Published online Jan 18, 2022. doi: 10.5312/wjo.v13.i1.58
Peer-review started: April 28, 2021
First decision: October 17, 2021
Revised: October 28, 2021
Accepted: December 25, 2021
Article in press: December 25, 2021
Published online: January 18, 2022
Processing time: 263 Days and 19.5 Hours
Bilateral one-stage total knee arthroplasty (BTKA) is now in greater use as an alternative option for patients with bilateral end-stage knee arthropathy. However, postoperative pain and disablement during convalescence from BTKA, and procedure-related complications have been concerning issues for patients and surgeons. Although some studies reported that BTKA in selected patients is as safe as the staged procedure, well-defined guidelines for patient screening, and perioperative care and monitoring to avoid procedure-related complications are still controversial.
To compare the perioperative outcomes including perioperative blood loss (PBL), cardiac biomarkers, pain intensity, functional recovery, and complications between unilateral total knee arthroplasty (UTKA) and BTKA performed with a similar perioperative protocol.
We conducted a retrospective study on consecutive patients undergoing UTKA and BTKA that had been performed by a single surgeon with identical perioperative protocols. The exclusion criteria of this study included patients with an American Society of Anesthesiologists score > 3, and known cardiopulmonary comorbidity or high-sensitivity Troponin-T (hs-TnT) > 14 ng/L. Outcome measures included visual analogue scale (VAS) score of postoperative pain, morphine consumption, range of knee motion, straight leg raise (SLR), length of stay (LOS), and serum hemoglobin (Hb) and hs-TnT monitored during hospitalization.
Of 210 UTKA and 137 BTKA patients, those in the BTKA group were younger and more predominately female. The PBL of the UTKA vs BTKA group was 646.45 ± 272.26 mL vs 1012.40 ± 391.95 mL (P < 0.01), and blood transfusion rates were 10.48% and 40.88% (P < 0.01), respectively. Preoperative Hb and body mass index were predictive factors for blood transfusion in BTKA, whereas preoperative Hb was only a determinant in UTKA patients. The BTKA group had significantly higher VAS scores than the UTKA group at 48, 72, and 96 h after surgery, and also had a significantly lower degree of SLR at 72 h. The BTKA group also had a significantly longer LOS than the UTKA group. Of the patients who had undergone the procedure, 5.71% of the UTKA patients and 12.41% of the BTKA patients (P = 0.04) had hs-TnT > 14 ng/L during the first 72 h postoperatively. However, there was no difference in other outcome measures and complications.
Following similar perioperative management, the blood transfusion rate in BTKA is 4-fold that required in UTKA. Also, BTKA is associated with higher pain intensity at 48 h postoperatively and prolonged LOS when compared to the UTKA. Hence, BTKA patients may require more extensive perioperative management for blood loss and pain, even if having no higher risk of complications than UTKA.
Core Tip: The safety of bilateral one-stage total knee arthroplasty (BTKA) is still debated because of greater blood loss, higher risk of cardiovascular events, increased postoperative pain, and longer disablement period than unilateral total knee arthroplasty (UTKA). After comparing consecutive patients underwent BTKA and UTKA with similar perioperative management, we found that the blood transfusion rate in the BTKA is 4-fold than UTKA. Moreover, BTKA is associated with significantly higher pain intensity at 48 h postoperatively and prolonged hospitalization. Although our study demonstrated that BTKA is a safe procedure in selected patients, extensive perioperative management for blood loss and pain is mandatory for BTKA patients.
- Citation: Laoruengthana A, Rattanaprichavej P, Samapath P, Chinwatanawongwan B, Chompoonutprapa P, Pongpirul K. Should we use similar perioperative protocols in patients undergoing unilateral and bilateral one-stage total knee arthroplasty? World J Orthop 2022; 13(1): 58-69
- URL: https://www.wjgnet.com/2218-5836/full/v13/i1/58.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i1.58
Total knee arthroplasty (TKA) is widely accepted as one of the most effective and safe surgical procedures for treating severe osteoarthritis (OA) of the knee. Currently, advances in anesthesia, surgical techniques, and perioperative care, including multimodal pain management and accelerated rehabilitation, have improved functional recovery and shortened the length of the hospital stay for patients undergoing unilateral total knee arthroplasty (UTKA)[1]. There have also been contemporary blood-conserving methods published that substantially decrease the rate of postoperative blood transfusions when kept below 10%[2-4].
Approximately 25% of patients undergoing UTKA have bilateral OA knees[5] and subsequently will undergo contralateral TKA within 1 year[6]. Thus, bilateral one-stage total knee arthroplasty (BTKA) is now in greater use as an alternative option for patients with bilateral OA knees because of the potential advantages that include single anesthesia, reduction in total hospitalization and rehabilitation time, as well as overall costs[7]. However, the safety of BTKA is still debated because of perioperative morbidity that is associated with greater blood loss and a higher risk of cardiovascular adverse events than UTKA[8,9]. Various blood-conserving strategies including regional anesthesia, tourniquet use and deflation after wound closure, femoral canal occlusion, and use of tranexamic acid (TXA) are commonly implemented in patients having BTKA with documented efficacy[10]. However, recently published studies revealed that blood loss after BTKA ranged between 874 and 1067 mL, and blood transfusion rate ranged between 24% and 44% even if TXA was administered[11-13].
The substantial blood loss related to BTKA may subsequently cause occult hypoperfusion of vital organs such as the heart and kidneys. Conversely, requirements for blood transfusions may also increase the risk of complications such as allergic reaction, cardiovascular volume overload, and subsequent heart failure or pulmonary edema[14,15]. The risk of myocardial infarction (MI) has been reported to significantly increase among the TKA group during the immediate postoperative phase when compared to the non-surgical group[16,17]. Taking data from the National Hospital Discharge database, 1.1% of patients were diagnosed with cardiac complications in the 90 d after TKA, and BTKA had a higher rate than UTKA (2.0% vs 1.7%)[18]. Therefore, these findings may emphasize the need for extensive perioperative care and monitoring to avoid such complications in BTKA.
Furthermore, significant pain after UTKA has been noted and inadequate pain control has been demonstrated to be associated with inferior functional outcomes at 2 years after TKA[19]. Thus, postoperative pain has been an issue frequently concerning patients as to whether the intensity of pain and disablement during convalescence from BTKA are worse than that following UTKA. Nevertheless, there has been limited evidence comparing postoperative pain and functional recovery after BTKA and UTKA, and the known results are still equivocal[20,21]. Therefore, the objective of the present study was to compare the perioperative outcomes including perioperative blood loss (PBL), cardiac biomarkers, pain intensity and functional recovery, and complications between patients undergoing UTKA and BTKA with a similar perioperative protocol. The authors hypothesized that patients undergoing BTKA may require additional perioperative care and monitoring to improve outcomes.
The study received institutional review board approval for retrospective analysis of data recorded prior to initiation and has been registered as TCTR20181220001. The authors’ criteria for BTKA were painful bilateral end-stage OA knees, and therefore the selection of BTKA or UTKA was based upon patient preference. Consecutive patients who had undergone UTKA and BTKA for primary OA, performed by a single surgeon between January 2016 and December 2019, were enrolled in the study. The exclusion criteria of this study were patients with a history of prior knee surgery or previous knee infection. Participants with an American Society of Anesthesiologists (ASA) score > 3, known cardiopulmonary comorbidity or high-sensitivity Troponin-T (hs-TnT) > 14 ng/L, CKD stage ≥ 3, or significant renal impairment (serum creatinine > 1.5 mg/dL) were also excluded.
All the UTKA and BTKA were performed by a single surgeon with identical pre-, peri-, and postoperative protocols. Regional anesthesia, prophylactic intravenous antibiotics (ATB), and tourniquet control at 250 mmHg were applied for all patients. A medial parapatellar approach was performed through an approximately 10 cm midline skin incision, the cruciate ligaments were excised, and conventional instruments were then used to prepare the proximal tibial and distal femoral bone cuts by using extramedullary and intramedullary reference guides, respectively. A bone plug was applied to occlude the opening hole of the distal femur after finishing all the bone cuts. Soft tissue balancing was performed to achieve appropriate flexion and extension gaps. The patella was selectively resurfaced. Before prosthesis implantation, local infiltration anesthesia (LIA) was induced by injecting Bupivacaine (0.5% Marcaine; AstraZeneca, Sweden), 30 mg of ketorolac tromethamine (ketorolac tromethamine 1 mL; SiuGuan, Taiwan), and sterile normal saline solution into the anterior and posterior compartment of the knee with the 2:1 ratio technique. All the patients received a fixed bearing, posterior stabilized prosthesis which was implanted with bone cement. A vacuum drain was then applied, and 15 mg/kg of topical tranexamic acid was poured into the knee joint before closure of the arthrotomy. The drain was clamped for 3 h and subsequently removed at 24 h after the surgery.
For postoperative management, intravenous patient-controlled analgesia morphine (100 mL solution containing 50 mg of morphine sulphate) was injected as an on-demand bolus of 1 mL with a 5 min lockout period, 30 mg of ketorolac was given intravenously every 8 h, and 500 mg of oral acetaminophen was administered three times a day. After 48 h, all the catheters were discarded, and 2 mg of morphine were injected every 8 h with an additional 2 mg of morphine used for a breakthrough pain throughout hospitalization. Also, oral medications including 250 mg of naproxen twice a day and 500 mg of acetaminophen three times a day were given. All patients were administered with low molecular weight heparin for the first 48 h and combined with oral warfarin for 10 d. Rehabilitation including active ankle pump was started after the surgery, and a continuous passive motion device was utilized on the day after surgery. Every patient was encouraged to attempt early ambulation with gait aids as able to be tolerated.
Data collected for analysis were patient demography, visual analogue scale (VAS) scores of postoperative pain, morphine consumption, range of knee motion (ROM), straight leg raise (SLR), length of stay (LOS), and laboratory evaluation comprising serum hemoglobin (Hb), blood transfusion rate, creatine phosphokinase (CPK), and hs-TnT preoperatively and at 24, 48, and 72 h after the surgery.
The patient's total blood volume (TBV) was calculated by the equation of Nadler et al[22]. The difference between preoperative and lowest postoperative Hb was applied with the Hb balance method to determine PBL[2].
Males: TBV (mL) = [0.0003669 × height3 (cm)] + [32.19 × body weight (kg)] + 604
Females: TBV (mL) = [0.0003561 × height3 (cm)] + [33.08 × body weight (kg)] + 183
PBL (mL) = TBV (mL) × (Hbi – Hbe)/Hbi + sum of blood products transfused (mL), where Hbi (g/dL) is the preoperative Hb, and Hbe (g/dL) is the postoperative Hb.
Serum Hb level that drops below 9.0 g/dL is indicated for blood transfusion for both the UTKA and BTKA at our institution. A hs-TnT level > 14 ng/L is considered as possible for MI in our laboratory system. Any complications and readmission rates at 90 d after the index surgery were recorded.
All demographic data and measured outcomes are summarized with descriptive statistics. Continuous data are presented as the mean and standard deviation, and Student’s t-test was used to compare between the UTKA and BTKA groups. Categorical data which are presented as counts and percentages were compared by using Chi-square or Fisher’s exact test. Repeated-measures analysis of variance was applied to compare the time-dependent variables including VAS, ROM, SLR, Hb, CPK, and hs-TnT between groups. The post hoc comparisons of all pairwise points in time were applied to account for multiple testing with Bonferroni adjustments. A multiple logistic regression analysis was performed to determine which of these variables, including age, gender, body mass index (BMI), ASA physical status classification, and preoperative Hb, were the predictive factors for allogeneic blood transfusion. The sample size of the UTKA and BTKA groups had 99.5% power to detect a difference of 200 mL in PBL, which could significantly impact on blood transfusion rate, with standard deviation (SD) of 400 mL, and 95.4% power to ascertain a difference of 1.0 for VAS with SD of 2.5, with type I error of 5%. Stata/MP 15.0 software (StataCorp LP, College Station, TX, United States) was used for all statistical analyses. Statistical significance was defined as P < 0.05.
There were 210 UTKA and 137 BTKA included for analysis. The demographic and perioperative characteristics are briefly summarized in Table 1. Patients in the BTKA group were younger and more predominately female, and had a longer total duration of operation (TDO).
| UTKA | BTKA | P value | |
| Age (yr) | 65.00 ± 7.48 | 63.10 ± 6.83 | 0.02a |
| Gender (female/male) | 178/32 | 129/8 | 0.01a |
| BMI (kg/m2) | 26.99 ± 3.49 | 26.54 ± 3.89 | 0.20 |
| ASA (1/2/3) | 4/134/72 | 5/101/31 | 0.05 |
| Preop. VAS pain score | 6.89 ± 2.33 | 6.77 ± 1.89 | 0.44 |
| Preop. ROM | 113.86 ± 13.55 | 111.16 ± 14.26 | 0.13 |
| Preop. Hb (g/dL) | 12.60 ± 1.19 | 12.44 ± 1.08 | 0.21 |
| Preop. CPK (u/L) | 125.05 ± 84.64 | 116.05 ± 65.12 | 0.41 |
| Preop. TnT (ng/dL) | 6.77 ± 3.04 | 6.46 ± 3.18 | 0.79 |
| TDO (min) | 62.21 ± 9.86 | 125.12 ± 16.30 | < 0.01a |
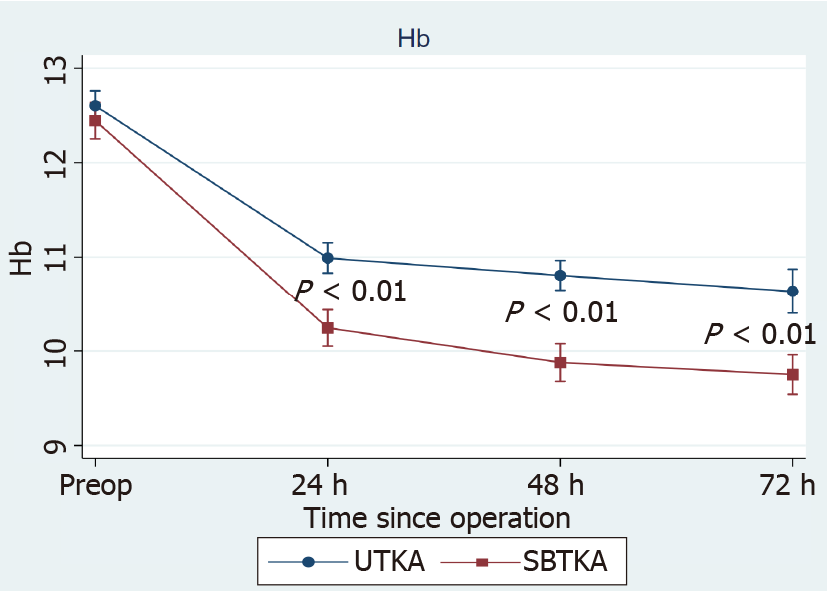
The postoperative Hb level of both groups gradually dropped and reached the lowest point at 72 h after the surgery. BTKA was associated with a significantly lower level of Hb than UTKA at 24, 48, and 72 h postoperatively (Figure 1). The PBL of the UTKA vs BTKA group was 646.45 ± 272.26 mL vs 1012.40 ± 391.95 mL (P < 0.01), respectively.
Blood transfusion rates in UTKA and BTKA were 10.48% (22/210) and 40.88% (56/137), (P < 0.01), respectively. For UTKA, 18 of 69 (26.09%) patients with preoperative anemia (defined as preoperative Hb < 12 g/dL in females and < 13 g/dL in males) received blood transfusion compared to 6 of 141 (4.26%) patients without anemia (P < 0.01). Twenty-eight of 43 (65.12%) patients with preoperative anemia in the BTKA group required a transfusion, whereas patients without anemia had a transfusion rate of approximately 1 in 4 (26/94, 27.67%; P < 0.01). The multivariate analysis demonstrated that preoperative Hb [odd ratio (OR): 0.33, 95% confidence interval (CI): 0.22-0.50, P < 0.01] and BMI (OR: 0.90, 95%CI: 0.81-0.99, P = 0.03) were predictive factors for blood transfusion in the BTKA group, whereas preoperative Hb (OR: 0.21, 95%CI: 0.12-0.37, P < 0.01) was only a determinant in the UTKA group when using similar perioperative blood management and cut-off values for transfusion.
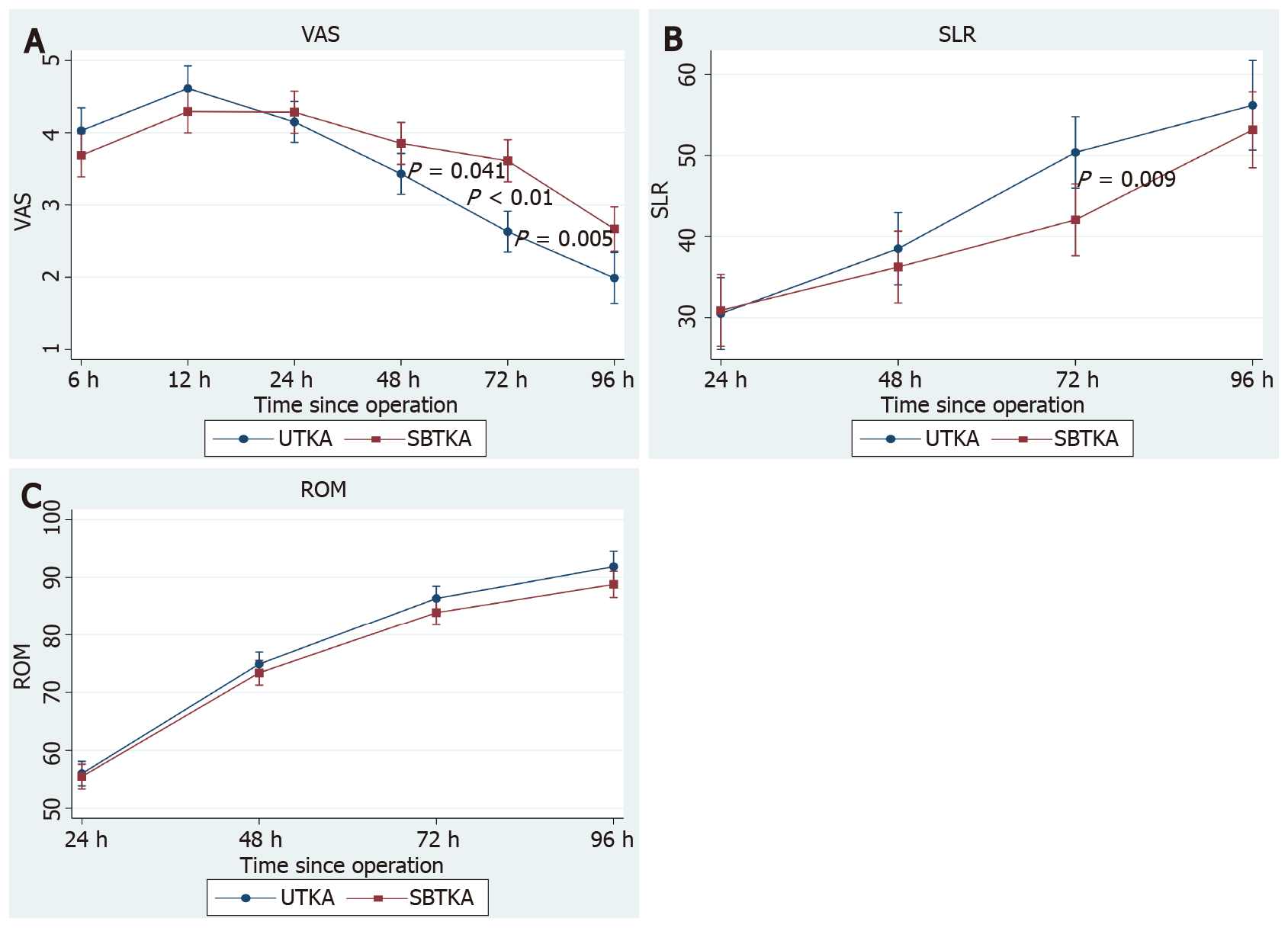
There was no difference between the UTKA and BTKA groups regarding VAS scores at 6, 12, and 24 h, but the BTKA group had significantly higher VAS scores than the UTKA group at 48, 72, and 96 h after surgery (Figure 2A). The BTKA group had a significantly lower degree of SLR than the UTKA group at 72 h; however, the ROM was comparable between groups throughout the study period (Figure 2B and C). Total morphine consumption in the UTKA vs BTKA group was 11.93 ± 9.20 vs 13.81 ± 10.81 (P = 0.16) at 24 h, and 16.78 ± 13.24 vs 19.51 ± 15.47 (P = 0.15) at 48 h postoperatively. The incidence of postoperative nausea and vomiting (PONV) during the first 24 h in the UTKA and BTKA groups was 38.79% (90/142) and 46.47% (112/129) (P = 0.09), respectively. The UTKA had an LOS of 4.01 ± 0.97 d, which was significantly shorter than that of the BTKA group (5.17 ± 1.32 d; P < 0.01).
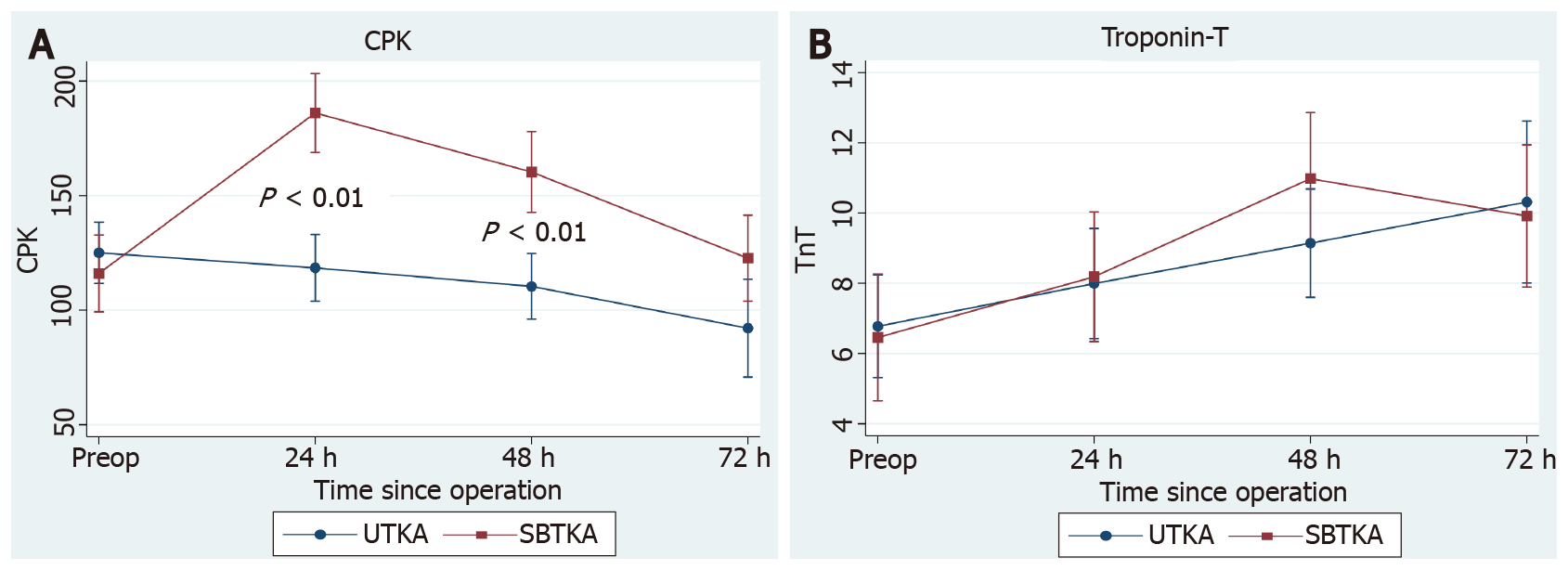
The BTKA group showed significantly higher CPK than the UTKA group at 24 h and 48 h after the surgery (Figure 3A). For the hs-TnT, it was gradually rising during 72 h after the UTKA and it was rising to a peak at 48 h after the BTKA, but the hs-TnT level was not significantly different between groups along the study period (Figure 3B). Nonetheless, there were 12 patients (5.71%) who had hs-TnT > 14 ng/L during the first 72 h after the UTKA compared to 17 patients (12.41%) following the BTKA (P = 0.04), but no patient presented cardiovascular symptoms and signs, or abnormal electrocardiogram indicating MI.
During the 90 d after the index surgery, there was one superficial infection, one cerebrovascular event, and two deep vein thromboses (DVT) in the UTKA group. For the BTKA group, one patient experienced peptic ulcer bleeding, one had DVT in the unilateral leg, and one had periprosthetic joint infection (PJI) which was successfully treated by two-stage revision TKA. Additionally, each group had one patient who required readmission due to severe pain at the surgical site.
Bilateral one-stage TKA potentially increases the rate of complications which are related to more soft tissue trauma, blood loss, postoperative pain, and cardiovascular adverse events, and therefore this is still a concerning issue for some patients and surgeons[8,9]. However, recent studies reported that BTKA in selected patients is as safe as the staged procedure, but proper patient screening, and perioperative care and monitoring to avoid complications and mortality are still controversial[23,24]. In the current study, BTKA was associated with significantly greater blood loss and higher allogeneic blood transfusion rates, as well as higher CPK levels, when compared to the UTKA group. The BTKA group tended to have higher hs-TnT levels at 48 h despite not reaching statistical significance. After 48 h, the BTKA group had a significantly higher VAS score than the UTKA group, and the SLR at 72 h after the BTKA was also worse than that after the UTKA. The LOS of the BTKA group was also significantly longer than that for the UTKA group. Nevertheless, the total morphine use, ROM, complications, and 90-d readmission rate were not different between the groups.
Generally, BTKA is known for its association with inevitably greater blood loss than UTKA. Advances in surgical techniques, use of TXA, and change in transfusion thresholds have substantially reduced postoperative transfusions following UTKA[3]. Recently, TXA is widely respected as an effective anti-fibrinolytic agent and has been demonstrated as having advantages when used in BTKA[25]. Although TXA is effective for reducing blood loss following BTKA, when it is applied either intravenously (IV) or intra-articularly (IA), the ideal regimen of TXA is still not well defined[13]. Arora et al[26] revealed no difference in average drop of Hb and blood transfusion rate between patients undergoing BTKA with IV-TXA or IA-TXA. Also, combined IA and IV TXA administration in BTKA did not show superior efficacy in blood loss reduction[27]. Therefore, the intraoperative IA-TXA use alone, in our study, should be sufficient to control blood loss, while avoiding potential complications related to systemic administration of TXA. However, our transfusion rate in BTKA is still quite high at 40.88%. Chalmers et al[28] retrospectively reviewed 475 patients who underwent BTKA and received double doses of TXA and contemporary blood management. They found that BTKA is still associated with a blood transfusion rate of approximately 1 in 5, and 50% of patients with a preoperative Hb < 12.5 required blood transfusion. Accordingly, we identified the preoperative Hb as a predictive factor for allogeneic transfusion in BTKA. Particularly, approximately 1 out of 3 patients in our study had preoperative anemia, and this finding may underline the opportunity for further improvement and for addressing this modifiable risk factor before BTKA. Delasotta et al[29] demonstrated that giving three preoperative doses of epoetin-α could significantly increase Hb levels and reduce blood transfusions in BTKA. Intravenous iron supplementation has also been reported for its efficacy in reducing the rate of transfusion in BTKA when combined with IA-TXA administration[30]. Other determinants including female gender, preoperative Hb level, operative time, and drain use have also been identified as risk factors for blood transfusion in BTKA[11,28]. In addition, soft tissue surface and intramedullary canal violation have been revealed as a possible significant source of bleeding[11,31-33]. Nevertheless, the efficacy of fibrin sealant applied to the bleeding soft tissue is unclear for blood loss reduction in BTKA[31], and also outcomes of emerging technologies such as computer-assisted or accelerometer-based navigation are still equivocal[13,34].
Significant pain after UTKA has been noted and this has been an issue frequently concerning patients as to whether the intensity of pain and disablement, during convalescence from BTKA, is worse than that of UTKA. Shetty et al[20] reported that BTKA had significantly higher VAS pain scores than UTKA on the first postoperative day. However, the VAS, ROM, and SLR were equal in both groups at the time of discharge. Other researchers found a 1-point higher VAS in the BTKA group during day 1, with 20% more narcotic use for the first 48 h, and patients in the BTKA group lagged behind the UTKA group in ambulatory milestones by approximately 36 h[21]. In the present study, we found that the UTKA and BTKA group had comparable pain intensity, morphine consumption, and knee function during the first 24 h after the surgery by using the same multimodal pain management. The neuroaxial anesthesia, LIA that was induced by injecting with bupivacaine and ketorolac tromethamine, and opioid-sparing analgesia with a multidrug regimen may be an explanation of the effective pain control during the first 24 h after UTKA and BTKA. Despite that, patients in the BTKA gradually developed higher pain scores afterwards and had worse SLR at 72 h. Higher postoperative CPK levels might reflect the certainty of more muscle injury in the BTKA, and so may indicate the need for intensive pain control extended beyond 48 h after the surgery. Intravenous administration of non-steroidal anti-inflammatory drugs (NSAIDs) is commonly used because of their efficacy in controlling post-TKA pain and may be administered up to 72 h after the surgery. Recently, Parecoxib, which is a selective cyclooxygenase-2 (COX-2) inhibitor, has been demonstrated to be effective in the reduction of post-TKA pain with the additional advantage of having less platelet inhibition and is consequently associated with less blood loss when compared to conventional NSAIDs[2]. Furthermore, intravenous corticosteroid and acetaminophen were also revealed as useful adjuncts for mitigating pain after TKA[35,36].
The safety of BTKA is still debated. Chen et al[24] recently demonstrated that patients aged > 80 years with an ASA score ≥ 3 who received careful screening for cardiopulmonary disorder and contemporary perioperative management for BTKA, had significantly decreased incidences of major and minor complications. Gromov et al[37] reported a 0% incidence of mortality in 284 selected patients without cardiopulmonary compromise, and they also found that ASA score ≥ 3 was a risk factor for 90-d readmission and prolonged LOS whereas higher BMI was a weak predictive factor for readmission. Lindberg-Larsen et al[23] conducted a study to compare outcomes after simultaneous and staged bilateral TKA in propensity-scores matched patients from nine centers. Of 232 matched patients in each group, perioperative complications and re-operation rates were significantly higher after simultaneous bilateral TKA. However, there was no difference in the rate of readmission within 30 d as well as the mortality between groups. In the present study, the hs-TnT level, which is a biomarker for cardiac muscle injury, was not different between UTKA and BTKA when patients had an ASA score ≤ 3 and preoperative hs-TnT within normal values. Although there were 12 and 17 patients after the UTKA and BTKA who had hs-TnT > 14 ng/L, no patients in either group presented symptoms and signs of cardiovascular complications. Hence, serial testing of cardiac biomarkers may be indicated only when patients have suspected clinical presentation[38]. Additionally, Hb evaluation seems to be unnecessary for non-anemic patients who undergo UTKA, due to the very low risk for blood transfusion. However, we suspect that Hb testing at 48 h after BTKA may be appropriate as a reflection of ongoing blood loss that is possibly linked to cardiac stress because the hs-TnT was rising to a peak at 48 h after BTKA when the Hb level was dropping. For other complications, the risk of PJI and DVT was not different between BTKA and UTKA when similar prophylaxis ATB and anticoagulants were applied. Nevertheless, further investigation may be needed to develop well-defined guidelines for perioperative monitoring in patients undergoing BTKA to decrease potential morbidity and mortality.
Nonetheless, we realized some limitations of the present study. First, this investigation is retrospective with some limitations accorded by study design, even if the selection of BTKA or UTKA as patient preference might be better accommodated with our real-life practice. Second, both study groups comprised predominantly female patients. However, previous studies found that gender has no effect on blood loss and functional recovery following TKA[12,39]. Third, variation of thresholds or cut-off values for blood transfusion among individual institutions may result in a different transfused rate. Indeed, the incidence of patients with preoperative anemia in our study seems to be higher than previously reported[3] and thereby may be a reason for higher transfusion rates than those reported in other studies[4,28]. Lastly, our sample size might not be sufficient to assess the exact risk of cardiovascular events and thromboembolism after UTKA and BTKA.
Following similar perioperative management, the blood transfusion rate in BTKA is 4-fold that required in UTKA. Also, BTKA is associated with higher pain intensity at 48 h postoperatively and prolonged LOS when compared to UTKA. Hence, patients undergoing BTKA may require more extensive perioperative management for blood loss and pain, even if they have no higher risk of complications and 90-d readmission than those receiving UTKA.
Bilateral one-stage total knee arthroplasty (BTKA) is a notable option for patients with bilateral end-stage knee arthropathy because of the potential advantages that include reduction in total hospitalization and rehabilitation time, as well as overall cost.
Despite previously acknowledged benefits, there is an issue frequently concerning patients as to whether the intensity of pain and disablement during convalescence from BTKA is worse than that following unilateral total knee arthroplasty (UTKA). Also, the risk of cardiovascular morbidity and other complications are subjects that lead some surgeons to refrain from BTKA. Thus, our objective was to identify what perioperative aspects of BTKA need to be improved and handled differently than for UTKA.
To compare the perioperative outcomes including perioperative blood loss (PBL), cardiac biomarkers, pain intensity, functional recovery, and complications between UTKA and BTKA by using an identical perioperative protocol.
All patients who had undergone UTKA and BTKA for primary osteoarthritis that had been performed by a single surgeon with identical perioperative protocols between January 2016 and December 2019 were retrospectively reviewed. The exclusion criteria of this study included patients with an American Society of Anesthesiologists score > 3, known cardiopulmonary comorbidity or high-sensitivity Troponin-T (hs-TnT) > 14 ng/L, CKD stage ≥ 3 or significant renal impairment (serum creatinine > 1.5 mg/dL), prior knee surgery, and previous knee infection.
Patients who received BTKA had significantly higher PBL with a 4-fold greater transfusion rate. As well, the patients in the BTKA group had higher visual analogue scale scores at 48, 72, and 96 h after the surgery and a higher postoperative creatine phosphokinase level. Consequently, a longer length of hospital stays than those who had UTKA was required. However, there was no difference regarding the postoperative hs-TnT level and complications.
Patients who undergo BTKA may require more extensive perioperative care for blood loss and pain than those patients who undergo UTKA.
Future prospective studies may be required to develop a particular perioperative protocol in patients undergoing BTKA to decrease potential morbidity and mortality.
We thank Mr. Roy I Morien of the Naresuan University Graduate School for his assistance in editing the English expression and grammar in this document. We also thank Passakorn Teekaweerakit, MD, Watcharapong Eiamjumras, MD, Thanawat Tantimethanon, MD, Panapol Varakornpipat, MD, and Kongpob Reosanguanwong, MD, for their technical assistance.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Xiao JL S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Fan JR
| 1. | Fransen BL, Hoozemans MJM, Argelo KDS, Keijser LCM, Burger BJ. Fast-track total knee arthroplasty improved clinical and functional outcome in the first 7 days after surgery: a randomized controlled pilot study with 5-year follow-up. Arch Orthop Trauma Surg. 2018;138:1305-1316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 2. | Laoruengthana A, Rattanaprichavej P, Reosanguanwong K, Chinwatanawongwan B, Chompoonutprapa P, Pongpirul K. A randomized controlled trial comparing the efficacies of ketorolac and parecoxib for early pain management after total knee arthroplasty. Knee. 2020;27:1708-1714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Warren JA, McLaughlin JP, Molloy RM, Higuera CA, Schaffer JL, Piuzzi NS. Blood Management in Total Knee Arthroplasty: A Nationwide Analysis from 2011 to 2018. J Knee Surg. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Kim TK, Chang CB, Kang YG, Seo ES, Lee JH, Yun JH, Lee SH. Clinical value of tranexamic acid in unilateral and simultaneous bilateral TKAs under a contemporary blood-saving protocol: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2014;22:1870-1878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Metcalfe AJ, Andersson ML, Goodfellow R, Thorstensson CA. Is knee osteoarthritis a symmetrical disease? BMC Musculoskelet Disord. 2012;13:153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 98] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 6. | Walmsley P, Murray A, Brenkel IJ. The practice of bilateral, simultaneous total knee replacement in Scotland over the last decade. Data from the Scottish Arthroplasty Project. Knee. 2006;13:102-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Odum SM, Troyer JL, Kelly MP, Dedini RD, Bozic KJ. A cost-utility analysis comparing the cost-effectiveness of simultaneous and staged bilateral total knee arthroplasty. J Bone Joint Surg Am. 2013;95:1441-1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 125] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 8. | Memtsoudis SG, Besculides MC, Reid S, Gaber-Baylis LK, González Della Valle A. Trends in bilateral total knee arthroplasties: 153,259 discharges between 1990 and 2004. Clin Orthop Relat Res. 2009;467:1568-1576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Bohm ER, Molodianovitsh K, Dragan A, Zhu N, Webster G, Masri B, Schemitsch E, Dunbar M. Outcomes of unilateral and bilateral total knee arthroplasty in 238,373 patients. Acta Orthop. 2016;87 Suppl 1:24-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 85] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 10. | Soranoglou V, Poultsides LA, Triantafyllopoulos GK, De Martino I, Memtsoudis SG, Sculco TP. Optimizing Intraoperative Blood Management for One-Stage Bilateral Total Knee Arthroplasty. HSS J. 2018;14:202-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Rattanaprichavej P, Laoruengthana A, Rasamimogkol S, Varakornpipat P, Reosanguanwong K, Pongpirul K. The Effect of Prosthesis Design on Blood Loss in Simultaneous Bilateral Total Knee Arthroplasty: Closed-Box vs Open-Box Prosthesis. Clin Orthop Surg. 2019;11:409-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Cao G, Chen G, Huang Q, Huang Z, Alexander PG, Lin H, Xu H, Zhou Z, Pei F. The efficacy and safety of tranexamic acid for reducing blood loss following simultaneous bilateral total knee arthroplasty: a multicenter retrospective study. BMC Musculoskelet Disord. 2019;20:325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Laoruengthana A, Rattanaprichavej P, Tantimethanon T, Eiamjumras W, Teekaweerakit P, Pongpirul K. Usefulness of an accelerometer-based navigation system in bilateral one-stage total knee arthroplasty. BMC Musculoskelet Disord. 2021;22:164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Friedman R, Homering M, Holberg G, Berkowitz SD. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. J Bone Joint Surg Am. 2014;96:272-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 177] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 15. | Silliman CC, Fung YL, Ball JB, Khan SY. Transfusion-related acute lung injury (TRALI): current concepts and misconceptions. Blood Rev. 2009;23:245-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 111] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 16. | Lu N, Misra D, Neogi T, Choi HK, Zhang Y. Total joint arthroplasty and the risk of myocardial infarction: a general population, propensity score-matched cohort study. Arthritis Rheumatol. 2015;67:2771-2779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 17. | Lalmohamed A, Vestergaard P, Klop C, Grove EL, de Boer A, Leufkens HG, van Staa TP, de Vries F. Timing of acute myocardial infarction in patients undergoing total hip or knee replacement: a nationwide cohort study. Arch Intern Med. 2012;172:1229-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Memtsoudis SG, González Della Valle A, Besculides MC, Gaber L, Sculco TP. In-hospital complications and mortality of unilateral, bilateral, and revision TKA: based on an estimate of 4,159,661 discharges. Clin Orthop Relat Res. 2008;466:2617-2627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 152] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 19. | Lakra A, Murtaugh T, Shah RP, Cooper HJ, Geller JA. Early Postoperative Pain Predicts 2-Year Functional Outcomes following Knee Arthroplasty. J Knee Surg. 2020;33:1132-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Shetty GM, Mullaji A, Bhayde S, Chandra Vadapalli R, Desai D. Simultaneous bilateral vs unilateral computer-assisted total knee arthroplasty: a prospective comparison of early postoperative pain and functional recovery. Knee. 2010;17:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Powell RS, Pulido P, Tuason MS, Colwell CW Jr, Ezzet KA. Bilateral vs unilateral total knee arthroplasty: a patient-based comparison of pain levels and recovery of ambulatory skills. J Arthroplasty. 2006;21:642-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51:224-232. [PubMed] |
| 23. | Lindberg-Larsen M, Pitter FT, Husted H, Kehlet H, Jørgensen CC; Lundbeck Foundation Centre for Fast-Track Hip and Knee Replacement Collaborative Group. Simultaneous vs staged bilateral total knee arthroplasty: a propensity-matched case-control study from nine fast-track centres. Arch Orthop Trauma Surg. 2019;139:709-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 24. | Chen SH, Chen JY, Wong TH, Buechel F Jr, Wu MH. Simultaneous Bilateral Total Knee Arthroplasty Becomes Safer after Institution of Optimal Perioperative Management: A Longitudinal Cohort Study. J Knee Surg. 2021;34:941-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Bagsby DT, Samujh CA, Vissing JL, Empson JA, Pomeroy DL, Malkani AL. Tranexamic Acid Decreases Incidence of Blood Transfusion in Simultaneous Bilateral Total Knee Arthroplasty. J Arthroplasty. 2015;30:2106-2109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Arora M, Singh S, Gupta V, Dongre A, Shetty V. Comparing the efficacy of intravenous or intra-articular tranexamic acid in reducing blood loss in simultaneous bilateral knee replacement surgery without the use of tourniquet. Eur J Orthop Surg Traumatol. 2018;28:1417-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 27. | Meshram P, Palanisamy JV, Seo JY, Lee JG, Kim TK. Combined Intravenous and Intraarticular Tranexamic Acid Does Not Offer Additional Benefit Compared with Intraarticular Use Alone in Bilateral TKA: A Randomized Controlled Trial. Clin Orthop Relat Res. 2020;478:45-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | Chalmers BP, Mishu M, Chiu YF, Cushner FD, Sculco PK, Boettner F, Westrich GH. Simultaneous Bilateral Primary Total Knee Arthroplasty With TXA and Restrictive Transfusion Protocols: Still a 1 in 5 Risk of Allogeneic Transfusion. J Arthroplasty. 2021;36:1318-1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Delasotta LA, Orozco F, Jafari SM, Blair JL, Ong A. Should We Use Preoperative Epoetin-α in the Mildly Anemic Patient Undergoing Simultaneous Total Knee Arthroplasty? Open Orthop J. 2013;7:47-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Suh DW, Han SB, Park JH, Cheong K, Kyung BS. Intravenous iron supplementation with intra-articular administration of tranexamic acid reduces the rate of allogeneic transfusions after simultaneous bilateral total knee arthroplasty. Blood Transfus. 2017;15:506-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 31. | Skovgaard C, Holm B, Troelsen A, Lunn TH, Gaarn-Larsen L, Kehlet H, Husted H. No effect of fibrin sealant on drain output or functional recovery following simultaneous bilateral total knee arthroplasty: a randomized, double-blind, placebo-controlled study. Acta Orthop. 2013;84:153-158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 32. | Aggarwal AK, Shashikanth VS, Marwaha N. Platelet-rich plasma prevents blood loss and pain and enhances early functional outcome after total knee arthroplasty: a prospective randomised controlled study. Int Orthop. 2014;38:387-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 33. | Kuo SJ, Wang FS, Wang CJ, Ko JY, Chen SH, Siu KK. Effects of Computer Navigation vs Conventional Total Knee Arthroplasty on Endothelial Damage Marker Levels: A Prospective Comparative Study. PLoS One. 2015;10:e0126663. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Jhurani A, Agarwal P, Aswal M, Jain P, Malepati S, Sharma R. Computer navigation has no beneficial effect on blood loss and transfusion in sequential bilateral total knee Arthroplasty. J Orthop Surg (Hong Kong). 2019;27:2309499019832440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Liang L, Cai Y, Li A, Ma C. The efficiency of intravenous acetaminophen for pain control following total knee and hip arthroplasty: A systematic review and meta-analysis. Medicine (Baltimore). 2017;96:e8586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 36. | Zhuo Y, Yu R, Wu C, Huang Y, Ye J, Zhang Y. The role of perioperative intravenous low-dose dexamethasone in rapid recovery after total knee arthroplasty: a meta-analysis. J Int Med Res. 2021;49:300060521998220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Gromov K, Troelsen A, Stahl Otte K, Ørsnes T, Husted H. Morbidity and mortality after bilateral simultaneous total knee arthroplasty in a fast-track setting. Acta Orthop. 2016;87:286-290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Reichlin T, Cullen L, Parsonage WA, Greenslade J, Twerenbold R, Moehring B, Wildi K, Mueller S, Zellweger C, Mosimann T, Rubini Gimenez M, Rentsch K, Osswald S, Müller C. Two-hour algorithm for triage toward rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Am J Med. 2015;128:369-79.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 112] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 39. | Alattas SA, Smith T, Bhatti M, Wilson-Nunn D, Donell S. Greater pre-operative anxiety, pain and poorer function predict a worse outcome of a total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25:3403-3410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 102] [Article Influence: 12.8] [Reference Citation Analysis (0)] |