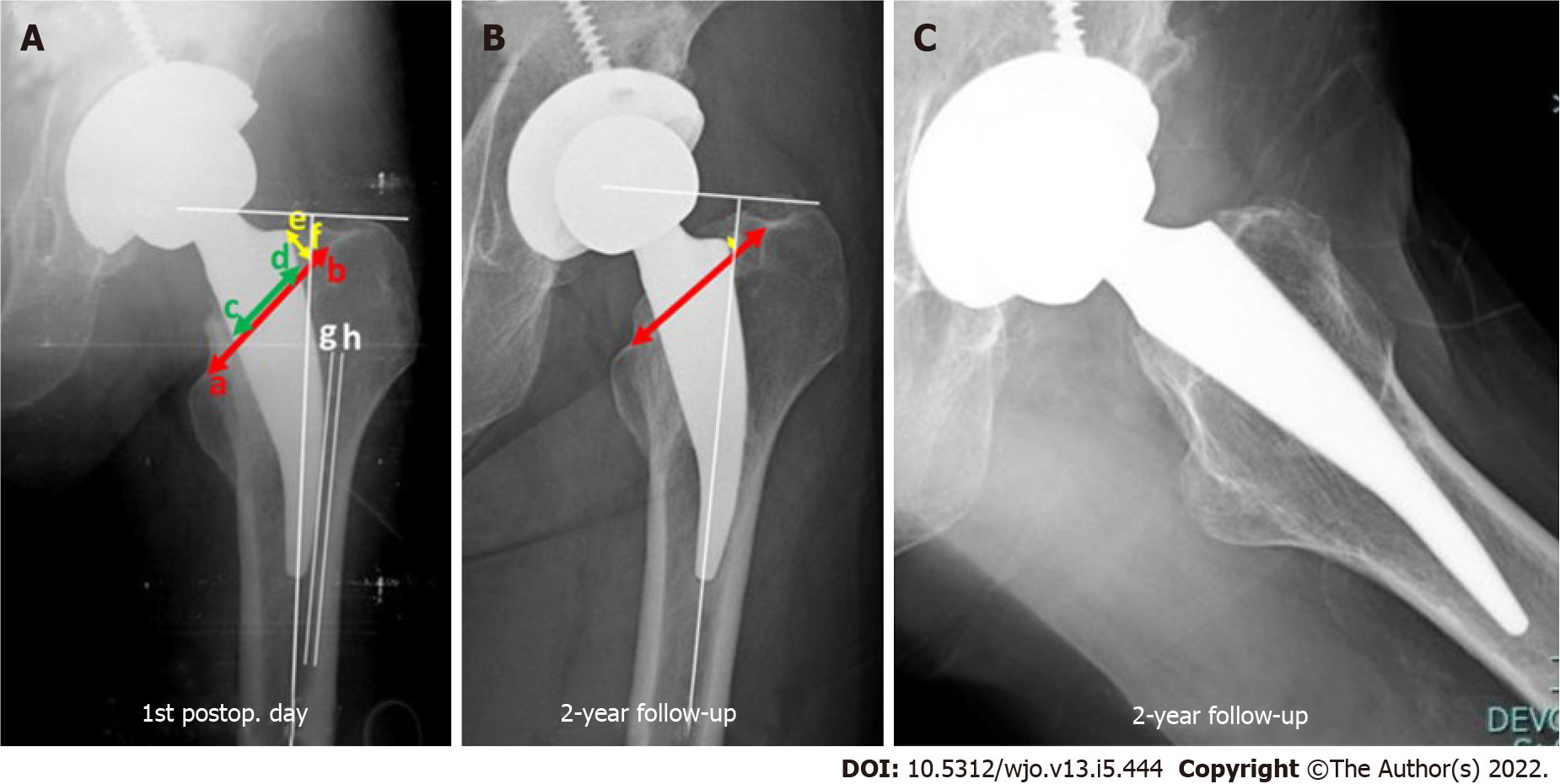
Pre-operative radiographs were assessed by using mediolateral cortical index as per Dorr et al[19]. Post-operative AP digital radiographs were calibrated with known femoral head size to minimize magnification error. The line from upper border of lessor trochanter to the notch of the femoral neck was defined as the base of femoral neck level. The Metha stem is designed for metaphyseal anchorage within the cortical ring of the femoral neck[17]; therefore, the neck-filling ratio (NFR) at the base of femoral neck level was defined, as the implant width divided by the distance from the inner cortex of the medial femoral neck to the inner cortex of the notch of the femoral neck. The distance from the shoulder point of the stem perpendicular to the base of the femoral neck level in millimeters was defined as the seating height of the femoral stem. Stem subsidence was calculated as the different distance from the shoulder point of the stem to the most prominent point of the greater trochanter between the first post-operative day and at two years follow-up by AP radiograph[20]. The subsidence threshold of more than 3 mm was considered as clinically significant subsidence[21,22]. A lateral stem contact was defined as the distance between the most lateral point of the stem and the inner lateral femoral cortex; a distance of less than 1 mm was defined as sufficient contact[23] (Figure 2).
Two independent observers (Tippimanchai T, Chuvanichanon P) measured each radiograph, and measurements were averaged into one final value after confirming that data reliability between the observers was sufficient. For the intra-observer reliability, the intraclass correlation coefficients (ICCs) for NFR were 0.85 (95%CI: 0.72-0.93) and 0.83 (95%CI: 0.68-0.91), for seating height they were 0.99 (95%CI: 0.99-0.99) and 0.98 (95%CI: 0.98-0.99), for lateral stem contact they were 0.98 (95%CI: 0.97-0.99) and 0.97 (95%CI: 0.95-0.99) and for subsidence they were 0.99 (95%CI: 0.99-0.99) and 0.99 (95%CI: 0.99-1.0) for observer 1 and observer 2, respectively. For the inter-observer reliability, the ICC for NFR was 0.77 (95%CI: 0.71-0.81), for seating height it was 0.99 (95%CI: 0.99-0.99), lateral stem contact was 0.97 (95%CI: 0.96-0.98), and subsidence was 0.99 (95%CI: 0.98-0.99) (Table 1).
| Neck-filling ratio | Seating height | Lateral stem contact | Subsidence | |
| Intra-observer | ||||
| Observer 1 | 0.85 (95%CI: 0.72-0.93) | 0.99 (95%CI: 0.99-0.99) | 0.98 (95%CI: 0.97-0.99) | 0.99 (95%CI: 0.99-0.99) |
| Observer 2 | 0.83 (95%CI: 0.68-0.91) | 0.98 (95%CI: 0.98-0.99) | 0.97 (95%CI: 0.95-0.99) | 0.99 (95%CI: 0.99-1.0) |
| Inter-observer | 0.77 (95%CI: 0.71-0.81) | 0.99 (95%CI: 0.99-0.99) | 0.97 (95%CI: 0.96-0.98) | 0.99 (95%CI: 0.98-0.99) |
The mean, SD, lowest and highest values, and ratio were used in the descriptive statistics of data. Mean subsidence between NFR < 0.8 and ≥ 0.8, seating height < 5 and ≥ 5 mm and lateral stem contact < 1 and ≥ 1 mm groups were compared using unpaired t-test. Univariate regression analysis was used to identify the factors related to significant subsidence including age (≥ 60 yr), diagnosis, body mass index (BMI) (≥ 30 kg/m2), Dorr’s type B, NFR (< 0.8)[24], seating height (< 5 mm)[17], and insufficient lateral stem contact (≥ 1 mm)[23]. Multivariate regression analysis was also conducted to assess the effect of insufficient lateral stem contact on significant subsidence. SPSS version 25.0 (SPSS Inc., Chicago, IL) was used for all statistical analyses with P < 0.05 defined as statistically significant.
There were 322 Metha stem THAs in the study period, 1 case died 1 year after surgery from a condition unrelated to the arthroplasty, 47 cases were lost before a minimum of two years follow-up, leaving 274 cases which including 186 males (67.9%) and 88 females (32.1%) to study. Their mean age was 48.1 years (range, 18-73 years) with a mean BMI of 23.8 (range, 14.7-40.9). There were 223 cases (81.4%) of Dorr’s type A and 51 cases (18.6%) of type B. The diagnoses included 213 cases (77.7%) of ONFH, 33 cases (12.1%) of DDH, 19 cases (6.9%) of primary osteoarthritis of the hip and 9 cases (3.3%) of femoral neck fractures (Table 2).
| Parameters | Values |
| No. of hips | 274 |
| Gender (male/female) | 186/88 |
| mean age (yr) (range, SD) | 48.1 (18-73, 11.2) |
| mean BMI (range, SD) (kg/m2) | 23.8 (14.7-40.9, 4.3) |
| Dorr’s classification, n (%) | |
| Dorr’s type A | 223 (81.4) |
| Dorr’s type B | 51 (18.6) |
| Diagnosis, n (%) | |
| ONFH | 213 (77.7) |
| DDH | 33 (12.1) |
| Primary osteoarthritis of the hip | 19 (6.9) |
| Femoral neck fracture | 9 (3.3) |
For the entire cohort, subsidence occurred in 75 cases (27.4%) with the mean stem subsidence of 0.5 mm. (0-12.7, 1.68). In most subsided cases the subsidence was occurred at the initial phase of about 3-6 mo after surgery and then no further subsidence was observed at two years follow-up. For the radiographic parameters, the mean subsidence of NFR < 0.8 and ≥ 0.8 groups were 0.5 mm. (0-11.89, 1.44) and 0.5 mm. (0-12.7, 2.02), of seating height < 5 and ≥ 5 mm groups were 0.51 mm. (0-12.7, 0.16) and 0.50 mm. (0-11.89, 0.11) respectively, there was no statistically significant difference with P = 0.99 in both compared groups. The mean subsidence of lateral stem contact < 1 and ≥ 1 mm groups were 0.39 mm. (0-11.89, 1.26) and 0.71 mm. (0-12.7, 1.94) respectively, there was no statistically significant difference (P = 0.09) (Table 3). Lateral cortical hypertrophy was detected on two years follow-up AP radiograph in 10 cases (5.03%) of non-subsided group and 3 cases (4%) in subsided group.
| Parameters (n) | Value, mean (mm) (range, SD) | P value |
| Subsidence of the entire cohort (75/274) | 0.5 (0-12.7, 1.68) | |
| Subsidence of any radiographic parameters | ||
| Neck-filling ratio < 0.8 (232) | 0.51 (0-11.89, 1.44) | 0.99 |
| Neck-filling ratio ≥ 0.8 (42) | 0.5 (0-12.7, 2.02) | |
| Seating height < 5 mm (110) | 0.51 (0-12.7, 0.16) | 0.99 |
| Seating height ≥ 5 mm (164) | 0.5 (0-11.89, 0.11) | |
| Lateral stem contact < 1 mm (178) | 0.39 (0-11.89, 1.26) | 0.09 |
| Lateral stem contact ≥ 1 mm (96) | 0.71 (0-12.7, 1.94) | |
Twelve hips (4.4%) had significant subsidence (> 3 mm) with the mean of 6.7 mm. (3.21-12.7), including 7 cases of Dorr’s type A and 5 cases of Dorr’s type B, 11 cases of ONFH and 1 case of DDH. The univariate regression analysis demonstrated that age, diagnosis, BMI, Dorr’s type B, NFR, and seating height had no significant influence on significant subsidence, whereas insufficient lateral stem contact did have a statistically significant influence [Odds ratio (OR) = 5.02; 95%CI: 1.3-18.9; P = 0.017] (Table 4). The multivariate regression analysis also demonstrated that insufficient lateral stem contact was a statistically significant influencing factor (OR = 5.5; 95%CI: 1.4-21.4; P = 0.014). The intra-operative calcar crack incidence was 6.6% (18/274) and all were treated with cerclage wire with no further subsidence.
| Variables | Univariate analysis | ||
| OR | 95%CI | P value | |
| Age (≥ 60 yr) | 0.96 | 0.2-4.6 | 0.96 |
| DDH | 0.65 | 0.1-5.2 | 0.69 |
| ONFH | 3.3 | 0.4-25.8 | 0.26 |
| BMI (≥ 30 kg/m2) | 0.95 | 0.1-7.6 | 0.96 |
| Dorr’s type B | 2.29 | 0.6-7.9 | 0.19 |
| Seating height (< 5 mm) | 0.91 | 0.3-2.9 | 0.87 |
| NFR (< 0.8) | 1.98 | 0.2-15.7 | 0.52 |
| Insufficient lateral stem contact (≥ 1 mm) | 5.02 | 1.3-18.9 | 0.0171 |
At the latest follow-up, there were 3 cases of revision. One case of femoral stem revision due to periprosthetic fracture, 4 years after index surgery from trauma, we revised using conventional stem with plate and screws and there were 2 cases of cup revision due to aseptic loosening, 2 and 5 years after index surgery. There was 1 case of significant subsidence (5.6 mm) with posterior dislocation, 5 years after index surgery from minor trauma, which was successfully treated with closed reduction. There was no femoral stem revision for aseptic loosening in our cohort.
Subsidence is one of the concerning early complications when using the cementless short stem. In this study we found subsidence occurred in 75 cases (27.4%) with the mean stem subsidence for the entire cohort of 0.5 mm, (0-12.7, 1.68), a finding consistent with Jahnke et al[24], who demonstrated mean subsidence of 1.01 ± 1.27 mm (0.05-8.23) at two years follow-up. Schwarze et al[25] also showed the mean subsidence of 0.86 mm with two years follow-up using Metha stem. Different results of subsidence at two years follow-up were reported from many previous studies[23-30] using different types of short stem according to Khanuja et al[18]. Klein et al[31] who studied short stem with collar, CFP stem (LINK, Germany) (type IIB), demonstrated that the mean subsidence was 0.3 mm (0.2-0.4) at two years follow-up (Table 5).
| Ref. | Femoral stem | Khanuja et al[18] classification | Follow-up (mo) | Subsidence(mm) | n |
| Christiansen et al[26] | Primoris, Biomed, UK | 1 | 24 | 0.38 | 50 |
| Schwarze et al[25] | Metha, Aesculap, Germany | 2A | 24 | 0.86 | 39 |
| Jahnke et al[24] | Metha, Aesculap, Germany | 2A | 24 | 1.28 ± 2.24 | 71 |
| This study | Metha, Aesculap, Germany | 2A | 24 | 0.5 | 274 |
| Budde et al[27] | Nanos, Smith + nephew, Germany | 2A | 24 | 0.46 ± 0.31 | 18 |
| Ferguson et al[28] | MiniHip, Corin, UK | 2A | 24 | 0.26 | 20 |
| Kutzner et al[23] | Optimys, Mathys AG, Switzerland | 2B | 24 | 1.23 (contact); 2.07 (non-contact) | 191 |
| Klein et al[31] | CFP, Link, Germany | 2B | 24 | 0.3 (0.2-0.4) | 39 |
| Mahmoud et al[29] | Proxima, DePuy, UK | 3 | 24 | 0.22 | 28 |
| Acklin et al[30] | Fitmore, Zimmer, Switzerland | 4 | 24 | 0.39 | 24 |
It is particularly important to identify the key intraoperative decision criteria to predict post-implantation subsidence of the short stem, which should be useful for choosing the proper size and position of the short stem and for allowance of early weight bearing post-operatively. In this study we demonstrated that the insufficient lateral stem contact group (≥ 1 mm) seemed to have higher subsidence than the sufficient lateral stem contact group (< 1 mm) in the entire cohort, but did not reach statistical significance (P = 0.09). For significant subsidence cohort, the only significant influencing factor was insufficient lateral stem contact, the univariate and multivariate regression analyses showed statistical significance, (OR = 5.02; 95%CI: 1.3-18.9; P = 0.017) and (OR = 5.5; 95%CI: 1.4-21.4; P = 0.014) respectively. This is consistent with Kutzner et al[23], whose study using Optimys stem (type IIB according to Khanuja et al[18]), demonstrated that the mean subsidence was significantly higher in the no-contact group (≥ 1 mm) (2.07 mm, range -7.7 to 1.7) than in the sufficient lateral contact group (< 1 mm) (1.23 mm, range -4.5 to 1.8) at five years follow-up. According to our findings, sufficient lateral contact should always be the intra-operative aim when using Metha short stem. It is a particularly important step that when starting to prepare the femoral stem with a curved awl, the surgeon should carefully check that it be in contact with the lateral cortical bone, then followed by rasping in the same direction until reaching the designed femoral size (Figure 3). Therefore, intra-operative fluoroscopy might be considered mandatory in some cases with doubtful lateral contact. Nevertheless, if post-operative radiographs show that the patient has insufficient lateral contact, initial partial weight bearing should be recommended for preventing stem subsidence.
Some studies have demonstrated the relationship between percentage of canal fill and subsidence in conventional cementless stems[14,15]. In short stems, Jahnke et al[24] studied fit and fill ratios in 40 patients using Metha stem with one year follow-up. They found 100% of cases had a tight fit and fill ratio (≥ 0.8) at the proximal level, and the mean subsidence in the whole cohort of their study was 1.28 ± 2.24 mm. In our own study, we could not find a significant correlation between NFR (< 0.8) and significant subsidence (OR = 1.98; 95%CI: 0.2-15.7; P = 0.52). One possible explanation might be that we found the cortical ring of the femoral neck in some patients had a flat oval shape, with the result that the proximal stem had stable fixation with the anterior and posterior neck, instead of mediolateral.
The seating height was also not a significant influencing factor for significant subsidence in this study (OR = 0.91; 95%CI: 0.3-2.9; P = 0.87). Consistent with Floerkemeier et al[17], who studied synthetic bone using Metha stem and demonstrated that the deeper the resection, the more similar the strain patterns when compared to a non-implanted synthetic bone.
In our cohort, age (≥ 60 yrs.), diagnosis, BMI (≥ 30 kg/m2), and Dorr’s type B had no statistically significant influence on significant subsidence. Interestingly, patients with ONFH and Dorr’s type B seemed to have higher chance of having significant subsidence, but did not reach statistical significance, (OR = 3.3; 95%CI: 0.4-25.8; P = 0.26) and (OR = 2.29; 95%CI: 0.6-7.9; P = 0.19) respectively. Similar to Schaer et al[32] who studied Optimys stem (type IIB according to Khanuja et al[18]) with subsidence of 2.04 ± 1.42 mm at five years follow-up, reported that age (≥ 65 yrs.), BMI (≥ 30 kg/m2), and Dorr’s type B did not have a statistically significant impact on the amount of stem subsidence.
Press-fit is one of the key factors for stability of cementless stems. The surgeon is guided by visual, sensory, and auditory clues during insertion of the short stem; a good balance between perfect press-fit level and not fracturing the calcar remains challenging. In this study, the incidence of intra-operative calcar crack was 6.6% (18/274) and all cases were treated with cerclage wire with no further subsidence. We believe this was because of the relatively narrow neck diameter of patients in our country. As in our previous mid-term study of Metha short stem in patients with ONFH, Suksathien et al[9] reported 4.8% of intra-operative calcar crack treated with cerclage wire without any complication. Lateral cortical hypertrophy was detected in both non-subsided and subsided groups at two yeas follow-up, 10 cases (5.03%) and 3 cases (4%) respectively. This finding demonstrated that lateral cortical hypertrophy had no influence for stem subsidence. In most subsided cases the subsidence was occurred at the initial phase of about 3-6 mo after surgery and then no further subsidence was observed at two years follow-up.
This study had some limitations. First, we used digital radiographs to measure all radiographic parameters, which is less accurate than radiostereometric analysis. Nevertheless, the aim of this study was to describe intraoperative key decision criteria with respect to proper positioning of short stems, that are suitable for intraoperative use by all surgeons, solely by performing intraoperative fluoroscopy, and post-operative radiographic evaluation of influencing factors to prevent stem subsidence. Second, our cohort was a consecutive study of Metha stem, which was classified as type IIA according to Khanuja et al[18], the surgical technique for femoral preparation might be different from type I, III and IV. Third, there were many patients which loss before two years follow-up in our cohort, most of them were young workers, after fully recovery from THAs they moved to work in any remote area which unable to contact. However, there was no record of any complication at their last follow-up. Fourth, our cohort was relatively small which we had only 12 cases with significant subsidence to analyze, resulting in a relatively low power to detect statistically significant difference. Finally, this study was a single institute experience; different outcomes might have been obtained by different surgeons with varying levels of experience in any type of short stem THA.
In the entire cohort, we found higher subsidence in insufficient lateral stem contact group than in sufficient group, but did not reach statistical significance. In significant subsidence cohort, the only statistically significant influencing factor for significant subsidence was insufficient lateral stem contact. Therefore, it is a particularly important step to create proper lateral cortical contact when performing the Metha stem THA and intra-operative fluoroscopy should be considered mandatory in some cases with doubtful lateral contact. Initial partial weight bearing should be recommended in patients whose post-operative radiographs demonstrate insufficient lateral cortical contact for preventing stem subsidence.
Many previous studies have shown satisfactory results using conventional total hip arthroplasty (THA), there may have some clinical problems related to proximodistal dimensional mismatch, thigh pain, stress shielding, periprosthetic fracture and difficulty during removal when revision is necessary. In an effort to reduce these problems, short-stem THA was developed, because the short stem has a metaphyseal fitting and no diaphyseal anchoring, so these problems may be minimized.
Few publications have studied the influencing factors for subsidence in short cementless stems, due to their metaphyseal fitting without diaphyseal anchoring, they might demonstrate different subsidence patterns than with the conventional stems.
This study aimed to analyze the influencing factors with subsidence in short stems.
Retrospectively reviewed the digitized radiographs of 274 consecutive short stem total hip arthroplasties. Subsidence, neck-filling ratio, seating height and lateral stem contact were evaluated after a minimum of two years follow-up. A threshold of subsidence > 3 mm was considered a clinically significant subsidence.
In this study we demonstrated that the insufficient lateral stem contact group (≥ 1 mm) seemed to have higher subsidence than the sufficient lateral stem contact group (< 1 mm) in the entire cohort, but did not reach statistical significance. For significant subsidence cohort, the only significant influencing factor was insufficient lateral stem contact, the univariate and multivariate regression analyses showed statistical significance.
Insufficient lateral stem contact was a statistically significant influencing factor on significant subsidence when using short stem. Therefore, it is a particularly important step to create proper lateral cortical contact when performing the Metha stem THA.
Long term follow-up for this study group will be the next study.
The authors wish to acknowledge Dr. Urawit Piyapromdee MD, for assisting with the statistical analysis and gratefully thank Mr. Jason Cullen for the careful proofreading of the manuscript.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hooper GJ, New Zealand; Prudhon JL, France S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1477] [Cited by in RCA: 1786] [Article Influence: 99.2] [Reference Citation Analysis (0)] |
| 2. | Floerkemeier T, Schwarze M, Hurschler C, Gronewold J, Windhagen H, von Lewinski G, Budde S. The Influence of Tribological Pairings and Other Factors on Migration Patterns of Short Stems in Total Hip Arthroplasty. Biomed Res Int. 2017;2017:8756432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Kamada S, Naito M, Nakamura Y, Shitama T. Total hip arthroplasty using a short stem, stem design, position and size influence the development of bone trabeculae and appearance of radiolucent lines around the stem. Curr Orthop Pract. 2011;22:52-58. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Simank HG, Greiner R. Clinical and radiographic short to midterm results with the short hip stem prosthesis “Metha” in 120 cases. J Orthopaedics. 2010;7:e8. |
| 5. | Wittenberg RH, Steffen R, Windhagen H, Bücking P, Wilcke A. Five-year results of a cementless short-hip-stem prosthesis. Orthop Rev (Pavia). 2013;5:e4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Capone A, Bienati F, Torchia S, Podda D, Marongiu G. Short stem total hip arthroplasty for osteonecrosis of the femoral head in patients 60 years or younger: a 3- to 10-year follow-up study. BMC Musculoskelet Disord. 2017;18:301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Floerkemeier T, Tscheuschner N, Calliess T, Ezechieli M, Floerkemeier S, Budde S, Windhagen H, von Lewinski G. Cementless short stem hip arthroplasty METHA® as an encouraging option in adults with osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2012;132:1125-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Kim YH, Park JW. Ultra-Short Anatomic Uncemented Femoral Stem and Ceramic-on-Ceramic Bearing in Patients With Idiopathic or Ethanol-Induced Femoral Head Osteonecrosis. J Arthroplasty. 2020;35:212-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Suksathien Y, Sueajui J. Mid-term results of short stem total hip arthroplasty in patients with osteonecrosis of the femoral head. Hip Int. 2019;29:603-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Buttaro MA, Slullitel PA, Zanotti G, Comba FM, Piccaluga F. Is a short stem suitable for patients with hip dysplasia? Hip Int. 2018;28:315-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Suksathien Y, Tippimanchai T, Akkrasaeng T, Ruangboon C. Mid-term results of short-stem total hip arthroplasty in patients with Crowe type I and II developmental dysplasia of the hip. Eur J Orthop Surg Traumatol. 2021;31:319-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Grant TW, Lovro LR, Licini DJ, Warth LC, Ziemba-Davis M, Meneghini RM. Cementless Tapered Wedge Femoral Stems Decrease Subsidence in Obese Patients Compared to Traditional Fit-and-Fill Stems. J Arthroplasty. 2017;32:891-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 13. | Ries C, Boese CK, Dietrich F, Miehlke W, Heisel C. Femoral stem subsidence in cementless total hip arthroplasty: a retrospective single-centre study. Int Orthop. 2019;43:307-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 75] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 14. | Streit MR, Haeussler D, Bruckner T, Proctor T, Innmann MM, Merle C, Gotterbarm T, Weiss S. Early Migration Predicts Aseptic Loosening of Cementless Femoral Stems: A Long-term Study. Clin Orthop Relat Res. 2016;474:1697-1706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 69] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 15. | Warth LC, Grant TW, Naveen NB, Deckard ER, Ziemba-Davis M, Meneghini RM. Inadequate Metadiaphyseal Fill of a Modern Taper-Wedge Stem Increases Subsidence and Risk of Aseptic Loosening: Technique and Distal Canal Fill Matter! J Arthroplasty. 2020;35:1868-1876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 16. | Kutzner KP, Pfeil D, Kovacevic MP, Rehbein P, Mai S, Siebert W, Pfeil J. Radiographic alterations in short-stem total hip arthroplasty: a 2-year follow-up study of 216 cases. Hip Int. 2016;26:278-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Floerkemeier T, Gronewold J, Berner S, Olender G, Hurschler C, Windhagen H, von Lewinski G. The influence of resection height on proximal femoral strain patterns after Metha short stem hip arthroplasty: an experimental study on composite femora. Int Orthop. 2013;37:369-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Khanuja HS, Banerjee S, Jain D, Pivec R, Mont MA. Short bone-conserving stems in cementless hip arthroplasty. J Bone Joint Surg Am. 2014;96:1742-1752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 151] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 19. | Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993;14:231-242. [PubMed] |
| 20. | Jahnke A, Wiesmair AK, Fonseca Ulloa CA, Ahmed GA, Rickert M, Ishaque BA. Outcome of short- to medium-term migration analysis of a cementless short stem total hip arthroplasty using EBRA-FCA: a radiological and clinical study. Arch Orthop Trauma Surg. 2020;140:247-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Kim YH, Kim JS, Joo JH, Park JW. A prospective short-term outcome study of a short metaphyseal fitting total hip arthroplasty. J Arthroplasty. 2012;27:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 22. | Albers A, Aoude AA, Zukor DJ, Huk OL, Antoniou J, Tanzer M. Favorable Results of a Short, Tapered, Highly Porous, Proximally Coated Cementless Femoral Stem at a Minimum 4-Year Follow-Up. J Arthroplasty. 2016;31:824-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Kutzner KP, Freitag T, Bieger R. Defining 'undersizing' in short-stem total hip arthroplasty: the importance of sufficient contact with the lateral femoral cortex. Hip Int. 2022;32:160-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 24. | Jahnke A, Engl S, Seeger JB, Basad E, Rickert M, Ishaque BA. Influences of fit and fill following hip arthroplasty using a cementless short-stem prosthesis. Arch Orthop Trauma Surg. 2015;135:1609-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Schwarze M, Budde S, von Lewinski G, Windhagen H, Keller MC, Seehaus F, Hurschler C, Floerkemeier T. No effect of conventional vs. minimally invasive surgical approach on clinical outcome and migration of a short stem total hip prosthesis at 2-year follow-up: A randomized controlled study. Clin Biomech (Bristol, Avon). 2018;51:105-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Christiansen JD, Ejaz A, Nielsen PT, Laursen M. An Ultra-Short Femoral Neck-Preserving Hip Prosthesis: A 2-Year Follow-up Study with Radiostereometric Analysis and Dual X-Ray Absorptiometry in a Stepwise Introduction. J Bone Joint Surg Am. 2020;102:128-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Budde S, Seehaus F, Schwarze M, Hurschler C, Floerkemeier T, Windhagen H, Noll Y, Ettinger M, Thorey F. Analysis of migration of the Nanos® short-stem hip implant within two years after surgery. Int Orthop. 2016;40:1607-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 28. | Ferguson RJ, Broomfield JA, Malak TT, Palmer AJR, Whitwell D, Kendrick B, Taylor A, Glyn-Jones S. Primary stability of a short bone-conserving femoral stem: a two-year randomized controlled trial using radiostereometric analysis. Bone Joint J. 2018;100-B:1148-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 29. | Mahmoud AN, Kesteris U, Flivik G. Stable migration pattern of an ultra-short anatomical uncemented hip stem: a prospective study with 2 years radiostereometric analysis follow-up. Hip Int. 2017;27:259-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Acklin YP, Jenni R, Bereiter H, Thalmann C, Stoffel K. Prospective clinical and radiostereometric analysis of the Fitmore short-stem total hip arthroplasty. Arch Orthop Trauma Surg. 2016;136:277-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Klein LJ, Puretic G, Mohaddes M, Kärrholm J. Similar clinical results and early subsidence between the Collum Femoris Preserving and the Corail stem: a randomized radiostereometric study of 77 hips with 2 years' follow-up. Acta Orthop. 2019;90:202-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Schaer MO, Finsterwald M, Holweg I, Dimitriou D, Antoniadis A, Helmy N. Migration analysis of a metaphyseal-anchored short femoral stem in cementless THA and factors affecting the stem subsidence. BMC Musculoskelet Disord. 2019;20:604. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (1)] |