Published online Oct 18, 2022. doi: 10.5312/wjo.v13.i10.911
Peer-review started: June 7, 2022
First decision: August 4, 2022
Revised: August 18, 2022
Accepted: September 12, 2022
Article in press: September 12, 2022
Published online: October 18, 2022
Processing time: 132 Days and 4.2 Hours
Osteoarthritis (OA) is the most common cause of pain and disability, predominantly affecting the knee. The current management of knee OA falls short of completely stopping disease progression, particularly in Kellgren-Lawrence (KL) grade 3 and 4 knee OA. As such, joint replacement is often recommended, although only 15%-33% of candidates accept it. Alternative therapeutic options are still needed to prevent the progression of joint damage and delay the need for knee arthroplasty.
To investigate the effect of adjunctive platelet rich plasma (PRP) and hyaluronic acid (HA) after arthroscopic debridement in KL grade 3 and 4 knee OA.
This retrospective cohort study used the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score and WOMAC sub-scores (pain, stiffness, and function) to assess 21 patients, grouped according to medical record data of treatment received: Arthroscopic debridement (n = 7); arthroscopic debridement with PRP (n = 7); or arthroscopic debridement with HA (n = 7). WOMAC scores and sub-scores at baseline and at 3 mo and 5 mo posttreatment were recorded. The three-group data were statistically analyzed using the tests of paired t, one-way analysis of variance, and post hoc least significant difference.
All three treatment groups showed significant improvements in WOMAC score and sub-scores from before treatment to 3 mo and 5 mo after treatment. However, the arthroscopic debridement with PRP treatment group, in particular, showed a significantly lower WOMAC pain score than the group who received arthroscopic debridement alone at 5 mo after the procedure (P = 0.03).
Compared to arthroscopic debridement alone, adjunctive PRP after arthroscopic debridement significantly lessened the patients’ pain symptom.
Core Tip: This manuscript highlights the alternative approaches in managing knee osteoarthritis of Kellgren-Lawrence grade 3 and 4. Outcomes of arthroscopic debridement, arthroscopic debridement with platelet-rich plasma (PRP), or arthroscopic debridement with hyaluronic acid were evaluated prior to treatment and at 3 mo and 5 mo after the procedure. According to the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score and sub-scores (pain, stiffness, function), arthroscopic debridement with PRP provided significantly lower pain than arthroscopic debridement after treatment, however neither treatment was superior in the ability to improve total WOMAC score.
- Citation: Tirtosuharto H, Wiratnaya IGE, Astawa P. Adjunctive platelet-rich plasma and hyaluronic acid injection after arthroscopic debridement in Kellgren-Lawrence grade 3 and 4 knee osteoarthritis. World J Orthop 2022; 13(10): 911-920
- URL: https://www.wjgnet.com/2218-5836/full/v13/i10/911.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i10.911
Osteoarthritis (OA) is the leading cause of pain and disability, with a 10-fold increased incidence and prevalence occurring in 30-years-old to 65-years-old age range[1-3]. In Indonesia, the prevalence of knee OA is appreciable, at 15.5% for men and 12.7% for women, with rates following the trend of increase with increased age[4].
To date, the management of knee OA is only capable of addressing symptomatic features and has been ineffective in halting progression of the disease itself. In the advanced stage of knee OA, joint replacement is the recommended management; since only 15%-33% of knee arthroplasty candidates are willing to submit themselves to the extensive surgery and recovery, an alternative treatment option is needed[5-8]. The proposed treatment involves adjunctive administration of platelet rich plasma (PRP) or hyaluronic acid (HA) following the knee arthroscopy. PRP is the blood’s plasma component that has been prepared with a high concentration of platelets, which express the cytokines and growth factors to stimulate cartilage repair and inflammation decrease[6,7,9]. In knee OA, PRP has been shown to improve both the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score and the 36-item Short Form survey (commonly known as the SF-36) score[10,11]. Intraarticular HA injection has shown the benefits of chondroprotective effect, pain decrease, inflammatory response modulation and endogenous HA synthesis increase, and its wide application has demonstrated success in decreasing knee OA symptoms[12-15].
In this study, we aimed to investigate whether adjunctive treatment with PRP or HA after arthroscopic debridement was able to provide better outcomes then arthroscopic debridement alone.
This was a retrospective cohort study based on medical record data. All treatments were performed by a single orthopedic surgeon in Denpasar, Bali, Indonesia between January 2021 and December 2021. Data were collected at Sanglah General Hospital and Surya Husada Ubung Hospital (Denpasar, Bali, Indonesia). The study sample was made up of KL grade 3 and 4 knee OA patients who had undergone arthroscopic debridement, arthroscopic debridement with PRP, or arthroscopic debridement with HA. The inclusion criteria were KL grade 3 and 4 knee OA patients, with diagnosis based on American College of Rheumatology Clinical and Radiological Classification Criteria, of ages 40-years-old to 70-years-old, and who had failed conservative treatment. Patients with knee deformity due to trauma or congenital knee deformity were excluded. The study sample size was calculated according to a false positive rate of 5% (α = 0.5) and 80% power (β = 0.2), and on a predicted difference 56.87 point on mean WOMAC score changes (standard deviation 37.26)[16]. Accordingly, for multiple-group comparison, a minimum of 6 patients per group were determined to be required, and we included 7 patients per group.
The total 21 patients (n = 7 per three treatment groups) underwent the standard arthroscopic debridement procedure under general anesthesia. As a minimally invasive procedure, arthroscopic debridement is performed by inserting arthroscopes through small incisions, followed by debridement and irrigation. Debridement of necrotic chondral tissue is carried out to remove it from the cartilage, with subsequent saline-solution washing by irrigation[17]. For our patients, either PRP or HA was administered at 1 wk postsurgically via intraarticular injection to the patelofemoral joint under aseptic conditions. The HA treatment consisted of 3 mL Hyajoint-plus® (Macopharma, Tourcoing, France) at 20 mg/mL, while the PRP preparation protocol consisted of RegenKit® (Regen Lab, New York, NY, United States) administered as 5 mL. Any meniscus tear found during surgery was recorded and noted for its potential to serve as a confounding factor. There were no adverse reactions noted in the medical record data for any of the total 21 patients.
WOMAC score is an assessment instrument specific to OA that is widely used to evaluate symptom improvement in knee OA. WOMAC sub-scores consist of pain, stiffness, and functional assessments. Overall, the WOMAC and its sub-scores are reputed as reliable, valid, and responsive to change in patients with OA symptoms[18]. The highest total score is 96, with a lower score indicating improvement in knee OA symptoms.
We did not use magnetic resonance imaging (MRI) assessment as outcome measurement since this imaging modality was not in routine use in our hospitals during the study period.
Data were analyzed using the Statistical Package for Social Sciences software (IBM Corp., Armonk, NY, United States). The Shapiro-Wilks normality test was performed. One-way analysis of variance was used to compare WOMAC scores among the three groups, and post hoc analysis was conducted using the least significant difference (commonly known as LSD) test. The paired t-test was used to compare baseline and follow-up WOMAC scores. P < 0.05 was considered statistically significant.
Among the 21 total patients included in the study, 61.9% were female and 38.1% were male. The mean age of the patients was 59.29 ± 6.61 years. Sixty-six percent of the patients had right knee OA and the remaining patients had left knee OA. None of the subjects had bilateral knee OA. Seventy-one percent of the patients had KL grade 3, and meniscus tear was found in 10 patients (47.6%) during surgery. The subjects’ characteristics are summarized in Table 1.
| Characteristic | Mean | Arthroscopic debridement | Arthroscopic debridement + HA | Arthroscopic debridement + PRP | P value | |
| Patients | 7 | 7 | 7 | 7 | N/A | |
| Age (yr) | 59.29 ± 6.61 | 58.29 ± 6.75 | 57.29 ± 7.16 | 62.29 ± 5.71 | 0.34 | |
| Sex | Male | 8 (38.1%) | 3 (42.9%) | 2 (28.6%) | 3 (42.9%) | 0.82 |
| Female | 13 (61.9%) | 4 (57.2%) | 5 (71.4%) | 4 (57.2%) | ||
| Affected knee | Right | 14 (66.7%) | 5 (71.4%) | 6 (85.7%) | 3 (42.9%) | 0.22 |
| Left | 7 (33.3%) | 2 (28.6%) | 1 (14.3%) | 4 (57.2%) | ||
| KL grade | 3 | 15 (71.4%) | 7 (100%) | 2 (28.6%) | 6 (85.7%) | 0.01 |
| 4 | 6 (28.6%) | 0 | 5 (71.4%) | 1 (14.3%) | ||
| Meniscus tear | Yes | 10 (47.6%) | 2 (28.6%) | 5 (71.4%) | 3 (42.9%) | 0.25 |
| No | 11 (52.4%) | 5 (71.4%) | 2 (28.6%) | 4 (57.1%) | ||
Before/after treatment comparisons showed that patients in all three groups had significantly lower WOMAC scores at 3 mo and 5 mo follow-up (Table 2). In the arthroscopic debridement group, a significant reduction was also found in pain score and physical function score at 3 mo follow-up (P = 0.002 and 0.011 respectively) and 5 mo follow-up (P = 0.000 and 0.001 respectively) but not in stiffness score, which was not significantly reduced at either the 3 mo or 5 mo follow-up (P = 0.091 and 0.067 respectively). In the arthroscopic debridement with HA group, a significant reductions was found in pain score and physical function score at 3 mo follow-up (P = 0.001 and 0.004 respectively) and 5 mo follow-up (P =0.001 and 0.000 respectively). In this group, the stiffness score was significantly reduced at the 5 mo follow-up (P = 0.026) but not at the 3 mo follow-up (P = 0.160). The arthroscopic debridement with PRP group showed a significant reduction in all WOMAC sub-scores at the 3 mo follow-up (P = 0.000, 0.019, and 0.001) and 5 mo follow-up (P = 0.000, 0.011, and 0.001 for pain, stiffness, and physical function scores respectively). Results from the paired t-test analyses are detailed in Table 2.
| Treatment | Outcome | Baseline | 3 mo | 5 mo | Paired t-test | |||
| Baseline vs 3 mo | Baseline vs 5 mo | |||||||
| t value | P value | t value | P value | |||||
| Arthroscopic debridement | WOMAC score | 49.43 ± 10.33 | 28.57 ± 9.09 | 18.57 ± 7.12 | 5.143 | 0.002 | 8.712 | 0.000 |
| Pain score | 12.43 ± 2.76 | 6.00 ± 2.65 | 4.14 ± 3.02 | 5.391 | 0.002 | 17.488 | 0.000 | |
| Stiffness score | 4.57 ± 2.15 | 3.00 ± 0.82 | 2.14 ± 2.12 | 2.008 | 0.091 | 2.232 | 0.067 | |
| Function score | 32.43 ± 8.89 | 19.57 ± 7.30 | 12.29 ± 3.64 | 3.658 | 0.011 | 6.134 | 0.001 | |
| Arthroscopic debridement + HA | WOMAC score | 54.43 ± 14.55 | 24.86 ± 12.09 | 14.86 ± 5.58 | 4.975 | 0.003 | 7.254 | 0.000 |
| Pain score | 12.57 ± 4.50 | 4.43 ± 2.44 | 2.14 ± 0.70 | 5.943 | 0.001 | 6.177 | 0.001 | |
| Stiffness score | 4.57 ± 2.82 | 2.43 ± 1.62 | 0.86 ± 1.21 | 1.605 | 0.160 | 2.931 | 0.026 | |
| Function score | 37.29 ± 9.66 | 18.00 ± 8.87 | 11.86 ± 4.22 | 4.559 | 0.004 | 7.0029 | 0.000 | |
| Arthroscopic debridement + PRP | WOMAC score | 49.86 ± 7.22 | 19.71 ± 5.74 | 15.00 ± 8.45 | 7.827 | 0.000 | 8.105 | 0.000 |
| Pain score | 13.14 ± 2.34 | 4.14 ± 1.86 | 1.71 ± 0.95 | 7.937 | 0.000 | 12.060 | 0.000 | |
| Stiffness score | 5.43 ± 3.16 | 1.71 ± 1.38 | 0.86 ± 1.07 | 3.176 | 0.019 | 3.600 | 0.011 | |
| Function score | 31.29 ± 6.26 | 13.86 ± 4.10 | 12.43 ± 6.80 | 6.397 | 0.001 | 5.781 | 0.001 | |
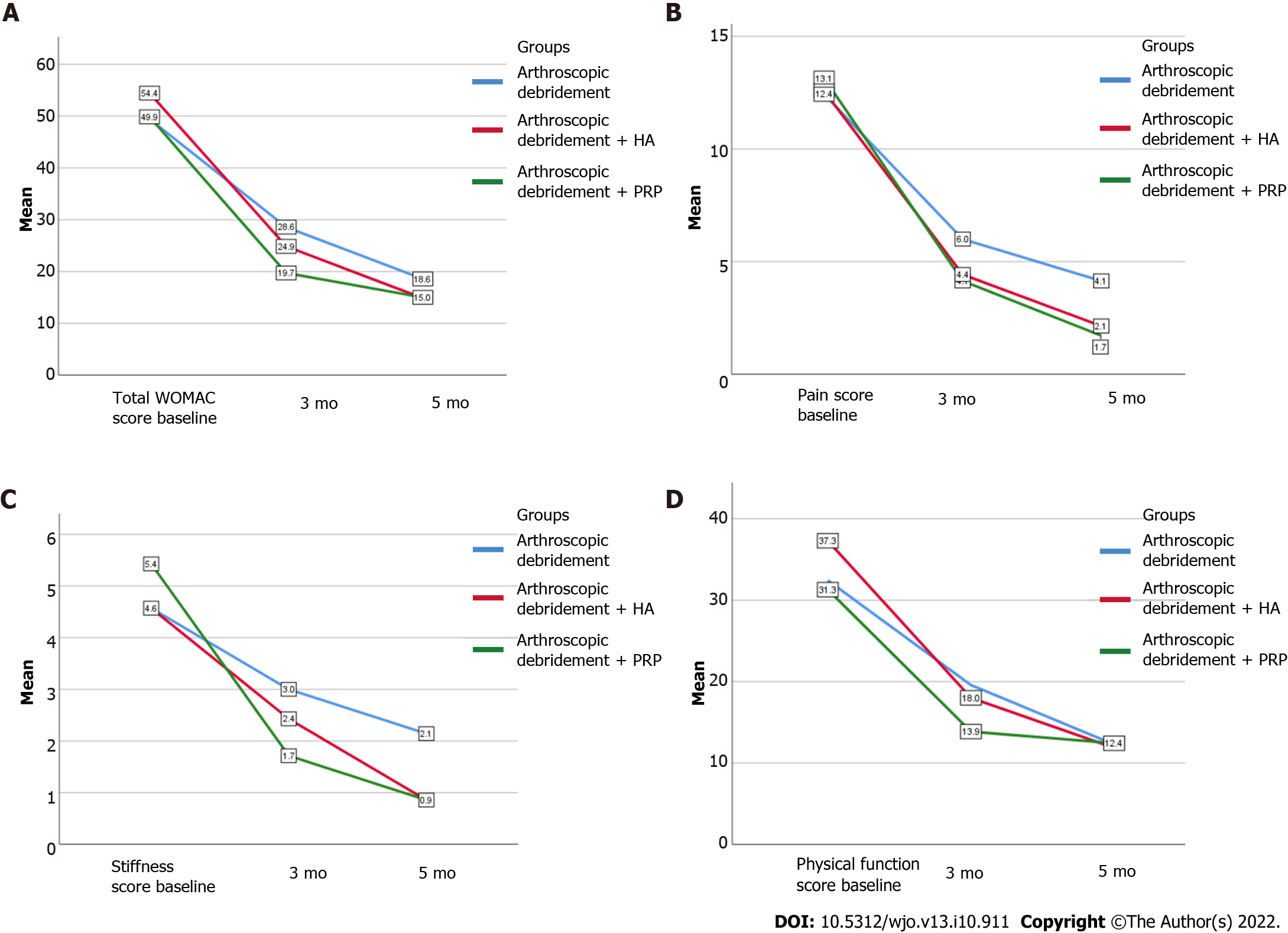
We also performed between-group comparisons for WOMAC score and sub-scores before treatment (at baseline) and after treatment (at the 3 mo and 5 mo follow-up); the findings are illustrated in Figure 1. At baseline, the mean WOMAC score was statistically similar among all groups (P = 0.65), with the arthroscopic debridement group having a mean ± SD score of 49.43 ± 10.33, the arthroscopic debridement with HA group having a mean ± SD score of 54.43 ± 14.55, and the arthroscopic debridement with PRP group having a mean ± SD score of 49.86 ± 7.22. No treatment was superior to another for WOMAC score at either the 3 mo follow-up or the 5 mo follow-up (P = 0.23 and 0.56 respectively); the same was seen for the WOMAC sub-scores (Table 3). Upon post hoc analysis using the LSD test, pain score at the 5 mo follow-up was found to be significantly lower in the arthroscopic debridement with PRP group compared to the arthroscopic debridement group (P = 0.03) (Table 3).
| Score | Period | Arthroscopic debridement | Arthroscopic debridement + HA | Arthroscopic debridement + PRP | ANOVA P value | LSD post hoc test; P value | ||
| I vs II | I vs III | II vs III | ||||||
| WOMAC score | Baseline | 49.43 ± 10.33 | 54.43 ± 14.55 | 49.86 ± 7.22 | 0.65 | 0.41 | 0.94 | 0.45 |
| 3 mo | 28.57 ± 9.09 | 24.86 ± 12.09 | 19.71 ± 5.74 | 0.23 | 0.47 | 0.09 | 0.32 | |
| 5 mo | 18.57 ± 7.12 | 14.86 ± 5.58 | 15.00 ± 8.45 | 0.56 | 0.34 | 0.36 | 0.97 | |
| Pain score | Baseline | 12.43 ± 2.76 | 12.57 ± 4.50 | 13.14 ± 2.34 | 0.91 | 0.94 | 0.69 | 0.75 |
| 3 mo | 6.00 ± 2.65 | 4.43 ± 2.44 | 4.14 ± 1.86 | 0.30 | 0.23 | 0.16 | 0.82 | |
| 5 mo | 4.14 ± 3.02 | 2.14 ± 0.70 | 1.71 ± 0.95 | 0.06 | 0.06 | 0.03 | 0.67 | |
| Stiffness score | Baseline | 4.57 ± 2.15 | 4.57 ± 2.82 | 5.43 ± 3.16 | 0.80 | 1.00 | 0.57 | 0.57 |
| 3 mo | 3.00 ± 0.82 | 2.43 ± 1.62 | 1.71 ± 1.38 | 0.22 | 0.43 | 0.08 | 0.32 | |
| 5 mo | 2.14 ± 2.12 | 0.86 ± 1.21 | 0.86 ± 1.07 | 0.22 | 0.14 | 0.14 | 1.00 | |
| Function score | Baseline | 32.43 ± 8.89 | 37.29 ± 9.66 | 31.29 ± 6.26 | 0.39 | 0.29 | 0.80 | 0.20 |
| 3 mo | 19.57 ± 7.30 | 18.00 ± 8.87 | 13.86 ± 4.10 | 0.32 | 0.68 | 0.15 | 0.29 | |
| 5 mo | 12.29 ± 3.64 | 11.86 ± 4.22 | 12.43 ± 6.80 | 0.98 | 0.83 | 0.96 | 0.84 | |
OA was once considered a degenerative or “wear-and-tear” joint disease. However, it is now known to be a result of multifactorial interplay among mechanical factors, joint integrity, local inflammation, cellular, and biochemical processes[19]. To the best of our knowledge, our retrospective cohort study presented herein is the first to compare WOMAC score and WOMAC sub-score parameters between arthroscopic debridement treatments, alone and with postsurgical adjunctive PRP or HA, in KL grade 3 and 4 knee OA patients.
Arthroscopic debridement in knee OA is carried out when conservative treatment does not give satisfactory improvement in clinical symptoms but when joint replacement is not yet indicated[17]. Arthroscopy removes cartilage degradation products, mechanical irritants, and inflammatory cells from the joints, thus reducing pain and improving knee symptoms in KL grade 3 and 4 knee OA patients[20,21]. According to Kirkley et al[20], arthroscopy is able to delay total knee replacement in KL grade 3 knee OA patients aged ≥ 55 years. Steadman et al[22] further pinpointed that it was able to delay total knee replacement for 6.8 years. Despite the beneficial outcome, the use of arthroscopy in knee OA has remained controversial, with some studies reporting no significant difference being achieved through placebo arthroscopy, physical therapy, or medication[20,23]. However, adjunctive treatment with intraarticular HA or PRP injection after arthroscopic debridement has been expected to give better outcome than arthroscopic debridement alone.
Application of exogenous HA increases lubrication and reduces friction at the joint surface, thereby preventing chondrocyte degradation[13]. It also stimulates endogenous HA production[12] and produces anti-inflammatory effects by inhibiting tumor necrosis factor-alpha, interleukin (IL)-1 beta, and IL-8 expression[13]. The analgetic effects of HA treatment occur by its prompting a decrease in stress-activated ion channel sensitivity[12].
PRP is a small amount of plasma with concentrated platelets, giving it appreciable therapeutic anti-inflammatory, analgetic, and tissue regeneration properties. The anti-inflammatory effects occur through inhibition of the nuclear factor-kappa B (NF-κB) pathway and matrix metalloproteinases (MMPs)[24-27]. Upon application to the human system, it releases protease-activated receptor 4 peptide and anabolic chondral factors to provide analgetic effects[27,28]. PRP therapy also works in cartilage by releasing growth factors (specifically, platelet-derived growth factor and vascular endothelial growth factor, among various other growth factors), which are able to increase endogenous HA synthesis, re-epithelization, and tissue repair[29-32].
Our study showed significant reductions in WOMAC score and the sub-scores of pain and function for patients in the arthroscopic debridement group at their 3 mo and 5 mo follow-ups. These findings are in line with those from a study by Su et al[9], who showed that patients with KL grade 3 and 4 knee OA had significantly reduced WOMAC score at 1 year and 2 years after arthroscopic debridement, compared to conservative treatment. In another study, Bohnsack et al[21] performed arthroscopy in KL grade 3 and 4 knee OA patients and showed that Lysholm score (an 8-item knee scoring scale) was significantly improved, resulting in the improved ability to perform daily activities. In contrast, a study from Kirkley et al[20] showed that patients with KL grade 2-4 knee OA who underwent arthroscopic debridement and lavage experienced no significant improvement in WOMAC and SF-36 scores, compared to patients who received conservative treatment. Similarly, another study by Moseley et al[23] that compared arthroscopic debridement and placebo surgery (skin incision only) in knee OA patients yielded no significant difference in the groups’ SF-36 and pain scale scores. Our study also showed that stiffness score did not significantly decrease in the arthroscopic debridement group. This could be due to the concept that application of the irrigation solution during arthroscopic debridement was not only meant to remove detritus but also synovial fluid and the HA-layer covering the cartilage; in this way, the shock absorbent layer and lubricating function would be affected[17].
We expected adjunctive treatment with HA intraarticular injection after arthroscopic debridement to overcome the limitation described directly above. And, indeed this was the case; our HA-treated arthroscopic debridement patients experienced significant improvement not only in WOMAC score, pain score, and function score at the 3 mo and 5 mo follow-ups but also in the stiffness score at the 5 mo follow-up. Similar improvements were shown in a study by Hempfling[17], which had compared knee arthroscopy with and without postprocedure HA injection. In that study, at the 12 mo follow-up, arthroscopy with HA was superior in clinical global impression, improved restricted ability to walk 100 m, pain on walking, and night pain. Atay et al[33] evaluated HA injections after arthroscopic debridement surgery in KL grade 2-3 knee OA and at 12 mo follow-up; there was a significant difference found in WOMAC score changes between the arthroscopy with HA group and the arthroscopy without HA group. Finally, a more recent meta-analysis by Shen et al[34] showed that HA after arthroscopy was able to reduce pain on motion, indicating that HA is significantly associated with increased physical function and WOMAC score.
Our search of the literature found no previous study on PRP injection following arthroscopic debridement in knee OA patients. In our study, this adjunctive treatment resulted in significantly lower WOMAC score and all WOMAC sub-scores at 3 mo and 5 mo follow-ups compared to baseline. Raeissadat et al[35] had evaluated WOMAC score in knee OA patients who received PRP injection; at the 6 mo follow-up, they found a significant improvement in WOMAC score and SF-36, compared to baseline. Another study by Patel et al[11] compared WOMAC score in knee OA patients who received one PRP injection, two PRP injections, or normal saline injection; a significant improvement in all WOMAC parameters occurred within 2 wk to 3 wk and lasted for 6 mo, whereas in the normal saline group, the WOMAC score worsened.
In our study, we compared WOMAC score and sub-scores between three treatment groups and there was no superiority between the groups. A pilot study by Trueba Vasavilbaso et al[16] comparing arthroscopic debridement, arthroscopic debridement with HA and arthroscopic debridement with PRP has shown that even though WOMAC score was significantly decreased at the 3 mo follow-up (vs baseline scores) in all groups, there was no significant difference in WOMAC score among them. A significant difference in WOMAC score was found at the 12 mo and 18 mo follow-ups, particularly between the group treated by arthroscopy alone and the group treated with arthroscopy and three HA injections. It is important to note that our relatively short follow-up time may have contributed to the non-significant differences in WOMAC score among the groups.
Post hoc analysis in our study showed a significant difference between the arthroscopic debridement and arthroscopic debridement with PRP groups in pain score at the 5 mo follow-up. This significant difference could have been due to the ability of PRP to inhibit pathways contributing to joint pain via its anti-inflammatory properties through inhibition of the NF-κB pathway and MMPs, decreasing IL-6 production, and releasing IL-10 anti-inflammatory cytokines[24-26].
According to Rajpoot et al[36], KL grade is positively correlated with WOMAC score, but to the best of our knowledge there has been no study specifically comparing WOMAC score in KL grade 3 and 4. In our study, the number of patients with KL grade 3 knees OA was significantly higher than those with KL grade 4, but we found no statistically significant difference either in WOMAC score or WOMAC sub-scores at baseline.
Lesions in knee OA not only affect the cartilage but also other structures, including the meniscus. A meniscal tear can contribute to progression of knee OA by its negative effects on load distribution, shock absorption, and stability of the knee joint. Individuals with meniscal tear frequently present with knee OA, which contributes to symptoms of the former. Reportedly, among KL grade 2-4 knee OA patients, 63% have meniscal tear[37,38]. Forty-seven percent of the patients in our study had meniscal tear discovered during the surgery. Even though a meniscal tear can contribute to knee OA symptoms, the occurrence of such was comparable at baseline in our patients, thus we did not do further statistical analysis or adjustment.
The main limitation of this study was the small number of participants, as only 21 patients were enrolled. The short follow-up period precluded our ability to evaluate long-term outcomes of the three treatment groups. We suggest a prospective cohort and a longer follow-up period for future research and including imaging evaluation, such as with MRI.
Adjunctive PRP after arthroscopic debridement gave better improvement in pain symptom compared to arthroscopic debridement alone. However, neither treatment was superior regarding the ability to improve WOMAC score and other knee OA symptoms.
The current management for knee osteoarthritis (OA) is not able to stop disease progression, particularly in Kellgren-Lawrence (KL) grade 3 and 4 OA. Thus, alternative therapeutic options are needed to prevent the progression of joint damage in OA and delay the need for knee arthroplasty.
Alternative therapies for knee OA are needed that can prevent disease progression. Such treatment is expected to increase quality of life and prevent or delay the need for arthroplasty.
To investigate whether adjunctive treatment with platelet-rich plasma (PRP) and hyaluronic acid (HA) after arthroscopic debridement provides better outcomes then arthroscopic debridement alone.
This was a retrospective cohort study using medical record data. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score and its sub-scores was used as the outcome parameter. The data were analyzed using the paired t-test, one-way analysis of variance, and post hoc least significant difference test.
Adjunctive PRP or HA after arthroscopic debridement was not superior to arthroscopic debridement alone in improving knee OA symptoms. However, adjunctive PRP resulted in improvement of pain symptoms. A longer evaluation period is needed to assess the long-term outcome.
Adjunctive PRP or HA after arthroscopic debridement was not superior to arthroscopic debridement alone in improving knee OA symptoms. Adjunctive PRP after arthroscopic debridement was more beneficial in reducing pain.
The results of this study are expected to provide clinicians with an alternative treatment for KL grade 3 and 4 knee OA. Future research with a prospective cohort and longer follow-up period is needed.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Ikatan Dokter Indonesia, No. 119318.
Specialty type: Orthopedics
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Mahmoud MZ, Saudi Arabia; Xu T, China; Yan ZQ, China S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Mobasheri A, Batt M. An update on the pathophysiology of osteoarthritis. Ann Phys Rehabil Med. 2016;59:333-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 261] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 2. | Chen D, Shen J, Zhao W, Wang T, Han L, Hamilton JL, Im HJ. Osteoarthritis: toward a comprehensive understanding of pathological mechanism. Bone Res. 2017;5:16044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 635] [Cited by in RCA: 783] [Article Influence: 97.9] [Reference Citation Analysis (0)] |
| 3. | Li D, Li S, Chen Q, Xie X. The Prevalence of Symptomatic Knee Osteoarthritis in Relation to Age, Sex, Area, Region, and Body Mass Index in China: A Systematic Review and Meta-Analysis. Front Med (Lausanne). 2020;7:304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 4. | Arief A, Budu, Usman MA, Sakti M, Lubis AMT, Bukhari A. Treatment of grade III knee osteoarthritis with bone marrow stimulation and intraarticular injection of triamcinolone and hyaluronic acid combination; three case report and literature review. Int J Surg Case Rep. 2022;95:107177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Hawker GA, Guan J, Croxford R, Coyte PC, Glazier RH, Harvey BJ, Wright JG, Williams JI, Badley EM. A prospective population-based study of the predictors of undergoing total joint arthroplasty. Arthritis Rheum. 2006;54:3212-3220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 169] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 6. | Knop E, Paula LE, Fuller R. Platelet-rich plasma for osteoarthritis treatment. Rev Bras Reumatol Engl Ed. 2016;56:152-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Moussa M, Lajeunesse D, Hilal G, El Atat O, Haykal G, Serhal R, Chalhoub A, Khalil C, Alaaeddine N. Platelet rich plasma (PRP) induces chondroprotection via increasing autophagy, anti-inflammatory markers, and decreasing apoptosis in human osteoarthritic cartilage. Exp Cell Res. 2017;352:146-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 211] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 8. | Li Z, Long H, Liu Q, Lin J. Willingness to Have Total Knee Arthroplasty in Rural Areas of Northern China. Orthop Surg. 2022;14:587-594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Su X, Li C, Liao W, Liu J, Zhang H, Li J, Li Z. Comparison of Arthroscopic and Conservative Treatments for Knee Osteoarthritis: A 5-Year Retrospective Comparative Study. Arthroscopy. 2018;34:652-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Akan Ö, Sarıkaya NÖ, Koçyiğit H. Efficacy of platelet-rich plasma administration in patients with severe knee osteoarthritis : can platelet-rich plasma administration delay arthroplasty in this patient population ? Int J Clin Exp Med. 2018;11(9):9473-9483. [DOI] [Full Text] |
| 11. | Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013;41:356-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 487] [Cited by in RCA: 497] [Article Influence: 41.4] [Reference Citation Analysis (1)] |
| 12. | Legré-Boyer V. Viscosupplementation: techniques, indications, results. Orthop Traumatol Surg Res. 2015;101:S101-S108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 13. | Altman RD, Manjoo A, Fierlinger A, Niazi F, Nicholls M. The mechanism of action for hyaluronic acid treatment in the osteoarthritic knee: a systematic review. BMC Musculoskelet Disord. 2015;16:321. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 266] [Cited by in RCA: 291] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 14. | Zhang HF, Wang CG, Li H, Huang YT, Li ZJ. Intra-articular platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: a meta-analysis. Drug Des Devel Ther. 2018;12:445-453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 79] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 15. | Maheu E, Rannou F, Reginster JY. Efficacy and safety of hyaluronic acid in the management of osteoarthritis: Evidence from real-life setting trials and surveys. Semin Arthritis Rheum. 2016;45:S28-S33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 125] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 16. | Trueba Vasavilbaso C, Rosas Bello CD, Medina López E, Coronel Granado MP, Navarrete Álvarez JM, Trueba Davalillo CA, Gil Orbezo FI. Benefits of different postoperative treatments in patients undergoing knee arthroscopic debridement. Open Access Rheumatol. 2017;9:171-179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Hempfling H. Intra-articular hyaluronic acid after knee arthroscopy: a two-year study. Knee Surg Sports Traumatol Arthrosc. 2007;15:537-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | White DK, Master H. Patient-Reported Measures of Physical Function in Knee Osteoarthritis. Rheum Dis Clin North Am. 2016;42:239-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | Lespasio MJ, Piuzzi NS, Husni ME, Muschler GF, Guarino A, Mont MA. Knee Osteoarthritis: A Primer. Perm J. 2017;21:16-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 210] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 20. | Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, Feagan BG, Donner A, Griffin SH, D'Ascanio LM, Pope JE, Fowler PJ. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359:1097-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 503] [Cited by in RCA: 458] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 21. | Bohnsack M, Lipka W, Rühmann O, Peters G, Schmolke S, Wirth CJ. The value of knee arthroscopy in patients with severe radiological osteoarthritis. Arch Orthop Trauma Surg. 2002;122:451-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Steadman JR, Briggs KK, Matheny LM, Ellis HB. Ten-year survivorship after knee arthroscopy in patients with Kellgren-Lawrence grade 3 and grade 4 osteoarthritis of the knee. Arthroscopy. 2013;29:220-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Moseley JB, O'Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, Hollingsworth JC, Ashton CM, Wray NP. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1395] [Cited by in RCA: 1204] [Article Influence: 52.3] [Reference Citation Analysis (0)] |
| 24. | Fotouhi A, Maleki A, Dolati S, Aghebati-Maleki A, Aghebati-Maleki L. Platelet rich plasma, stromal vascular fraction and autologous conditioned serum in treatment of knee osteoarthritis. Biomed Pharmacother. 2018;104:652-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 25. | McCarrel TM, Mall NA, Lee AS, Cole BJ, Butty DC, Fortier LA. Considerations for the use of platelet-rich plasma in orthopedics. Sports Med. 2014;44:1025-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 26. | Xie X, Zhang C, Tuan RS. Biology of platelet-rich plasma and its clinical application in cartilage repair. Arthritis Res Ther. 2014;16:204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 193] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 27. | Gobbi A, Lad D, Karnatzikos G. The effects of repeated intra-articular PRP injections on clinical outcomes of early osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23:2170-2177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 90] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 28. | Chang KV, Hung CY, Aliwarga F, Wang TG, Han DS, Chen WS. Comparative effectiveness of platelet-rich plasma injections for treating knee joint cartilage degenerative pathology: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95:562-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 158] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 29. | Dhillon MS, Behera P, Patel S, Shetty V. Orthobiologics and platelet rich plasma. Indian J Orthop. 2014;48:1-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 30. | Jayabalan P, Hagerty S, Cortazzo MH. The use of platelet-rich plasma for the treatment of osteoarthritis. Phys Sportsmed. 2014;42:53-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 31. | Lana JF. Platelet Rich Plasma and Its Growth Factors: The State of the Art. In: Lana, J., Andrade Santana, M., Dias Belangero, W., Malheiros Luzo, A. Platelet-Rich Plasma - Lecture Notes in Bioengineering. Berlin, Heidelberg: Springer, 2014: 1-59. [DOI] [Full Text] |
| 32. | Laver L, Marom N, Dnyanesh L, Mei-Dan O, Espregueira-Mendes J, Gobbi A. PRP for Degenerative Cartilage Disease: A Systematic Review of Clinical Studies. Cartilage. 2017;8:341-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 79] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 33. | Atay T, Aslan A, Baydar ML, Ceylan B, Baykal B, Kirdemir V. [The efficacy of low- and high-molecular-weight hyaluronic acid applications after arthroscopic debridement in patients with osteoarthritis of the knee]. Acta Orthop Traumatol Turc. 2008;42:228-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 34. | Shen D, Chen M, Chen K, Wang T, Lu L, Yang X. Efficacy of hyaluronic acid after knee arthroscopy: A systematic review and meta-analysis. J Rehabil Med. 2018;50:860-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 35. | Raeissadat SA, Rayegani SM, Hassanabadi H, Fathi M, Ghorbani E, Babaee M, Azma K. Knee Osteoarthritis Injection Choices: Platelet- Rich Plasma (PRP) Versus Hyaluronic Acid (A one-year randomized clinical trial). Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 188] [Cited by in RCA: 206] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 36. | Rajpoot M, Peepra D, Pandey K, Varma H. Clinico-radiological correlation of osteoarthritis knee using Western Ontario and McMaster Universities score and Kellegren and Lawrance grading. Int J Res Med Sci. 2016;4:4873-4876. [DOI] [Full Text] |
| 37. | McHugh CG, Opare-Addo MB, Collins JE, Jones MH, Selzer F, Losina E, Katz JN. Treatment of the syndrome of knee pain and meniscal tear in middle-aged and older persons: A narrative review. Osteoarthr Cartil Open. 2022;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 38. | MacFarlane LA, Yang H, Collins JE, Guermazi A, Jones MH, Teeple E, Xu L, Losina E, Katz JN. Associations among meniscal damage, meniscal symptoms and knee pain severity. Osteoarthritis Cartilage. 2017;25:850-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |