Published online Apr 18, 2022. doi: 10.5312/wjo.v13.i4.400
Peer-review started: August 10, 2021
First decision: November 17, 2021
Revised: December 2, 2021
Accepted: March 7, 2022
Article in press: March 7, 2022
Published online: April 18, 2022
Processing time: 244 Days and 17.5 Hours
Current literature shows no clear answer on the question how to manage the capsule after hip arthroscopy. Regarding patient reported outcome measures there seems to be no difference between capsular repair or unrepaired capsulotomy.
To evaluate and compare the integrity of the hip capsule measured on a magnetic resonance imaging (MRI) scan after capsular repair or unrepaired capsulotomy.
A case series study was performed; a random sample of patients included in a trial comparing capsular repair vs unrepaired capsulotomy had a postoperative MRI scan. The presence of a capsular defect and gap size were independently evaluated on MRI.
A total of 28 patients (29 hips) were included. Patient demographics were comparable between treatment groups. There were 2 capsular defects in the capsular repair group and 7 capsular defects in the unrepaired capsulotomy group (P = 0.13). In the group of patients with a defect, median gap sizes at the acetabular side were 5.9 mm (range: 2.7-9.0) in the repaired and 8.0 mm (range: 4.5-18.0) in the unrepaired group (P = 0.462). At the muscular side gap sizes were 6.6 mm (range: 4.1-9.0) in the repaired group and 11.5 mm (range: 3.0-18.0) in the unrepaired group (P = 0.857). The calculated Odds ratio (OR) for having a capsular defect with an increasing lateral center-edge (CE) angle was 1.12 (P = 0.06). The OR for having a capsular defect is lower in the group of patients that underwent a labral repair with an OR of 0.1 (P = 0.05).
There is no significant difference in capsular defects between capsular repair or unrepaired capsulotomy. Regarding clinical characteristics our case series shows that a larger CE angle increases the likelihood of a capsular defect and the presence of a labral repair decreases the likelihood of a capsular defect.
Core Tip: In this case series we evaluated the integrity of the hip capsule after hip arthroscopy with a magnetic resonance imaging scan and compared between patients in a capsular repair group and unrepaired capsulotomy group. The magnetic resonance imaging scan of 29 hips was observed to determine whether there was a capsular defect or not. After 12 mo follow-up no difference was found between groups regarding the presence of a capsular defect or not.
- Citation: Bech NH, van Dijk LA, de Waard S, Vuurberg G, Sierevelt IN, Kerkhoffs GM, Haverkamp D. Integrity of the hip capsule measured with magnetic resonance imaging after capsular repair or unrepaired capsulotomy in hip arthroscopy. World J Orthop 2022; 13(4): 400-407
- URL: https://www.wjgnet.com/2218-5836/full/v13/i4/400.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i4.400
Hip arthroscopy is a more and more popular technique to address intra-articular pathology of the hip[1,2]. Entrance to the hip is made by several portals and usually an interportal or T-shaped capsulotomy is performed to improve workspace in the joint[3]. In the early days of hip arthroscopy these capsulotomies were usually left unrepaired[4]. In recent years there has been debate on what to do with the capsulotomy at the end of the procedure. Some papers suggest that routine capsular closure might result in improved outcomes after surgery where other papers report conflicting evidence and show no superiority of routine capsular repair[5-10]. However, there are cadaveric studies that show the biomechanical importance of complete capsular repair[11,12]. Restoration of the hip joint capsule results in hip joint kinematics to near normal levels after interportal or T-shaped capsulotomy[12]. The unrepaired hip capsulotomy might be a reason for developing postoperative iatrogenic hip instability[13,14]. As the (un)repaired capsulotomy might be a contributor to postoperative complaints of patients with iatrogenic hip instability, this may be quantified by assessment of the quality and morphologic appearance of the hip capsule with magnetic resonance imaging (MRI)[15].
The purpose of this study is to evaluate the integrity of the hip capsule after capsular repair or unrepaired capsulotomy measured with MRI. Our secondary aim is to evaluate the association between pre- and perioperative details and the quality and integrity of the capsule.
For the current study a random sample of 28 patients (29 hips) with residual hip complaints after surgery or complaints of the contralateral hip had an MRI scan postoperatively and were enrolled in the current study. All patients were part of a trial that was designed and approved after local medical ethical committee approval (NL55669.048.15). Inclusion criteria for the trial were age between 18-65 years, a body mass index (BMI) lower than 35 and good understanding of Dutch/English language and with intra-articular hip pathology who opt for hip arthroscopy. Exclusion criteria were revision hip arthroscopy, extra-articular hip pathology, a documented systemic connective tissue disease or hypermobility, a center-edge (CE) angle of less than 25 degrees, prior hip surgery or a hip fracture in the past. After randomization patients were either allocated to repaired capsulotomy or the unrepaired capsulotomy group. All patients were operated by the senior author. Functional outcome was measured at baseline and after 12 mo follow-up with the Copenhagen Hip and Groin Outcome Score (HAGOS)[16].
The postoperative MRI scans were independently evaluated for capsular integrity by Bech NH and Haverkamp D to assess inter observer reliability. Both authors were blinded to clinical and detailed operative information to prevent bias.
Final cohort consisted of 29 hips (28 patients) of which 16 were in the unrepaired group and 13 in the capsular repair (repair) group that had received a postoperative MRI scan.
Patients were operated via standard technique and 2 or 3 portals were made. An interportal capsulotomy was done in all patients. No T-shaped capsulotomies were done. Repair of the capsule took approximately 15 min of operating time. The capsular repair was done with 2 or 3 sutures by arthroscopic technique (Capsular Close Scorpion, Arthrex). Standard sutures were used (Fibrewire, Arthrex).
In both groups the rehabilitation protocol was similar. The first 4 wk no weight bearing was allowed. After that, patients started weight bearing with crutches. From week 5 till week 12 patients started with passive and active exercises and were guided by a physiotherapy. After week 12 there were no more restrictions. All patients received standard 4 wk of non-steroid anti-inflammatory drugs (diclofenac) to inhibit heterotopic ossification.
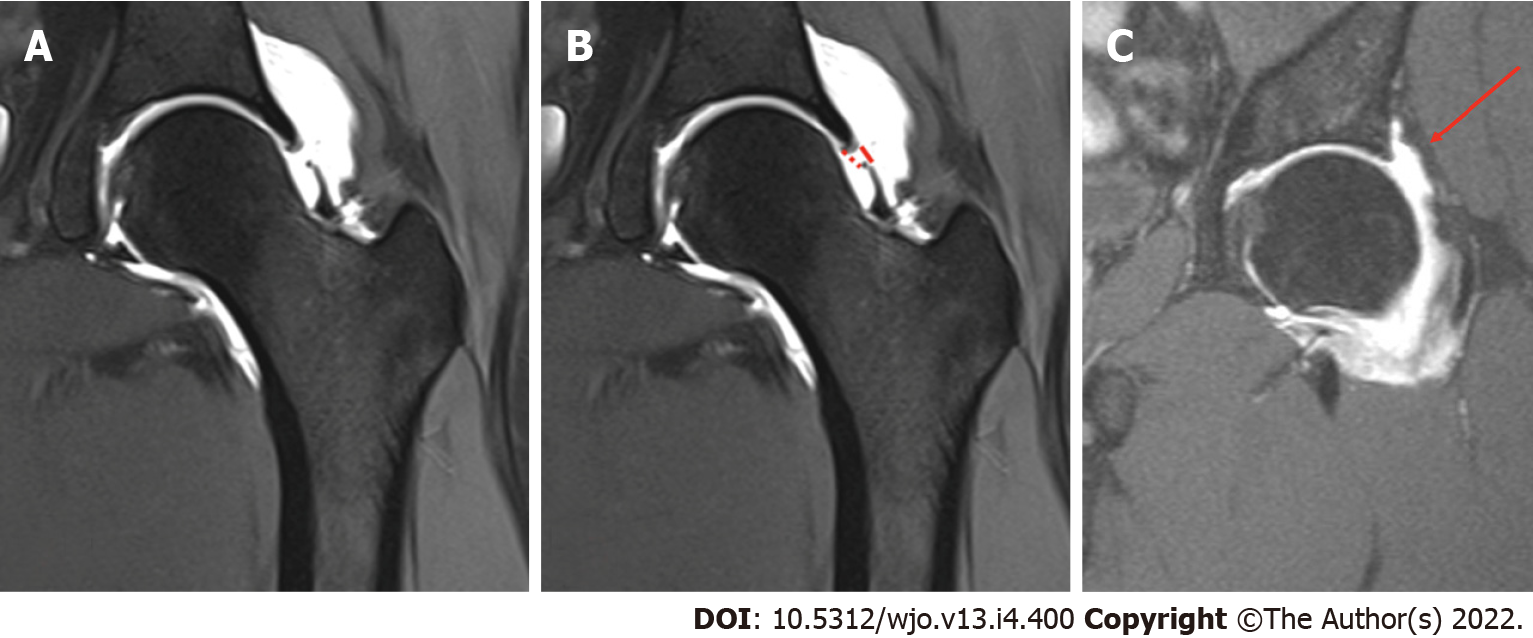
The used technique for measuring capsular defects has been previously described in the paper of Strickland et al[17]. Capsular integrity was measured on a proton weighted density sequence or the T2 weighted fat-saturated sequence in the coronal plane. First step was to determine if there was a capsular defect (Figure 1). The definition of a capsular defect was described by Weber et al[18]; being any visual disruption of the iliofemoral ligament or any appearance of communication between the joint and the iliofemoral bursa seen with contrast (Figure 1A and B)[18]. Furthermore, we measured 2 parameters: Gap length on the acetabular side and the gap length on the muscular side of the defect (Figure 1A and B)
Patient and clinical characteristics are described as means ± SD in case of normally distributed continuous variables. Otherwise, medians with ranges are presented. Comparisons between repair groups were performed by use of t-tests or non-parametric Mann Whitney U-tests where appropriate. Categorical variables are presented as numbers with accompanying proportions and analyzed by use of χ2 tests or Fischer Exact-tests (in case of expected numbers < 5). For the presence of a capsular gap, absolute agreement was calculated to present inter observer reliability. The association between pre- and perioperative details and the presence of a defect was analyzed by use of a univariate logistic regression analysis and Odds ratios (OR) with 95%CI were calculated. Intra class correlation coefficients (ICCagreement, 2-way random effect model) were calculated for both acetabular and muscular gap length. A P value < 0.05 was considered statistically significant.
Analysis was performed by use of SPSS statistical software (IBM Corp. IBM SPSS Statistics for Macintosh Version 26.0. Armonk, NY: IBM Corp).
The mean age in the unrepaired group was 33.3 ± 6.1 and in the repair group 31.4 ± 9.1. Average follow-up in the repair group was 15.8 ± 6.5 mo and in the unrepaired group 12.6 ± 6.7 mo. Regarding baseline characteristics there were no significant differences between both groups (Table 1).
| Repaired (n = 13) | Unrepaired (n = 16) | P value | |
| Sex | 0.36 | ||
| Male | 4 (30.8) | 2 (12.5) | |
| Female | 9 (69.2) | 14 (87.5) | |
| BMI | 23.8 ± 3.9 | 23.1 ± 2.3 | 0.67 |
| Age (yr) | 31.4 ± 9.1 | 33.3 ± 6.1 | 0.49 |
| Follow-up (mo) | 15.8 ± 6.5 | 12.6 ± 6.7 | 0.72 |
| Impingement type | |||
| CAM | 5 (38.5) | 3 (18.8) | 0.62 |
| Pincer | 5 (38.5) | 9 (56.3) | 0.34 |
| Labral repair | 5 (38.5) | 7 (43.8) | 0.22 |
| CE angle at time of MRI (degrees) | 38.2 ± 7.7 | 34.0 ± 9.8 | 0.48 |
Regarding the HAGOS functional outcome score both baseline and 12 mo follow-up values are given in Table 2. In the capsule defect group, 7 patients reached the 12 mo follow-up, in the capsule intact group, 16 patients reached the 12 mo follow-up. Between the capsule intact and the capsular defect group, there were no differences on all 5 domains of the HAGOS outcome score (Table 2).
| Capsular intact (n = 20) | Capsular defect (n = 9) | P value | |
| Baseline | |||
| HAGOS, median (IQR) | |||
| Symptoms | 44.6 (35.7-58.9) | 35.7 (28.6-37.5) | 0.08 |
| Pain | 43.8 (32.5-54.4) | 35.0 (31.3-48.8) | 0.39 |
| ADL | 47.5 (26.3-65.0) | 40.0 (40.0-67.5) | 0.84 |
| Sport | 32.8 (19.5-43.0) | 25.0 (19.5-37.5) | 0.71 |
| QoL | 25.0 (15.0-35.0) | 25.0 (21.3-38.8) | 0.64 |
| 12 mo FU | |||
| HAGOS, median (IQR) | |||
| Symptoms | 51.8 (32.1-74.1) | 39.3 (35.7-64.3) | 0.82 |
| Pain | 70.0 (48.8-86.3) | 60.0 (40.0-92.5) | 0.87 |
| ADL | 67.5 (40.0-90.0) | 60.0 (50.0-95.0) | 0.62 |
| Sport | 53.6 (25.8-80.5) | 53.1 (35.7-81.3) | 0.87 |
| QoL | 40.0 (26.3-53.8) | 60.0 (40.0-60.0) | 0.28 |
In total there were 9 capsular defects measured on MRI, 20 hips did not have a capsular defect. For the assessment of the presence of capsular defect there was 100% agreement between observers. In the repair group, there were 2 patients (15.4%) with a measurable capsular defect on MRI, and in the unrepaired group 7 patients (43.8%) (P = 0.13).
In the capsular repair group, there were 2 failures. The first was a 23-year-old woman with a large CE angle (44 degrees) and a BMI of 24,6. The second patient was a 45-year-old woman with a hip that had already some signs of osteoarthritis, a CE angle of 36.9 degrees and a BMI of 33.3.
Inter observer reliability of gap size measurements was good to excellent with ICC values of 0.83 and 0.94 of the gap measurements at the acetabular and muscular side.
Among patients with a capsular defect, median gap sizes at the acetabular side were 5.9 mm (range: 2.7-9.0) and 8.0 mm (range: 4.5-18.0) in the repaired and unrepaired group, respectively (P = 0.462). At the muscular side, gap sizes were 6.6 mm (range: 4.1-9.0) and 11.5 mm (range: 3.0-18.0), respectively (P = 0.857).
Although not significant patients with a larger CE angle were more likely to have a capsular defect on MRI with an OR of 1.12 (P = 0.06).
In the group of patients with a capsular defect, there were 2 with a CAM-type deformity and 5 with a pincer-type deformity. In the capsule intact group, there were 6 patients with a CAM-type deformity and 9 patients with a pincer-type deformity. There was no significant association between the presence of a CAM or pincer deformity and a capsular defect (Table 3).
| OR (95%CI) | P value | |
| CE angle at time of MRI | 1.12 (1.00-1.26) | 0.06 |
| CAM | 0.67 (0.11-4.20) | 0.67 |
| Pincer | 1.53 (0.31-7.44) | 0.60 |
| Labral repair | 0.10 (0.01-0.98) | 0.05 |
In the capsular defect group, there was 1 patient that underwent a labral repair; in the capsule intact group, 11 patients underwent a labral repair. Patients with a labral repair were less likely to have a capsular defect on MRI with an OR of 0.1 compared to patients without labral repair (P = 0.05) (Table 3).
In this case series we found that the incidence of a capsular defect, although not significant, was higher in the unrepaired capsulotomy group than in the repaired group. Our results are comparable to available current literature. In the randomized controlled trial of Strickland et al[17] they investigated 30 hips and compared capsular closure vs unrepaired interportal capsulotomy during simultaneous bilateral arthroscopy. They measured the capsular defect and the quality of the capsule postoperatively and report no significant differences between treatment groups at final endpoint at 24 wk after surgery. Kraeutler et al[19] performed a multicenter randomized trial between capsular repair and unrepaired capsulotomy. They also report no differences between both treatment groups regarding healing of the capsule measured on MRI[19].
In the paper of Weber et al[18] symptomatic patients were evaluated with MRI after capsular repair. They reported that 1 year after surgery 92.5% of the repaired capsules remained closed and that the capsule was thickened at the site of the repaired capsulotomy compared to the unaffected contralateral hip capsule[18].
To our best knowledge there is no literature that investigated the association between the size of the CE-angle and the presence of a capsular defect. In our series the likelihood of a capsular defect was larger with an increasing CE angle. An explanation for this finding could be that in this group the incidence of pincer impingement was higher. As part of the procedure of pincer impingement the surgeon must resect a part of the acetabulum and detach a part of the iliofemoral ligament. Extended resection and concomitant ligament damage could lead to possible higher incidence of capsular defects after surgery. In our series there were only 2 failures in the capsular repair group that showed a capsular defect on MRI. Possibly the rather large CE angle in both patients was of influence and led to subsequent failure of capsular healing.
Regarding labral repair there was a significant larger portion of patients with an intact capsule in the labral repair group. It is unsure where the difference in capsular defects between labral repair and no repair originates from. A possibility is that more stability from a repaired labrum influences the capsular healing. Cadaveric studies show that an intact labrum absorbs a lot of strain during motion of the hip[20]. Without the intact labrum the hip capsule might have to compensate for these forces resulting in possibly a higher incidence of capsular defects.
A strength of this study is that the capsular defect was measured by two authors separately and that an intra classifier coefficient was calculated to verify the accuracy of the measured defects.
The first limitation of this study is that small number of patients were included. We expect that although there was a clinically relevant difference in measurable defect between the groups, this difference was not statistically different because of the small sample size. Secondly, only symptomatic patients or patients with complaints of the contralateral hip had an MRI scan and this could have introduced a bias in our results.
Our current study shows that there is no significant difference in capsular healing on MRI between capsular repair or unrepaired capsulotomy. Furthermore, a higher CE angle increases the likelihood of having a capsular defect and the presence of a labral repair decreases the likelihood of a capsular defect. Although there seems to be no reason for routinely capsular closure after hip arthroscopy, knowing these patient specific factors might help the orthopedic surgeon to decide to perform a capsular repair in specific cases.
Capsular management after hip arthroscopy remains topic of debate after an interportal capsulotomy
More studies are needed to determine what the effect is of capsular repair on capsular healing after hip arthroscopy.
To determine whether capsular repair or not may result in a capsular defect measured on an MRI scan. Secondary objective is to determine of the presence of a capsular defect might influence the clinical outcome after hip arthroscopy.
A random sample of patients were enrolled in this case series. All were operated and had a magnetic resonance imaging (MRI) scan in the postoperative phase. Patients were part of an earlier performed randomized trial and were randomized into a capsular repair or unrepaired capsulotomy group. Outcome was the presence of a capsular defect on MRI and the Copenhagen Hip and Groin Outcome Score (HAGOS).
A total of 29 hips were included. There was no significant different number of capsular defects between the capsular repair or unrepaired capsulotomy groups. There was also no difference in outcome measured with HAGOS outcome score between the capsular defect or capsule intact group.
There was no difference in the number of capsular defects between the capsular repair or unrepaired capsulotomy group.
Future larger studies are needed to confirm that capsular repair or unrepaired capsulotomy has no influence on the presence of a capsular defect or not. In addition; long term analysis needs to be done to determine whether the presence of a capsular defect might result in long term complications or influence outcome.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Netherlands
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ali T, Egypt; Greco T, Italy S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Truntzer JN, Shapiro LM, Hoppe DJ, Abrams GD, Safran MR. Hip arthroscopy in the United States: an update following coding changes in 2011. J Hip Preserv Surg. 2017;4:250-257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 2. | Griffin DR, Dickenson EJ, Wall PDH, Achana F, Donovan JL, Griffin J, Hobson R, Hutchinson CE, Jepson M, Parsons NR, Petrou S, Realpe A, Smith J, Foster NE; FASHIoN Study Group. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet. 2018;391:2225-2235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 392] [Cited by in RCA: 405] [Article Influence: 57.9] [Reference Citation Analysis (0)] |
| 3. | Larson CM, Guanche CA, Kelly BT, Clohisy JC, Ranawat AS. Advanced techniques in hip arthroscopy. Instr Course Lect. 2009;58:423-436. [PubMed] |
| 4. | Byrd JW, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25:365-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 209] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 5. | Domb BG, Stake CE, Finley ZJ, Chen T, Giordano BD. Influence of capsular repair versus unrepaired capsulotomy on 2-year clinical outcomes after arthroscopic hip preservation surgery. Arthroscopy. 2015;31:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 6. | Economopoulos KJ, Chhabra A, Kweon C. Prospective Randomized Comparison of Capsular Management Techniques During Hip Arthroscopy. Am J Sports Med. 2020;48:395-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 7. | Acuña AJ, Samuel LT, Roth A, Emara AK, Kamath AF. How capsular management strategies impact outcomes: A systematic review and meta-analysis of comparative studies. J Orthop. 2020;19:237-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Lund B, Mygind-Klavsen B, Grønbech Nielsen T, Maagaard N, Kraemer O, Hölmich P, Winge S, Lind M. Danish Hip Arthroscopy Registry (DHAR): the outcome of patients with femoroacetabular impingement (FAI). J Hip Preserv Surg. 2017;4:170-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | Atzmon R, Sharfman ZT, Haviv B, Frankl M, Rotem G, Amar E, Drexler M, Rath E. Does capsular closure influence patient-reported outcomes in hip arthroscopy for femoroacetabular impingement and labral tear? J Hip Preserv Surg. 2019;6:199-206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Bech NH, Sierevelt IN, de Waard S, Joling BSH, Kerkhoffs GMMJ, Haverkamp D. Capsular closure versus unrepaired interportal capsulotomy after hip arthroscopy in patients with femoroacetabular impingement, results of a patient-blinded randomised controlled trial. Hip Int. 2021;11207000211005762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 11. | Khair MM, Grzybowski JS, Kuhns BD, Wuerz TH, Shewman E, Nho SJ. The Effect of Capsulotomy and Capsular Repair on Hip Distraction: A Cadaveric Investigation. Arthroscopy. 2017;33:559-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 79] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 12. | Baha P, Burkhart TA, Getgood A, Degen RM. Complete Capsular Repair Restores Native Kinematics After Interportal and T-Capsulotomy. Am J Sports Med. 2019;47:1451-1458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 13. | Abrams GD, Hart MA, Takami K, Bayne CO, Kelly BT, Espinoza Orías AA, Nho SJ. Biomechanical Evaluation of Capsulotomy, Capsulectomy, and Capsular Repair on Hip Rotation. Arthroscopy. 2015;31:1511-1517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 144] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 14. | Bayne CO, Stanley R, Simon P, Espinoza-Orias A, Salata MJ, Bush-Joseph CA, Inoue N, Nho SJ. Effect of capsulotomy on hip stability-a consideration during hip arthroscopy. Am J Orthop (Belle Mead NJ). 2014;43:160-165. [PubMed] |
| 15. | Wagner FV, Negrão JR, Campos J, Ward SR, Haghighi P, Trudell DJ, Resnick D. Capsular ligaments of the hip: anatomic, histologic, and positional study in cadaveric specimens with MR arthrography. Radiology. 2012;263:189-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Thorborg K, Hölmich P, Christensen R, Petersen J, Roos EM. The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. Br J Sports Med. 2011;45:478-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 376] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 17. | Strickland CD, Kraeutler MJ, Brick MJ, Garabekyan T, Woon JTK, Chadayammuri V, Mei-Dan O. MRI Evaluation of Repaired Versus Unrepaired Interportal Capsulotomy in Simultaneous Bilateral Hip Arthroscopy: A Double-Blind, Randomized Controlled Trial. J Bone Joint Surg Am. 2018;100:91-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 18. | Weber AE, Kuhns BD, Cvetanovich GL, Lewis PB, Mather RC, Salata MJ, Nho SJ. Does the Hip Capsule Remain Closed After Hip Arthroscopy With Routine Capsular Closure for Femoroacetabular Impingement? Arthroscopy. 2017;33:108-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Kraeutler MJ, Strickland CD, Brick MJ, Garabekyan T, Woon JTK, Chadayammuri V, Mei-Dan O. A multicenter, double-blind, randomized controlled trial comparing magnetic resonance imaging evaluation of repaired versus unrepaired interportal capsulotomy in patients undergoing hip arthroscopy for femoroacetabular impingement. J Hip Preserv Surg. 2018;5:349-356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Safran MR, Giordano G, Lindsey DP, Gold GE, Rosenberg J, Zaffagnini S, Giori NJ. Strains across the acetabular labrum during hip motion: a cadaveric model. Am J Sports Med. 2011;39 Suppl:92S-102S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |