Published online Dec 18, 2022. doi: 10.5312/wjo.v13.i12.1056
Peer-review started: September 17, 2022
First decision: October 12, 2022
Revised: October 12, 2022
Accepted: November 29, 2022
Article in press: November 29, 2022
Published online: December 18, 2022
Processing time: 89 Days and 15 Hours
Orthopedic oncology surgeons commonly engage in prolonged and complex surgical procedures. These types of surgeries increase the risk of physical and psychological stressors, which may in turn make these physicians prone to work-related occupational injuries.
The aim of this study was to explore in orthopedic oncologists, the prevalence of work-related physical injuries and psychological disturbances.
A modified version of the physical discomfort survey was developed to assess occupational injuries among orthopedic oncology surgeon members of the Musculoskeletal Tumor Society, the Canadian Orthopedic Oncology Society and European Musculoskeletal Oncology Societies. The survey was sent by email, and it explored musculoskeletal complaints, psychological disturbances, treatment required for these complaints and the requirement of time off work.
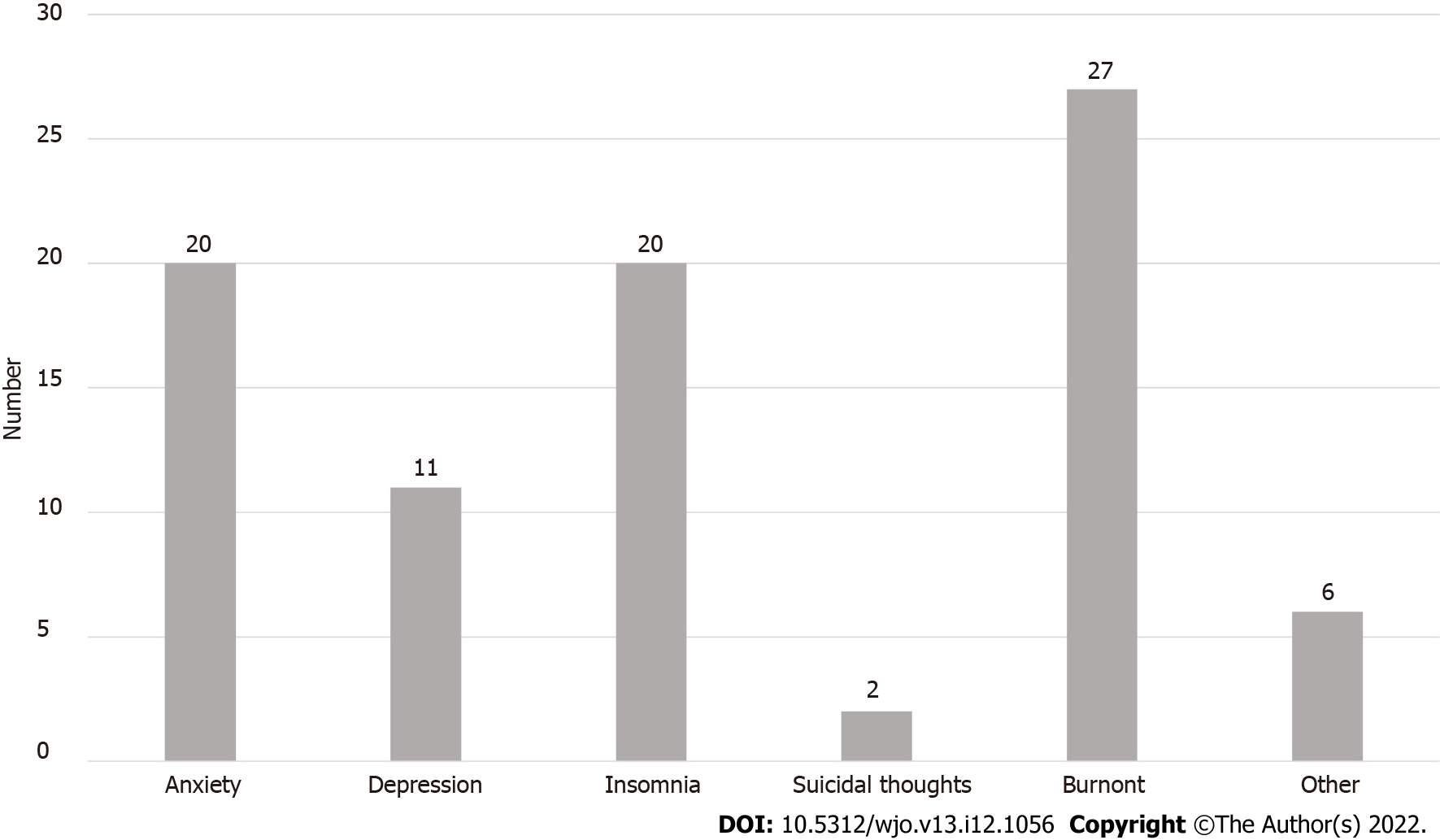
A total of 67 surgeon responses were collected. A high number of orthopedic oncologists (84%) reported an occupational injury. Low back pain (39%) was the most prevalent musculoskeletal condition, followed by lumbar disk herniation (16%), shoulder tendinitis (15%) and lateral epicondylitis (13%). Of the cohort, 46% required surgery and 31% required time off work due to their injury. Thirty-three respondents reported a psychological disorder. Burnout (27%), anxiety (20%) and insomnia (20%) were the most commonly reported. Time required off work due to injury was associated with old age and years in practice.
Orthopedic oncology surgeons report a high prevalence of work-related disorders. Lower back related injury and burnout were the most reported disorders. Improving operative room ergonomics and prevention of stress related to the work environment should be areas to explore in upcoming research.
Core Tip: Orthopedic oncologists reported a high prevalence of occupational injury and work-related stress. Futures studies should be directed towards exploring areas to improve the operative environment and methods to decrease conditions associated with stress at work.
- Citation: Alaseem AM, Turcotte RE, Ste-Marie N, Alzahrani MM, Alqahtani SM, Goulding KA. Occupational injuries and burn out among orthopedic oncology surgeons. World J Orthop 2022; 13(12): 1056-1063
- URL: https://www.wjgnet.com/2218-5836/full/v13/i12/1056.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i12.1056
Alarming rates of occupational injuries have been previously reported in different surgical fields including orthopedic surgery[1-5]. It has been an area of interest and investigation due to the implications of these injuries on surgeons, health care system and the quality of provided care[6-9]. Occupational injuries are either work-related injuries or illnesses caused by incidents at a workplace or previous illnesses aggravated by work-related injuries, that could negatively impact the well-being of the affected workers or the quality of provided care[10-12]. Orthopedic surgeons are more vulnerable to a variety of work-related injuries and hazards associated with the nature of their profession such as blood born infections, sharp injuries, noise-induced hearing impairment, exposure to radiation and chemicals, heavy physical workload, emotional and psychological disturbances[13-16].
Several studies have suggested that orthopedic surgeons are at increased rates of occupational injuries[17-20]. When compared to general surgeons, orthopedic surgeons were found to have higher rates of subjective physical injuries. The most reported injuries were back pain, neck pain and upper extremity related complaints[15,21,22]. Furthermore, the psychological disturbances including burnout rates, were found to be higher among orthopedic surgeons as compared to other medical professions and the general population, which in turn may negatively impact the quality of patient care due to increased medical errors and depersonalization[10,23].
Orthopedic oncology is a subspecialty of orthopedics that is physically and psychologically challenging as it involves prolonged and complex surgical procedures, as well as higher rates of serious surgical complications and limited survivorship and functional outcome relating to the oncology patient population. Consequently, such physical and psychological stressors may subject orthopedic oncology surgeons to higher rates of work-related “occupational” injuries that can impact their quality of life, wellness and the quality of delivered patient care. These occupational stressors can lead to preventable musculoskeletal injuries, time off work, increased burnout rates, emotional and psychological disturbances. Investigating this aspect among orthopedic oncology surgeons can help institutions and occupational health agencies to develop preventive strategies to minimize the negative implications of these injuries on the quality of provided care and promote surgeons’ personal well-being.
To our knowledge, there are no studies to date investigating the occupational injuries among orthopedic oncology surgeons. The aim of this survey is to explore occupational injuries in orthopedic oncologists, including their prevalence and characteristics.
An anonymous online, web-based, modified version of the Physical Discomfort Survey (originally developed by the Workplace Safety and Health Division of Manitoba, Canada)[24] and modified version of Maslach Burnout Inventory-Human services survey for medical personnel[25] was emailed to all surgeon members of Musculoskeletal Tumor Society (MSTS), Canadian Orthopedic Oncology Society (CANOOS), and European Musculoskeletal Oncology Society (EMSOS). Only practicing orthopedic oncology surgeon members of the above-mentioned societies were eligible to participate in our study. The first invitation email was sent out in November 2016 and a reminder email was sent out in January 2017. The survey was closed by mid-February 2017. To minimize the magnitude of potential selection and response biases, we sent our survey to all surgeon members of three large orthopedic oncology societies in North America and Europe. Furthermore, we attempted to reduce the potential response bias by sending a subsequent reminder email.
The survey was divided into 3 parts, the first part included questions about participant’s demographic data (age, gender, hand dominance), practice setting (academic, community or private), practice duration in years and the average operative caseload per year. The second part of the survey was about the musculoskeletal complaints by region (neck, lower back, upper extremity and lower extremity). For each question, participants were asked about the diagnosis, medical or surgical treatments (if any) and if they ever required work stoppage consequently. The third part of the survey involved questions concerning psychological disturbances (anxiety, depression, insomnia, suicidal thoughts and burnout symptoms) and symptoms of “burnout” (emotional exhaustion, depersonalization, low job satisfaction), treatments required (if any) and any time off work needed as a result.
Descriptive statistics were used to report participants’ demographics. The prevalence of occupational injury was estimated as the number of injuries per total number of respondents. To determine significant associations between patient demographics and occupational hazards, we performed classical tests of hypothesis as well as logistic regression analysis. Statistical significance was set at an alpha of 0.05 and analysis was carried out using Stata v12.1 (Statacrop).
Sixty-seven orthopedic oncology surgeons (58 male and 9 female surgeons) completed the survey (22% response rate). Of the respondent, 40.3%, 43.3% and 6% of respondents were from MSTS, EMSOS and CANOOS, respectively. Most of the participant surgeons are practicing in academic setting (83.3%). The oncologic yearly caseload was seventy-five cases or more in 38.8% of the surgeons.
Eighty four percent of surveyed orthopedic oncology surgeons reported an occupational injury. Musculoskeletal injuries were reported by 76% of participating surgeons, psychological injuries by 50% and both by 43%. The most common musculoskeletal injuries were low back pain (39%), shoulder symptoms (27%), neck pain (24%), lumbar disc herniation (16%), shoulder tendinitis (15%), lateral epicondylitis (13%), hip or knee osteoarthritis and varicose veins (10 % each) (Figure 1). Consequently, time off work was reported by 33.3% surgeons and 27% required treatment including either medical or surgical treatment. Exacerbation of musculoskeletal injuries was experienced by 18% of respondents (Table 1).
| Region | Proportion of injured respondents (%) | Proportion of injured respondents requiring treatment (%) | Proportion of injured respondents requiring surgery (%) | Proportion of treated respondents requiring time off work (%) |
| Neck | 24 | 56 | 6 | 13 |
| Shoulder | 27 | 72 | 22 | 22 |
| Elbow | 13 | 67 | 0 | 0 |
| Forearm, wrist and hand | 39 | 62 | 23 | 23 |
| Hip and thigh | 7 | 80 | 20 | 17 |
| Knee and lower leg | 13 | 56 | 56 | 40 |
| Ankle/foot | 7 | 100 | 20 | 40 |
| Lower back | 55 | 51 | 8 | 24 |
Thirty-three surgeons reported a psychological disturbance (50%). The most prevalent were burnout (27%), anxiety and insomnia (20% each) and depression (11%). More seriously, suicidal thought was reported by one participant (Figure 2). Medical and/or psychiatric treatment was required by 18% of respondents and the time off work was required by 3% (Table 2). Young age (35-45 years) was the only significant factor associated with developing symptoms of burnout (P < 0.015).
| Disorder | Number of respondents with disorders | Number of treated respondents requiring treatment | Proportion of treated respondents requiring medical treatment | Proportion of treated respondents requiring time-off |
| Anxiety | 20 | 5 | 2 | 1 |
| Depression | 11 | 5 | 3 | 1 |
| Insomnia | 20 | 2 | 1 | 0 |
| Suicidal thoughts | 2 | 1 | 1 | 0 |
| Burnout | 27 | 5 | 2 | 1 |
| Other | 6 | 1 | 1 | 0 |
| Total | 33 | 19 | 10 | 3 |
Eighteen surgeons (26.9%) required time off work due to occupational injuries (17 musculoskeletal injuries and 1 psychological disturbance). Factors significantly associated with time off work were age and years of practice of the surgeon (P < 0.011) in the logistic regression analysis models performed.
Our study revealed a concerning prevalence of occupational injuries among orthopedic oncology surgeons (84%), which is much higher than the previously reported rates in other orthopedic subspecialties[11,17-20]. This could lead to consequences not only on the surgeon’s career, but also on the quality and cost of provided health care. One third (33.3%) of participating surgeons reported periods of work stoppage due to work-related injuries and 27% required either medical or surgical treatments. Fifty percent of respondents reported symptoms of occupational psychological disturbances, with burnout being the most reported (27%) followed by insomnia and anxiety (20% each). Orthopedic surgeons in general have higher work-related subjective musculoskeletal symptoms when compared to general surgeons[15]. However, orthopedic oncology is a unique field in orthopedics which deals with complex osseous and soft tissue tumors and therefore, orthopedic oncologists are involved in prolonged meticulous surgical procedures with relatively higher complication rates than any other orthopedic specialties. Furthermore, Orthopedic oncologists face psychological stressors as they are involved in psychological and emotional aspects associated with the management of oncology patients. Hence, it is not surprising that this surgeon population have higher rates of occupational injuries including musculoskeletal and psychological disturbances as shown in the results of this study.
Several factors have been shown in the literature as contributing factors to the high rates of occupational injuries among surgeons[4-8]. The nature of their work involves poor ergonomics such as lengthy non-neutral postures while operating, repetitive intra-operative physically demanding tasks, the height of operating table and the non-ergonomically designed surgical instruments[5-8]. New ergonomic innovations have been suggested to improve the operating room environment and minimize the risks of occupational injuries; however, the utilization of these devices is not yet popularized. These factors are applicable even more to orthopedic oncologists due to the complexity and nature of their profession. However, if such work-related injuries are not addressed early, it may progress to more sever morbidity and adversely influence the surgeon’s wellbeing and career lifespan.
In addition, psychological disturbances were also found to be high in surgeons, especially in surgical oncologists in the current literature[26]. This is consistent with our results showing high psychological morbidity rates among orthopedic oncologists. Nevertheless, many surgeons may neglect their occupational health issues and thus not pursue the appropriate help when needed, likely due to lack of mindfulness about the potential occupational health injuries and the heavy workload nature of their professions[8].
The limitations of our survey study are similar to most survey studies in the literature. One of the limitations is the subjective nature of self-reported occupational musculoskeletal and psychological complaints. However, our participants are practicing surgeons and most likely they are accurately reporting their health issues. Additionally, the primary focus of our study is to assess the magnitude of occupational injuries among orthopedic oncologist and the characteristics of these injuries. Most work-related symptoms are subjective complaints and may not be associated with objective clinical findings. Therefore, it is widely accepted to evaluate the prevalence of occupational injuries by self-administered surveys. Another possible argument is the significantly higher prevalence rate of occupational injuries reported in our study. This possibly inflated prevalence could be related to that some participants in such surveys are currently or have previously been affected by occupational injuries, thus probably leading to possible response or selection bias. Although we believe this is certainly a valid concern, we still anticipate a high rate of occupational injuries among orthopedic oncologists if we assume the non-respondents are not affected with occupational injuries. The surveys used in our current study included modified self-reported outcomes, which could be an area of limitation. Future research should be directed at studying the reliability, validity, and area of weaknesses of these surveys. One of the strengths of our study is that the study sample, although relatively small, is representative of the orthopedic oncology surgeons’ population in North America and Europe, which is considered not a large population.
The purpose of this survey was to increases the mindfulness of work-related health issues and its possible consequences on surgeons’ wellness, patient care delivery and institutional health quality measures. Our data should help health institutions and occupational health services develop early educational programs directed to surgeons and provide preventive and supportive ergonomic measures in order to improve the surgeons’ wellness and minimize the undesirable consequences of occupational injuries on the health care system.
Orthopedic oncology surgeons commonly perform complex and prolonged surgical. This places the surgeon at increased risk of not only physical but also psychological stressors.
The effect of these physical and mental burdens on both the surgeon and healthcare system has not been adequately studied.
We aimed to explore occupational injuries among orthopedic oncology surgeons, especially prevalence, characteristics and their effect on practice.
A modified version of the physical discomfort web-based survey was used to determine prevalence and patterns of occupational injuries among orthopedic oncology and this survey was sent to multiple orthopedic oncology societies.
The overall prevalence of occupational injury among our surgeon cohort was 84% (musculoskeletal 76%; psychological 50%; and both 43%). Low back pain was the most prevalent musculoskeletal conditions and burnout was the most prevalent psychological disorder. Old age and years in practice were associated with requirement of time off work.
We found a high prevalence of occupational injuries in orthopedic oncologists, with a large proportion of them requiring time off due to these injuries.
Future research should be directed towards exploring strategies directed at decreasing the prevalence of these injuries through improved ergonomics and optimized working environments to minimize stress associated with the workplace.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Canada
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jian X, China; Mollaei N, Portugal; Temesgen LM, Ethiopia S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Giberti C, Gallo F, Francini L, Signori A, Testa M. Musculoskeletal disorders among robotic surgeons: a questionnaire analysis. Arch Ital Urol Androl. 2014;86:95-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Davis WT, Fletcher SA, Guillamondegui OD. Musculoskeletal occupational injury among surgeons: effects for patients, providers, and institutions. J Surg Res. 2014;189:207-212.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 126] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 3. | Capone AC, Parikh PM, Gatti ME, Davidson BJ, Davison SP. Occupational injury in plastic surgeons. Plast Reconstr Surg. 2010;125:1555-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 83] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Dianat I, Bazazan A, Souraki Azad MA, Salimi SS. Work-related physical, psychosocial and individual factors associated with musculoskeletal symptoms among surgeons: Implications for ergonomic interventions. Appl Ergon. 2018;67:115-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 5. | Park A, Lee G, Seagull FJ, Meenaghan N, Dexter D. Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg. 2010;210:306-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 346] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 6. | Soueid A, Oudit D, Thiagarajah S, Laitung G. The pain of surgery: pain experienced by surgeons while operating. Int J Surg. 2010;8:118-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 137] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 7. | Szeto GP, Ho P, Ting AC, Poon JT, Cheng SW, Tsang RC. Work-related musculoskeletal symptoms in surgeons. J Occup Rehabil. 2009;19:175-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 178] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 8. | Vijendren A, Yung M, Sanchez J. The ill surgeon: a review of common work-related health problems amongst UK surgeons. Langenbecks Arch Surg. 2014;399:967-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Vijendren A, Yung M, Sanchez J, Duffield K. Occupational musculoskeletal pain amongst ENT surgeons - are we looking at the tip of an iceberg? J Laryngol Otol. 2016;130:490-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 10. | Daniels AH, DePasse JM, Kamal RN. Orthopaedic Surgeon Burnout: Diagnosis, Treatment, and Prevention. J Am Acad Orthop Surg. 2016;24:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Davis WT, Sathiyakumar V, Jahangir AA, Obremskey WT, Sethi MK. Occupational injury among orthopaedic surgeons. J Bone Joint Surg Am. 2013;95:e107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 12. | Lester JD, Hsu S, Ahmad CS. Occupational hazards facing orthopedic surgeons. Am J Orthop (Belle Mead NJ). 2012;41:132-139. [PubMed] |
| 13. | Maniar HH, Tawari AA, Suk M, Bowen TR, Horwitz DS. Percutaneous and Mucocutaneous Exposure Among Orthopaedic Surgeons: Immediate Management and Compliance With CDC Protocol. J Orthop Trauma. 2015;29:e391-e394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Matityahu A, Duffy RK, Goldhahn S, Joeris A, Richter PH, Gebhard F. The Great Unknown-A systematic literature review about risk associated with intraoperative imaging during orthopaedic surgeries. Injury. 2017;48:1727-1734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 15. | Mirbod SM, Yoshida H, Miyamoto K, Miyashita K, Inaba R, Iwata H. Subjective complaints in orthopedists and general surgeons. Int Arch Occup Environ Health. 1995;67:179-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 31] [Reference Citation Analysis (0)] |
| 16. | Romanova K, Vassileva J, Alyakov M. Radiation exposure to the eye lens of orthopaedic surgeons during various orthopaedic procedures. Radiat Prot Dosimetry. 2015;165:310-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | AlQahtani SM, Alzahrani MM, Harvey EJ. Prevalence of musculoskeletal disorders among orthopedic trauma surgeons: an OTA survey. Can J Surg. 2016;59:42-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Alqahtani SM, Alzahrani MM, Tanzer M. Adult Reconstructive Surgery: A High-Risk Profession for Work-Related Injuries. J Arthroplasty. 2016;31:1194-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 19. | Alzahrani MM, Alqahtani SM, Tanzer M, Hamdy RC. Musculoskeletal disorders among orthopedic pediatric surgeons: an overlooked entity. J Child Orthop. 2016;10:461-466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Auerbach JD, Weidner ZD, Milby AH, Diab M, Lonner BS. Musculoskeletal disorders among spine surgeons: results of a survey of the Scoliosis Research Society membership. Spine (Phila Pa 1976). 2011;36:E1715-E1721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 93] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 21. | Alzahrani MM, Alqahtani SM, Pichora D, Bicknell R. Work-related musculoskeletal injuries among upper extremity surgeons: A web-based survey. World J Orthop. 2021;12:891-898. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Alqahtani SM, Alzahrani MM, Bicknell R, Pichora D. Prevalence and factors of work-related musculoskeletal disorders among hand surgeons. World J Orthop. 2022;13:465-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 23. | Sargent MC, Sotile W, Sotile MO, Rubash H, Barrack RL. Quality of life during orthopaedic training and academic practice. Part 1: orthopaedic surgery residents and faculty. J Bone Joint Surg Am. 2009;91:2395-2405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 138] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 24. | Physical Discomfort Survey-Workplace Safety and Health Division of Manitoba, Canada. [Internet] [accessed 20 October 2022]. Available from: http://www.gov.mb.ca/inr/publications/safe_workplace/section-i/section-i-c/pubs/appendix-i-c-2-symptoms-survey.pdf. |
| 25. | Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual (4th Edition). Menlo Park, CA: Mind Garden, Inc, 2018. |
| 26. | Taylor C, Graham J, Potts HW, Richards MA, Ramirez AJ. Changes in mental health of UK hospital consultants since the mid-1990s. Lancet. 2005;366:742-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 111] [Article Influence: 5.6] [Reference Citation Analysis (0)] |