Published online Feb 18, 2022. doi: 10.5312/wjo.v13.i2.139
Peer-review started: April 28, 2021
First decision: June 16, 2021
Revised: July 2, 2021
Accepted: January 7, 2022
Article in press: January 7, 2022
Published online: February 18, 2022
Processing time: 295 Days and 9.3 Hours
Failure in restoring individual anatomy could be a reason for persistent functional limitations post total hip arthroplasty. Femoroacetabular offset (FAO) plays an important role in anatomic restoration, as loss of offset ≥ 5 mm is associated with altered gait and decreased functional outcome. Preoperative assessment by use of digital templating has shown to be a reliable method for sizing the components in total hip arthroplasty, and can show if anatomic restoration is achieved. In recent years, short stems are growing in popularity as it could allow better restoration due to more variety in placement.
To assess whether restoration of the FAO differs between a short or a conventional stem by use of digital templating. Additionally, association of the preoperative offset and caput-colllum-diaphyseal angle (CCD-angle) within restoration of both stems was investigated, and the reliability of measurements was assessed.
A total of 100 standardized hip radiographs were used for digital templating. Restoration of FAO was classified into “restored” or “not restored”, when a < 5 mm or ≥ 5 mm difference from baseline value presented, respectively. Differences between the two stems concerning proportions of correct restoration of the FAO were analyzed by use of McNemar tests. To assess association between CCD-angle and preoperative FAO with absolute FAO restoration, multi-level analysis was performed by use of a linear mixed model to account for paired measurements. Through determination of the optimal point under the curve in operating curve-analysis, bootstrapping of thousand sets was performed to determine the optimal cutoff point of the preoperative FAO for restoration within the limits of 5 mm. Three observers participated for inter-observer reliability, with two observers measuring the radiographs twice for intra-observer reliability.
The mean preoperative FAO was 79.7 mm (range 62.5-113 mm), with a mean CCD-angle of 128.6° (range 114.5°-145°). The conventional stem could only restore the FAO in 72 of the cases, whereas the short stem restored the FAO in all cases. CCD-angle was not a predictor, but the preoperative FAO was. A cut-off point of 81.25 mm (95% confidence interval of 80.75-84.75 mm) in preoperative FAO was found where the conventional stem was unable to restore the FAO. Reliability of measurements was excellent, with an intra-observer reliability of 0.99 and inter-observer reliability in baseline measurements higher than 0.9 between the three observers.
In preoperative planning of FAO restoration in total hip arthroplasty, digital templating shows that short stems with a curve following the medial calcar are potentially better at restoring the FAO compared to conventional stems if the preoperative offset is ≥ 80.0 mm.
Core Tip: This is a retrospective study, consisting of digital templating a short stem and conventional stem in the same X-ray of the hip to see if there is a difference in restoring the femoroacetabular offset. We found that in a larger femoroacetabular offset (> 80 mm) the short stem could provide better restoration when compared to a conventional stem.
- Citation: de Waard S, Verboom T, Bech NH, Sierevelt IN, Kerkhoffs GM, Haverkamp D. Femoroacetabular offset restoration in total hip arthroplasty; Digital templating a short stem vs a conventional stem. World J Orthop 2022; 13(2): 139-149
- URL: https://www.wjgnet.com/2218-5836/full/v13/i2/139.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i2.139
In recent years, failure of anatomical restoration has gained more attention as a reason for persistent complaints after total hip arthroplasty (THA). Despite considerable improvement, up to 22% of the patients experience functional limitations in daily life[1–4]. Since there has been an increase of young and active patients receiving THA, who have higher expectations of their functional outcome[4,5], excellent results are needed. Nowadays, there is more focus on anatomical restoration as related to clinical outcome[6]. An important part of accurate anatomical reconstruction is a restored femoroacetabular offset (FAO). A loss of ≥ 5 mm between the preoperative offset and postoperative offset is associated with altered gait and decreased functional outcome[7,8]. Restoration of offset improves hip stability, range-of-motion, abductor function and reduced wear[9-13].
Conventional stems are the most common choice for elective THA, due to the amount of experience in placement of these stems and good long-term results. However, individual anatomy can hinder proper femoral offset restoration as the diaphyseal anchorage of this type of stem limits placement options. Short hip stems were designed for preservation of proximal bone stock, but it seems that anatomical restoration is also achievable with short stems. As there are many different designs, short stems can be classified based on osteotomy or anchoring principle. Metadiaphyseal anchoring short stems allow for excellent restoration of individual anatomy[6,14,15], as the placement of these curved short stems can be angled in the desired position to follow the natural curvature of the medial calcar. Due to this feature, it mimics the physiological load transfer on the proximal femur[16,17].
For correct placement of the hip stem, digital 2d-templating is common clinical practice and is a reliable method to estimate the correct size of hip stems prior to surgery[18-21]. It provides information on the level of osteotomy, insight on the probable size of components, and whether anatomical restoration can be achieved.
The primary aim of this study was therefore to see if the FAO could be restored by use of preoperative digital 2d-templating with a short metadiaphyseal anchoring stem and a conventional stem, within a wide range of anatomical hip variations. The secondary aim was to examine the association of secondary measurements required for digital templating, such as the caput-colllum-diaphyseal angle (CCD-angle) and preoperative offset, with offset restoration. Additionally, the intra- and inter-observer reliability of the measurements by use of digital 2d-templating was investigated, as there is limited data on this particular subject and its reliability[21,22].
One hundred standardized preoperative hip measurement radiographs of patients were included, with primary or secondary osteoarthritis as indication for THA. The radiographs were randomly chosen from two ongoing cohorts, the Optimys trial (Mathys Ltd, Bettlach, Switzerland) and the CBH trial (Mathys Ltd, Bettlach, Switzerland). Fifty radiographs were randomly selected from either cohort, creating a variability in coxa norma, vara and valga. If preoperative measurement radiographs were missing, containing a magnification marker for determination of the amount of magnification used, these radiographs were excluded. Approval for inclusion has been attained from the medical ethics review committee, under registry numbers NL47055.048.13 and NL48211.048.14.
Standardised preoperative hip radiographs with magnification marker were used for 2D-digital templating. An internal rotation angle of 20° was used to produce the full profile of the femoral neck on anteroposterior radiography[23,24]. Computer-assisted measurements and 2d-templating were performed by use of Orthoview (Materialise NV, Leuven, Belgium)[25,26].
Pre-templating FAO was measured by first determining the femoral offset, defined as the distance of the longitudinal axis of the femur to the center of rotation. The longitudinal axis was determined from a 4-point box in the intramedullary cavity of the femur. The acetabular offset was determined next, defined as the distance from the center of rotation to the lateral edge of the pelvic teardrop[6,23,24,27-29]. The CCD-angle was used to identify the difference in hip-anatomy, i.e., to identify if patients had a coxa vara (< 120°), coxa norma (120°-135°) or coxa valga (> 135°).
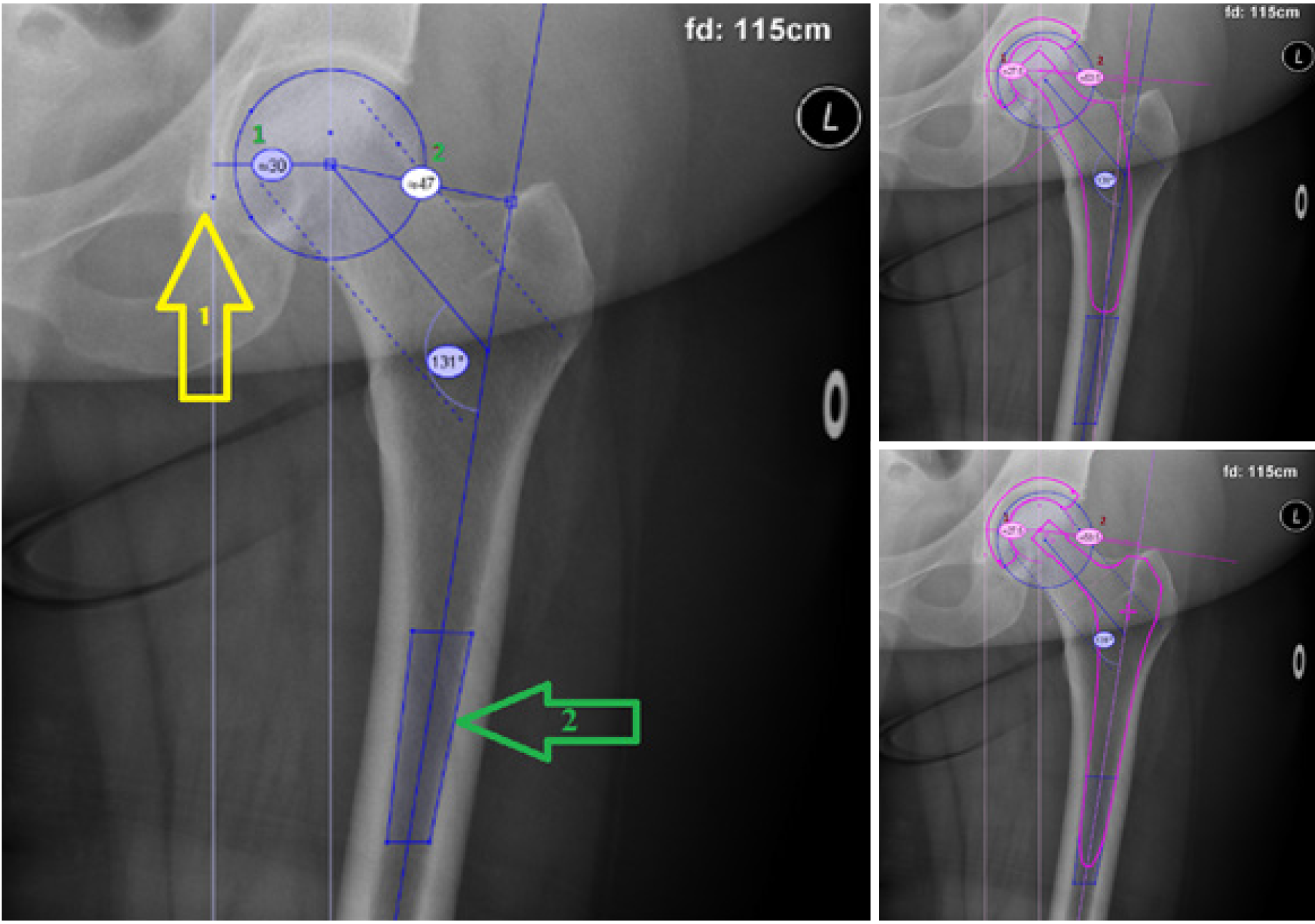
Digital templating of the short and conventional stem was then performed, with the cup as fixed factor in both images. The variables were measured again after templating, with femoral offset now being defined as the distance from the longitudinal axis of the femur to the center of rotation of the prosthetic head. The post-templating acetabular offset was defined as the distance from the center of rotation of the cup to the lateral edge of the pelvic teardrop (Figure 1).
Radiological measurements and templating were performed independently by three observers. To assess intra- and inter-observer reliability, the measurements were performed twice by a medical student (Verboom T) and by a resident in orthopaedic surgery (de Waard S), and once by an experienced orthopaedic hip surgeon (Haverkamp D).
Implants used for templating in this study were the CBH as the conventional stem and the Optimys as the short stem. In both cases the RM Pressfit Vitamys (Mathys Ltd, Bettlach, Switzerland) cup was used. The CBH is a widely used conventional press fit hip stem with a diaphyseal anchorage. Since the CBH hip stem follows the longitudinal femoral axis, femoral offset can only be increased (after determining the correct stem size) by choosing a larger head size and/or a lateral neck.
The Optimys is a short press fit hip stem, which anchors in the metadiaphyse. The shape of the Optimys follows the curvature of the medial calcar and can be placed into varus or valgus position, allowing to increase or decrease the femoral offset as needed. Also, extra femoral offset can be given with head size and a lateral neck.
Patient characteristics and outcome variables are described as means with ranges or frequencies with accompanying percentages. Restoration of FAO was dichotomized into “restored” when < 5 mm from baseline or “not restored” when ≥ 5 mm from baseline[7,30]. Differences between the short stem and the conventional stem concerning the proportions of correct restoration of the offset were analyzed by use of McNemar tests. To assess the association between absolute offset restoration and both CCD-angle and preoperative offset, multi-level analyses were performed by use of linear mixed model to account for paired measurements for both hip stems. In case of effect modification of stem type, linear regression analyses were performed for each stem separately. A P value < 0.05 was considered statistically significant.
For the determinants that were significantly associated with offset restoration (CCD-angle or preoperative offset), an operating curve (ROC) -analysis was performed to determine the optimal cutoff point of this independent variable for restoration within the limits of 5 mm. To provide a 95 % confidence interval (CI), bootstrapping procedure was performed. By using a 1000 bootstrap samples and calculating their respective cut-off values, the Standard Error was obtained to acquire the 95 %CI of the optimal cut-off point. Accompanying area under the curve (AUC) was calculated as measure of accuracy.
Additionally, to assess inter-observer and intra-observer reliability, intra-class correlation coefficients (ICC2,1) were calculated. Statistical analysis was performed using IBM SPSS Statistics, version 24.0 (Armonk, NY: IBM Corp.).
A pilot study was performed where 20 radiographs were randomly chosen and evaluated, in which 30% of conventional stems had more than 5 mm loss in FAO. Based on a 10% difference with the short stem being clinically relevant, a sample of 89 radiographs was required to identify superiority of the short stem in FAO restoration when compared to the conventional stem, with an a = 0.05 and a power of 90%. A total of 100 radiographs were included in this study.
Radiographs in a total of 100 patients were included, 72 were female. A mean age of 67 years was found, with a mean BMI of 27. Almost all patients were diagnosed with primary coxarthrosis. The mean preoperative FAO was 80mm, with a CCD-angle of 128.6° (Table 1).
| Patient characteristic | (n = 100) |
| Female, % | 72 |
| Age, mean (range) | 66.7 (41-90) |
| BMI, mean (range) | 27.3 (18.7-42.8) |
| Right hip, % | 54 |
| Indication, % | |
| Primary coxarthrosis | 98 |
| Perthes coxarthrosis | 1 |
| Posttraumatic coxarthrosis | 1 |
| Femoral offset (mm), mean (range) | 47 (30.5-67) |
| Acetabular offset (mm), mean (range) | 32.5 (22.5-47.5) |
| Femoro-acetabular offset (mm), mean (range) | 80 (62-113) |
| CCD-angle (°) | 128.6 (114.5-146) |
The short stem reached a post-templating difference of < 5 mm in FAO in all cases (100%) for both student and resident, whereas the conventional stem only achieved this in 76% and 72% of the radiographs for student and resident, respectively. The difference in FAO restoration was significant (P < 0.001), in benefit of the short stem compared to the conventional stem. A varus hip showed a failure rate of 14.3% (n = 4/24) of the non-restored hips, while a valgus hip showed no failure at all (Figure 2).
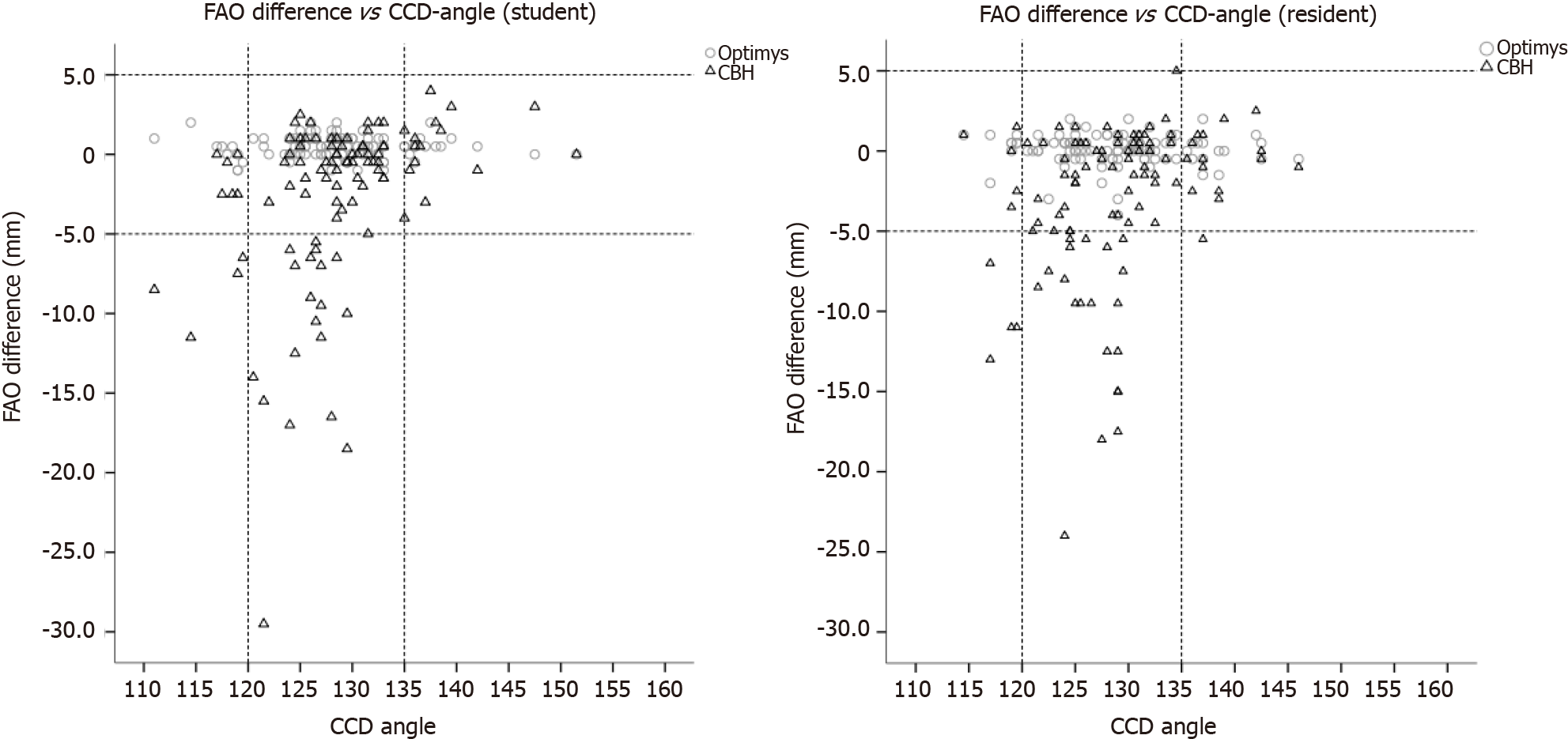
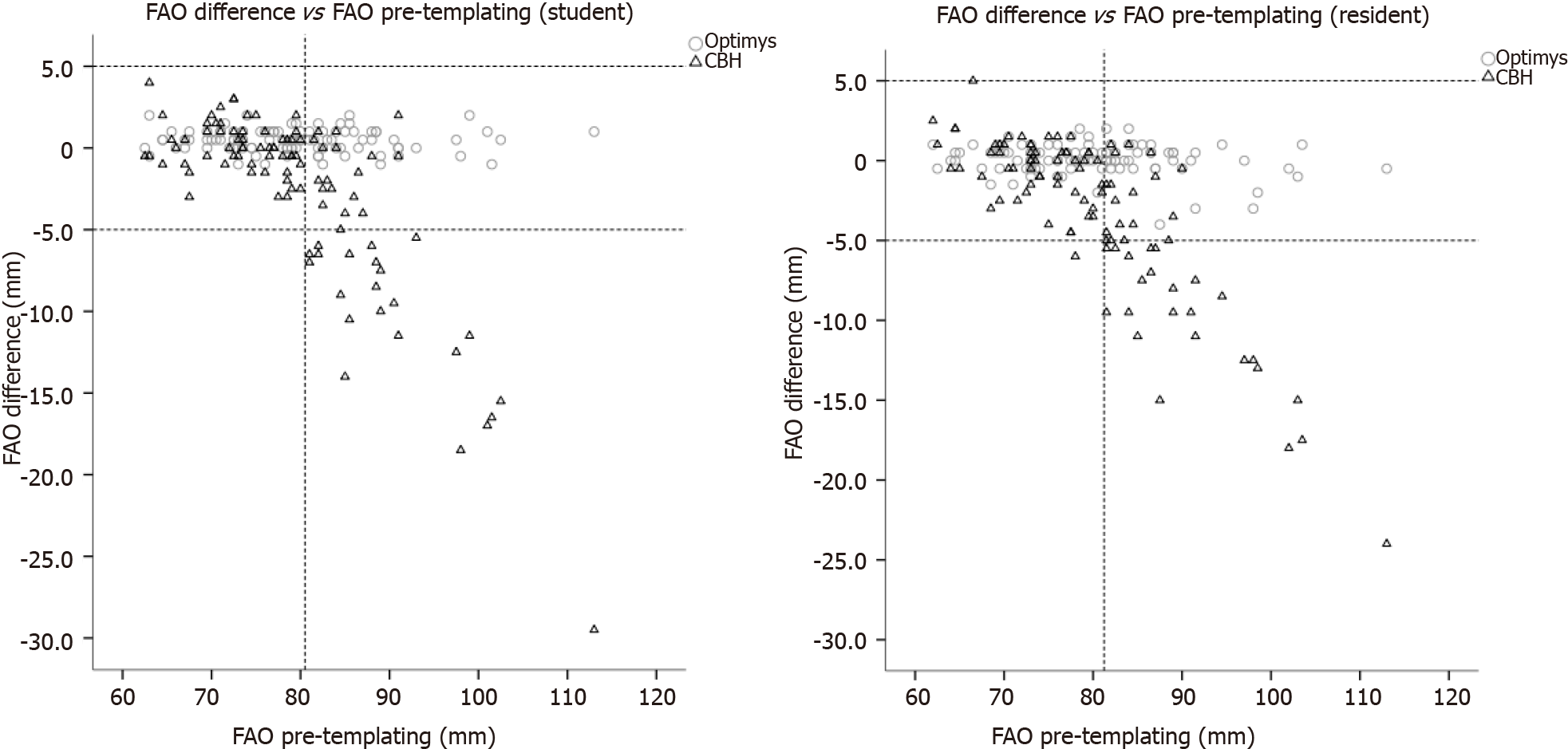
Significant interactions (P < 0.001 for all analyses) were observed between the stems and the determinants (CCD-angle and preoperative FAO), therefore analyses of the stem types were performed separately. Significant association of the CCD-angle and pre-templating FAO with the FAO restoration was only observed for the conventional stem, with the highest explained variance for the pre-templating FAO of 68% (Table 2).
| β coefficient (95%CI) | R2 | P value | |
| Student | |||
| CCD-angle (short stem) | -0.01 (-0.03, -0.02) | 0.002 | 0.62 |
| CCD-angle (conventional stem) | 0.34 (0.18, 0.50) | 0.15 | < 0.001 |
| Pre-templating FAO (short stem) | -0.004 (-0.02, 0.01) | 0.002 | 0.62 |
| Pre-templating FAO (conventional stem) | -0.45 (-0.53, -0.38) | 0.63 | < 0.001 |
| Resident | |||
| CCD-angle (short stem) | -0.01 (-0.04, 0.02) | 0.004 | 0.55 |
| CCD-angle (conventional stem) | -0.25 (-0.10, 0.41) | 0.09 | 0.002 |
| Pre-templating FAO (short stem) | -0.02 (-0.04, 0.00) | 0.03 | 0.05 |
| Pre-templating FAO (conventional stem) | -0.44 (-0.50, -0.38) | 0.68 | 0.000 |
An FAO of more than 81.25 mm showed a failure in 79% of the templated conventional stems with the resident, compared to the student with a failure rate of 76% above 80.5 mm. A negative trend-line in FAO restoration is seen as the pre-templating FAO increases by both student and resident (Figure 3). For a correct cut-off point for failure in the conventional stem, bootstrapping was performed for a ROC-analysis for the pre-templating FAO with a restoration within 5 mm. The CCD-angle was not used for bootstrapping, as the AUC was smaller than 0.5. After bootstrapping the measurements of the resident, the optimal threshold of the pre-templating FAO was 81.25 mm (95%CI: 80.75-84.75), above which the conventional stem could not restore the FAO (Figure 1), with a sensitivity of 0.96, specificity of 0.79, and an AUC of 0.94.
The results of the post-templating measurements are shown in Table 3. The short stem restored the femoral offset in all cases, whereas the conventional stem restored the femoral offset in 91% of the cases. There was a mean decrease of acetabular offset of -4 mm.
| Short stem | Conventional stem | |
| Post-templating measurements | ||
| Femoral offset (mm), mean (range) | 51.5 (3679) | 48 (3757.5) |
| Acetabular offset (mm), mean (range) | 28.5 (23.535.5) | 28.5 (23.535.5) |
| Femoro-acetabular offset (mm), mean (range) | 80 (62112.5) | 76.5 (63.589.5) |
| Difference pre- and post-templating | ||
| Femoral offset (mm), mean (range) | 4 (-2.513) | 1 (-11.511) |
| Acetabular offset (mm), mean (range) | -4 (-142.5) | -4 (-142.5) |
| Femoro-acetabular offset (mm), mean (range) | 0 (-42) | -3 (-245) |
| Restoration of femoral offset, % | 100 | 91 |
| Restoration of femoro-acetabular offset, % | 100 | 72 |
The intra-reliability of the student and the resident was both 0.99 for the pre-templating FAO. All other reliability scores were > 0.9 for both the student and the resident. Compared to the hip surgeon in pre-templating FAO, the inter-observer reliability was 0.93 and 0.95, between the student vs hip surgeon and resident vs hip surgeon respectively (Tables 4 and 5).
| Student | Resident | |
| Pre-templating FAO | 0.99 | 0.99 |
| Post-templating FAO short stem | 0.98 | 0.98 |
| Post-templating FAO conventional stem | 0.92 | 0.93 |
| CCD-angle | 0.93 | 0.94 |
| Student vs Resident | Student vs Hip surgeon | Resident vs Hip surgeon | |
| Pre-templating FAO | 0.98 | 0.93 | 0.95 |
| Pre-templating FO | 0.97 | 0.93 | 0.94 |
| Pre-templating AO | 0.97 | 0.91 | 0.92 |
| Post-templating FAO short stem | 0.97 | 0.93 | 0.95 |
| Post-templating FAO conventional stem | 0.90 | 0.84 | 0.86 |
| CCD-angle | 0.87 | 0.81 | 0.76 |
The goal of this study was to determine whether a metadiaphyseal anchoring short stem potentially facilitated a better restoration of FAO in digital templating compared to a conventional hip stem. The FAO was taken as primary measurement and not the femoral offset, as the acetabular offset can decrease postoperative due to medial placement of the acetabular component[31]. Therefore, the femoral offset must increase additionally to compensate for the loss in acetabular offset or the cup must be placed more lateral. How the acetabular component is placed varies per orthopedic surgeon. However, the acetabular cup used in this study showed an average decrease of 3.7 mm in acetabular offset in literature[32,33]. In this study there was a decrease in acetabular offset of 4 mm, which is comparable to the other studies. The FAO restoration rate within 5 mm limits for the short stem was achieved in all cases, whereas the conventional stem achieved a restoration rate of 72% (resident) and 76% (student) during digital templating. The pre-templating FAO was associated with failure in FAO restoration when using the conventional stem, as pre-templating FAO values > 81 mm had a non-restoration rate of 60% in this group. The cutoff value was determined to use for a future reference standard, as it could provide a cutoff point if clinical relevance is shown. The cutoff point of 80 mm for pre-templating FAO was chosen conservatively, at the found cutoff value (81.25 mm), because of the rapid decrease in restoration rate beyond these points, to account for variance in the general population. The CCD-angle was not clinically relevant for FAO restoration, nor was the pre-templating FAO clinically relevant for the short stem. While it was expected that varus hips would comprise the majority of hips where a conventional stem would prove insufficient in FAO restoration, this was only observed in 14% (n = 4/24) of the cases. While it stands to reason that a varus angle would increase femoral offset, a varus hip is not the primary reason for failure of FAO restoration. There was no difference in FAO restoration between both stems in valgus hips. Since there is no prior data on this specific subject, these results cannot be compared to other studies.
The short stem used in this study is a metadiaphyseal anchoring stem, with a curved design. It is to be expected that other similar designs are capable to restore the FAO in the same manner, which has previously been shown with the Nanos stem (Smith and Nephew, Marl, Germany)[15]. During surgery, the resection of the femoral neck determines for a large part the placement of the hip stem. In varus hips, a smaller part of the femoral neck will be resected for optimal placement as compared to valgus hips. Thus, a short stem thus can be neck preserving or trochanter sparing, depending on the anatomy of the patient. This is the main reason why the FAO can be restored within the 5 mm limit. Metaphyseal stems are not comparable to our outcomes, due to stem design differences.
Conventional hip stems are anchored in the diaphysis, where placement variability is limited and increasing femoral offset is only facilitated by using a larger head size or a lateral neck. Due to this rigidity in placement options, the results of this study can be interpreted for all conventional hip stems. Conventional stems can be placed into a varus position using smaller stem size, resulting in an increased femoral offset. However, long term survival could be compromised due to increased stress on the tip of the prosthesis. Therefore, this manner of placement is not recommended. In the results between the experienced hip surgeon and resident and medical student, the ICC values were lower for the conventional stem than expected. However, the hip surgeon was inclined to sooner place the conventional stem into a varus position, restoring the FAO better than the resident and medical student.
The high level of inter- and intra-observer reliability is indicative of high accuracy and reproducibility of the measurements. This reliability has also been shown in other templating studies[21,29,34,35], along with a high predictive value for prosthesis placement[6,21]. The found cutoff point may, after further clinical research, be a reason to introduce digital 2d-templating as a tool for stem type selection in combination with clinical considerations. Also, this study shows that preoperative templating can be performed reliably by medical students and orthopedic residents, after a learning curve.
There were some limitations to this study. Firstly, 2d-templating was used to measure 3-dimensional distances, which may cause underestimation of femoral offset and modification of CCD-angles[28,34]. However, radiographic 2d-templating is the method of choice for the majority of hip surgeons due to cost, radiation load, availability and has been shown to be similar in reliability and accuracy to 3d-templating with use of computed tomography[36]. The CCD-angle modification from 2d-templating may have been disadvantageous to the assessment of the CCD-angle as a predicting factor for FAO restoration. Secondly, other characteristics of the femoral canal were not examined in this study. The Dorr classification could help decide on type of femoral stem chosen for the surgery[37]. A Dorr type A with a large offset would be very difficult for a conventional stem to restore the offset, whereas a Dorr type C could lead to inadequate fixation of a short stem.
Another limitation is the fact that no postoperative measurements were done, which means that the results cannot be directly translated to clinical practice. However, the short stem was able to restore the FAO postoperative in the study of Kutzner et al[6] and recent studies showed that preoperative digital 2d-templating assured a satisfying restoration of the individual anatomy in short stems[22,26,38].
An advantage in usage of conventional stems over short stems is that there are many available studies with long-term outcomes, while these are only limited for short stems. It may also be preferable to use conventional stems in patients with suboptimal bone quality, as there is a lower load per hip stem surface unit due to the larger diaphyseal anchoring area. Theoretically, short stems could lose initial press-fit in softer bone with a higher chance on subsidence, increasing the risk of implant instability or periprosthetic fractures. Especially in older patients, the advantage of short stems, i.e., preservation of proximal bone stock, is less important and not worth the risk for potentially increasing the risk of complications. Another topic is the costs of hip stems. Conventional stems are less expensive than short stems, which is also relevant once all clinical factors have been properly considered.
The advantage in FAO restoration in this study may contribute to the use of short stems in a broadened patient group with hips with a large offset. Clinical trials will have to show whether the improved restoration in FAO will grant the expected improved functional. Other reasons to choose conventional stems over short stems still may have priority over the advantage found in this study.
In preoperative planning of FAO restoration in THA, digital templating shows that short stems with a curve following the medial calcar are potentially better at restoring the FAO compared to conventional stems if the preoperative offset is ≥ 80.0 mm.
The following steps that are necessary to take are the postoperative measurements of the short stem to see if the offset can be restored. Also, a pilot study with gait measurements in a case-matched study of patients with either a short or conventional stem will help to define if there is a difference.
If the native offset was > 80 mm, the short stem was better at restoring FAO than the conventional stem in digital templating. This could indicate that there is a specific patient population that could benefit if a short stem with a curve is chosen as femoral stem instead of the conventional stem.
A FAO more than 80mm showed a large failure rate in restoration in the conventional stems, whereas the short stem could restore the offset in all cases. The reliability of all measurements were good between in both inter- as intra-reliability, with no difference in experience.
Digital templating in a standardized X-ray of the hip were used from two ongoing cohorts, varying in hip anatomy. Orthoview was used as digital templating program. Pre-templating FAO was measured, as well as post-templating FAO measurements in the short and conventional stem. The results were divided into restored (< 5 mm difference in offset) or not-restored (> 5 mm difference in offset).
Primary objective was the femoroacetabular offset restoration in all types of hip anatomy between a short and conventional hip stem, where the acetabular component is used as a fixed parameter. Second objectives were the reliability of the measurements.
As digital templating is a reliable tool for measuring component sizes in total hip arthroplasty, this is used as measurement to see if there is a difference between a short and conventional hip stem in a wide range of hip anatomy.
Short stems are gaining popularity, as one of the possible advantages is the restoration of offset. Offset restoration improves functional outcome. This could benefit the younger patient population, as they have higher expectations of their total hip arthroplasty in their more active lifestyle.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Netherlands
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bondarenko S S-Editor: Liu M L-Editor: A P-Editor: Liu M
| 1. | Judge A, Cooper C, Williams S, Dreinhoefer K, Dieppe P. Patient-reported outcomes one year after primary hip replacement in a European Collaborative Cohort. Arthritis Care Res (Hoboken). 2010;62:480-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 120] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 2. | Hawker GA, Badley EM, Borkhoff CM, Croxford R, Davis AM, Dunn S, Gignac MA, Jaglal SB, Kreder HJ, Sale JE. Which patients are most likely to benefit from total joint arthroplasty? Arthritis Rheum. 2013;65:1243-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 146] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 3. | Singh JA, Lewallen DG. Patient-level clinically meaningful improvements in activities of daily living and pain after total hip arthroplasty: data from a large US institutional registry. Rheumatology (Oxford). 2013;52:1109-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Amlie E, Havelin LI, Furnes O, Baste V, Nordsletten L, Hovik O, Dimmen S. Worse patient-reported outcome after lateral approach than after anterior and posterolateral approach in primary hip arthroplasty. A cross-sectional questionnaire study of 1,476 patients 1-3 years after surgery. Acta Orthop. 2014;85:463-469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 89] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 5. | Skyttä ET, Jarkko L, Antti E, Huhtala H, Ville R. Increasing incidence of hip arthroplasty for primary osteoarthritis in 30- to 59-year-old patients. Acta Orthop. 2011;82:1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Kutzner KP, Kovacevic MP, Roeder C, Rehbein P, Pfeil J. Reconstruction of femoro-acetabular offsets using a short-stem. Int Orthop. 2015;39:1269-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Renkawitz T, Weber T, Dullien S, Woerner M, Dendorfer S, Grifka J, Weber M. Leg length and offset differences above 5mm after total hip arthroplasty are associated with altered gait kinematics. Gait Posture. 2016;49:196-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 116] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 8. | Sariali E, Klouche S, Mouttet A, Pascal-Moussellard H. The effect of femoral offset modification on gait after total hip arthroplasty. Acta Orthop. 2014;85:123-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 9. | McGrory BJ, Morrey BF, Cahalan TD, An KN, Cabanela ME. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995;77:865-869. [PubMed] |
| 10. | Asayama I, Chamnongkich S, Simpson KJ, Kinsey TL, Mahoney OM. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005;20:414-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 237] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 11. | Sakalkale DP, Sharkey PF, Eng K, Hozack WJ, Rothman RH. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. 2001;125-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 217] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 12. | Mahmood SS, Mukka SS, Crnalic S, Wretenberg P, Sayed-Noor AS. Association between changes in global femoral offset after total hip arthroplasty and function, quality of life, and abductor muscle strength. A prospective cohort study of 222 patients. Acta Orthop. 2016;87:36-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 136] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 13. | Foucher KC, Freels S. Preoperative factors associated with postoperative gait kinematics and kinetics after total hip arthroplasty. Osteoarthritis Cartilage. 2015;23:1685-1694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Kutzner KP, Freitag T, Donner S, Kovacevic MP, Bieger R. Outcome of extensive varus and valgus stem alignment in short-stem THA: clinical and radiological analysis using EBRA-FCA. Arch Orthop Trauma Surg. 2017;137:431-439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 15. | Ettinger M, Ettinger P, Ezechieli M, Büermann S, Budde S, Calließ T, Petri M, Thorey F. CCD and offset after Nanos short stem in total hip arthroplasty. Technol Health Care. 2013;21:149-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Bieger R, Ignatius A, Reichel H, Dürselen L. Biomechanics of a short stem: In vitro primary stability and stress shielding of a conservative cementless hip stem. J Orthop Res. 2013;31:1180-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 17. | Parchi PD, Cervi V, Piolanti N, Ciapini G, Andreani L, Castellini I, Poggetti A, Lisanti M. Densitometric evaluation of periprosthetic bone remodeling. Clin Cases Miner Bone Metab. 2014;11:226-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Sariali E, Mauprivez R, Khiami F, Pascal-Mousselard H, Catonné Y. Accuracy of the preoperative planning for cementless total hip arthroplasty. A randomised comparison between three-dimensional computerised planning and conventional templating. Orthop Traumatol Surg Res. 2012;98:151-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 19. | The B, Diercks RL, van Ooijen PM, van Horn JR. Comparison of analog and digital preoperative planning in total hip and knee arthroplasties. A prospective study of 173 hips and 65 total knees. Acta Orthop. 2005;76:78-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 90] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 20. | Shaarani SR, McHugh G, Collins DA. Accuracy of digital preoperative templating in 100 consecutive uncemented total hip arthroplasties: a single surgeon series. J Arthroplasty. 2013;28:331-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 21. | Schmidutz F, Steinbrück A, Wanke-Jellinek L, Pietschmann M, Jansson V, Fottner A. The accuracy of digital templating: A comparison of short-stem total hip arthroplasty and conventional total hip arthroplasty. Int Orthop. 2012;36:1767-1772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Snijders TE, van Erp JHJ, de Gast A. Restoring femoral offset and leg length; the potential of a short curved stem in total hip arthroplasty. J Orthop. 2019;16:396-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Lecerf G, Fessy MH, Philippot R, Massin P, Giraud F, Flecher X, Girard J, Mertl P, Marchetti E, Stindel E. Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res. 2009;95:210-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 265] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 24. | Flecher X, Ollivier M, Argenson JN. Lower limb length and offset in total hip arthroplasty. Orthop Traumatol Surg Res. 2016;102:S9-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 153] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 25. | Archibeck MJ, Tripuraneni KR, Carothers JT, Junick DW, Munson NR, Murray-Krezan CM. Prospective, Randomized, Surgeon-Blinded Comparison of Standard Magnification Assumption vs Magnification Marker Usage for Preoperative Templating in Total Hip Arthroplasty. J Arthroplasty. 2017;32:3061-3064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Kutzner KP, Pfeil J, Kovacevic MP. Preoperative digital planning vs postoperative outcomes in total hip arthroplasty using a calcar-guided short stem: frequent valgization can be avoided. Eur J Orthop Surg Traumatol. 2017;27:643-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 27. | Mahmood SS, Mukka SS, Crnalic S, Wretenberg P, Sayed-Noor AS. Association between changes in global femoral offset after total hip arthroplasty and function, quality of life, and abductor muscle strength. A prospective cohort study of 222 patients. Acta Orthop. 2016;87:36-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 136] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 28. | Amenabar T, Marimuthu K, Hawdon G, Gildone A, McMahon S. Total hip arthroplasty using a short-stem prosthesis: restoration of hip anatomy. J Orthop Surg (Hong Kong). 2015;23:90-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | González Della Valle A, Comba F, Taveras N, Salvati EA. The utility and precision of analogue and digital preoperative planning for total hip arthroplasty. Int Orthop. 2008;32:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 30. | Cassidy KA, Noticewala MS, Macaulay W, Lee JH, Geller JA. Effect of femoral offset on pain and function after total hip arthroplasty. J Arthroplasty. 2012;27:1863-1869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 31. | Bhaskar D, Rajpura A, Board T. Current Concepts in Acetabular Positioning in Total Hip Arthroplasty. Indian J Orthop. 2017;51:386-396. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 32. | Erivan R, Aubret S, Villatte G, Mulliez A, Descamps S, Boisgard S. Does using a polyethylene RM press-fit cup modify the preparation of the acetabulum and acetabular offset in primary hip arthroplasty? Orthop Traumatol Surg Res. 2017;103:669-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Meermans G, Doorn JV, Kats JJ. Restoration of the centre of rotation in primary total hip arthroplasty: the influence of acetabular floor depth and reaming technique. Bone Joint J. 2016;98-B:1597-1603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 63] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 34. | Mahmood SS, Al-Amiry B, Mukka SS, Baea S, Sayed-Noor AS. Validity, reliability and reproducibility of plain radiographic measurements after total hip arthroplasty. Skeletal Radiol. 2015;44:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 35. | Bertz A, Indrekvam K, Ahmed M, Englund E, Sayed-Noor AS. Validity and reliability of preoperative templating in total hip arthroplasty using a digital templating system. Skeletal Radiol. 2012;41:1245-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 36. | Merle C, Waldstein W, Pegg EC, Streit MR, Gotterbarm T, Aldinger PR, Murray DW, Gill HS. Prediction of three-dimensional femoral offset from AP pelvis radiographs in primary hip osteoarthritis. Eur J Radiol. 2013;82:1278-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 37. | Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993;14:231-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 579] [Cited by in RCA: 666] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 38. | Erivan R, Muller AS, Villatte G, Millerioux S, Mulliez A, Boisgard S, Descamps S. Short stems reproduce femoral offset better than standard stems in total hip arthroplasty: a case-control study. Int Orthop. 2020;44:45-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |