Published online Aug 18, 2021. doi: 10.5312/wjo.v12.i8.575
Peer-review started: January 29, 2021
First decision: May 3, 2021
Revised: May 12, 2021
Accepted: June 22, 2021
Article in press: June 22, 2021
Published online: August 18, 2021
Processing time: 194 Days and 3.4 Hours
Limb lengthening techniques play an increasingly important role in the pediatric orthopedic field. The principles of the osteogenesis distraction bonded traditionally with external fixators; however, the recent deployment of fully implantable systems has been able to overcome severities related to external fixators. The PRECICE® is an implantable limb lengthening intramedullary nail system that is remotely controlled and magnetically driven.
To review the current literature available on this matter in order to assess the PRECICE clinical and radiological outcomes and its possible complications in a population of pediatric patients undergoing limb lengthening.
Only five studies met the inclusion criteria and were consequently included in the review for a total of 131 patients and 135 femurs. The clinical and radiological outcomes of interest were: the main lengthening obtained, the distraction rate, the period of time to full weight bearing, the consolidation index, and the Association for the Study and Application of Methods of Ilizarov score.
In conclusion, data collected from the articles under investigation were comparable with the exception of the consolidation index. Unfortunately, the study population was too small and the patients’ follow-up was too short to make definitive conclusions.
This review shows that the PRECICE Nail System is still a therapeutic challenge in limb lengthening for pediatric orthopedic surgeons; however, careful pre-operative planning and an accurate surgical technique could allow the correction of more complex deformities with a low rate of complications.
Core Tip: Limb lengthening techniques play an increasingly important role in the pediatric orthopedic field. The PRECICE® is an implantable limb lengthening intramedullary nail system that is remotely controlled and magnetically driven. The aim of our study was to review the current literature in order to assess the clinical and radiological outcomes and possible complications in a population of pediatric patients undergoing limb lengthening. This review shows that the PRECICE allows correction of the more complex deformities with a low rate of complications.
- Citation: Masci G, Palmacci O, Vitiello R, Bonfiglio N, Bocchi MB, Cipolloni V, Maccauro G, Pola E. Limb lengthening with PRECICE magnetic nail in pediatric patients: A systematic review. World J Orthop 2021; 12(8): 575-583
- URL: https://www.wjgnet.com/2218-5836/full/v12/i8/575.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i8.575
Limb lengthening techniques play an increasingly important role in the field of pediatrics orthopedics with regard to length discrepancy, angular deformities (referable either to fractures sequelae or congenital malformations), and short stature correction[1-4]. The osteogenesis distraction is a reparative process involving not only the bone but also the soft tissues including the muscles, nerves, and skin. Therefore, accurate distraction control is required since too rapid correction could lead to nonunion, nerve damage, and joint contractures, while on the other hand a process that is too slow could result in premature consolidation[5].
The principles of the osteogenesis distraction bonded traditionally with the external fixators, considering both monolateral and circular fixators[6,7]. More recently, the deployment of fully implantable systems for limb lengthening has allowed over
At present, three types of telescopic nails are mainly used: mechanically activated nails, motorized nails, and magnetically driven nails[14-16]. The PRECICE® Intramedullary Limb Lengthening System (NuVasive Specialized Orthopedics, San Diego, CA, United States) is a remotely controlled, magnetically driven, implantable limb lengthening intramedullary nail system first used in Europe in 2012[17-19]. The PRECICE nail is a magnet-operated telescopic internal lengthening device with an ERC that contains two rotating magnets[20]. When placed by the patient on the skin, above the magnet which is within the nail, it causes this internal magnet to rotate, which translates to the thinner nail element telescoping out of the thicker surrounding nail; the nail can be both extended and retracted by altering the settings on the ERC as well as accurately setting the rate of distraction. A distance of 1 mm requires the ERC to be placed over the magnet within the nail for 7 min[21].
The PRECICE represents a safe and accurate technique able to correct both deformity and limb-length discrepancy, lengthening but also shortening (unlike other lengthening nails[22]) with reduced side effects . Among the advantages of opting for this implant, there is the ability to maintain the knee range of motion during the lengthening process and also the rapid bone healing allows a relatively early return to weight bearing[23,24].
The aim of our study was to review the current literature available on this matter in order to assess the PRECICE clinical and radiological outcomes and its possible complications in a population of pediatric patients undergoing limb lengthening.
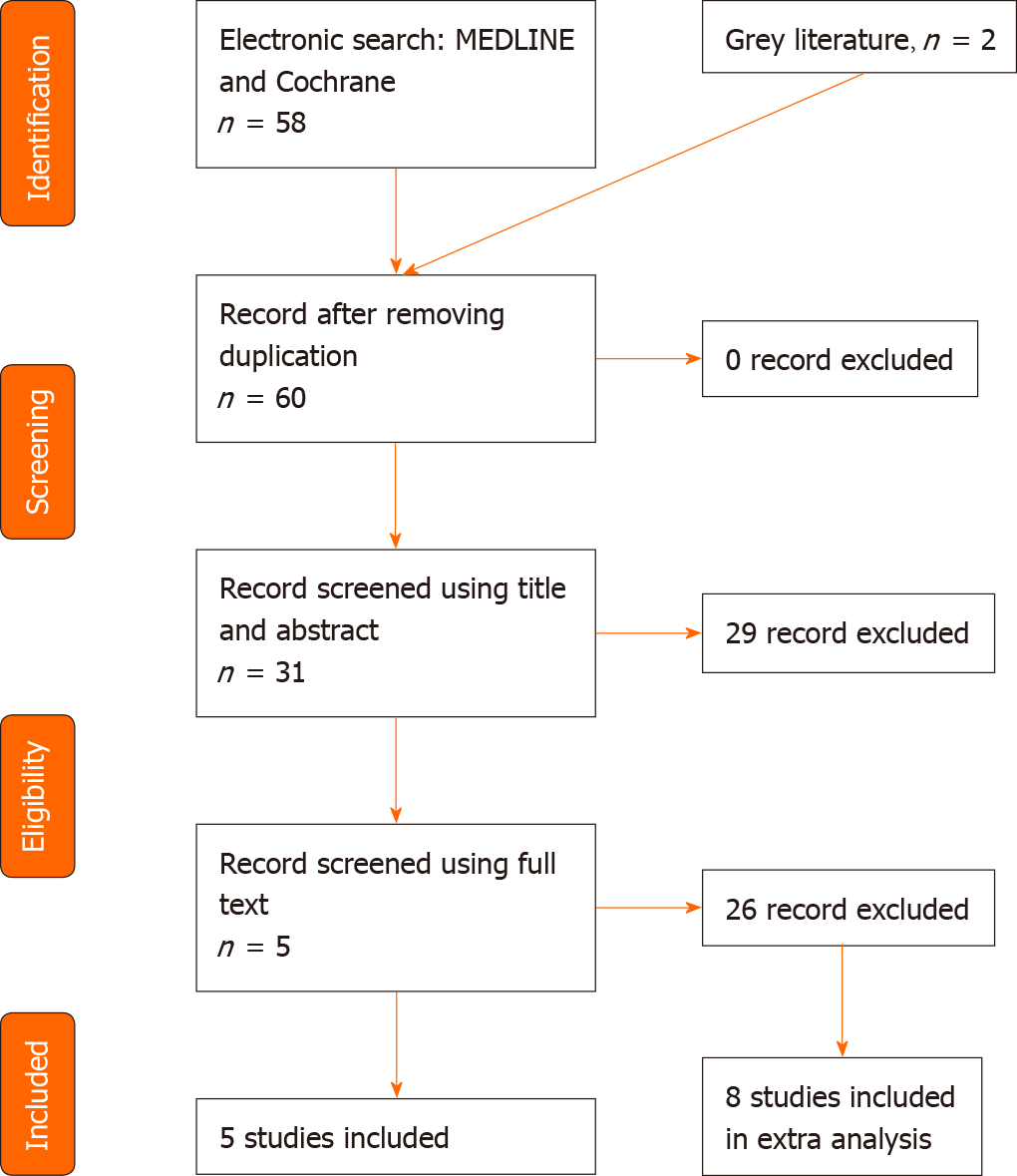
A systematic review of the literature indexed in PubMed MEDLINE and Cochrane Library databases using the search key word “PRECICE” was carried out. To minimize the number of missed studies, no filters were applied to the search strategy. The bibliography of the selected studies was accurately searched by hand, in order to identify further studies not found during our electronic search. No restrictions on the date of publication or language were applied. The title of the journal, name of authors, or supporting institutions were not masked at any stage. No attempt to contact authors in order to obtain individual patient data was made. The Preferred Reporting Items for Systematically Reviews and Meta-Analyses (PRISMA) was followed as reported in Figure 1. In order to be considered for this review, the articles needed to comply with the following inclusion criteria: use of the PRECICE® Intramedullary Limb Leng
The electronic search resulted in 60 hits. Following the PRISMA flow chart[26], only five studies met the inclusion criteria and were taken into consideration in the review[27-31]. Eight papers partially followed the inclusion criteria; these studies included a non-specific pediatric population. An extra analysis was performed for these latter papers. All of the selected studies were retrospectively analyzed. The target population consisted of 131 patients for a total of 135 femurs. According to the mCMS evaluation, the mean score of the studies reached was 47 points (25-57 points) showing a poor-mediocre result. The papers we took into consideration had several methodological issues, particularly when considering the procedure in assessing the outcomes. Moreover, the study population was too small and the patient’s follow-up was too short. However, all of the papers accurately reported the indications for surgical intervention and the surgical technique (respectively 5 points each). Studies by Szymczuk et al[30] and Hammouda et al[32] compared the PRECICE intramedullary nailing with external fixation, but in our analysis, we only took into account the PRECICE nailing results. In studies by Nasto et al[27] and Iliadis et al[29], both retrograde and antegrade approaches were used, and some tibia nailing was included. Other studies preferred the antegrade approach to the femur.
We reached a population of 131 male and female patients for a total of 135 femurs. Males and females numbered 69 and 62, respectively. The mean age was 14.8 years old, ranged between 7 and 18 years old[31]. All of the studies reported pre-operative discrepancy except one[31], with a mean value of 5.2 cm (range, 4.9 to 6.3). The mean follow-up was 1.7 years when reported (Table 1). Concerning surgical indications, one study only focused on a single pathology; in particular, Szymczuk et al[30] focused on congenital femoral deficiency treatment for a total of 30 femurs (Table 2). Among other papers, the principal surgical indication was congenital femoral deficiency (19 femurs), and yet post-traumatic malformations (18 femurs), achondroplasia (8 femurs), hemihypertrophy (8 femurs) and Ollier disease (6 femurs). Nevertheless, the main indication remained “miscellaneous” (46 femurs).
| Ref. | Number of patients | Gender | Tibia nailing | Age (yr) | Discrepancy (cm) | Follow-up (yr) | mCMS |
| Hammouda et al[32] | 28 patients; 31 femurs | 17 males; 11 females | - | 12.9 | - | 1.9 | 49 |
| Szymczuk et al[30] | 30 | 14 males; 16 females | - | 15.4 | 4.9 | 1.9 | 51 |
| Iliadis et al[29] | 42 patients; 43 femurs | 20 males; 22 females | 7 | 15 | 4.9 | - | 54 |
| Nasto et al[27] | 26 | 15 males; 11 females | 5 | 14.7 | 4.9 | 1.4 | 57 |
| Tomaszewski et al[28] | 5 | 3 males; 2 females | - | 16.3 | 6.3 | - | 27 |
Regarding the PRECICE system results, the studies examined focused on the following issues: The main lengthening obtained with particular reference to accuracy and reliability, the distraction rate, the period to reach full weight bearing, the consolidation index, and the Association for the Study and Application of Method of Ilizarov (ASAMI) score (Table 3 and Table 4). Nail accuracy is defined as the ratio between the lengthening obtained and the planned length, while nail reliability is the ratio between the number of implanted lengthening devices and the number of successfully ended lengthening treatments. Analyzing the main lengthening obtained, the results were similar across all studies. In particular, Hammouda et al[31] reported a mean lengthening of 5.6 (3-6.7), with no reference to accuracy and reliability. It is relevant to notice that the authors performed intramedullary nailing using the trochanteric entry. During the follow-up time no patients showed radiographic nor clinical signs of femoral head necrosis. The average lengthening achieved reported by Nasto et al[27] was 4.4 ± 1.2, with a nail accuracy and reliability of 91% and 88% respectively. Iliadis et al[29] reported a nail accuracy of 96% and a nail reliability of 98%, due to a single case where a nail was implanted without lengthening because of the patient’s mental health issues.
| Ref. | Mean lengthening (cm) | Accuracy | Reliability | Distraction rate (mm/d) | Day to full weight bearing | Consolidation index (d/cm) | ASAMI functional score | ASAMI bone score |
| Hammouda et al[32] | 5.6 (3-6.7) | - | - | - | - | - | - | - |
| Szymczuk et al[30] | 4.75 ± 1.43 | 95% | - | 0.7 ± 0.18 | - | 34.7 ± 11.2 | - | - |
| Iliadis et al[29] | - | 96% | 98% | 0.92 (0.67-1) | 45 (21-132) | 28 (18-43) | 35 excellent; 11 good; 3 fairs; 1 poor | 41 excellent; 8 good; 1 fair |
| Nasto et al[27] | 4.4 ± 1.2 | 91% | 88% | 0.9 ± 0.1 | - | 11.9 ± 2.1 | 22 excellent; 3 good; 1 fair | 24 excellent; 1 fair; 1 poor |
| Tomaszewski et al[28] | 4.9 (4-5.8) | - | - | 0.8 (0.8-1) | - | 29.3 (21-33) | - | - |
The distraction index (DI), defined as the ratio between the number of days of distraction and the achieved length (days/cm), was reported in all of the studies analyzed, except for Hammouda et al[31]. Among the articles, the results were almost comparable. Szymczuk et al[30] described a DI of 0.7 ± 0.18, while Iliadis et al[29] reported a DI of 0.92 (0.67-1). Furthermore, this latter retrospective review was the only one considering the days to full weight bearing from lengthening accom
Adverse events were divided into problems, obstacles, and complications in accordance with the data previously described by Paley[17]. Problems were defined as difficulties after the surgical procedure resolved with conservative treatment, obstacles were difficulties that required surgical treatment, and complications were true intra or post-operative complications that persisted after the treatment. Hammouda et al[31] reported no problems or obstacles in 28 patients and two complications. Among them, 1 patient developed hip subluxation and delayed union of the regenerate, which was treated surgically. In addition, the nail was exchanged 6 mo after surgery. Iliadis et al[29] reported instead seven problems, four obstacles, and four complications. In 7 cases, they reported joint stiffness during the lengthening period, which was resolved with physiotherapy and by slowing down the distraction. Two femoral nails required the locking bolts removal as they were causing discomfort after consolidation. One patient with fibrous dysplasia, who previously underwent proximal femoral osteotomy with locking plate fixation, had a periprosthetic fracture so the PRECICE was exchanged with a trauma nail, but with loss of about 30 mm of lengthening.
Tomaszewski et al[28] reported no inflammatory complications, but in 1 case, after a lengthening of more than 45 mm, they noted a knee flexion contracture of about 10° despite the physiotherapy. Moreover, they had to stop the lengthening treatment in 1 case due to the pain and femoral nerve paresthesia. In the retrospective multi-center study conducted by Nasto et al[27], a total of five problems (joint contractures), one obstacle (femur fracture), and three complications (hip subluxation, 1 deep infection and 1 nail running back) were encountered. No bone healing complications were reported. Considering the patient who developed deep infection, the treatment was suspended and the nail removed. Regarding the case of hip subluxation, we would like to note that the patient had a developmental hip dysplasia history treated with proximal femur varus derotation osteotomy (VDRO) and Dega osteotomy. This complication was surgically treated with periacetabular osteotomy and VDRO; at the latest follow-up, the patient was asymptomatic and pain free during walking.
Analyzing the entire population, a great heterogeneity has emerged in terms of age (7-72), male/female ratio, surgical access and surgical site[18,19,21,32-36]. The rise in the average population age has led to an increase of post-traumatic etiology[32], although the congenital and syndromic causes are still well represented[18,32,36]. All of the reviewed articles analyzed both femoral and tibial lengthening nails outcomes, except one[32]. In a retrospective review by Wagner et al[18], both PRECICE nail accuracy and precision reached 97.3% and 92.4%, respectively, with a total of nine complications (28%), all of which were successfully resolved without any long-term sequelae. In his 24-nail series, Kirane et al[21] revealed an accuracy of 96% and a precision of 86% with only one (4%) implant-related failure caused by a non-functional distractor mechanism and 6 (24%) non-implant-related obstacles; the minimum follow-up was 3 wk (mean 14 wk). In a different 9 case series by Wiebking et al[34], there were significant differences regarding the lengthening goal achievement and thus also the full weight bearing among patients. Consequently, the accuracy and the precision rate were 78% vs 61%, respectively. Despite the complications, patient satisfaction was generally positive.
A slight improvement in the quality of life was shown in preoperative and 12-mo postoperative Enneking scores; no differences were revealed in the physical and mental SF-12 score[18].
Concerning complications, a low complication rate was demonstrated in a series of 17 post-traumatic femoral lengthening nails with 2.2-year follow-up[32]. Hammouda et al[32] reported 3 patients (18%) with non-implant related complications that all resolved without permanent sequelae. Similar outcomes were reported by Horn et al[35] who described 8 of 50 complications, which were treated by surgery without sequelae and therefore were graded as obstacles. However, in this study, 16 nails were not PRECICE[35].
This review shows that the PRECICE Nail System is still a therapeutic challenge in limb lengthening for pediatric orthopedic surgeons. In the literature, only few studies have been published; nevertheless, the outcome demonstrates excellent clinical results and patient satisfaction. Careful pre-operative planning and an accurate surgical technique could allow correction of the more complex deformities with a low rate of complications.
Limb lengthening devices have evolved in the last century to correct limb length discrepancies, congenital short statures, and limb deformities. The unilateral external fixator has been the standard method of fixation for a long time; however, the method of fixation has rapidly evolved from unilateral external fixator to the ring fixator, to the computer-assisted fixator, and finally to the lengthening of intramedullary nails.
The large number of complications related to the use of external fixation has led to the development of alternatives. The PRECICE represents an innovative and less invasive option to external fixation with regard to limb lengthening, allowing a controlled lengthening phase with the ability to shorten and regulate the device if necessary.
To review the current literature available on the specific matter in order to assess the PRECICE clinical and radiological outcomes and its possible complications in a population of pediatric patients undergoing femur lengthening.
The current study is the result of a systematic review of the available literature using a single search term “PRECICE”. The articles were sorted according to both pre
Five studies met the inclusion criteria for a total of 131 patients. The studies examined focused on the following issues: the main lengthening obtained, the distraction rate, the number of days necessary to reach full weight bearing, the consolidation index and the ASAMI score. Among the articles all the results were almost comparable with the only exception of the consolidation index. Adverse events that emerged in a low percentage were divided into problems, obstacles, and complications.
Although the PRECICE nail system is still a therapeutic challenge, the results have shown excellent clinical results and patient satisfaction with a low rate of complications. Therefore this approach could represent a valid alternative to the traditional limb lengthening systems.
Future studies on larger and more homogeneous samples are needed to validate the use of PRECICE.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang XQ S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Li X
| 1. | Popkov A, Dučić S, Lazović M, Lascombes P, Popkov D. Limb lengthening and deformity correction in children with abnormal bone. Injury. 2019;50 Suppl 1:S79-S86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Chilbule SK, Dutt V, Madhuri V. Limb lengthening in achondroplasia. Indian J Orthop. 2016;50:397-405. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Alrabai HM, Gesheff MG, Conway JD. Use of internal lengthening nails in post-traumatic sequelae. Int Orthop. 2017;41:1915-1923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Vitiello R, Lillo M, Donati F, Masci G, Noia G, De Santis V, Maccauro G. Locking plate fixation in pediatric femur fracture: evaluation of the outcomes in our experience. Acta Biomed. 2019;90:110-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 5. | Ippolito E, Peretti G, Bellocci M, Farsetti P, Tudisco C, Caterini R, De Martino C. Histology and ultrastructure of arteries, veins, and peripheral nerves during limb lengthening. Clin Orthop Relat Res. 1994;54-62. [PubMed] |
| 6. | Calder PR, Faimali M, Goodier WD. The role of external fixation in paediatric limb lengthening and deformity correction. Injury. 2019;50 Suppl 1:S18-S23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 7. | Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990;8-26. [PubMed] |
| 8. | Hosny GA. Limb lengthening history, evolution, complications and current concepts. J Orthop Traumatol. 2020;21:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 9. | Green SA. Complications of external skeletal fixation. Clin Orthop Relat Res. 1983;109-116. [PubMed] |
| 10. | Farsetti P, De Maio F, Potenza V, Efremov K, Marsiolo M, Caterini A, Ippolito E. Lower limb lengthening over an intramedullary nail: a long-term follow-up study of 28 cases. J Orthop Traumatol. 2019;20:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Axelrod D, Rubinger L, Shah A, Guy P, Johal H. How should we lengthen post-traumatic limb defects? Eur J Orthop Surg Traumatol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464-1480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 302] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 13. | Socci AR, Horn D, Fornari ED, Lakra A, Schulz JF, Sharkey MS. What's New in Pediatric Limb Lengthening and Deformity Correction? J Pediatr Orthop. 2020;40:e598-e602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Thonse R, Herzenberg JE, Standard SC, Paley D. Limb Lengthening with a Fully Implantable, Telescopic, Intramedullary Nail. Oper Tech Orthop. 2005;15:355-362. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Cole JD, Justin D, Kasparis T, DeVlught D, Knobloch C. The intramedullary skeletal kinetic distractor (ISKD): first clinical results of a new intramedullary nail for lengthening of the femur and tibia. Injury. 2001;32 Suppl 4:SD129-SD139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 125] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 16. | Baumgart R, Betz A, Schweiberer L. A fully implantable motorized intramedullary nail for limb lengthening and bone transport. Clin Orthop Relat Res. 1997;135-143. [PubMed] |
| 17. | Paley D. PRECICE intramedullary limb lengthening system. Expert Rev Med Devices. 2015;12:231-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 147] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 18. | Wagner P, Burghardt RD, Green SA, Specht SC, Standard SC, Herzenberg JE. PRECICE® magnetically-driven, telescopic, intramedullary lengthening nail: pre-clinical testing and first 30 patients. SICOT J. 2017;3:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Schiedel FM, Vogt B, Tretow HL, Schuhknecht B, Gosheger G, Horter MJ, Rödl R. How precise is the PRECICE compared to the ISKD in intramedullary limb lengthening? Acta Orthop. 2014;85:293-298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 20. | Calder PR, Laubscher M, Goodier WD. The role of the intramedullary implant in limb lengthening. Injury. 2017;48 Suppl 1:S52-S58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 21. | Kirane YM, Fragomen AT, Rozbruch SR. Precision of the PRECICE internal bone lengthening nail. Clin Orthop Relat Res. 2014;472:3869-3878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 154] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 22. | Kariksiz M, Karakoyun O. Limb lengthening with one Precice nail over its capacity. Saudi Med J. 2019;40:1058-1062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 23. | Couto A, Freitas J, Alegrete N, Coutinho J, Costa G. Two consecutive limb lengthenings with the same PRECICE nail: a technical note. Strategies Trauma Limb Reconstr. 2018;13:199-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Chaudhary M. Limb lengthening over a nail can safely reduce the duration of external fixation. Indian J Orthop. 2008;42:323-329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 647] [Cited by in RCA: 767] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 26. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13930] [Cited by in RCA: 13358] [Article Influence: 834.9] [Reference Citation Analysis (0)] |
| 27. | Nasto LA, Coppa V, Riganti S, Ruzzini L, Manfrini M, Campanacci L, Palmacci O, Boero S. Clinical results and complication rates of lower limb lengthening in paediatric patients using the PRECICE 2 intramedullary magnetic nail: a multicentre study. J Pediatr Orthop B. 2020;29:611-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 28. | Tomaszewski R, Wiktor Ł, Kler J, Pethe K, Gap A. Results of Femoral Elongation Treatment Using Electromagnetic Intramedullary Nail. Preliminary Report. Ortop Traumatol Rehabil. 2020;22:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Iliadis AD, Palloni V, Wright J, Goodier D, Calder P. Pediatric Lower Limb Lengthening Using the PRECICE Nail: Our Experience With 50 Cases. J Pediatr Orthop. 2021;41:e44-e49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 30. | Szymczuk VL, Hammouda AI, Gesheff MG, Standard SC, Herzenberg JE. Lengthening With Monolateral External Fixation Versus Magnetically Motorized Intramedullary Nail in Congenital Femoral Deficiency. J Pediatr Orthop. 2019;39:458-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 31. | Hammouda AI, Jauregui JJ, Gesheff MG, Standard SC, Herzenberg JE. Trochanteric Entry for Femoral Lengthening Nails in Children: Is It Safe? J Pediatr Orthop. 2017;37:258-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 32. | Hammouda AI, Jauregui JJ, Gesheff MG, Standard SC, Conway JD, Herzenberg JE. Treatment of Post-Traumatic Femoral Discrepancy With PRECICE Magnetic-Powered Intramedullary Lengthening Nails. J Orthop Trauma. 2017;31:369-374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 33. | Karakoyun O, Sokucu S, Erol MF, Kucukkaya M, Kabukçuoğlu YS. Use of a magnetic bone nail for lengthening of the femur and tibia. J Orthop Surg (Hong Kong). 2016;24:374-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 34. | Wiebking U, Liodakis E, Kenawey M, Krettek C. Limb Lengthening Using the PRECICETM Nail System: Complications and Results. Arch Trauma Res. 2016;5:e36273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 35. | Horn J, Hvid I, Huhnstock S, Breen AB, Steen H. Limb lengthening and deformity correction with externally controlled motorized intramedullary nails: evaluation of 50 consecutive lengthenings. Acta Orthop. 2019;90:81-87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 36. | Shabtai L, Specht SC, Standard SC, Herzenberg JE. Internal lengthening device for congenital femoral deficiency and fibular hemimelia. Clin Orthop Relat Res. 2014;472:3860-3868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |