Published online Jan 18, 2022. doi: 10.5312/wjo.v13.i1.112
Peer-review started: March 29, 2021
First decision: October 17, 2021
Revised: October 26, 2021
Accepted: December 21, 2021
Article in press: December 21, 2021
Published online: January 18, 2022
Processing time: 293 Days and 20.7 Hours
Four-corner fusion (4CF) is a motion sparing salvage procedure that is used to treat osteoarthritis secondary to advanced scapholunate collapse or longstanding scaphoid nonunion advanced collapse. Little is known about the long-term survivorship and outcomes of 4CF.
To report on clinical and functional long-term outcomes as well as conversion rates to total wrist fusion or arthroplasty.
The systematic review protocol was registered in the international prospective register of systematic reviews (PROSPERO) and followed the PRISMA guidelines. Original articles were screened using four different databases. Studies with a minimum Level IV of evidence that reported on long-term outcome after 4CF with a minimum follow-up of 5 years were included. Quality assessment was performed using the Methodological Index for Non-Randomized Studies criteria.
A total of 11 studies including 436 wrists with a mean follow-up of 11 ± 4 years (range: 6-18 years) was included. Quality assessment according to Methodological Index for Non-Randomized Studies criteria tool averaged 69% ± 11% (range: 50%-87%). Fusion rate could be extracted from 9/11 studies and averaged 91%. Patient-reported outcomes were extracted at last follow-up from 8 studies with an average visual analog scale of 1 ± 1 (range: 0-2) and across 9 studies with an average Disabilities of the Arm, Shoulder and Hand score of 21 ± 8 (range: 8-37). At last follow-up, the cumulative conversion rate to total wrist fusion averaged 6%. There were no conversions to total wrist arthroplasty.
The 4CF of the wrist is a reliable surgical technique, capable of achieving a good long-term patient satisfaction and survivorship with low rates of conversion to total wrist fusion.
Core Tip: Four-corner fusion is a motion sparing salvage procedure that is used to treat osteoarthritis secondary to scaphoid advanced collapse or longstanding scaphoid nonunion advanced collapse. Our systematic review evaluated long-term clinical and radiographic outcomes of the four-corner fusion and critically appraised the methodology of studies. The results showed that four-corner fusion is capable of achieving a good long-term patient satisfaction and survivorship with low rates of conversion to total wrist fusion. Recommendations for future research are provided.
- Citation: Andronic O, Nagy L, Burkhard MD, Casari FA, Karczewski D, Kriechling P, Schweizer A, Jud L. Long-term outcomes of the four-corner fusion of the wrist: A systematic review. World J Orthop 2022; 13(1): 112-121
- URL: https://www.wjgnet.com/2218-5836/full/v13/i1/112.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i1.112
Four-corner fusion (4CF) is a motion sparing salvage procedure that is used to treat osteoarthritis secondary to advanced scapholunate collapse or longstanding scaphoid nonunion advanced collapse. Proximal row carpectomy (PRC) and 4CF are the two mainly used surgical techniques in such cases[1]. The decision to choose one technique over the other is primarily based on the surgeon’s preference and experience, as long-term results are not clearly elucidated in the current literature so far[2]. 4CF seems to show longer survivorship, where PRC seems to provide better wrist motion[1,3-5]. Since the introduction of the 4CF by Watson and Ballet in 1984[6], various fixation techniques have been described, including Kirschner wires, headless compression screws, staples and plates[6-9]. However, using these techniques, different potential complications have been observed, in particular: nonunion, progressive osteoarthritis (OA) or hardware impingement/irritation[1,10-12].
The long-term survivorship and ultimate conversion rate of 4CF to wrist arthrodesis remains an unelucidated aspect. Although different studies are emerging that report on long-term outcomes of 4CF, it remains difficult to draw conclusions based on individual studies due to heterogeneity of outcome measures and surgical techniques. Hence, it was the aim of the current study to provide a systematic approach on evaluating evidence reporting on the long-term outcomes of 4CF with appropriate tools for critical appraisal.
A systematic computer-based database search was conducted using CENTRAL (Cochrane Central Register of Controlled Trials), MEDLINE (Pubmed), EMBASE and Web of Science Core Collection. A total of fifteen combinations for each database using the following key-words were used: “four corner,” “4 corner,” “midcarpal,” “scapholunate advanced collapse” and “scaphoid nonunion advanced collapse” with the terms “surgery,” “fusion” and “arthrodesis.” All published studies from January 1, 1978 until January 1, 2020 were included in the systematic search. First, a blinded and independent process of selection was carried out by two authors (D.K., P.K.) based on title and abstract. Next, a thorough analysis of eligible studies was performed by evaluating full texts. Any excluded study together with the reason of exclusion was noted and compared between readers. Studies reporting clinical or radiographic outcomes of 4CF for the treatment of degenerative wrist conditions were selected based on predefined eligibility criteria. The protocol of a parallel ongoing systematic review used by the same group regarding the 4CF has been published and registered in the international prospective register of systematic reviews (PROSPERO) under the registration number: CRD42020164301. Inclusion and exclusion criteria are empha
| Inclusion criteria | Exclusion criteria |
| Human studies in English or German language | Oral presentations, cadaveric or review articles, animal studies |
| Minimum Level IV case series studies using Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence | Language not in English or German |
| Four corner fusion surgery using any technique | Minimum follow-up less than 5 yr |
| A minimum follow-up of 5 yr | Inflammatory arthropathy as etiology |
| Clinical and radiographic data including patient-reported outcomes, grip/pinch strength, range of motion, fusion rates, revisions or complications have been reported | Insufficient outcome data reported |
Data collection included fusion rates, revision rates and conversion rates to total wrist arthrodesis. Wrist range of motion (ROM), including wrist flexion and extension, total flexion-extension arc as well as radial-ulnar deviation, was extracted. Grip strength was noted as percentage of the opposite hand. Patient-reported outcome measures were included as the Disabilities of the Arm, Shoulder and Hand questionnaire (DASH) and the visual analog scale (VAS) scores. Where available, data regarding incidence of radiolunate arthritis was included. The quality of all the studies was then assessed using the Methodological Index for Non-Randomized Studies criteria[13]. Methodological Index for Non-Randomized Studies criteria assess eight critical aspects of the study design for non-comparative clinical studies and an additional four aspects of study design for comparative clinical studies. Each item is given a score of zero if information is not reported, one if information is reported but inadequate, and two if information is reported and adequate. Therefore, the maximum possible score is 16 for non-comparative studies and 24 for comparative studies. Each score was then converted into a percentage to harmonize the scoring system.
The statistical analysis was performed using Review Manager (RevMan Cochrane) and Comprehensive Meta-Analysis Software. For quantification of methodological inconsistency and heterogeneity across studies, an I² test was performed, with a P value of P = 0.10. A level of more than 75% was considered as considerable. This has assessed whether observed differences in results are compatible with chance alone.
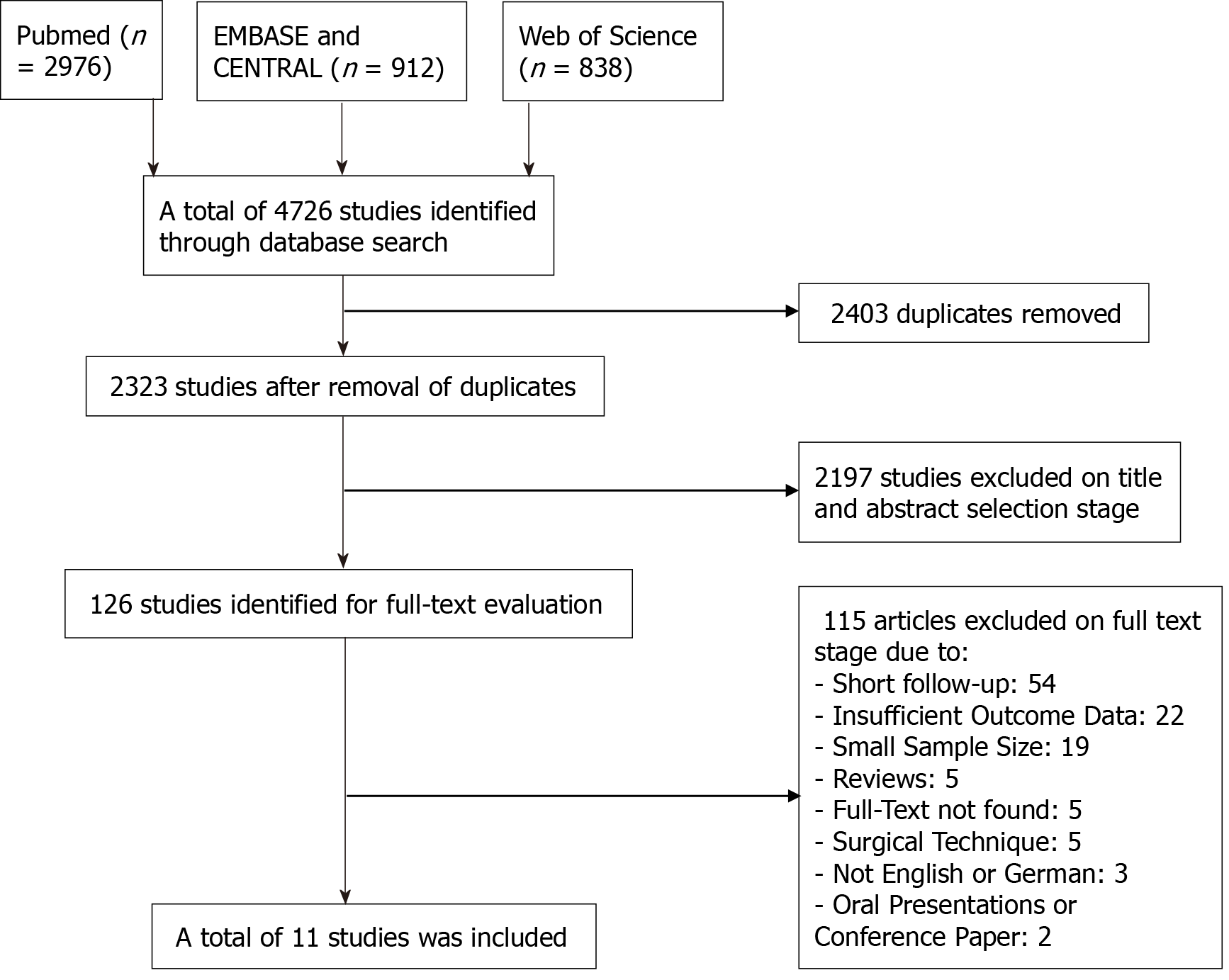
The initial database search yielded 4726 studies. After removal of duplicates, 2323 studies remained. Next, screening based on title and abstract was performed, and 126 studies remained for further assessment. These were then screened for eligibility against the inclusion and exclusion criteria based on abstract and full-text review. Finally, 11 studies could be included in the final analysis (Figure 1) with the reasons for exclusion separately emphasized in the flow-chart.
A quality assessment was performed in all included studies (Table 2). There were seven retrospective case series[3,5,14-18], three retrospective cohort studies[19-21] and one prospective cohort study[22]. The calculated average from scores according to the Methodological Index for Non-Randomized Studies criteria tool was 69.0% ± 11.1% (range: 50%-87%).
| Author | Year | Study design | Number of wrists | Indication | Mean age (yr) | Fixation Technique | VAS | DASH | MINORS (%) | ||
| Preop | Postop | Preop | Postop | ||||||||
| Cha SM | 2013 | Retrospective case series | 40 | SLAC | 47 | K-wires | 6.3 | 2.0 | 44 | 17 | 75 |
| Luegmair M | 2012 | Retrospective case series | 24 | SLAC, SNAC, SCAC | 53 | Plates | - | - | - | 19 | 75 |
| Bain GI | 2010 | Prospective cohort study | 31 | SLAC | 47 | Staples | 6.0 | 1.0 | - | - | 87 |
| Berkhout MJL | 2015 | Retrospective cohort study | 8 | SLAC, SNAC | 45 | K-wires | - | 0.3 | - | - | 62 |
| Kitzinger HB | 2003 | Retrospective case series | 37 | SLAC, SNAC | 46 | K-wires | 2.7 | 1.7 | - | 24 | 62 |
| Trail I | 2015 | Retrospective case series | 116 | SLAC, SNAC | 47 | K-wires, Plates, Staples, Screws | - | 1.9 | - | 37 | 62 |
| Neubrech F | 2012 | Retrospective case series | 60 | SLAC, SNAC, unclassified OA | 63 | K-Wires | - | 1.4 | - | 20 | 87 |
| Odella S | 2018 | Retrospective case series | 20 | SLAC, SNAC | 53 | Plates | - | 2.0 | - | 17 | 62 |
| Traverso P | 2017 | Retrospective case series | 15 | SLAC, SNAC | 49 | K-wires | - | - | - | 8 | 62 |
| Wagner ER | 2017 | Retrospective cohort study | 51 | Unclassified OA | 34 | Plates | - | - | - | 19 | 75 |
| Williams J | 2018 | Retrospective cohort study | 61 | SLAC, SNAC, perilunate OA | 52 | K-wires, Plates, Screws | - | 1.0 | - | 27 | 50 |
| Total/Averages | 463 | 49 | 1.4 | 21 | 69 | ||||||
| SD | ± 7 | ± 0.6 | ± 8 | ± 11 | |||||||
A total of 463 wrists was included for further analysis (Table 2). The mean age at time of surgery over all included studies was 49 ± 7 years (range: 34-63 years). The most frequent indications were degenerative wrist conditions such as scapholunate collapse (10/11 studies)[3,5,14-19,21,22] or scaphoid nonunion advanced collapse (8/11 studies)[3,5,15-19,21]. Other less frequent indications were scaphoid chondrocalcinosis advanced collapse[16], an unclassified OA[5,20] and perilunate OA[21]. The following fixation techniques were used: Kirschner wires[3,5,14,15,18,19,21], locking or non-locking plates[3,16,17,21], staples[3,22] and screws[3,21].
Preoperative VAS and DASH scores were only reported in a minority of studies (3 for VAS[14,15,22] and 1 for DASH[14]), which did not allow direct pre- to postoperative comparison (Table 2). Eight studies reported on postoperative VAS score and averaged 1 ± 1 (range: 0-2) at the latest follow-up. Postoperative data on DASH scores were pooled from 9 studies[3,5,14-18,20,21], which averaged 21 ± 8 (range: 8-37).
The mean follow-up was 11 ± 4 years (range: 6-18 years) (Table 3). Revision rates were reported in 8 studies[3,14,16-18,20-22] and had an overall average of 13% (range: 5%-34%). Nine studies (82%)[3,14,16-22] included data on the total number of nonunions, averaging 9% (range: 0%-24%) at last follow-up, resulting in a fusion rate of 91% (range: 76%-100%). Eight studies[3,14,16-18,20-22] reported on conversion rates to a total wrist fusion (TWF). A conversion to a TWF was needed on average in 6% of cases (range: 0%-20%). There were no cases reported of conversion to total wrist arthroplasty.
| Author | Number of wrists | Fixation technique | Nonunion (n) | Fusion (%) | Revisions (%) | Conversion to TWF (%) | Complications |
| Cha SM | 40 | K-wires | 0 | 100 | 2 (5) | 1 (3) | 1 x impingement |
| Luegmair M | 24 | Plates | 2 | 92 | 2 (8) | 0 | - |
| Bain GI | 31 | Staples | 3 | 90 | 5 (16) | 2 (7) | 1 x delayed union |
| Berkhout MJL | 8 | K-wires | 1 | 88 | - | - | 1 x CRPS, 1 x delayed union |
| Kitzinger HB | 37 | K-wires | - | - | - | - | - |
| Trail I | 116 | K-wires, plates, staples, screws | 28 | 76 | 14 (12) | 6 (5) | 3 x impingement |
| Neubrech F | 60 | K-wires | - | - | - | - | - |
| Odella S | 20 | Plates | 0 | 100 | 1 (5) | 0 | 1 x implant loosening |
| Traverso P | 15 | K-wires | 0 | 100 | 2 (13) | 1 (7) | - |
| Wagner ER | 51 | Plates | 6 | 88 | 15 (29) | 6 (12) | 1 x infection, 8 x impingement |
| Williams J | 61 | K-wires, plates, screws | 3 | 95 | 21 (34) | 12 (20) | 4 x impingement, 1 x ulnar impaction, 1 x infection |
| Totals/Averages | 463 | 43 (9%) | 91 ± 7 | 62 (13%) | 28 (6%) |
None of the included studies reported on preoperative signs of radiocarpal OA (Table 3). Five studies[5,14,15,18,20] reported on postoperative signs of radiocarpal OA of grade 2 or higher with an average incidence of 42% ± 26% (range: 5%-73%) at an average follow-up of 13 ± 3 years (range: 8-18 years). This was determined radiographically on conventional radiographs.
Preoperative grip strength was only available in 5 studies and preoperative data on ROM in only 4 studies (Table 4), which did not allow meaningful comparison to the postoperative results. The postoperative grip strength was noted in 8 studies[3,5,14-17,20,22] and averaged 68% ± 18% of the contralateral side (range: 30%-85%). Total postoperative flexion-extension arc, noted in 10 studies[3,5,14-20,22], was on average 66 ± 9 (range: 54-87). Postoperative ROM for radial-ulnar deviation, available in 9 studies[3,5,14-16,18-20,22], averaged 34 ± 6 (range: 26-49).
| Author | Grip strength (%) | ROM Flexion-extension | ROM radial-ulnar (%) | |||
| Preop | Postop | Preop | Postop | Preop | Postop | |
| Cha SM | 71 | 85 | 84 | 66 | 45 | 39 |
| Luegmair M | 38 | 70 | 57 | 64 | 24 | 30 |
| Bain GI | 27 | 30 | 78 | 57 | 35 | 30 |
| Berkhout MJL | - | - | - | 87 | - | 49 |
| Kitzinger HB | 69 | 80 | 68 | 62 | 35 | 34 |
| Trail I | - | 53 | - | 60 | - | 26 |
| Neubrech F | - | 85 | - | 63 | - | 30 |
| Odella S | - | 75 | - | 79 | - | - |
| Traverso P | - | - | - | 69 | - | 33 |
| Wagner ER | 60 | 65 | - | 54 | - | 32 |
| Williams J | - | - | - | - | - | - |
| Averages | 53 | 68 | 72 | 66 | 35 | 34 |
| SD | ± 17 | ± 18 | ± 10 | ± 10 | ± 8 | ± 6 |
The level of evidence of studies that were included lacked randomized controlled trials and did not allow performance of meta-analysis.
This is the first systematic review to investigate outcomes of the 4CF procedure at the long-term follow-up. The most important finding of the study is that 4CF can achieve good long-term patient satisfaction as well as good functional results. This can be observed out of the pooled data with low VAS values and positive DASH scores on last follow-up. An average fusion rate over 90% could be achieved, however with large variations across studies. Trail et al[3] reported a high nonunion percentage with only 76% fusion, further indicating the future need of 4CF for technique improvements and advancements in implant choice. Surprisingly, in the case of a successful 4CF, only an average of 6% of ultimate conversion to TWF was observed. This was in the context of lacking data on the preoperative state of the radiolunate joint, where a substantial amount could have been present at the time of surgery.
Nevertheless, the quality assessment provided important data on the evidence level of the studies, where relevant issues were elucidated. First, there were no double-blinded randomized controlled trials. Second, the single prospective cohort study, as declared by authors, had a questionable design whereas only the data collection might have been prospective[22]. The lack of preoperative data for almost all functional outcomes (ROM, grip strength) in the majority of studies precludes the quantification of the clinical gain from surgery[5,17-21]. Another important limitation was the fact that the outcomes were mostly reported in a cumulative fashion and not longitudinally over time. As such, a subgroup analysis of outcomes based on etiology (degenerative or post-traumatic) or the creation of a Kaplan-Meier survivorship curve to observe the time points of conversions could not be performed.
Although many treatments are available for scapholunate collapse and scaphoid nonunion advanced collapse wrist[23], the main debatable alternative to 4CF is the PRC[24,25]. A systematic review of long-term outcomes of PRC studies reported a reoperation rate of 14.3%[26].Of particular value is to mention that these failures were not only represented by conversions to TWF but also contained cases where revision arthroplasty was undertaken[4]. As such, the reoperation rates and conversion rates to TWF were not equal in this systematic review[26]. Generally, it was thought that PRC might yield better ROM[27]. However, this cannot be stated consistently, as recent systematic reviews and meta-analysis question the clinical relevance of differences that were observed between these techniques[2]. These relevant differences were limited to ROM, grip strength and patient-reported outcomes. In contrast, another systematic review reported a benefit in 4CF in terms of grip strength[28].
A further subject that was recently explored is the cost-effectiveness of PRC, where findings yielded either superior[29,30] or similar results[31] when compared to 4CF. Revision rates, especially during early follow-up, are higher in 4CF among some reports[21], highlighting impingement of hardware and nonunion as main reasons of revision[32]. This is attributed by authors to technical challenges and aspects, such as incomplete removal of the cartilage and subchondral bone, which is a key step of the procedure[11], quality and location of bone graft[33] as well as compression and carpal height achieved[34]. Optimal placement has yet to be defined to avoid revisions in 4CF due to impingement[32].
As such, in the context of continuous debate, an analysis of the long-term results, especially of the ultimate conversion rate to TWF or wrist arthroplasty, is crucial in determining the long-term benefit when choosing the surgical treatment option. The current systematic review is a substantial contribution to the understanding and knowledge of 4CF long-term outcomes as well as an analytical exploration of the limitations of studies (sources of heterogeneity and bias) that provide recommendations for future work.
The 4CF of the wrist is a reliable surgical technique, capable of achieving a good long-term patient satisfaction and survivorship with low rates of conversion to total wrist fusion.
Four-corner fusion (4CF) is a motion sparing salvage procedure that is used to treat osteoarthritis secondary to advanced collapse or longstanding scaphoid nonunion advanced collapse. Proximal row carpectomy and 4CF are the two mainly used surgical techniques in such cases. The decision to choose one technique over the other is primarily based on the surgeon’s preference and experience, as long-term results are not clearly elucidated in the current literature so far.
The long-term survivorship and ultimate conversion rate of 4CF to wrist arthrodesis remains poorly described. As various fixation techniques have been employed (Kirschner wires, headless compression screws, staples, plates), different potential complications have been observed, in particular, nonunion, progressive osteoarthritis or hardware impingement/irritation. There is no consensus on the best surgical implant and no synthesis on the long-term outcomes.
To provide a systematic approach on evaluating evidence reporting on the long-term outcomes of 4CF with appropriate tools for critical appraisal. We aimed to compare patient-reported outcomes, fusion rates, grip strength, range of motion and rates of development of radiocarpal osteoarthritis and revision to total wrist fusion.
A study protocol for the systematic search was registered prospectively in the international prospective register (PROSPERO) and performed according to the PRISMA guidelines. Data collection included fusion rates, revision rates and conversion rates to total wrist arthrodesis. Wrist range of motion, including wrist flexion and extension, total flexion-extension arc, as well as radial-ulnar deviation, was extracted. Grip strength was noted as percentage of the opposite hand. Patient-reported outcome measures were included as the Disabilities of the Arm, Shoulder, and Hand questionnaire and the visual analog scale scores (Table 4). Where available, data regarding incidence of radiolunate arthritis was included. The quality of all the studies were then assessed using the Methodological Index for Non-Randomized Studies criteria.
A total of 11 studies including 436 wrists with a mean follow-up of 11 ± 4 years (range: 6-18 years) was included. Quality assessment according to Methodological Index for Non-Randomized Studies criteria tool averaged 69% ± 11% (range: 50%-87%). Fusion rate could be extracted from 9/11 studies and averaged 91%. Patient-reported outcomes were extracted at last follow-up from 8 studies with an average visual analog score of 1 ± 1 (range: 0-2) and across 9 studies with an average Disabilities of the Arm, Shoulder, and Hand score of 21 ± 8 (range: 8-37). The postoperative grip strength was noted in 8 studies and averaged 68% ± 18% of the contralateral side. Total postoperative flexion-extension arc was on average 66 ± 9. At last follow-up, the cumulative conversion rate to total wrist fusion averaged 6%.
The 4CF of the wrist is a reliable surgical technique, capable of achieving a good long-term patient satisfaction and survivorship with low rates of conversion to total wrist fusion.
Future studies should define their study populations and protocols a priori before analysis. More in-depth details regarding patient selection (mostly preoperative data on range of motion, grip strength and radiolunate osteoarthritis) should be provided that would allow objective comparison.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Switzerland
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anand P S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
| 1. | Mulford JS, Ceulemans LJ, Nam D, Axelrod TS. Proximal row carpectomy vs four corner fusion for scapholunate (SLAC) or scaphoid nonunion advanced collapse (SNAC) wrists: A systematic review of outcomes. Hand Surg Eur Vol. 2009;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Amer KM, Thomson JE, Vosbikian MM, Ahmed I. Four-Corner Arthrodesis Versus Proximal Row Carpectomy for Scapholunate Advanced Collapse: A Systematic Literature Review and Meta-analysis. Ann Plast Surg. 2020;85:699-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Trail I, Murali R, Stanley J, Hayton M, Talwalkar S, Sreekumar R, Birch A. The Long-Term Outcome of Four-Corner Fusion. J Wrist Surg. 2015;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 4. | Ali MH, Rizzo M, Shin AY, Moran SL. Long-term outcomes of proximal row carpectomy: a minimum of 15-year follow-up. Hand (N Y). 2012;7:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Neubrech F, Mühldorfer-Fodor M, Pillukat T, Schoonhoven Jv, Prommersberger KJ. Long-term results after midcarpal arthrodesis. J Wrist Surg. 2012;1:123-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 6. | Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9:358-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 760] [Cited by in RCA: 674] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 7. | Krakauer JD, Bishop AT, Cooney WP. Surgical treatment of scapholunate advanced collapse. J Hand Surg Am. 1994;19:751-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 210] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Espinoza DP, Schertenleib P. Four-corner bone arthrodesis with dorsal rectangular plate: series and personal technique. J Hand Surg Eur Vol. 2009;34:609-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Ozyurekoglu T, Turker T. Results of a method of 4-corner arthrodesis using headless compression screws. J Hand Surg Am. 2012;37:486-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. J Hand Surg Am. 1995;20:965-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 189] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | Vance MC, Hernandez JD, Didonna ML, Stern PJ. Complications and outcome of four-corner arthrodesis: circular plate fixation versus traditional techniques. J Hand Surg Am. 2005;30:1122-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 125] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 12. | Bedford B, Yang SS. High fusion rates with circular plate fixation for four-corner arthrodesis of the wrist. Clin Orthop Relat Res. 2010;468:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3743] [Cited by in RCA: 5619] [Article Influence: 255.4] [Reference Citation Analysis (0)] |
| 14. | Cha SM, Shin HD, Kim KC. Clinical and radiological outcomes of scaphoidectomy and 4-corner fusion in scapholunate advanced collapse at 5 and 10 years. Ann Plast Surg. 2013;71:166-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Kitzinger HB, Löw S, Karle B, Lanz U, Krimmer H. Der posttraumatische karpale Kollaps-Längerfristiger Verlauf nach mediokarpaler Teilarthrodese. Handchirurgie Mikrochirurgie Plast Chir. 2003;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Luegmair M, Houvet P. Effectiveness of four-corner arthrodesis with use of a locked dorsal circular plate hand. Clin Orthop Relat Res. 2012;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Odella S, Querenghi AM, Locatelli FM, Dacatra U, Creta E, Tos P. Locking Dorsal Plate in Four-Bone Arthrodesis in SLAC and SNAC 3 Wrist. Joints. 2018;6:37-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 18. | Traverso P, Wong A, Wollstein R, Carlson L, Ashmead D, Watson HK. Ten-Year Minimum Follow-Up of 4-Corner Fusion for SLAC and SNAC Wrist. Hand (N Y). 2017;12:568-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Berkhout MJ, Bachour Y, Zheng KH, Mullender MG, Strackee SD, Ritt MJ. Four-Corner Arthrodesis Versus Proximal Row Carpectomy: A Retrospective Study With a Mean Follow-Up of 17 Years. J Hand Surg Am. 2015;40:1349-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Wagner ER, Werthel JD, Elhassan BT, Moran SL. Proximal Row Carpectomy and 4-Corner Arthrodesis in Patients Younger Than Age 45 Years. J Hand Surg Am. 2017;42:428-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 21. | Williams J, Weiner H, Tyser A. Long-Term Outcome and Secondary Operations after Proximal Row Carpectomy or Four-Corner Arthrodesis. J Wrist Surg. 2018;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Bain GI, Watts AC. The outcome of scaphoid excision and four-corner arthrodesis for advanced carpal collapse at a minimum of ten years. J Hand Surg Am. 2010;35:719-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 23. | Abdelaziz AM, Aldahshan W, Elsherief FAH, Wahd YESH, Soliman HAG, El Behairy HF, Ismail MA. Scaphoid excision with lunatocapitate fusion for the treatment of scaphoid nonunion with advanced collapsed wrist. Int Orthop. 2020;44:1153-1157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Streich NA, Martini AK, Daecke W. Proximal row carpectomy: an adequate procedure in carpal collapse. Int Orthop. 2008;32:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Zhang Y, Gillis JA, Moran SL. Management of scapholunate advanced collapse and scaphoid nonunion advanced collapse without proximal row carpectomy or four corner fusion. J Hand Surg Eur Vol. 2021;46:50-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Chim H, Moran SL. Long-term outcomes of proximal row carpectomy: a systematic review of the literature. J Wrist Surg. 2012;1:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 27. | Van Nuffel M, Vanhees M, Maeckelbergh L, Degreef I, De Smet L. Four-corner fusion versus proximal row carpectomy : a retrospective review with a minimal follow-up of 9 years. Acta Orthop Belg. 2020;86:146-150. [PubMed] |
| 28. | Saltzman BM, Frank JM, Slikker W, Fernandez JJ, Cohen MS, Wysocki RW. Clinical outcomes of proximal row carpectomy versus four-corner arthrodesis for post-traumatic wrist arthropathy: a systematic review. J Hand Surg Eur Vol. 2015;40:450-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 92] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 29. | Yoo M, Nelson RE, Illing DA, Martin BI, Tyser AR, Kazmers NH. Cost-Effectiveness Analysis Comparing Proximal Row Carpectomy and Four-Corner Arthrodesis. JB JS Open Access. 2020;5:e0080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Retrouvey H, Sander B, von Schroeder HP, Binhammer P, Baltzer HL. Cost-Effectiveness Analysis of Motion-Preserving Operations for Wrist Arthritis. Plast Reconstr Surg. 2020;146:588e-598e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Daar DA, Shah A, Mirrer JT, Thanik V, Hacquebord J. Proximal Row Carpectomy versus Four-Corner Arthrodesis for the Treatment of Scapholunate Advanced Collapse/Scaphoid Nonunion Advanced Collapse Wrist: A Cost-Utility Analysis. Plast Reconstr Surg. 2019;143:1432-1445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 32. | Shindle MK, Burton KJ, Weiland AJ, Domb BG, Wolfe SW. Complications of circular plate fixation for four-corner arthrodesis. J Hand Surg Eur Vol. 2007;32:50-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 33. | Athlani L, Sabau S, Pauchard N, Dap F, Dautel G. Four-corner arthrodesis with a dorsal locking plate: 4-9-year follow-up. J Hand Surg Eur Vol. 2020;45:673-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 34. | Laronde P, Christiaens N, Aumar A, Chantelot C, Fontaine C. Carpal height and postoperative strength after proximal row carpectomy or four-corner arthrodesis: Clinical, anatomical and biomechanical study. Hand Surg Rehabil. 2016;35:100-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |