Published online Apr 18, 2022. doi: 10.5312/wjo.v13.i4.365
Peer-review started: July 27, 2021
First decision: November 11, 2021
Revised: November 30, 2021
Accepted: February 23, 2022
Article in press: February 23, 2022
Published online: April 18, 2022
Processing time: 258 Days and 7.8 Hours
Neuromuscular scoliosis is commonly associated with a large pelvic obliquity. Scoliosis in children with cerebral palsy is most commonly managed with posterior spinal instrumentation and fusion. While consensus is reached regarding the proximal starting point of fusion, controversy exists as to whether the distal level of spinal fusion should include the pelvis to correct the pelvic obliquity.
To assess the role of pelvic fusion in posterior spinal instrumentation and fusion, particularly it impact on pelvic obliquity correction, and to assess if the rate of complications differed as a function of pelvic fusion.
This was a retrospective, cohort study in which we reviewed the medical records of children with cerebral palsy scoliosis treated with posterior instrumentation and fusion at a single institution. Minimum follow-up was six months. Patients were stratified into two groups: Those who were fused to the pelvis and those fused to L4/L5. The major outcomes were complications and radiographic parameters. The former were stratified into major and minor complications, and the latter consisted of preoperative and final Cobb angles, L5-S1 tilt and pelvic obliquity.
The study included 47 patients. The correction of the L5 tilt was 60% in patients fused to the pelvis and 67% in patients fused to L4/L5 (P = 0.22). The pelvic obliquity was corrected by 43% and 36% in each group, respectively (P = 0.12). Regarding complications, patients fused to the pelvis had more total complications as compared to the other group (63.0% vs 30%, respectively, P = 0.025). After adjusting for differences in radiographic parameters (lumbar curve, L5 tilt, and pelvic obliquity), these patients had a 79% increased chance of developing complications (Relative risk = 1.79; 95%CI: 1.011-3.41).
Including the pelvis in the distal level of fusion for cerebral palsy scoliosis places patients at an increased risk of postoperative complications. The added value that pelvic fusion offers in terms of correcting pelvic obliquity is not clear, as these patients had similar percent correction of their pelvic obliquity and L5 tilt compared to children whose fusion was stopped at L4/L5. Therefore, in a select patient population, spinal fusion can be stopped at the distal lumbar levels without adversely affecting the surgical outcomes.
Core Tip: The value of including the pelvis in the distal level of fusion in children with cerebral palsy scoliosis is not clear with respect to correcting pelvic obliquity or L5 tilt. This does, however, increase the risk of complications. After careful patient selection, spinal fusion can be stopped at the distal lumbar levels without adversely affecting the surgical outcomes.
- Citation: Strom SF, Hess MC, Jardaly AH, Conklin MJ, Gilbert SR. Is it necessary to fuse to the pelvis when correcting scoliosis in cerebral palsy? World J Orthop 2022; 13(4): 365-372
- URL: https://www.wjgnet.com/2218-5836/full/v13/i4/365.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i4.365
Patients with neuromuscular scoliosis may benefit from surgery with improved standing balance, sitting positioning, and overall better caregiver satisfaction[1]. However, these surgeries are challenging due to severe deformity and presence of comorbidities. Complications are high (20% to 40%) compared to adolescent idiopathic scoliosis (5% to 23%)[2-5]. Posterior spinal instrumentation and fusion is the most common procedure performed. Proximally, fusion is begun T1 or T2 to prevent the development of proximal junctional kyphosis (PJK) which can lead to pain and neurologic deficits[6,7]. The distal extent of the fusion, however, remains controversial. Neuromuscular scoliosis is commonly characterized by pelvic obliquity which affects sitting balance and the development of iliac ulcers[8]. There is debate as to whether pelvic fixation is necessary to correct pelvic obliquity with some authors advocating that those with pelvic obliquity less than 10˚-15˚ do not require fixation to the pelvis[6-8]. The majority of authors, however, advocate for fusion to the pelvis to not only correct the pelvic obliquity but also decrease the risk of distal curve progression and revision surgery[9-11].
The studies that discuss pelvic fusion either focus on children with flaccid forms of paralysis or include a pooled patient cohort including both spastic and flaccid disorders[9-13]. Since these neuromuscular disorders have varying levels of pelvic obliquity and do not necessarily act the same way, we sought to analyze our patients with cerebral palsy (CP) with regards to radiographic outcomes and complications as a function of fusion to the pelvis compared with higher levels of fusion.
Following institutional review board approval, we retrospectively reviewed our electronic medical records. Surgically treated CP scoliosis patients who had gross motor function classification system levels IV or V and were less than 21 years of age were included. Exclusion criteria were surgery for predominant kyphosis, follow-up less than six months, or incomplete charts. The analysis spanned records from 2007 to 2018 at a single institution. We excluded patients with other indications for surgery, patients with unavailable radiographs, and those with follow-up less than six months. Demographic information, operative details, and the development of complications were recorded. We stratified complications into major and minor as previously described.14 Major complications were those that prolonged the duration of hospitalization or required additional surgical procedures. These included severe pulmonary complications (pneumonia, respiratory failure), deep surgical site infections (SSI), hemodynamic instability, pseudarthrosis, and PJK. Minor complications were those that were asymptomatic, self-resolving, or effectively treated non-surgically. Examples include intraoperative durotomy, fever occurring more than 24 h after surgery, decubitus ulcers, superficial SSIs, and superficial wound dehiscence. Pre-operative and final follow up radiographs were measured and Cobb angles, L5-S1 tilt and pelvic obliquity using the Maloney method were recorded[14-17].
Statistical analysis was performed using the IBM SPSS Statistics for Windows, version 25 (IBM Corp., Armonk, NY, USA). T-tests and χ2 tests were used when appropriate. The relative risk (RR) and 95%CI were calculated to assess whether the fusion level affected the risk of developing postoperative complications. P values ≤ 0.05 were considered statistically significant.
Over the study period, 65 children with CP had surgery for scoliosis at our hospital. We excluded 18 cases: 3 had predominant kyphosis rather than scoliosis, 8 had unavailable radiographs, and 7 were lost to follow-up. Our analysis therefore included 47 patients. These were 29 males and 18 females, with an average age of 13.9 years (range: 9.6–19.9 years). All procedures were posterior spinal fusion and instrumentation. The median number of fused vertebrae was 16 (range: 14-17), and 27 patients (57.4%) were fused to the pelvis. Median follow-up duration was 31 mo (range: 7–101 mo).
Patients fused to the pelvis and those fused to L4/L5 were similar with regards to their age, sex distribution, weight, follow-up, and comorbidities. The one exception was that fewer patients fused to the pelvis had seizures. Patient details are included in Table 1. The operative duration and blood loss were not different between both groups. Length of stay was also similar in both groups and was six days on average. With respect to pre-operative radiographic parameters, patients fused to the pelvis had a larger lumbar curve by 17˚ (P = 0.017), greater L5 tilt by 4˚ (P = 0.04), and greater pelvic obliquity by 10˚ (P = 0.0033). The thoracic curve magnitude was similar in both groups (P = 0.17). Table 2 includes the radiographic parameters immediately before surgery and at final follow-up. At the final follow-up, patients who were fused to the pelvis had their thoracic curve corrected by 53%, and their lumbar curve corrected by 38%. Corrections of their L5 tilt and pelvic obliquity were 60% and 43%, respectively. Patients who were fused to L4/L5 had 43% correction of their thoracic curve, 64% of their lumbar curve, 67% of their L5 tilt, and 36% of the pelvic obliquity. The degree of correction of the L5 tilt and pelvic obliquity was similar regardless of fusing to the pelvis (P = 0.22 and 0.12, respectively).
| Characteristics | Fusion to pelvis (n = 27) | Fusion to L4/L5 (n = 20) | P value |
| Demographics | |||
| Average age (yr) | 14.2 | 13.4 | 0.303 |
| Sex, number of males | 19 | 13 | 0.52 |
| Average weight (kg) | 34.2 | 35.6 | 0.66 |
| Average follow-up (mo) | 41.7 | 31.0 | 0.11 |
| Gastrostomy (n) | 15 | 6 | 0.061 |
| VP shunt (n) | 4 | 3 | 0.95 |
| Seizures (n) | 10a | 14a | 0.050 |
| Operative details | |||
| Average operative duration (min) | 341 | 334 | 0.72 |
| Average blood loss (mL) | 989 | 1049 | 0.74 |
| Pre-operative values, mean (Range) | Final values, mean (Range) | |
| Fusion to pelvis | ||
| Thoracic curve (degrees) | 30 (0–64) | 14 (0-38) |
| Lumbar curve (degrees) | 56 (4–106) | 32 (0-68) |
| L5 tilt (degrees) | 10 (0-41) | 4 (0-16) |
| Pelvic obliquity (degrees) | 21 (1-59) | 12 (0-34) |
| Fusion to L4/L5 | ||
| Thoracic curve (degrees) | 42 (2-109) | 24 (1-88) |
| Lumbar curve (degrees) | 39 (5-75) | 14 (1-47) |
| L5 tilt (degrees) | 6 (0-13) | 2 (0-8) |
| Pelvic obliquity (degrees) | 11 (1-30) | 7 (2-20) |
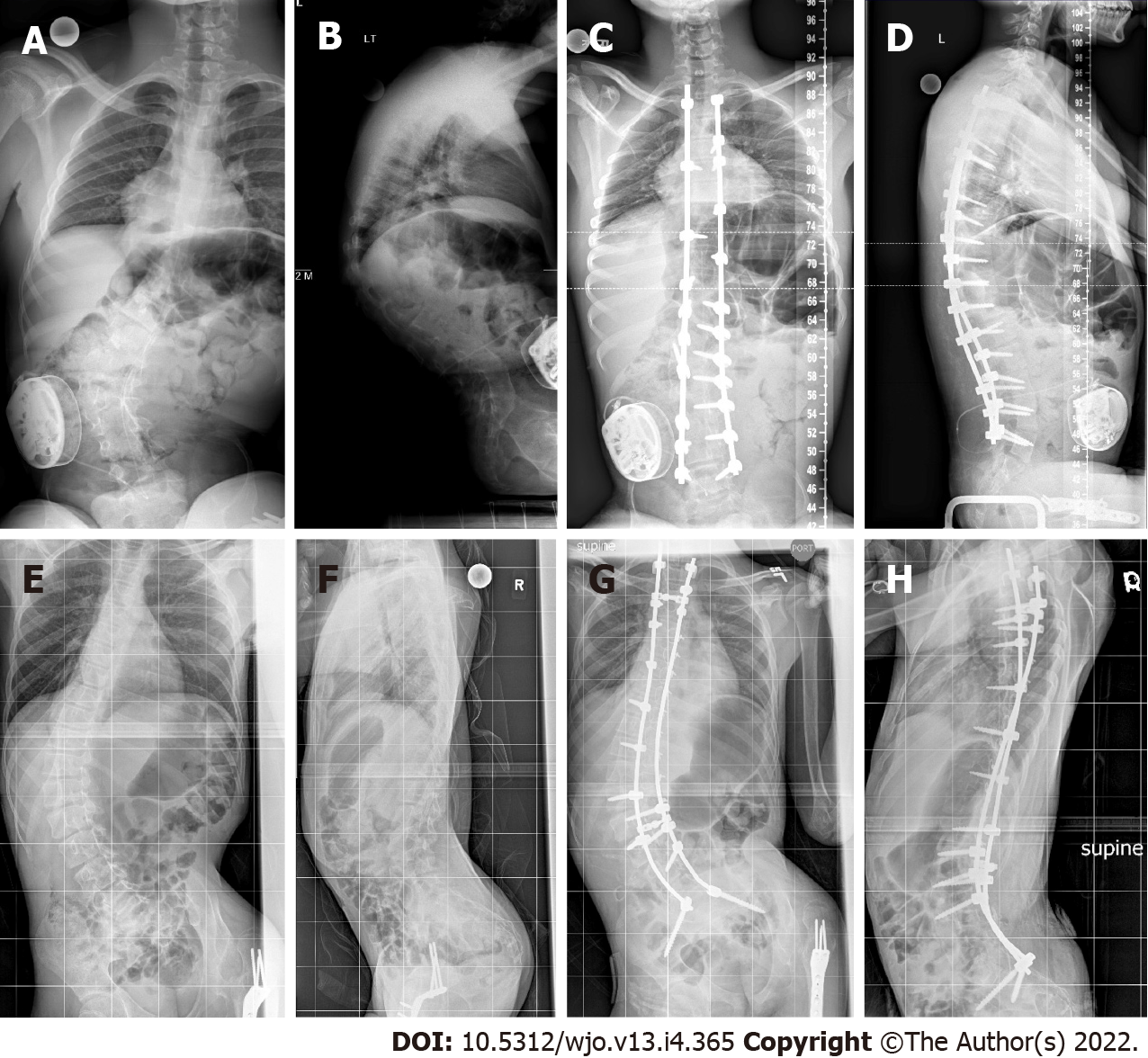
Pelvic obliquity of 10˚ is considered by some to be the threshold for pelvic fusion[6]. Twenty-one of 27 patients fused to the pelvis exceeded this threshold, with a mean of 25˚ (range: 11˚-59˚). This was corrected by 40% to 15˚ (range: 2˚-34˚). In the L4/L5 group, 10 of 20 also had a pelvic obliquity greater than 10˚, with an average of 18˚ (range: 11˚-30˚). Their pelvic obliquity was corrected by 44%, from a mean of 18˚ (range: 11˚–30˚) to 10˚ (range: 4˚-20˚). The magnitude of pelvic obliquity correction was clinically and statistically similar in both groups (P = 0.12). Table 3 stratifies patients according to their preoperative and final pelvic obliquity, and Figure 1 is sample cases of patients who were fused short of the pelvis or whose fusion included the pelvis, respectively.
| Pelvic obliquity | |||
| < 10˚ | 10˚-15˚ | > 15˚ | |
| Fusion to pelvis | |||
| Preoperative | 6 | 6 | 15 |
| Final | 12 | 6 | 9 |
| Fusion to L4/L5 | |||
| Preoperative | 10 | 5 | 5 |
| Final | 15 | 1 | 4 |
The complications encountered are detailed in Table 4. The most frequent complications were pulmonary complications (14.9%), pressure ulcers (12.8%), and instrumentation (8.5%). No post-operative neurological deficits or deaths occurred. Two patients underwent reoperation for deep SSI and PJK. Both had been fused to the pelvis. Also two patients had hardware break and one had instrumentation prominence, but all were asymptomatic and were simply observed. Patients with fusion to the pelvis had more total complications (63.0% vs 30%, P = 0.025; RR = 2.099; 95%CI: 1.012–4.35, P = 0.046). Their RR for minor complications was 2.41 (95%CI: 0.92–6.29, P = 0.073) and for major complications was 1.48 (95%CI: 0.30–7.31, P = 0.63). Even after adjusting for the differences in radiographic parameters (lumbar curve, L5 tilt, and pelvic obliquity), the risk for complications remained increased (RR = 1.79; 95%CI: 1.011–3.41).
| Complications | Fusion to pelvis (n = 27) | Fusion to L4/L5 (n = 20) | Total (n = 47) |
| Pulmonary complications | |||
| Respiratory failure1 | 1 (3.7) | 1 (5) | 2 (4.2) |
| Atelectasis | 3 (11.1) | 1 (5) | 4 (8.5) |
| Pneumonia1 | 0 | 1(5) | 1 (2.1) |
| Pressure ulcer | 5 (18.5) | 1 (5) | 6 (12.8) |
| Instrumentation | |||
| Hardware break or prominence | 3 (11.1) | 0 | 3 (6.4) |
| PJK1 | 1 (3.7) | 0 | 1 (2.1) |
| Superficial SSI | 0 | 2 (10) | 2 (4.2) |
| Deep SSI1 | 1 (3.7) | 0 | 1 (2.1) |
| Wound dehiscence | 1 (3.7) | 0 | 1 (2.1) |
| SIRS1 | 1 (3.7) | 0 | 1 (2.1) |
| Durotomy | 1 (3.7) | 0 | 1 (2.1) |
| Total | 17 (63) | 6 (30) | 23 (49.9) |
Children with CP scoliosis frequently have pelvic obliquity that affects their sitting balance and interferes with transfers. To correct pelvic obliquity and reduce risk of distal adding on, fusion to the pelvis is often recommended[1,10]. Pelvic fusion, however, can lead to surgical morbidity and complications[11,18]. In this study, we compare outcomes in children with CP scoliosis with regards to the distal extent of spine fusion. Pelvic fusion did not increase the operative time or blood loss compared to higher levels of fusion. Published studies have differed, with some demonstrating longer surgeries and more blood loss with pelvic fixation, while other studies did not find a difference[13,19-21]. The long duration of surgery and magnitude of blood loss along with case to case variation may make it difficult to detect differences with statistical significance.
We did find differences in complication rates. In our cohort, children fused to the pelvis had an increased risk to develop post-operative complications, with a RR of 2.099, mainly attributable to higher occurrences of minor complications, most notably pressure ulcers and hardware complications. Pelvic fusion leads to a more rigid seating position[1]. In patients with limited mobility, this could increase their risk for decubitus ulcers. We only had few occurrences of SSIs and wound complications, but they are also an important consideration. Deep SSIs are a common cause for reoperation which puts patients at repeated risks of anesthetic complications, bleeding, and injury due to reinstrumentation. This is particularly important in patients with GMFCS levels IV and V, who have significant co-morbidities, are frequently malnourished, and are at increased risk for abnormal wound healing and infections. Again, published reports have conflicting results. Toll et al[14] in their evaluation of risk factors following scoliosis surgery in neuromuscular patients did not find that fusion to the pelvis was a risk factor for complications. On the other hand, other studies found an increased risk[22,23]. One possible explanation of this discrepancy is the heterogeneity of the reports which include different neuro
The two most commonly used determinants for including the pelvis in the fusion are L5 stability and pelvic obliquity. The L5-sacrum articulation is considered stable when the L5 tilt is less than 15˚, and it is considered unstable when it is greater than 15˚. Fusion to the pelvis is also recommended for pelvic obliquity greater than 10˚. In our cohort, even though decision making was not standardized, all patients with a large L5 tilt were fused to the pelvis. However, not all patients with pelvic tilt were fused to the pelvis. The pelvic fusion did have greater L5 tilt and pelvic obliquity than patients fused to L4/L5. Interestingly, the degree of correction of both parameters was similar in both groups. The L5 tilt was corrected by 60% with pelvic fusion and by 67% with fusion to L4/L5 (P = 0.22). Similarly, the pelvic obliquity was corrected by 43% and 36% in each group, respectively (P = 0.12), so fusing to the pelvis did not offer a significantly greater correction of pelvic obliquity. This was also true for the subset of patients with a pelvic obliquity greater than 10˚. In this population, correction of pelvic obliquity was 40% for patients fused to the pelvis and 44% for those fused to L4/L5, indicating that even with patients who have a large pelvic tilt, fusion to the pelvis does not necessarily achieve better pelvic obliquity correction. Therefore, a large pelvic obliquity by itself might not be an indication to include the pelvis in the distal extent of the spinal fusion, particularly since these patients experience more complications. Furthermore, fusion to the pelvis may not be necessary in all children with CP scoliosis. This could still lead to satisfactory surgical outcomes including pelvic tilt while decreasing the risk of postoperative complications. Future studies can better delineate selection criteria regarding whether to fuse to the pelvis or not in these children.
Our study has several limitations. As a retrospective study, information was gathered from the medical records, which might lead to some inaccuracies. We aimed to have a homogenous cohort, so we only included children with CP, making our sample size moderate. This made the study underpowered to detect differences at the level of individual complications, but did allow identification of higher total complication rate. Sagittal plane deformities were not assessed. There were no predetermined selection criteria for choosing distal fusion level to the pelvis. Although traditional criteria for fusion to the pelvis were not strictly followed, patients who were fused to the pelvis had more pelvic and L5 tilt, indicating selection bias. This might limit the generalizability of the present study, but the conclusion that in a select patient population, posterior fusion does not necessarily have to include the pelvis remains valid. In addition, our outcomes focused on complications. Other factors that can affect surgical planning, like patient and caregiver satisfaction, were not assessed. Additional studies that focus on patient reported outcomes in this patient population will provide valuable insights.
In conclusion, this study demonstrated that in children with CP scoliosis, fusion short of the pelvis can lead to acceptable final pelvic tilt in some cases and may decrease the risk of developing post-operative complications.
The distal extent of the fusion in children with cerebral palsy scoliosis is a controversial topic. There is not enough evidence on whether it is necessary to include the pelvis in the distal fusion to correct for pelvic obliquity in these patients.
This study was carried out to fill the gap in the literature on whether it is necessary to fuse to the pelvis when correcting cerebral palsy scoliosis. The need for a homogeneous cohort (i.e. children with cerebral palsy and not other forms of neuromuscular scoliosis) was an additional reason for carrying out the study.
The primary objective was to compare the radiographic outcome (Cobb angles and pelvic obliquity) of cerebral palsy scoliosis treatment in children who were fused to the pelvis vs those who were fused to L4/L5. The secondary objective was to determine the complications associated with each of the two procedures.
The study was a retrospective, cohort study that utilized chart and radiographic review to determine the outcomes and complications associated with cerebral palsy scoliosis correction in children who were fused to L4/L5 as compared to those fused to the pelvis.
In the analysis of 47 patients, the L5 tilt was corrected by 60% in patients fused to the pelvis, comparable to the 67% achieved in patients fused to L4/L5 (P = 0.22). The pelvic obliquity was also corrected by a similar degree; 43% in patients fused to the pelvis and 36% in patients fused to L4/L5 (P = 0.12). As for complications, patients fused to the pelvis had a higher number of total complications (63.0% vs 30%, respectively, P = 0.025).
Fusing to the pelvis in cerebral palsy scoliosis did not achieve better correction of patients' pelvic obliquity and L5 tilt. However, it did increase the risk of postoperative complications. Therefore, spinal fusion can be stopped at the distal lumbar levels in a select patient population, without necessarily compromising the surgical outcomes.
Future studies can investigate delineating specifically which patients might benefit from including the pelvis in their distal fusion. This might aid the surgeons in their preoperative planning and in guiding their choice of surgical technique.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bizzoca D, Italy; Płaszewski M, Poland S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Halawi MJ, Lark RK, Fitch RD. Neuromuscular Scoliosis: Current Concepts. Orthopedics. 2015;38:e452-e456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Hasler CC. Operative treatment for spinal deformities in cerebral palsy. J Child Orthop. 2013;7:419-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Reames DL, Smith JS, Fu KM, Polly DW Jr, Ames CP, Berven SH, Perra JH, Glassman SD, McCarthy RE, Knapp RD Jr, Heary R, Shaffrey CI; Scoliosis Research Society Morbidity and Mortality Committee. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine (Phila Pa 1976). 2011;36:1484-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 295] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 4. | Murphy RF, Mooney JF 3rd. Current concepts in neuromuscular scoliosis. Curr Rev Musculoskelet Med. 2019;12:220-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 5. | Sink EL, Newton PO, Mubarak SJ, Wenger DR. Maintenance of sagittal plane alignment after surgical correction of spinal deformity in patients with cerebral palsy. Spine (Phila Pa 1976). 2003;28:1396-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Hasler C, Brunner R, Grundshtein A, Ovadia D. Spine deformities in patients with cerebral palsy; the role of the pelvis. J Child Orthop. 2020;14:9-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 7. | Takaso M, Nakazawa T, Imura T, Fukuda M, Takahashi K, Ohtori S. Segmental Pedicle Screw Instrumentation and Fusion Only to L5 in the Surgical Treatment of Flaccid Neuromuscular Scoliosis. Spine (Phila Pa 1976). 2018;43:331-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (2)] |
| 8. | Modi HN, Suh SW, Song HR, Yang JH, Jajodia N. Evaluation of pelvic fixation in neuromuscular scoliosis: a retrospective study in 55 patients. Int Orthop. 2010;34:89-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Peelle MW, Lenke LG, Bridwell KH, Sides B. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rod versus iliac and lumbosacral screws. Spine (Phila Pa 1976). 2006;31:2392-8; discussion 2399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 117] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 11. | Janjua MB, Toll B, Ghandi S, Sebert ME, Swift DM, Pahys JM, Samdani AF, Hwang SW. Risk Factors for Wound Infections after Deformity Correction Surgery in Neuromuscular Scoliosis. Pediatr Neurosurg. 2019;54:108-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Nielsen E, Andras LM, Bellaire LL, Fletcher ND, Minkara A, Vitale MG, Troy M, Glotzbecker M, Skaggs DL. Don't You Wish You Had Fused to the Pelvis the First Time: A Comparison of Reoperation Rate and Correction of Pelvic Obliquity. Spine (Phila Pa 1976). 2019;44:E465-E469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Tøndevold N, Lastikka M, Andersen T, Gehrchen M, Helenius I. Should instrumented spinal fusion in nonambulatory children with neuromuscular scoliosis be extended to L5 or the pelvis? Bone Joint J. 2020;102-B:261-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (2)] |
| 14. | Toll BJ, Samdani AF, Janjua MB, Gandhi S, Pahys JM, Hwang SW. Perioperative complications and risk factors in neuromuscular scoliosis surgery. J Neurosurg Pediatr. 2018;22:207-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 15. | McCall RE, Hayes B. Long-term outcome in neuromuscular scoliosis fused only to lumbar 5. Spine (Phila Pa 1976). 2005;30:2056-2060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 48] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Maloney WJ, Rinsky LA, Gamble JG. Simultaneous correction of pelvic obliquity, frontal plane, and sagittal plane deformities in neuromuscular scoliosis using a unit rod with segmental sublaminar wires: a preliminary report. J Pediatr Orthop. 1990;10:742-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 58] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Brooks JT, Sponseller PD. What's New in the Management of Neuromuscular Scoliosis. J Pediatr Orthop. 2016;36:627-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 18. | Subramanyam R, Schaffzin J, Cudilo EM, Rao MB, Varughese AM. Systematic review of risk factors for surgical site infection in pediatric scoliosis surgery. Spine J. 2015;15:1422-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Sharma S, Wu C, Andersen T, Wang Y, Hansen ES, Bünger CE. Prevalence of complications in neuromuscular scoliosis surgery: a literature meta-analysis from the past 15 years. Eur Spine J. 2013;22:1230-1249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 127] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 20. | Kothari P, Somani S, Lee NJ, Guzman JZ, Leven DM, Skovrlj B, Steinberger J, Kim J, Cho SK. Thirty-Day Morbidity Associated with Pelvic Fixation in Adult Patients Undergoing Fusion for Spinal Deformity: A Propensity-Matched Analysis. Global Spine J. 2017;7:39-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Ramo BA, Roberts DW, Tuason D, McClung A, Paraison LE, Moore HG 4th, Sucato DJ. Surgical site infections after posterior spinal fusion for neuromuscular scoliosis: a thirty-year experience at a single institution. J Bone Joint Surg Am. 2014;96:2038-2048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 114] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 22. | Labbé AC, Demers AM, Rodrigues R, Arlet V, Tanguay K, Moore DL. Surgical-site infection following spinal fusion: a case-control study in a children's hospital. Infect Control Hosp Epidemiol. 2003;24:591-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 75] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 23. | Perry JW, Montgomerie JZ, Swank S, Gilmore DS, Maeder K. Wound infections following spinal fusion with posterior segmental spinal instrumentation. Clin Infect Dis. 1997;24:558-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 2.5] [Reference Citation Analysis (0)] |