INTRODUCTION
Lateral epicondylitis (LE) is the most common cause of musculoskeletal pain in the elbow and is associated with significant pain and severe limitation of upper limb function. This condition is also known as periostitis, tendinitis of extensor carpi radialis brevis muscle (ECRB), epicondyloalgia, radial epicondyliti, etc., but is most commonly described in the literature as tennis elbow (TE) or LE[1]. LE could be caused by previous trauma but is mainly associated with overload activities that require repetitive prono-supination of the forearm and full extension of the elbow. Other risk factors include degenerative changes of the tendons and disruption of the local blood supply in the area. Usually, there is no pain at rest, but the so-called "extensor activity" provokes pain. Statistics show that LE mainly targets patients of “active” age and has a negative impact on their job and social life, thus indirectly affecting the economics of the country. Although it has been highly researched in the last few decades and there are many different articles concerning the causes, pathogenesis, and treatment, it still presents a challenge for specialists. The aim of this article is to briefly summarize the existing knowledge about this condition, emphasizing the risk factors, the development of symptoms and the prognostic value of individual factors, as well as different treatment approaches. In this manuscript, we will critically review the available literature, including recent publications, and outline some future prospects for the development of research on LE.
HISTORY OF LE
In 1873, Runge first described LE as a "writer's cramp." The term “tennis elbow” was introduced by Morris in 1882, but it was Momberg in 1910, who first described this condition in detail[2]. In his monograph on TE in 1936, James Cyriax concluded that the natural course of LE is between six months and two years[3]. This statement has been widely accepted by different authors over the years, but currently, it is considered that the symptoms of LE could persist for many years and relapses are very common[4].
In 1979, Nirschl et al[5] were the first to present surgical treatment of LE, with 97.7% good and excellent results, and in 85.2% of the cases, patients returned to active sports.
EPIDEMIOLOGY AND RISK FACTORS
LE is a relatively common pathology, affecting between 1%-3% of the population. Approximately 4-7/1000 of the patients visit their general practitioners due to symptoms of LE. It is estimated that approximately 40% of all people show some symptoms of LE throughout their life. An interesting fact is that Sanders et al[6], in their population study, observed a significant decrease in the annual incidence of LE in 2000 from 4.5/1000 to 2.4/1000 in 2012. According to them, the lower frequency could be due to either changes in the diagnostic approach or to a real decrease in the LE cases. LE usually affects men and women aged between 30-50, and there is no gender predominance[7]. An interesting fact is that more than 50% of nonprofessional tennis players suffer from this disease, but only 5% of professional tennis players complain of LE. Players in other sports, such as badminton and squash, can also be affected. In athletes, the symptoms are associated with poor backhand performance, low grip of the racket, too tight cord of the racket or in cases when players use wet and heavy balls[8]. LE most commonly affects the dominant hand, especially when performing daily repetitive motions. It is the reason for some of the longest absences from work. Up to 17% of factory workers, as well as meat processors who have repetitive and similar hand movements, suffer from LE. Typists, artists, musicians, electricians, mechanics, and others can also be affected. It is well known that workers involved with repetitive movements of the hands and wrists have an increased risk of LE[9,10], are more resistant to treatment and have a worse prognosis[11,12]. One of the reasons for persistent pain in LE is central sensitization, associated with reduced thresholds of nociception and increased time summation[13]. There is evidence that patients with LE exhibit widespread hyperalgesia, which results in a higher score on the pain scale and prolonged duration of the symptoms. Herquelot et al[10] studied the influence of physical and psychological factors on the occurrence of elbow and LE diseases among a group of 3710 workers in France. Elbow pain without LE was reported in 10.5% of the workers, and LE was diagnosed in 2.4% of the workers. Age, body mass index (> 25) and low social support (men only) were significant risk factors. Heavy exercise combined with repetitive elbow flexion/extension for more than two hours a day and wrist flexion for more than two hours a day were the most significant risk factors for elbow pain and LE.
According to Sanders et al[6], the most common professional activities of patients with LE are office workers or secretaries and medical staff, mainly nurses.
In a recently published case–control study of the influence of various factors on the occurrence of LE, Park et al[14] found that female sex, dominant hand involvement, manual labor, and ipsilateral rotator cuff rupture were risk factors for LE. The results of the study show that excessive use of the limb is a stronger risk factor for LE than metabolic factors[14].
According to some reports, there could be a link between LE and the use of fluoroquinolones. Such a consequence has been reported in Achilles tendon degeneration[15].
Studies show that LE leads to absences from work for up to 219 working days of the year, with a cost of $8099 per patient. Data from the Workcover Queensland show that diseases affecting the upper limb (shoulder and elbow) accounted for 18% of all occupational diseases from 2009 to 2013, which is equal to the prevalence of diseases in the back[16].
SYMPTOMS, DIAGNOSIS AND EVOLUTION
Clinical examination usually presents with increased sensitivity and pain during palpation in the lateral epicondyle area, which is exacerbated by prono-supination of the forearm. The pathognomonic sign of LE is the test in which pain is provoked by the extension of the wrist against resistance, as well as the "chair back test".
Precise evaluation of the pain should be assessed at the beginning of the symptoms because there is evidence that patients with more severe pain syndrome in the first presence of the disease have a higher potential for persistence of the pain at the twelfth month[17]. The “Patient Rated Tennis Elbow Evaluation” is an LE-specific questionnaire that includes pain and impairment scales that are collected to give an overall score from 0 (no pain or injury) to 100 (strongest pain or injury)[18]. A minimum change of 11 points or 37% of the baseline assessment is considered clinically significant[19]. The most common functional limitation in LE is grip pain, which can be measured as painless grip strength and is a reliable and valid indicator that is more sensitive than measuring maximum grip strength[20]. It is measured with the patient lying, the elbow is in a slight extension and the forearm is in pronation, as the patient squeezes the dynamometer until the first appearance of pain. The final calculation consists of the average of three tests performed at one-minute intervals.
From the imaging tools, the X-ray could exclude other pathological conditions of the elbow, and in rare cases, small calcifications could be observed. Ultrasound can provide more accurate data by visualizing the initial location of the muscle and the possible thickening of the tissues around the tendon as a result of the inflammatory process[21]. The most accurate assessment can be made by magnetic resonance imaging (MRI). It shows thickening of the proximal muscle insertion with increased signal in T1 and T2 presented in 2/3 of patients. These characteristics may persist for a long time after the symptoms have resolved[22]. Ultrasound and MRI are highly sensitive but are nonspecific for proving LE. However, the absence of a pathological finding from these tests can certainly rule out LE. The presence of a large rupture (≥ 6 mm) in the tendon or lateral collateral ligament is a crucial part of the differential diagnosis, as it is associated with unsuccessful conservative treatment[23]. Infrared thermography in 94%-100% of patients with LE shows abnormally increased epicondylar activity around the lateral epicondyle. Isotope testing is also positive in 72% of the patients[24], although these two methods are practically not used routinely.
Electromyography and cervical and thoracic spine examinations could also be helpful in diagnosing the source of pain symptoms in the spine. Although the influence of cervical and thoracic spinal diseases on LE is not fully understood, some studies show that neck pain is more common in people with LE[25]. Moreover, patients with LE who also complain of shoulder or neck pain have a worse prognosis[18].
Current data show that the disease usually develops over the years, with common recurrences. This changes the initial assessment that LE is limited from six months to two years. Over 50% of patients report that elbow pain still persists after 12 mo[26,27]. Follow-up of participants in a clinical trial[4] of nonsurgical treatment of LE showed that 20% of patients (27/134) reported pain after three to five years (3.9 years on average), regardless of treatment regimens, and that those with an initial severe pain syndrome had a 5.5 times higher rate of pain symptoms due to LE. Therefore, LE is considered a nonself-limiting condition and is associated with continuous pain in a large number of patients. Sanders et al[6] indicated an 8.5% recurrence rate over two years, and it remained constant over time. The surgically treated cases within two years after diagnosis have increased three times for the period of the study/2001-2012/, from 1.1% for the period between 2000-2002 up to 3.2% after 2009. One of ten patients with persistent symptoms at the sixth month required surgical treatment.
CONSERVATIVE TREATMENT
Conservative treatment of LE includes nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics, topical corticosteroid application, rest, cryotherapy, acupuncture, kinesitherapy, physical therapy including ultrasound, iontophoresis, deep transverse frictions, shock wave and lazer therapy, manual therapy, exercises strengthening the muscles, etc. Wearing an epicondylar bandage is also a part of conservative treatment[28].
Although there is still no generally approved algorithm for the treatment of LE, it is now accepted that the start of the treatment should be with oral NSAIDs[29]. In the short term, oral NSAIDs affect pain compared to placebo, but there are still no data for the 6- to 12-mo period. There are insufficient data on the efficacy of NSAIDs on pain compared with injectable corticosteroids, but as a global effect on symptoms, NSAIDs have shown lower efficacy. In terms of arm function improvement, NSAID administration did not show a significant improvement compared with placebo[30]. Topical NSAIDs improve pain symptoms, but arm function compared with placebo effects is uncertain[30]. Studies in the treatment of LE have shown a significant improvement in the symptoms of topical corticosteroid injection compared with placebo or NSAIDs. A positive effect is reported in both pain and arm function. There is no comparison of efficacy with different types of corticosteroids[30]. In addition to the corticosteroid, a local anesthetic injection was given. The results of the studies showed an overall improvement in pain symptoms and arm function in both groups, with no significant difference between the groups treated with corticosteroids or anesthetics[31]. Interestingly, there is evidence that corticosteroid injections have a higher recurrence rate after 6 wk in patients with LE than in the placebo group or untreated patients. Additionally, compared with combined physical therapy, corticosteroid injections appear to cause a higher recurrence rate after 6 wk[30].
OTHER CONSERVATIVE TREATMENT OPTIONS
In 2011, Creaney et al[32] published the results of a prospective randomized study using growth factors to improve the healing processes of musculoskeletal injuries in sports medicine. It is believed that injecting autologous blood stimulates an inflammatory response, which would prompt healing stimulation. However, the benefit of the method has not been found in long-term follow-up, and its use is recommended only in those cases where other treatment options have failed. Autologous platelet-rich plasma (PRP) is another option used to treat LE. PRP is made by using a sample from the patient's own blood. It is widely used in orthopedics and sports medicine as a method of recovery after various soft tissue injuries or after surgical interventions. PRP is a potential treatment option in patients with LE in cases of physiotherapy failure[33]. Mishra et al[34] reported the results after PRP in a prospective cohort study in 230 patients who did not respond to at least three months of conservative treatment for LE. At 24 wk, PRP injection resulted in a significant improvement in pain compared to the control group (71.5% vs 56.1%, P = 0.019), as well as a significantly lower percentage of patients reporting residual sensitivity in the elbow area (29.1% vs 54.0%, P = 0.009). A study by Shim et al[35] found no difference between PRP administration and own blood injection. However, the significant differences between the various PRP systems and the different techniques used in producing them complicate the comparison of the results of the various studies[33]. Leukocyte concentration affects the quality of PRP. New data suggest that leukocyte-rich PRP may provide pain relief and good outcomes for LE patients compared to alternative topical injections. Additionally, better results are seen with the use of leukocyte-rich PRP than with the use of leukocyte-poor PRP[35]. In a pilot study of 12 patients with refractory LE, Connell et al[36] showed that collagen-producing tenocyte-like cells derived from autologous skin fibroblasts that were injected with a PRP-rich matrix led to clinical and ultrasound improvement. In 2013, Wang et al[37] published the results of a study on the use of autologous tenocytes derived from patellar tendon cells and injected under ultrasound control for the treatment of severe refractory LE in 16 patients. These cells are preferred because of their potential for collagen synthesis and rapid proliferation.
Botulinum toxin A has also been proposed for the treatment of LE. In 1997, Morré et al[38] first described its use in LE. The authors suggest that botulinum toxin injections could aid in the treatment of LE by causing reversible paresis of the extensors, especially m. ECRB, thus preventing the development of microtraumas in its proximal insertion. Placzek et al[39] conducted a multicenter randomized controlled trial in which 130 patients were treated with botulinum toxin or placebo. Patients treated with botulinum showed significant improvements in pain measured by the analog scale at the 6th, 12th, and 18th weeks. However, the application could provoke weakness in the wrist extensors and reduced grip strength. Regardless of the results obtained from these studies, Hayton et al[40] failed to prove a significant difference between the Botox-treated group and the control group.
PHYSICAL THERAPY
Physiotherapy and kinesitherapy play a significant role in the treatment of TE. Their use could start in the acute phase or immediately after diagnosis to reduce pain and continue in the early and late postoperative period to restore range of motion, joint function, recovery of muscle strength and prevention of contractures. In the different stages, specific combinations of the above-described methods could be used by preparing individual rehabilitation programs.
Different combinations of exercises have also been used for the treatment. They are usually part of a complex treatment. Despite controversial results, there is evidence from several randomized controlled trials that exercise may be more effective in reducing pain and improving arm function than other procedures, such as ultrasound, placebo ultrasound and manual therapy, but there is no difference in muscle strength and function between various types of exercises[30,41,42]. Manual therapy for the elbow, wrist and cervicothoracic spine can reduce pain and increase the strength of the pain-free grip immediately after treatment. Unfortunately, meta-analysis is not possible due to heterogeneity between manual therapy techniques and follow-up time. There is insufficient evidence of the long-term clinical effects of manual therapy alone in LE[43-47].
The use of ortheses is another popular LE treatment option. The variety of different orthotic devices and the different follow-up methods for evaluating their effectiveness makes it difficult to analyze the published data. Overall, there is generally controversial evidence for the effectiveness of orthoses as an improved method for arm function and pain relief compared to placebo or in untreated patients. There is no evidence of the superiority of one type of orthosis over others[48-52].
Topical application of ice is a traditional method for pain management. However, evidence for its effectiveness in LE is limited. In a controlled clinical trial, Manias et al[53] failed to demonstrate the advantage of using ice in combination with exercise over using exercise alone.
Acupuncture is used in the treatment of many musculoskeletal disorders, and LE is no exception. After reviewing the literature on the subject, Trinh et al[54] concluded that acupuncture is effective in relieving complaints in the short term. Acupuncture is shown to be more effective in relieving pain and improving function than ultrasound, both at the end of the treatment and at the six-month follow-up[55].
The use of laser therapy in LE is effective in the short term compared to placebo, but in the long term, however, no advantages are found compared to other physical methods. Lasers with a wavelength other than 904 nm did not show better efficacy than placebo[56-58]. The analysis of data from clinical trials on the effect of ultrasound therapy and iontophoresis in LE shows that they do not have an advantage over the use of placebo[30]. The data for the application of shock-wave therapy are similar and are not more effective than placebo or other physical methods[59].
Recently, published data from a meta-analysis show that in the conservative treatment of LE, electrophysiotherapy and physiotherapy should be given priority over other interventions[60].
SURGICAL TREATMENT
Usually, most patients respond to conservative treatment. Nonetheless, in some patients, the symptoms persist for a long time despite treatment. In such cases, a surgical approach is indicated. There are many surgical techniques (Figure 1 and 2), and most of them include debridement of the affected tendon of the m. ECRB and decortication of the lateral epicondyle. Surgery can be performed using open, percutaneous, or arthroscopic techniques.
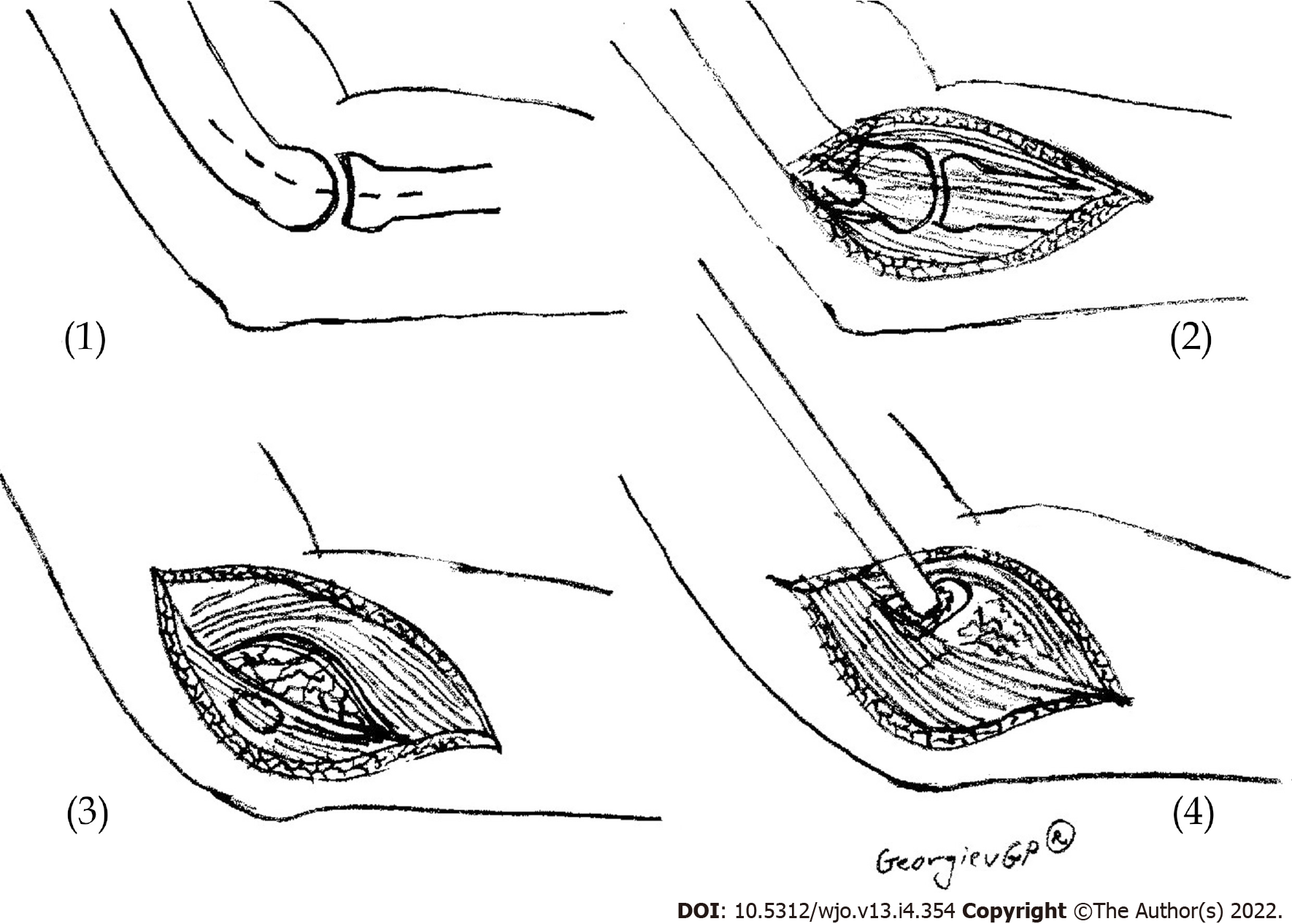
Figure 1 Scheme presenting the open release of lateral epicondylitis.
(1) Skin incision; (2) Extensor carpi radialis longus – extensor digitorum communis interface is identified; (3) Degenerated tissue at extensor carpi radialis brevis muscle is identified and incised; and (4) Osteotome decortication.
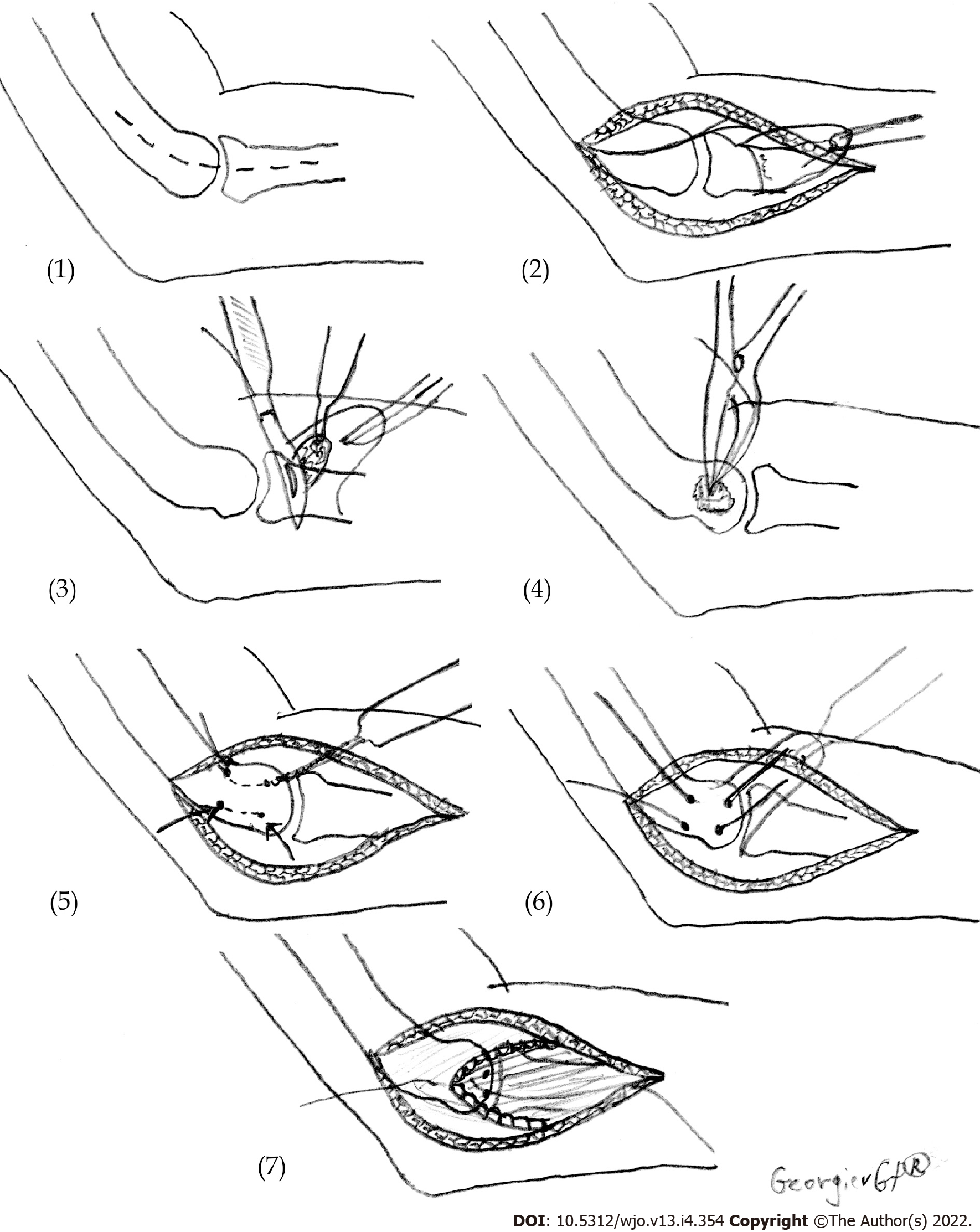
Figure 2 Scheme presenting the technique for the surgical treatment of lateral epicondylitis.
(1) Skin incision; (2) Reflection in the distal direction of the extensor mechanism; (3) Excision of pathologic tissue under the flap of the extensor mechanism; (4) Osteotome decortication; (5) Drilling of two V-shaped tunnels for reattachment of the extensors; (6) Reattachment of the extensor mechanism to the lateral epicondyle; and (7) Restoration of the extensor tendon mechanism.
Open surgery
In 1979, Nirshl et al[5] published an operative technique for the treatment of LE, which involved excision of all visibly damaged parts in the area of the insertion of the ECRB muscle. The authors reported an improvement in 97.7% of the patients after surgery. In 2008, Dunn et al[61] applied the Nirshl technique in 139 elbows and reported improvement in 97% of them. Numerous surgical techniques have been described in the literature: Excision of the painful area and ablation of the common extensor origin according to Garden; Hohmann surgery in which the initial attachment sites of the extensors are released from the lateral epicondyle; and Kaplan denervation of the humeroradial joint. The most popular technique is that of Boyd and McLeod, which eliminates all possible causes of the disease. It involves excision of the proximal part of the annular ligament, releasement of the insertion of the extensors, excision of the bursa in the area and excision of the synovium of the humeroradial joint. There is no evidence of an advantage of any of the open techniques for the treatment of LE over the others[30].
Percutaneous technique
In 1962, Loose performed a percutaneous technique for releasement of the proximal insertion of the ECRB with local anesthesia for the first time. Good results after percutaneous releasement have also been reported by different authors[62-65]. This procedure is effective in pain relief, uses a minimally invasive approach and can be performed as a one-day surgery. However, the application of percutaneous operative techniques is still controversial. Recently, data on a new percutaneous technique called ultrasound guided percutaneous tenotomy (UGPT) have been published. It is safe and secure and leads to improvement of pain symptoms, hand function and ultrasound imaging at the one-year follow-up[66]. This new surgical technique is applied through an incision of five millimeters using ultrasound energy to remove damaged tissue and cause an inflammatory reaction that promotes the healing process in the tendon[67]. The technique requires the use of special equipment - the TX1 Tissue Removal System (Tenex Health, Lake Forest, CA). Seng et al[68] administered UGPT via the TX1 Tissue Removal System to a group of 20 patients with refractory LE, reporting improvement in arm function and pain relief after 3 years of follow-up. Boden et al[69] compared the results after treatment with PRP or UGPT in patients with medial or LE. No statistically significant difference was found between the two techniques. The authors conclude that both techniques are effective in the treatment of epicondylitis and lead to pain relief and improved arm function and quality of life.
Arthroscopic technique
Arthroscopic surgery is becoming increasingly popular in treating LE in the United States. This procedure involves arthroscopic release of the tendon of the ECRB. The potential benefit of arthroscopic surgery is a shorter recovery time and a better tolerance of the patient. The results of this technique have been reported mainly in a series of patients with positive results. Baker et al[70] were the first to apply arthroscopic operative techniques in LE treatment. In arthroscopic surgery, debridement of the pathological tissue is performed. The authors reported good results in 30 patients[71]. Jerosch et al[72] also reported good results from arthroscopic treatment in Germany. Currently, a prospective, single-center, double-blind, randomized, controlled study of the efficacy of arthroscopic release of ECRB in patients with LE is conducted[73]. The expected results will allow optimization of the therapeutic approach in patients with LE with a high degree of reliability.
LIMITATIONS AND FUTURE SCOPE
In this review, we used only English language sources from medical databases. It is worth mentioning here that some of the studies included in this literature review are gaining small sample sizes, which increases the likelihood of a type II error. There are significant methodological differences in the design of the studies between the different studies. In addition, we see a great variety in the methods used to evaluate the results, which means that meaningful data synthesis, which may counteract some of the limitations of individual studies, is difficult.
Although LE has been a known disease for centuries and numerous studies have been conducted on it, there is still a wide horizon for future research and supplementation of our knowledge regarding this disease. First, it is necessary to study in depth the importance of risk factors in light of developing strategies for primary prevention. Another promising area is the study and application of imaging methods using artificial intelligence, which are already entering medical practice[74-76]. Additionally, nonsurgical treatment using various cellular derivatives is a promising therapeutic method[77]. In the near future, we expect to improve the existing methods and introduce new minimally invasive methods of treatment. Researchers’ efforts will also focus on establishing an effective therapeutic strategy for patients with recurrent LE.
CONCLUSION
LE is a common musculoskeletal disorder caused by chronic repetitive overload of the proximal insertion of the extensor carpi radialis brevis muscle that results in local microinjuries, which heal partially and thus induce aseptic inflammation, swelling and pain. Without adequate treatment, this disease could become chronic and lead to significant limitations in daily activities and quality of life impairment. Knowing the nature of this disease is a prerequisite for the implementation of correct therapeutic strategies and therefore achieves a good therapeutic approach and positive results.
ACKNOWLEDGEMENTS
The authors wish to express their gratitude to Dr. Georgi Andreev for the proofreading of this manuscript.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Bulgarian Orthopedic and Traumatology Association.
Specialty type: Orthopedics
Country/Territory of origin: Bulgaria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Apiratwarakul K, Thailand; Bharati S, Bangladesh S-Editor: Wang JL L-Editor: A P-Editor: Wang JL