Published online Mar 18, 2022. doi: 10.5312/wjo.v13.i3.259
Peer-review started: June 29, 2021
First decision: October 16, 2021
Revised: October 28, 2021
Accepted: February 10, 2022
Article in press: February 10, 2022
Published online: March 18, 2022
Processing time: 261 Days and 5.5 Hours
Intra-articular glenohumeral joint injections are essential procedures for treating various shoulder disorders. Fluoroscopy-guided injections have been extensively used; however, they pose a risk of radiation exposure and are expensive and time-consuming. Recently, it has been suggested that ultrasound-guided injections are accurate and cost effective procedures.
To evaluate the accuracy of ultrasound-guided glenohumeral injections using a posterior approach that is confirmed using magnetic resonance arthrography (MRA).
The study included 179 shoulders of patients with recurrent anterior instability (150 patients; 103 and 76 right and left shoulders, respectively; 160 males and 19 females; average age = 20.5 years; age range: 14-63 years) who underwent MRA for preoperative diagnosis. They were injected with 12 mL lidocaine (1%) using the ultrasound-guided posterior approach and then underwent magnetic resonance imaging. Two shoulder surgeons, except for the injector, evaluated the transverse relaxation (T2)-weighted images of axial planes and classified the intra-articular condition of injected contrast into three groups based on one of the three following scenarios: no leakage, injection into the glenohumeral joint without leakage; minor leakage, practical intra-articular injection with some leakage outside the posterior rotator cuffs; and major leakage, inaccurate injection with mass leakage without any contrast into the joint. The inter-rater reliability between two assessors was also evaluated by calculating Cohen’s kappa coefficient. The learning curve was assessed regarding the inaccurate injection rate by analyzing Spearman’s rank correlation coefficient.
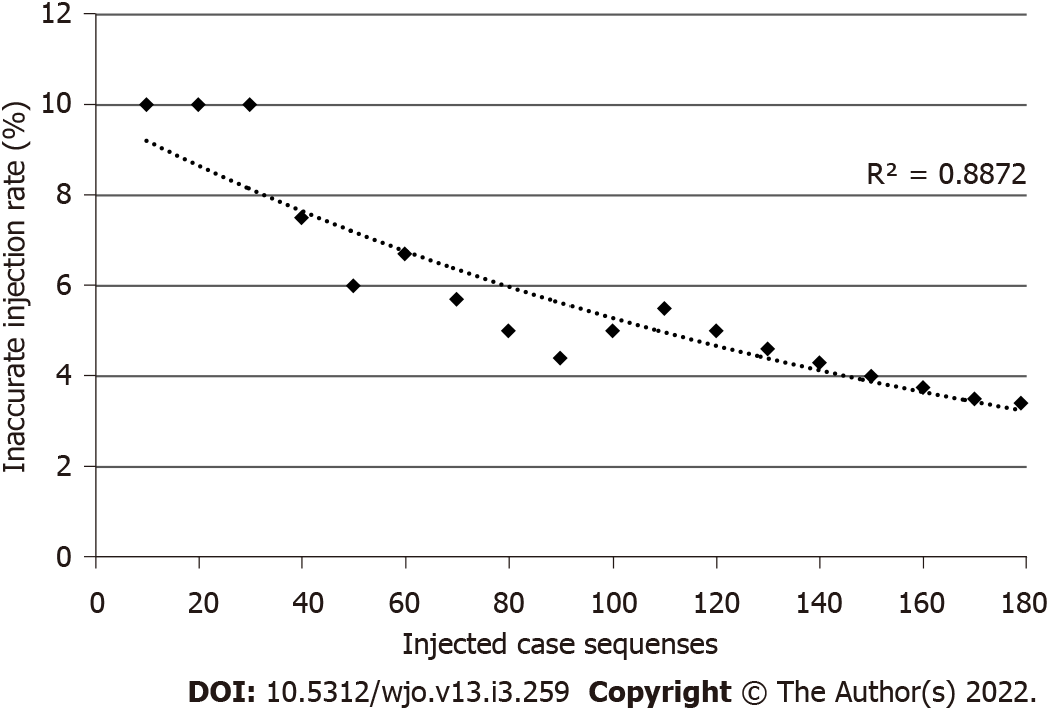
Of the 179 injections, 163 shoulders (91.0%) had no leakage, 10 shoulders (5.6%) had minor leakage, and six shoulders (3.4%) had major leakage. In total, 173 shoulders (96.6%) were intra-articularly injected; thus, we could detect anterior labrum and capsular pathologies. Regarding the inter-rater reliability, the kappa coefficient was 0.925, indicating consistency in the evaluations by both examiners. Regression analysis of the inaccurate injection rate for assessingtechnical learning showed a logarithmic curve with a downward trend (R2 = 0.887, P < 0.001). Three (50%) of the six inaccurate injections classified into “major leakage” were observed in the first 30 injections, indicating that the accurate injection showed a leaning effect.
Ultrasound-guided intra-articular glenohumeral injections using a posterior approach had high accuracy; however, injection accuracy depends on clinical experience.
Core Tip: This is a retrospective study that has evaluated the accuracy of ultrasound-guided glenohumeral injection confirmed using magnetic resonance arthrography. In this study, 163 shoulders (91.0%) were accurately injected without leakage outside the glenohumeral joint. Ten shoulders (5.6%) had minor leakage. In total, 173 shoulders (96.6%) were intra-articularly injected. Ultrasound-guided intra-articular glenohumeral injection using a posterior approach is an accurate injection procedure.
- Citation: Kuratani K, Tanaka M, Hanai H, Hayashida K. Accuracy of shoulder joint injections with ultrasound guidance: Confirmed by magnetic resonance arthrography. World J Orthop 2022; 13(3): 259-266
- URL: https://www.wjgnet.com/2218-5836/full/v13/i3/259.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i3.259
Intra-articular glenohumeral joint injections are essential procedures for treating various shoulder disorders at clinical settings, such as frozen shoulder, osteoarthritis, and rheumatoid arthritis[1]. These injections are distinguished from subacromial injections commonly used for treating subacromial bursitis, rotator cuff tears, and impingement syndrome. Accurate intra-articular injections of drugs can provide good clinical outcomes and enhance patients’ satisfaction with treatment. Furthermore, accurate intra-articular injections of lidocaine, commonly referred to as the lidocaine test, help develop accurate clinical diagnoses. Conversely, injections at erroneous locations may cause damage to nerves, vessels, muscles, or ligaments around the shoulder, and inaccurate injections of lidocaine may mislead the clinical assessment.
Various shoulder injection techniques have been used by orthopedic surgeons or radiologists in their efforts to perform arthrograms. These injection techniques include: (1) blind injections with structures that can be palpated from the body surface, such as the acromion and coracoid process; and (2) image-guided injections with fluoroscopic or ultrasonic guidance, using the anterior, posterior, or supraclavicular approach[2-5].
Conversely, magnetic resonance arthrography (MRA) is a valuable tool used for detecting rotator cuff tears or anterior shoulder instabilities associated with anterior labrum and capsular pathologies. Some studies have reported that MRA is superior to magnetic resonance imaging (MRI) and computed tomography arthrography (CTA) in detecting lesions associated with anterior shoulder instabilities[6,7]. Precise imaging of these shoulder abnormalities can help plan operative procedures.
A fluoroscopy-guided shoulder injection has been extensively used in conjunction with MRA. This technique was first reported by Baert et al in 1933[8], while other studies have reported that the accuracy of fluoroscopy-guided shoulder injections is in the range of 62%-100%[9-11]. However, fluoroscopy-guided injections expose both the examiners and patients to radiation. When MRA is considered helpful for diagnosis, outsourcing the MRA examinations to special institutions is common. However, in Japan, only a few institutions offer MRA examinations because of the lack of dedicated radiologists who can conduct arthrograms. Accordingly, orthopedic surgeons themselves are often needed to perform intra-articular injections before MRI examinations. In these cases, fluoroscopy and MRI reservations are required that is cost-demanding and time-consuming. Therefore, at our institution, we typically perform ultrasonography-guided shoulder injections in conjunction with MRA. The ultrasonographic examinations can be performed before MRI. These procedures are not as time-consuming as the injections performed with fluoroscopy. Recently, ultrasonography has become a widely used diagnostic tool in the field of orthopedics because of its availability, safety, and high diagnostic potential. Particularly, the shoulder joint is one of the bodily areas for which ultrasonography is most useful. Ultrasonography can detect tendons, fluid around the biceps or subacromial bursa, and the contours of the glenohumeral joint clearly that it enables early detection of rotator cuff or intra-articular pathologies, such as tears and fractures[12]. Moreover, ultrasound-guided injections have been gaining attention due to their accessibilities and safety withoutradiation exposure and direct observation of the needle[13]. Although some reports have described the convenience of ultrasound-guided injections, no reports have evaluated its accuracy.
This study was designed to evaluate the accuracy of ultrasound-guided glenohumeral joint injections using a posterior approach confirmed using MRA.
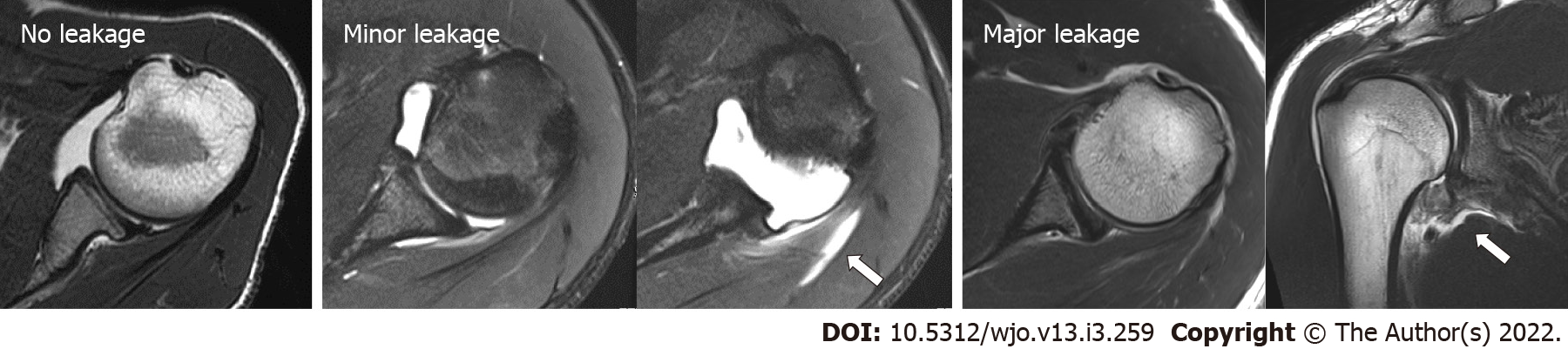
We retrospectively reviewed the MRA images of patients with recurrent anterior shoulder instability. This study has been approved by the Internal Review Board of the corresponding author’s affiliated institution. We excluded patients with rotator cuff tears and posterior shoulder instabilities and those who underwent surgeries. In total, 179 shoulders of 150 patients (including 103 right and 76 Left shoulders; 160 males and 19 females; average age of 20.5 years; age range, 14–63 years) were included in this study. Injections were performed with ultrasound guidance using the posterior approach, followed by MRI examinations (Magnetom Spectra 3T; Siemens Japan, Tokyo, Japan). Two shoulder surgeons, except for the injector, evaluated the transverse relaxation (T2)-weighted images of axial planes and classified the intra-articular condition of the injected contrast into three groups based on one of the three following scenarios. “No leakage” indicates injection into the glenohumeral joint without evidence of leakage. “Minor leakage” indicates intra-articular injections with some leakage outside the posterior rotator cuffs. “Major leakage” indicates inaccurate injection with severe/mass leakage without any contrast into the glenohumeral joint. Diagnosing joint pathologies in the last case was impossible (Figure 1). The chi-square test was used to compare the injection accuracy of the right and left shoulders. The inter-rater reliability between two assessors was evaluated by calculating Cohen’s kappa coefficient. Moreover, the learning curve was assessed by determining the inaccuracy rate relative to the total cases. We defined inaccurate injection rate as the total number of “major leakage” divided by the total number of cases that was recorded every 10 cases and examined the correlation between the inaccurate injection rate and number of cases. This was analyzed using Spearman’s rank correlation coefficient. All statistical analyses were performed using Statistical Package for the Social Sciences (version 26; IBM, NY, United States), and P values of less than 0.05 were used to denote statistical significance.
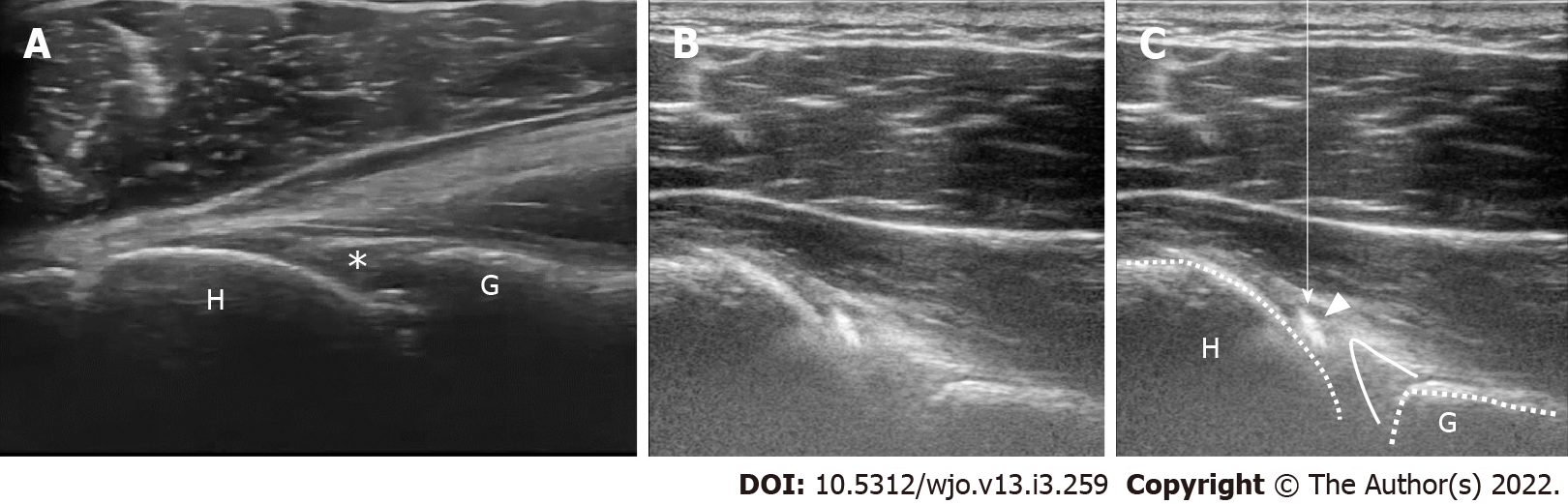
All injections were performed by an experienced surgeon (M.T.). The procedures were performed with the patients in the upright sitting position with their shoulders at the neutral rotation position. Ultrasound examinations were performed using a portable equipment (HI VISION Avius, HITACHI, Japan). The linear ultrasonic probe was operated within a variable frequency range (i.e., 6–14 Hz) and was held horizontally and placed over the posterior aspect of the shoulder (Figure 2), allowing the detection of the glenohumeral joint space (Figure 3A). A 23-gage cathelin needle was inserted using an out-of-plane technique toward the gap between the humeral head and glenoid rim, and 12 mL lidocaine (1%) was administered. In the out-of-plane technique, observing the needle tip at all times during injection is difficult; however, the movement of the needle tip can be detected through the movement of soft tissues. Furthermore, as long as the needle does not deviate from the center of the ultrasound probe, the needle tip theoretically reaches the target in the glenohumeral joint. When the needle tip reaches the joint, the drug can be smoothly injected, and simultaneously, the flow of the fluid can be confirmed in the joint on the ultrasound image (Figure 3B and C).
MRI scans were obtained within 60 min after the injections.
No patient complained of poor physical conditions after the injections. Additionally, no neurological disturbances were observed. From the 179 injections, 163 (91.0%) were completely administered in the glenohumeral joint and were classified as “no leakage.” Furthermore, intra-articular injection with some leakage out of the rotator cuffs was detected in 10 shoulders (5.6%), and these were classified as “minor leakage” (Table 1). We could detect anterior labrum and capsular pathologies in 96.6% (173/179 shoulders) of the tested cases. Six shoulders were classified as “major leakage.” In these cases, the leakages were mostly observed around the axillary area. No significant differences in the accuracy were observed between the right and left shoulders. Regarding the inter-rater reliability, the kappa coefficient was 0.925, indicating consistency in the evaluations by both examiners. Regression analysis of the inaccurate injection rate showed that the curve was logarithmic with a downward trend (R2 = 0.887; P < 0.001) (Figure 4). Three (50%) of the six inaccurate injections that were classified into “major leakage” were observed in the first 30 injections. This indicated that the accurate injection showed a leaning effect.
| No leakage | Minor leakage | Major leakage | Total | |
| Right | 94 (91.3%) | 7 (6.8%) | 2 (1.9%) | 103 |
| Left | 69 (90.1%) | 3 (3.9%) | 4 (5.3%) | 76 |
| Total | 163 (91.0%) | 10 (5.6%) | 6 (3.4%) | 179 |
An intra-articular shoulder injection is an important technique for diagnosing and treating various shoulder disorders. However, it is reported: (1) that these injections are more difficult to perform than other joint injection types; and (2) that theaccuracy of injection into the glenohumeral joint is poor when performed without image guidance.
Some studies have reported about the accuracy and techniques of shoulder injection. Cunnington et al[2] have compared the accuracy of ultrasound-guided injections conducted by research fellows with that of blind (clinical examination-guided) injections conducted by rheumatology consultants for the shoulders, elbows, knees, and ankles and found that ultrasound-guided injections were significantly more accurate than blind injections. Moreover, they have reported that the accuracy of blind injections to the glenohumeral joint was only 40% (8/20 shoulders), which tended to be more difficult than other joint injections. Tobola et al[14] have reported on the technique and accuracy of blind injections using theanterior, posterior, and supraclavicular approaches implemented by different providers. As indicated, the anterior approach was the most accurate (22/34 shoulders, 64.7%) in shoulder cases, regardless of the experience of the clinicians who performed them. Patel et al[4] have evaluated the accuracy of the ultrasound-guided posterior approach on fresh cadaver shoulders and reported that the accuracy was 92.5% (37/40 shoulders) and showed no significant differences owing to the clinical experiences of the injectors. Most injection accuracy reports have been associated with the use of fluoroscopic images (acquired after the injection procedures) to confirm the intra-articular contrast. Sethi et al[15] performed injections using the blind approach with an accuracy of 26.8% with fluoroscopic confirmation. In this study, we evaluated the accuracy of intra-articular shoulder injections using the ultrasound-guided posterior approach in conjunction with MRA images acquired from 179 shoulders (150 patients) for the preoperative diagnosis of anterior shoulder instabilities.
There have been various reports of the accuracy of shoulder injections. However, no reports have neither evaluated injections into the shoulders of living patients nor assessed these using MRA images. In this study, intra-articular shoulder injections that can provide helpful information on labrum and capsular pathologies were performed on 173/179 shoulders (96.6%). The accuracy was equally good or better than those reported in previous cadaveric studies[4].
In current clinical settings, a fluoroscopy-guided injection technique is still extensively used when CTA or MRA is available. Dépelteau et al[9] have reported the accuracy of fluoroscopy-guided injections. In these, 59/65 shoulders (90.8%) were successfully injected on the first attempt, four shoulders (6.2%) on the second attempt, and one (1.5%) shoulder on the third attempt. A fluoroscopy-guided technique allows multiple punctures until accurate injection is achieved given that judging whether the contrast material has been injected into the joint during the injection is possible. Conversely, in an ultrasound-guided technique, only indirect information, such as the patient’s pain or injector’s sensation (e.g., injection pressure), can determine whether the injection is accurate or not. Another disadvantage of an ultrasound-guided injection technique is that detecting the glenohumeral joint space in obese patients it could be difficult because of deep attenuation of ultrasound, unlike the fluoroscopy-guided injection. In such cases, passive movement of the upper arm during ultrasound examination could make detecting the joint space easier. Eventually, we could perform intra-articular injections into the glenohumeral joint with the same or higher accuracy than that reported previously in fluoroscopy-guided injections.
Ultrasound-guided injections have some benefits. They allow more accurate intra-articular injections based on the visualization of the needle’s position. Additionally, the portability of the ultrasound equipment could allow the execution of the injections quickly in the examination room; thus, reserving a fluoroscopy room is not needed, and there is no risk of radiation exposure for both doctors and patients. Additionally, the ultrasound-guided injection technique is a simple procedure and is considered superior to fluoroscopy-guided injection techniques in terms of time and cost-effectiveness[16].
In this study, we performed injections using the ultrasound-guided out-of-plane technique; however, observing the needle path continually from the insertion point was more difficult than that using the in-plane technique. Therefore, fulfilling the aim of this injection is necessary, that is, the clear detection and visualization of the gap between the glenoid rim and humeral head achieved by holding the probe in a stable manner at the target position. Conversely, unlike the in-plane technique, in the out-of-plane technique, the injector does not need to change the hand sides that hold the ultrasound probe or the syringe, depending on the side the patient’s shoulder. Correspondingly, we can always perform injections using the same procedure. In a blind injection technique, an anterior approach was reported to be the most accurate. In previous reports, fluoroscopy-guided injections had been performed using the anterior approach. This is because landmarks around the shoulder palpated from the anterior body surface, such as the acromion and coracoid process, can provide helpful indications for the injection. However, in an ultrasound-guided injection technique, a posterior approach may allow easier detection of the joint space, given that there are no structures on the posterior shoulder.
The study strengths are the patient size and the technique used to accurately evaluate the accuracy of intra-articular shoulder injections. This study represents the largest patient size among all available reports that targeted the accuracy of injection techniques. In previous reports, fluoroscopy images were used to evaluate the condition of the joint and the accuracy of the injection; however, MRA images could allow us to clearly evaluate intra-articular contrast and leakage outside the joint because identifying the location of the contrast material in a three-dimensional view is possible.
This study has some limitations. First, this study evaluated the accuracy of ultrasound-guided injections performed by a single shoulder surgeon. Whether inexperienced physicians, surgeons who do not specialize in shoulder surgeries, or trainee surgeons who specialize in shoulder surgeries could equally achieve accurate injection outcomes is unclear. Additional studies, including the participation of injectors with different experiences and comparisons with other image-guided techniques or approaches are needed. Second, this study has no control group with blind injections. MRA is an essential test for patients with anterior shoulder instability to detect capsular and labral pathologies. A control group could not be established because of the potential disadvantage to the patients if ultrasound guidance is not used.
Third, the subjects of this study were patients with anterior shoulder instabilities in a relatively young age. We have not assessed the accuracy of intra-articular injections for other shoulder disorders, such as osteoarthritis, rheumatoid arthritis, and frozen shoulders. An ultrasound-guided intra-articular injection could be more difficult for older patients owing to capsular contractures or the presence of osteophytes.
Ultrasound-guided intra-articular glenohumeral injections using the posterior approach were an accurate procedure. Of the 179 shoulders, 163 (91.0%) were accurately injected, and 173/179 injections were conducted intra-articularly and provided useful MRA images to detect abnormalities in the glenohumeral joint. We encourage using ultrasonic guidance during shoulder injections because it is a simple and cost effective procedure with acceptable accuracy.
Intra-articular glenohumeral joint injections are essential procedures in a clinical setting of shoulder surgery. In general, a fluoroscopy-guided shoulder injection has been extensively used.
At our institution, we typically perform ultrasound-guided shoulder injections for magnetic resonance arthrography (MRA). The accuracy of ultrasound guided shoulder injection has not been reported.
To evaluate the accuracy of ultrasound-guided shoulder injections with MRA images.
We reviewed the shoulder MRA images of patients with anterior shoulder instability and classified the intra-articular condition in three groups and calculated the injection accuracy.
From the total of 179 injections, 163 (91.0%) were completely administered in the glenohumeral joint. In addition, intra-articular injection with some leakage was detected in 10 shoulders (5.6%).
The ultrasound-guided shoulder injection was shown to be a very accurate procedure.
Further, it is necessary to evaluate whether this technique is effective even for inexperienced examiners.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mastrantonakis K S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Sun Y, Zhang P, Liu S, Li H, Jiang J, Chen S, Chen J. Intra-articular Steroid Injection for Frozen Shoulder: A Systematic Review and Meta-analysis of Randomized Controlled Trials With Trial Sequential Analysis. Am J Sports Med. 2017;45:2171-2179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 2. | Cunnington J, Marshall N, Hide G, Bracewell C, Isaacs J, Platt P, Kane D. A randomized, double-blind, controlled study of ultrasound-guided corticosteroid injection into the joint of patients with inflammatory arthritis. Arthritis Rheum. 2010;62:1862-1869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Aly AR, Rajasekaran S, Ashworth N. Ultrasound-guided shoulder girdle injections are more accurate and more effective than landmark-guided injections: a systematic review and meta-analysis. Br J Sports Med. 2015;49:1042-1049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (1)] |
| 4. | Patel DN, Nayyar S, Hasan S, Khatib O, Sidash S, Jazrawi LM. Comparison of ultrasound-guided vs blind glenohumeral injections: a cadaveric study. J Shoulder Elbow Surg. 2012;21:1664-1668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Koraman E, Turkmen I, Uygur E, Poyanlı O. A Multisite Injection Is More Effective Than a Single Glenohumeral Injection of Corticosteroid in the Treatment of Primary Frozen Shoulder: A Randomized Controlled Trial. Arthroscopy. 2021;37:2031-2040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Roy JS, Braën C, Leblond J, Desmeules F, Dionne CE, MacDermid JC, Bureau NJ, Frémont P. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med. 2015;49:1316-1328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 206] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 7. | Smith TO, Drew BT, Toms AP. A meta-analysis of the diagnostic test accuracy of MRA and MRI for the detection of glenoid labral injury. Arch Orthop Trauma Surg. 2012;132:905-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Baert AL. Imaging of the Shoulder, Techniques and Applications. Leuven: Springer Science & Business Media, 2003: 15-16. |
| 9. | Dépelteau H, Bureau NJ, Cardinal E, Aubin B, Brassard P. Arthrography of the shoulder: a simple fluoroscopically guided approach for targeting the rotator cuff interval. AJR Am J Roentgenol. 2004;182:329-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 73] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Gupton TB Jr, Delgado J, Jaramillo D, Cahill AM, Chauvin NA. Comparative analysis of anterior and posterior contrast injection approaches for shoulder MR arthrograms in adolescents. Pediatr Radiol. 2016;46:1848-1855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Rutten MJ, Collins JM, Maresch BJ, Smeets JH, Janssen CM, Kiemeney LA, Jager GJ. Glenohumeral joint injection: a comparative study of ultrasound and fluoroscopically guided techniques before MR arthrography. Eur Radiol. 2009;19:722-730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Blankstein A. Ultrasound in the diagnosis of clinical orthopedics: The orthopedic stethoscope. World J Orthop. 2011;2:13-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 43] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 13. | Royall NA, Farrin E, Bahner DP, Stawicki SP. Ultrasound-assisted musculoskeletal procedures: A practical overview of current literature. World J Orthop. 2011;2:57-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 14. | Tobola A, Cook C, Cassas KJ, Hawkins RJ, Wienke JR, Tolan S, Kissenberth MJ. Accuracy of glenohumeral joint injections: comparing approach and experience of provider. J Shoulder Elbow Surg. 2011;20:1147-1154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Sethi PM, Kingston S, Elattrache N. Accuracy of anterior intra-articular injection of the glenohumeral joint. Arthroscopy. 2005;21:77-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 90] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 16. | Gyftopoulos S, Abballe V, Virk MS, Koo J, Gold HT, Subhas N. Comparison Between Image-Guided and Landmark-Based Glenohumeral Joint Injections for the Treatment of Adhesive Capsulitis: A Cost-Effectiveness Study. AJR Am J Roentgenol. 2018;210:1279-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |