Published online Sep 18, 2021. doi: 10.5312/wjo.v12.i9.672
Peer-review started: February 24, 2021
First decision: May 3, 2021
Revised: May 7, 2021
Accepted: August 6, 2021
Article in press: August 6, 2021
Published online: September 18, 2021
Processing time: 201 Days and 12.8 Hours
Telemedicine was originally created as a way to treat patients who were located in remote places far away from local health facilities or in areas with shortages of medical professionals. Telemedicine is still used today to address those problems, and is increasingly becoming a tool for convenient medical care. With the emergence of pandemics, telemedicine became almost a mandatory and valuable option for continuing to provide medical care in various specialties. As the threat of pandemic progress has continued for months and may continue for years, it is essential to validate existing tools to maintain clinical assessment and patient treatment to avoid negative consequences of the lack of medical follow-up. Therefore, the establishment of a virtual assessment technique that can be conducted effectively is of outmost importance as a way of adapting to the current situation. This study evaluated the role of telemedicine in the assessment of various orthopedic pathologies by means of a systematic virtual evaluation.
Core Tip: Telemedicine can be used to diagnose many orthopedic disorders and can be used for follow-up care after medical and surgical treatment. Its importance has increased dramatically with the emergence of epidemic diseases. However, an initial face-to-face assessment is recommended, especially in complicated cases where the diagnosis is uncertain. In this article, describe the role of telemedicine in the assessment of various orthopedic pathologies by systematic virtual evaluation.
- Citation: Emara KM, Diab RA, Amr M, Mahmoud SA, Nour M, Abdelsalam A, Elshobaky MA, Farhan M, Gemeah M, Emara AK. Virtual orthopedic assessment: Main principles and specific regions. World J Orthop 2021; 12(9): 672-684
- URL: https://www.wjgnet.com/2218-5836/full/v12/i9/672.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i9.672
Telemedicine uses technology for distant communication for health care purposes. With the emergence of epidemic diseases and need for social distance, telemedicine has become a valuable, almost a mandatory option for maintaining medical care provided in various medical specialties. Orthopedic surgery is one of the medical fields to which telemedicine can provide a good channel for continuous follow-up of patients, diagnosing, and managing many diseases during the awful worldwide situation[1].
Virtual assessment and management of orthopedic patients can bypass geographical and time boundaries, improve patient comfort, increase data transmission security, reduce costs, digitize healthcare systems, and facilitate the establishment of medical databases with potential research and audit benefits. On the other hand, its implementation is impeded by the fact that certain steps in the clinical examination cannot be performed without face-to-face interactions are vital for making the diagnosis[2].
Virtual orthopedic assessment depends on three items. The first is history taking, which has a very high impact in telemedicine to guide the physician throughout the entire assessment session. Examination is the next step of the assessment, and it must be adjusted to match the virtual setting of examining the patient without touch. After obtaining the data, physician orders the required laboratory or radiological investigations needed to reach the final diagnosis[3]. In this study, we evaluated the role of telemedicine in the assessment of various orthopedic pathologies through a systematic virtual assessment. Noted that in case of emergencies and inability to reach a definite diagnosis a consultation with an actual visit to a physician cannot be replaced.
The infrastructure and technical requirements needed for telemedicine assessment of orthopedic patients are easily available. Hardware devices include computers, cell phones, or tablets. Cameras and microphones are needed, and a wireless network connection, cable internet connection, or cellular network should be available. Many video platforms can be used during video conference consultations, such as Skype, Zoom, and Google Duo, etc.[4]. Specialized orthopedic software such as goniometer applications are useful for both initial consultations and in follow-up assessments of treatment efficacy. They can be also used for X-ray measurements (e.g., to determine the degree of scoliosis). Gait analysis software can be used as it is an important clinical tool to assess gait deviations[5,6].
For reaching an appropriate diagnosis of a patient problem by telemedicine, the surgeon should take a full patient history, with more time for history taking and patient inspection as he cannot assess the patient by touch, but only by visual inspection and by listening to the patient history to gather information that he can interpret before ordering specific investigations needed to confirm his suspected diagnosis. A full, accurate personal history, patient complaints, history of trauma if it occurred, medical, surgical, and family history, can raise the surgeon’s suspicion of a specific cause of the patient problem that can be confirmed by examination and investigation. The personal history, including age, sex, occupation, residence, special habits like smoking, sports, and marital status, is important, as many diseases or fracture types are more likely in specific age groups have a sex difference. For example Freiber's disease is common in female patients 13-18 years of age[7].
Pain is the commonest patient complaint. Surgeon should fully analyze the pain to determine if it is localized or generalized, and the type of pain, what increases the pain, and to what extent it affects the activity of patient. For example how many kilometers can the patient walk or if the pain awakes the patient from sleep. During sleep, muscle spasms, which are a protective mechanism, do not occur, and movement can cause severe pain. Generalized pain usually associated with degenerative changes, complex regional pain syndrome or nerve injury. Localized pain that can be pointed to with a finger may be caused by a fracture, ligament injury, or tendinitis[7,8].
Early morning stiffness or stiffness after rest complain is usually an indicator of arthritis, as rheumatoid arthritis or osteoarthritis. Another cause of stiffness is post traumatic fracture malunion. It should be determined whether swelling is generalized or localized. Generalized swelling has many causes such as rheumatoid, septic, or osteoarthritis, severe soft tissue injury, or systemic diseases affecting the heart, like heart failure. Localized swelling has many causes, like bone fracture or ligament injury. If there is history of trauma, the mode should be determined, as the specific mode of trauma causes specific problems[7,9].
Shoulder pain is a common reason for seeking medical advice. Localized anterolateral shoulder pain in the “Codman zone" associated with night pain is a clue of some degenerative shoulder pathology, either impingement or rotator cuff tear. Posterior shoulder pain usually occurs with scapular dyskinesia as well as cervical muscle spasm. Shoulder stiffness is a complaint usually associated with pain that may occur because of impingement, rotator cuff tear, arthritis, or frozen shoulder "adhesive capsulitis". Instability and recurrent shoulder dislocation complains are often seen in athletes and in young age groups[10,11].
Inspection should be done for swelling, muscle wasting, or scars of previous operations. Inspection from the front is done to see whether there is a prominent sternoclavicular joint (subluxation) or clavicle deformity (old fracture), prominent acromioclavicular joint (subluxation or osteoarthritis), or deltoid wasting (disuse or axillary nerve palsy). Assessment done from side and behind is done to see whether the scapulae is normally shaped and situated, or small and high, as in Sprengel’s shoulder or Klippel–Feil syndrome, or if there is winging of the scapula owing to paralysis of the serratus anterior[11].
An active range of motion (ROM) evaluation is done by instructing the patient to perform movements shown by physician, with assessment of obvious limitation if present and asking the patient which movement is painful, which most often is shoulder abduction. Ask the patient to perform external rotation with adduction and with abduction, if limited in comparison to other side it may indicate a frozen shoulder[10,11].
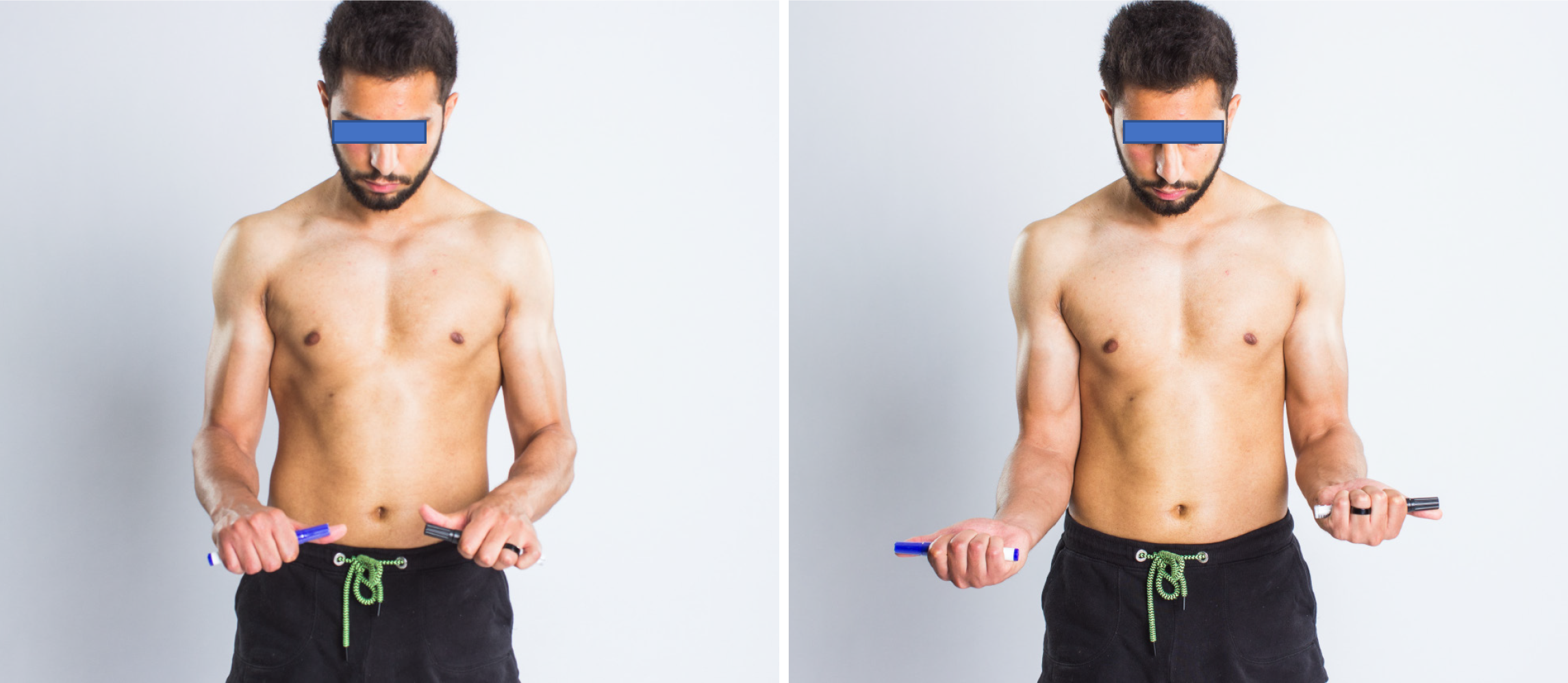
Special shoulder examination tests include an impingement assessment done by asking the patient to perform forward flexion of the shoulder with 90 degrees of elbow flexion and then shoulder internal rotation. Ask the patient whether it is painful or not and where exactly he feels the pain. If it is "mostly in the lateral and anterolateral shoulder region", then it indicates the presence of impingement. The resisted abduction test requires equipment, any item that weighs 2 kg, and is done by asking the patient to do a shoulder abduction while lifting the 2 kg object with internal rotation of the shoulder. The test simulates the empty can test for rotator cuff tear (Figure 1). Testing for slap lesion is done by resisted shoulder flexion with the forearm pronated and asking the patient resist the movement with his other hand over the forearm. The test is positive with a slap lesion and it simulates the speed test. An abduction external rotation test is performed by asking the patient to perform external rotation with abduction of the shoulder and ask if he/she feels afraid of dislocation. The test simulates the apprehension test for anterior shoulder instability. Scapular dyskinesia is tested by asking the patient to perform forward flexion of the shoulder while inspecting his back to follow scapular motion and monitor the symmetry of scapular motion during the movement. Scapular winging is tested by instructing the patient to lean with both hands against a wall. Watch the inferior angle of the scapula. Any tendency of winging of the scapula immediately becomes apparent[12].
A patient complaint of localized pain related to the lateral epicondyle is specific for tennis elbow, radial tunnel syndrome, or osteochondritis of the capitellum. Localized pain over the medial epicondyle is specific for golfer's elbow, cubital tunnel syndrome, and ulnar collateral ligament injury. Aching pain usually caused by arthritic changes. Pain with activity is usually caused by tendinosis or instability[13]. Virtual elbow assessment should include inspection of the elbow from all sides in flexion and extension, looking for any swelling, muscle wasting, scars of previous operations, and any deformity. The elbow should be inspected in extension with the arm by the side and the forearm supinated for determining carrying angle. It is increased (cubitus valgus) in cases of lateral condyle fracture nonunion and premature lateral epiphysis closure, and decreased (cubitus varus) in supracondylar humerus fracture[13].
Active ROM is tested by a flexion and extension test done with the patient’s shoulder abducted 90 degrees. Normal flexion is to 140 degrees and extension to −10 degrees. Pronation and supination ROM are tested after instructing the patient to place the elbow flexed 90 degrees by his side. Normal pronation is from 0 to 70 degrees and supination is from 0 to 85 degrees (Figure 2). Limited range is usually found in patients with old fractures and arthritis. Both sides should be compared[14,15].
Special tests, such as Thomsen's test, specific for tennis elbow is done by asking the patient to clench his fist, extend his elbow and dorsiflex his wrist against resistance. Patients with tennis elbow will experience pain over lateral epicondyle[7]. For Tinel's test, which is specific for ulnar nerve entrapment and neuropathy, the patient should be asked to flex his elbow to 20 degrees and a healthcare giver is asked to tap gently between the olecranon and medial epicondyle over the ulnar groove. The test is positive for ulnar neuropathy if the patient has a tingling sensation down the forearm until the ulnar part of hand. For a specific test of golfer's elbow, the patient is asked to flex his elbow and then supinate the forearm. A healthcare giver is asked to extend the elbow against resistance. If positive, the patient will have pain over the medial epicondyle. The chair pushup test is for assessment of posterolateral rotator instability in cases of injury to the lateral collateral ligament complex. It is done with the patient in a seated position with the hands grasping the arms of the chair. The elbows, in about 90° of flexion, are supinated and the arms abducted. The patient attempts to rise from the chair by pushing down. A positive result is pain as the elbow slowly extends while the patient rises[14,15].
Specific patients complaints are very important for making a specific diagnosis. Localized ulnar-side wrist pain may indicate conditions including a triangular fibrocartilage complex tear, or distal radioulnar joint instability/arthritis. Radial-side wrist pain suggests De Quervain’s tendinitis, scaphoid fractures, etc.[16]. Wrist drop suggests radial nerve injury, while partial claw hand suggests ulnar nerve involvement[16,17]. A painless, slowly growing swelling at the dorsum of the hand just distal to the lister tubercle is suggestive of ganglion. Complaints of clicking and locking suggest Trigger finger, especially in the presence of a nodule on the corresponding metacarpophalangeal (MP) joint[18].
Hand inspection should be from the shoulders to the hands from all sides, with comparison between both sides. We inspect the hand to detect any deformity of alignment, scars, swelling, color changes, callosities, and ulcerations. Deformities such as short stumpy fingers seen in achondroplasia, as swan neck deformity, mallet finger, Boutonniere deformity, Z deformity of the thumb, and Dupuytren's contracture deformities should be inspected. Muscle wasting should also be noted as it suggests a root, plexus, or nerve lesion. A wasted Theaner eminence is associated with median nerve injury, wasted hypotheanar and interossei with ulnar nerve injury, and wasted anatomical snuff box with radial nerve injury[19].
Active movement of the finger joints is tested individually. Each finger is flexed maximally, while other fingers are extended and clearly seen, and then extended maximally. The normal active ROM is 0 to 90 degrees for the metacarpophalangeal (MP) joint, 0-100° for the proximal interphalangeal (IP) joint, 0 to 80 degrees for the distal IP joint, −20 to 15 degrees for thumb carpometacarpal joint, −5 to 55 degrees for thumb MP joint, and −20 to 80 degrees for the thumb IP joint. Similar assessments of thumb adduction, abduction, and apposition, wrist flexion and extension, ulnar and radial deviation can be made. The patient abducts and adducts the fingers as possible, with thumb adduction, radial abduction, and apposition[17].
Neurological sensory assessment can be assessed by asking a care giver to touch specific sites with cotton while comparing both sides with the patient’s eyes closed. The sites are the tip of index finger (for median nerve injury), tip of little finger (for ulnar nerve injury), and the snuff box region (for radial nerve injury)[20,21]. Neurological motor assessments are done by asking the patient to make an “OK” sign by touching tip of thumb and the index finger to assess injury of the anterior interosseous nerve. With injury of the posterior interosseous nerve, the patient will have weak wrist extension with radial deviation. Loss of wrist extension is seen with radial nerve injury[20]. The ulnar nerve is assessed with Froment’s test by asking the patient to grasp a piece of paper in the first web space on both sides while a caregiver holds the other side. Failure to adduct the thumb, and flexing it instead, indicates a positive test, with ulnar nerve injury[22]. For assessment of carpel tunnel syndrome Phalen’s test (Figure 3) can be done by asking the patient to place the wrists in a maximal flexion position, which will reproduce the symptoms, if positive[23].
Hip pain is a common complaint of those seeking medical advice. Patients with hip problems also complain of limping, mechanical symptoms such as, clicking, snapping, catching, popping, and locking. The patient should be asked about a history of constitutional symptoms as fever, sweating, and nocturnal pain. The medical history should also address avascular necrosis of hip, usually seen in patients with systemic lupus and immune system disorders. Hip function can be objectively assessed with validated hip scores that can be assessed in the initial and in follow-up visits, especially after treatment. The Harris Scoring System and Western Ontario and McMaster Universities Arthritis Index hip scores are commonly used[3,10].
For inspection of the hip, undressing to underwear, if possible, is required to inspect the whole lower limb. Inspect from the front, sides, and back for skin scars, sinuses, discoloration, swellings, and muscle weakness or wasting (e.g., Trendelenburg test). Inspect for any deformities in the sagittal plane and in the coronal view. Observe the gait, positive or negative limb length discrepancy from the front, sides and behind. Try to assess stride length, its components, and possible associated stiffness, shortening, pain and gluteal insufficiency[10].
Active ROM can be performed via telemedicine. For flexion, ask the patient to lie supine then flex each hip one time as possible. For extension, ask the patient to lie supine at the edge of a couch, then ask him/her to lie down one limb a time. For abduction and adduction, the camera should be at a level high enough to have a top view. Ask the patient to lie supine and then move the thighs away from each other far as possible and then back to the other side, crossing over as far as possible. For internal and external rotation, ask the patient to sit on the edge of the couch, and then move the legs away from each other as far as possible and then back toward the other side, crossing over as far as possible[10].
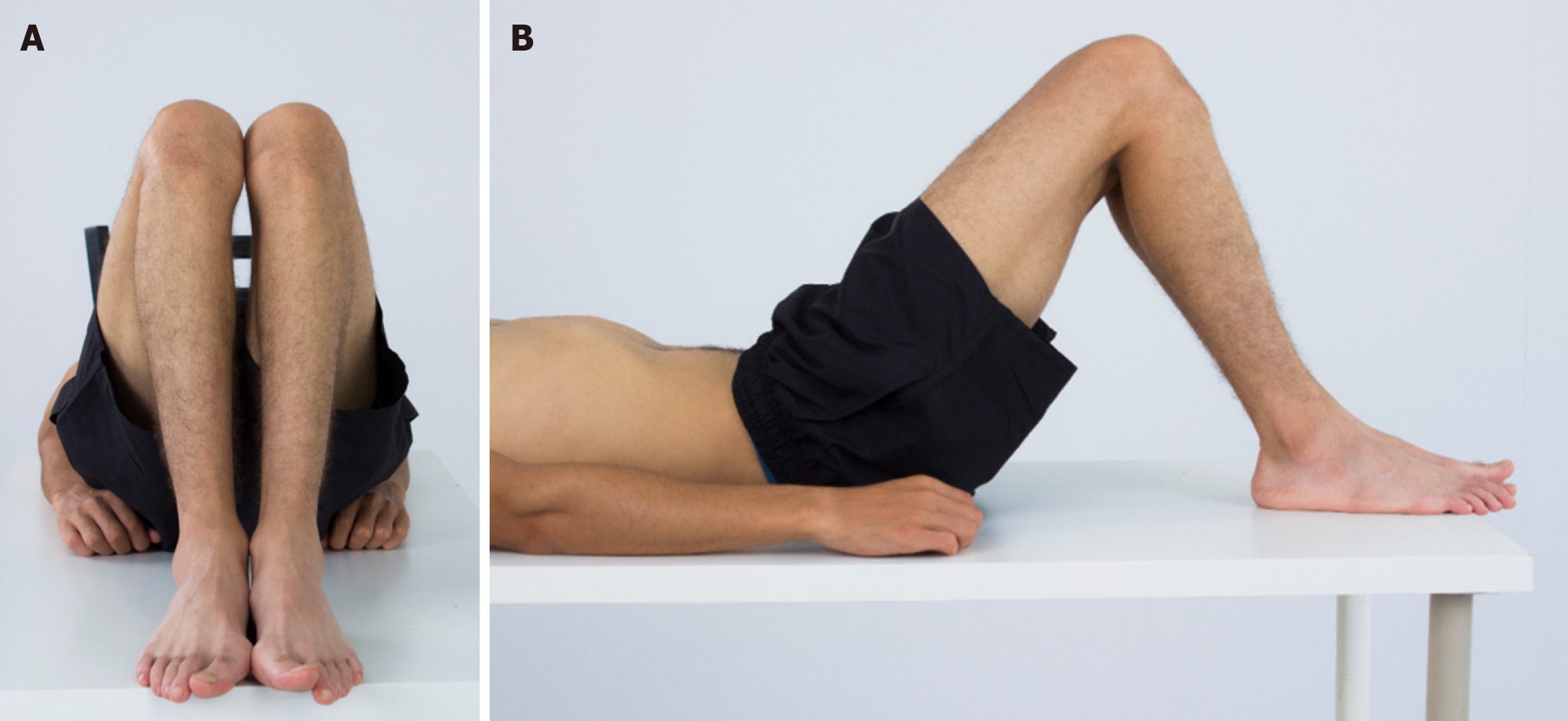
Fixed flexion deformities also can be assessed. An alternative to the Thomas test that can be conducted via telemedicine is to ask the patient to lie supine. Then starting in the knee-to-chest position and ask to actively extend each limb. Limb length assessment for discrepancy is done with the Geleazzi test (Figure 4), which can be effectively conducted via telemedicine. Ask the patient to lie supine and then flex both knees and hips 45 degrees. A static shot is taken from the top and the side views. Another way to determine limb length discrepancy is that in a normal patient the heels should be level with each other and the plane of the anterior superior iliac spines at right angles to the edge of the couch. If there is significant, true shortening the heels will not be level and the discrepancy is a guide to the amount of shortening. The pelvis will not be tilted[10].
Specific complaints reveal the most common symptoms of patients with knee instability. Accurate assessment of the symptoms tells the physician a lot about the exact diagnosis[10,24]. Inspection should be done with bilateral knee exposure after instructing the patient to wear short swimwear. Look for genu recurvatum, genuvalgum, and genuvarum while patient is standing and for the position of the patella relative to the femoral condyles. The position of the patella should also be examined with knee flexion to assess the lateral position in case of lateral patellar dislocation. Then ask the patient to extend the knees, and look for any gross disturbance of patellar tracking. It should move smoothly in the patellar groove. Quadriceps wasting is assessed by asking the patient to put a towel underneath the popliteal fossa and push against it[24].
Active ROM done by instructing the patient to flex and extend the knees, assess if there is any limitation of movement, and ask the patient if the movement is painful or not. If the patient cannot fully extend the knee actively, extension lag and knee flexion deformity are differentiated by asking the patient to put his other leg beside the examined leg and try to complete the range of extension. If the examined leg is extended more, the reason is extension lag, and if it is not extended more, then it is knee flexion deformity[10,24].
Rupture of the posterior cruciate ligament may permit the tibia to sublux backwards. The knee should be flexed to 20°, with a sandbag under the thigh. The patient should be asked to lift the heel from the couch while observing the knee from the lateral aspect. Any posterior subluxation should normally correct during extension of the knee, confirming the diagnosis[10,24].
The Thessaly test (Figure 5) is done to examine for meniscal injury. It is performed at 5° and 10° of flexion. The patient can use a front wall as a support during a single leg squat to maintain balance the knee is flexed to the required amount. With the other lifted clear, the patient twists slowly from side to side. The result is positive if the patient experiences joint-line pain or sensations of locking or catching within the knee[10,24]. Common peroneal nerve testing is done easily by assessing the patient’s ability to do ankle and big toe dorsiflexion[24].
Ankle joint assessment should be done with ipsilateral foot and knee assessment. For full inspection of ankle and foot, the patient should be asked to remove the shoes and socks with exposure to at least above the knee. Inspection should be from all sides, the anterior, posterior, lateral, medial, dorsal, and plantar surfaces of foot, and while standing and sitting. The surgeon should inspect the gait of the patient and also inspect the other side. We inspect the ankle and foot to detect any alignment deformity, scars, swelling, color change, callosities, and ulcerations[25]. While the patient is standing in an anterior view, the surgeon should note whether the external rotation of the foot in the sagittal plane is within the normal range of 5-18 degrees. Causes of toe-out or toe-in signs should be investigated if noticed[25,26]. The big toe should be evaluated for abnormalities such as hallux valgus or hallux varus. Alignment of the lesser toes should be inspected to detect any abnormal alignment, such as hammertoe[25]. From the medial aspect with the patient standing, the surgeon should note whether the medial longitudinal arch of foot if normal or shows a deformity such as pescavus or pesplanus[7,25]. From the posterior with the patient standing, hindfoot alignment is evaluated by the angle between an imaginary line bisecting heel and another line bisecting the calf, which is normally in valgus about 5-10 degrees[25]. The importance of palpation of the foot is to determine the point of maximum tenderness, which is easily done in the ankle and foot by asking the patient to use the index finger to palpate all over the sides and surfaces of ankle and foot and asking which is the point of maximum tenderness.
Active ROM done by instructing the patient to do the same movements as the surgeon or as shown in a figure, with assessment of any obvious limitations. The patient should be asked which movement is painful and to compare both ankles. Active ROM is tested by asking the patient to stand on tiptoes to assess active plantarflexion and to stand over the heels to assess active dorsiflexion. Active inversion and eversion are tested by asking the patient to stand over the inner and outer borders of the foot. Ankle passive dorsiflexion and planter flexion are done with the help of caregiver by holding the patient's heel neutral with one hand, inverting the midfoot with the other hand, and dorsiflex the ankle with the knee extended and then with the knee flexed at 90 degrees. Flexion is limited in case of stiffness, ankle fracture, or posterior structure. If the angle of dorsiflexion is same with knee flexion or extension, then the cause is the soleus muscle. If dorsiflexion is greater with the flexed knee, then the cause is gastrocnemius contracture[26].
Thompson's test is used to test the integrity of the tendon Achilles. The patient is asked to take the prone position with the feet off the end of table. A caregiver is asked to squeeze the calf on the normal and on the affected side. If the planter flexion movement is lost on the affected side, then a tear in the Achilles tendon is indicated[25]. The Coleman Block Test (Figure 6) is performed by placing the patient's foot on wooden block, 2.5-4 cm thick, with the heel and lateral border of foot on the block and bearing full weight while the first, second, and third metatarsals are allowed to hang freely. The test is used to assess the flexibility of hindfoot deformity in cases of cavovarus foot[27]. The tiptoe test is used to differentiate between flexible and rigid pesplanus deformity. In flexible flatfoot, the foot arch forms again when standing tiptoe[27,28].
Deformity with a progressive course in adolescence suggests scoliosis, while in old age and obesity back pain radiating to the extremity can suggest spondylosis. Ambulation or inadequate upper or lower limb function may indicate myelopathy or signify the degree of compression and possible need of surgical intervention. Bowel/bladder and sexual symptoms must to be evaluated to exclude the possible development of cauda equina syndrome[29,30]. The proper inspection of the entire spine is done by asking the patient to undress to underwear as possible. Normal sagittal curvature has cervical lordosis, thoracic kyphosis, and lumbar lordosis. Lost lumbar lordosis may indicate a protective spasm or posterior pelvic tilt, while exaggerated lumbar lordosis may suggest spondylolisthesis. Coronal alignment assessment should be done in a systematic descending manner, looking from head to heels. Gait should be inspected. Abnormal gaits related to spine disorders include a short step gait for back muscle spasm, an unsteady gait for myelopathy, and a sciatica gait for nerve root tension and lumbar disc prolapse. Heel to toe walking helps to approximately assess the motor power of the L4 and S1 nerve roots[31,32].
Start with cervical ROM assessment by asking the patient to point the camera sagittal to the of neck. Then ask the patient to move the chin to the chest and measure the distance between them (flexion) using a virtual ruler. Extension is determined with the patient looking at the ceiling and measuring the angle between the face and a horizontal line using goniometer-based software if available. Lateral bending is determined with the camera pointed at the front of the neck. Ask the patient to touch the ear to the shoulder and measure the distance between them using a virtual ruler. Rotation can then be determined by asking the patient to turn the chin to the shoulder. The same concepts are followed in thoracolumbar ROM assessment. Ask the patient to lean forward with extended knees and measure the degrees of flexion, Extension is the determined by extending the back as much as possible and measuring the degrees of extension as the angle between the back and a vertical line. Coronally, lateral bending is determined by asking the patient to lean laterally and advance the fingers down the legs with extended knees and measuring the degree of bending by finger to floor distance. Then, for thoracic rotation, with the patient sitting on a chair and the camera at a higher level, ask him/her to rotate the trunk, and measure the angle between shoulder and the coronal planes.
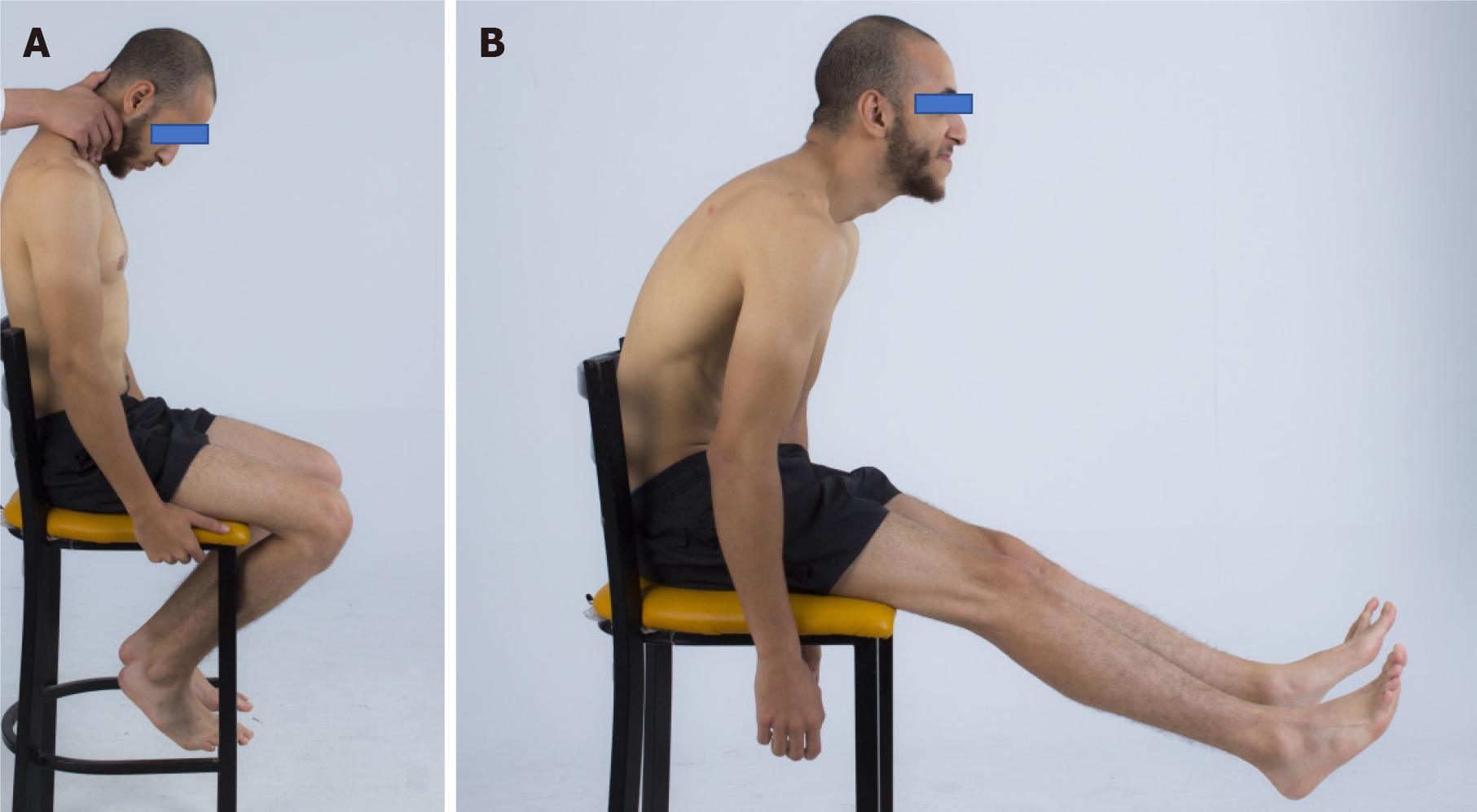
Sensory assessment can be done with a chart of the upper and lower limbs that shows the dermatomes at clear, easily located points. A caregiver can help by using cotton and the chart to compare both sides, with the patient’s eyes closed. Motor assessment can be performed using simple measures to exclude weakness. If the patient can perform the movement against resistance, then the muscle grading is three or more. If any degree of resistance is offered, the grade is four or five. For cervical nerve root motor assessment, ask the patient to flex the elbow (C5), to extend the elbow (C7), to extend the wrist (C6), to flex the fingers (C8), and to abduct them (T1). Similarly, lumbar nerve root assessment can be conducted by asking the patient to sit and then elevate the hip maximally (L1, 2), to lie supine with knees flexed 30 degrees into a triangle. Ask the patient to extend completely (L3), then to lie on the side and ask him/her to elevate the limb with the knee extended (L5). In all the previous motions, a caregiver is asked to provide resistance. We can rely on slump test to diagnose lumbar nerve root stretch via telemedicine instead of the straight leg test. Ask the patient to sit on the edge of the couch, lean the trunk forward while the neck extended to maintain a forward gaze, and then extend the knee as actively as possible. Ask for presence of pain and its location to confirm the diagnosis (Figure 7). The Valsalva maneuver with the knee is extended can confirm nerve stretch by pain accentuation[31,33].
The age of the child is crucial for developing a differential diagnosis, for example, hip symptoms in a 7-year-old boy with delayed bone age can suggest Perthes disease[34,35]. Birth history is an important consideration especially when neuromuscular conditions such as cerebral palsy are suspected. Birth history can be divided into prenatal, natal, and postnatal periods. In the prenatal period, any history of maternal infection in the first trimester or vaginal bleeding may provide a clue for possible brain injury that could lead to cerebral palsy. Important factors to consider in the natal period include birth weight, type of presentation, mode of delivery, home or hospital delivery, any birth injuries, and whether the child was delivered full-term or preterm. Postnatally, any neonatal jaundice necessitating UV light intervention, need for neonatal intensive care unit, incidence of hypoxia or cyanosis, and Apgar score should be noted[36,37]. A family history can be important for detecting diseases such as neurofibromatosis. A nutritional history is important to consider as well, especially in the pediatric patient, and may help identify nutritional rickets as the underlying etiology for deformities in toddlers. Finally, a developmental history with both physical and mental milestones can be useful, particularly in suspected cases of neurodevelopmental disorders[38].
General examination should include facial abnormalities that may occur in Down syndrome, blue sclera that can suggest osteogenesis imperfecta, and abnormalities in height and proportions that suggest dysplasia, and café au lait spots that are characteristic of neurofibromatosis[39]. The evaluation should include observation of joint alignment to determine whether the patient has a symmetrical shoulder level, symmetrical scapulae, and a level pelvis. Search for any possible coronal knee deformities, and document intermalleolar and intercondylar distance. Observe for other potential knee deformities, including squinting patellae caused by excessive femoral anteversion, ankle deformities, and deformities of the forefoot, midfoot, and hindfoot. A similar systematic sequence can be applied to the upper limb[39].
Gait assessment should be done from coronal and sagittal views while observing the appearance of the hip, knee, and foot. Inspect for any possible anterior or posterior pelvic tilt, scissoring of the thighs, any coronal knee deformities, squinting patellae, any flexed knee gait, pes planovalgus or pes cavovarus, forefoot abduction, big toe deformities, and coronal ankle deformities. Observe for general patterns of gait deformities such as jumping, crouch, equine, ataxic, and circumduction gaits. Trendelenburg gait may occur in the setting of hip diseases like developmental dysplasia of the hip or coxa vara, short limb gait in a limb length discrepancy, out-toeing gait which may be seen in slipped capital femoral epiphysis (SCFE), and high stepping gait that often occurs in knee flexion deformities[34,35,39]. The Geleazzi test for limb length measurement can be effectively translated to telemedicine. Ask the patient to lie supine and then flex both knees and hips to 45 degrees from the top and the side views, which can then be used to interpret the cause of limb length discrepancy[39].
Plain X-rays are usually needed for evaluation of fractures, loose bodies, and the presence of arthritis. Anteroposterior and lateral views are standard and are usually required. Special views such as foot obliques or mortise view of the ankle are useful for assessment of syndesmosis, scaphoid view for scaphoid fracture diagnosis, stress views, such as clenched fist, for carpal instability, Other plain X-ray views are useful. The Zanca view may help visualize acromioclavicular joint pathologies, The Stryker notch view can show a Hill-Sachs lesion[40-42]. Computed tomography is used to show details, configuration of fractures as evaluation of intra-articular extension as in pilon fracture, or evaluation of osteochondral lesions and arthritis. Magnetic resonance imaging is used to assess the integrity of soft tissues, ligaments, tendons, occult fracture, vascular status of bone, and is also useful to detect disc herniation and nerve root compression. Nerve conduction tests are used for evaluation of nerve entrap
Laboratory studies like complete blood count, erythrocyte sedimentation rate, and C-reactive protein can be useful for detecting the presence of infection. A metabolic profile and vitamin D assay can be useful for the evaluation of nutritional rickets and SCFE. Renal function tests should be ordered if renal osteodystrophy is suspected. Finally, a serum creatin kinase-MB test should be ordered if muscle dystrophy is suspected.
Virtual assessment and management of orthopedic patients can cross geographical and temporal boundaries, improve patient comfort, increase data transmission security, reduce cost, digitize healthcare system data, and facilitate the establishment of medical databases, with potential research and audit benefits, which confirm its efficacy during health crises and epidemic diseases.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhou YH S-Editor: Wang JL L-Editor: Filipodia P-Editor: Wang LYT
| 1. | Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010;79:736-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 855] [Cited by in RCA: 628] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 2. | Daruwalla ZJ, Wong KL, Thambiah J. The application of telemedicine in orthopedic surgery in singapore: a pilot study on a secure, mobile telehealth application and messaging platform. JMIR Mhealth Uhealth. 2014;2:e28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-Effectiveness of Telemedicine in Remote Orthopedic Consultations: Randomized Controlled Trial. J Med Internet Res. 2019;21:e11330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 153] [Cited by in RCA: 215] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 4. | National Consortium of Telehealth Resource Centers. CTEC program guide room design. Available from: http://www.telehealthresourcecenter.org/sites/main/files/file-attachments/09-0824-2_ctec_program_guide-room_design_w_cm_edits.pdf. |
| 5. | Zanaboni P, Wootton R. Adoption of telemedicine: from pilot stage to routine delivery. BMC Med Inform Decis Mak. 2012;12:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 156] [Cited by in RCA: 155] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 6. | Ackerman M, Craft R, Ferrante F, Kratz M, Mandil S, Sapci H. Telemedicine/telehealth: an international perspective. Telemedicine technology. Telemed J E Health. 2002;8:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Amendola A. Physical Examination of the Foot and Ankle. In: Malanga GA, Mautner K, editors. Musculoskeletal Physical Examination E-Book: An Evidence-Based Approach. Elsevier Health Sciences, 2016: 199. |
| 8. | Flandry F, Hunt JP, Terry GC, Hughston JC. Analysis of subjective knee complaints using visual analog scales. Am J Sports Med. 1991;19:112-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 258] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 9. | Chang AL, Mandell JC. Syndesmotic Ligaments of the Ankle: Anatomy, Multimodality Imaging, and Patterns of Injury. Curr Probl Diagn Radiol. 2020;49:452-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | McRae R. Clinical orthopaedic examination. Churchill Livingstone: Elsevier, 2010. |
| 11. | Lazaro LE, Cordasco FA. Physical exam of the adolescent shoulder: tips for evaluating and diagnosing common shoulder disorders in the adolescent athlete. Curr Opin Pediatr. 2017;29:70-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Colak C, Winalski CS. Fundamentals in Shoulder Radiology. In: Huri G, Familiari F, Moon YL, Doral MN, Muccioli GMM, editors. Shoulder Arthroplasty. Cham: Springer, 2020: 123-140. |
| 13. | Dhatt SS, Prabhakar S. Handbook of clinical examination in orthopedics: an illustrated guide. Cham: Springer, 2019: 1-3. |
| 14. | Skirven TM, Osterman AL, Fedorczyk J, Amadio PC. Rehabilitation of the Hand and Upper Extremity, 2-Volume Set E-Book: Expert Consult. 6th ed. St Louis: Mosby, 2011: 320-350. |
| 15. | Karbach LE, Elfar J. Elbow Instability: Anatomy, Biomechanics, Diagnostic Maneuvers, and Testing. J Hand Surg Am. 2017;42:118-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 16. | American Society for Surgery of the Hand. The hand: examination and diagnosis. Churchill Livingstone: American Society for Surgery of the Hand, 1990. |
| 17. | Rayan G, Akelman E. The hand: anatomy, examination, and diagnosis. Lippincott Williams & Wilkins, 2012. |
| 18. | Welch JP, Temtamy SA. Hereditary contractures of the fingers (camptodactyly). J Med Genet. 1966;3:104-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Abboud JA, Bozentka DJ, Beredjiklian PK. Telemedicine consultation for patients with upper extremity disorders is reliable. Clin Orthop Relat Res. 2005;250-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Collins S, Visscher P, De Vet HC, Zuurmond WW, Perez RS. Reliability of the Semmes Weinstein Monofilaments to measure coetaneous sensibility in the feet of healthy subjects. Disabil Rehabil. 2010;32:2019-2027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Phalen GS. The carpal-tunnel syndrome. Seventeen years' experience in diagnosis and treatment of six hundred fifty-four hands. J Bone Joint Surg Am. 1966;48:211-228. [PubMed] |
| 22. | Aulicino PL, DuPuy TE. Clinical examination of the hand. In: Hunter JM, Mackin EJ, Callahan AD, editors. Rehabilitation of the hand: surgery and therapy, 4. St Louis: Mosby, 1995: 53-75. |
| 23. | Duckworth AD, Jenkins PJ, McEachan JE. Diagnosing carpal tunnel syndrome. J Hand Surg Am. 2014;39:1403-1407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Bronstein RD, Schaffer JC. Physical Examination of Knee Ligament Injuries. J Am Acad Orthop Surg. 2017;25:280-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Lampley AJ, Gross CE, Klement M, Easley ME. Clinical Examination. In: Valderrabano V, Easley M, editors. Foot and Ankle Sports Orthopaedics. Cham: Springer, 2016: 39-48. |
| 26. | van Ochten JM, de Vries AD, van Putte N, Oei EHG, Bindels PJE, Bierma-Zeinstra SMA, van Middelkoop M. Association between Patient History and Physical Examination and Osteoarthritis after Ankle Sprain. Int J Sports Med. 2017;38:717-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Alazzawi S, Sukeik M, King D, Vemulapalli K. Foot and ankle history and clinical examination: A guide to everyday practice. World J Orthop. 2017;8:21-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 28. | Deakins-Roche M, Fredericson M, Kraus E. Ankle and Foot Injuries in Runners. In: Harrast MA, editor. Clinical Care of the Runner. Elsevier, 2020: 231-245. |
| 29. | Choudhry MN, Ahmad Z, Verma R. Adolescent Idiopathic Scoliosis. Open Orthop J. 2016;10:143-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 142] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 30. | Korse NS, Pijpers JA, van Zwet E, Elzevier HW, Vleggeert-Lankamp CLA. Cauda Equina Syndrome: presentation, outcome, and predictors with focus on micturition, defecation, and sexual dysfunction. Eur Spine J. 2017;26:894-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 31. | Fine NF, Stokes OM. Clinical examination of the spine. Surgery (Oxford). 2018;36:357-361. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Haddas R, Ju KL, Belanger T, Lieberman IH. The use of gait analysis in the assessment of patients afflicted with spinal disorders. Eur Spine J. 2018;27:1712-1723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 33. | Roberts TT, Leonard GR, Cepela DJ. Classifications In Brief: American Spinal Injury Association (ASIA) Impairment Scale. Clin Orthop Relat Res. 2017;475:1499-1504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 412] [Article Influence: 51.5] [Reference Citation Analysis (1)] |
| 34. | Gordon JE, Schoenecker PL, Osland JD, Dobbs MB, Szymanski DA, Luhmann SJ. Smoking and socio-economic status in the etiology and severity of Legg-Calvé-Perthes' disease. J Pediatr Orthop B. 2004;13:367-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 35. | Peck DM, Voss LM, Voss TT. Slipped Capital Femoral Epiphysis: Diagnosis and Management. Am Fam Physician. 2017;95:779-784. [PubMed] |
| 36. | practice guideline: early detection of developmental dysplasia of the hip. Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip. American Academy of Pediatrics. Pediatrics. 2000;105:896-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 212] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 37. | Pearl PL, Sable C, Evans S, Knight J, Cunningham P, Lotrecchiano GR, Gropman A, Stuart S, Glass P, Conway A, Ramadan I, Paiva T, Batshaw ML, Packer RJ. International telemedicine consultations for neurodevelopmental disabilities. Telemed J E Health. 2014;20:559-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Cass AD, Camasta CA. A review of tarsal coalition and pes planovalgus: clinical examination, diagnostic imaging, and surgical planning. J Foot Ankle Surg. 2010;49:274-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 39. | Sarup S. Common Orthopedic Problems in Children. In: Sawhney S, Aggarwal A, editors. Pediatric Rheumatology 2017. Singapore: Springer, 2017: 181-199. |
| 40. | Terry MA, Winell JJ, Green DW, Schneider R, Peterson M, Marx RG, Widmann RF. Measurement variance in limb length discrepancy: clinical and radiographic assessment of interobserver and intraobserver variability. J Pediatr Orthop. 2005;25:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 41. | Thierfelder KM, Gemescu IN, Weber MA, Meier R. [Injuries of ligaments and tendons of foot and ankle: What every radiologist should know]. Radiologe. 2018;58:415-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | Farber JM, Buckwalter KA. Sports-related injuries of the shoulder: instability. Radiol Clin North Am. 2002;40:235-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 43. | Medina LS, Applegate KE, Blackmore CC. Evidence-based imaging in pediatrics: optimizing imaging in pediatric patient care. Springer, 2010. |
| 44. | Cohen MD. Clinical utility of magnetic resonance imaging in pediatrics. Am J Dis Child. 1986;140:947-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |