Published online Jun 18, 2021. doi: 10.5312/wjo.v12.i6.433
Peer-review started: December 1, 2020
First decision: February 15, 2021
Revised: March 21, 2021
Accepted: May 8, 2021
Article in press: May 8, 2021
Published online: June 18, 2021
Processing time: 191 Days and 18.8 Hours
Flexible flatfoot (FFF) is a very common condition in children, characterized by the loss of the medial arch and by an increase in the support base with valgus of the hindfoot. Arthroereisis (AR) procedures are widely performed corrective surgeries and are classified as subtalar AR and calcaneo-stop (CS).
We investigated the literature published in the last 5 years with the aim of providing an update on the evidence related to AR treatment in FFF patients. We report the principal findings of subtalar AR and CS procedures concerning clinical and radiological outcomes and complication rates in the general population, young athletes, and obese people according to material device.
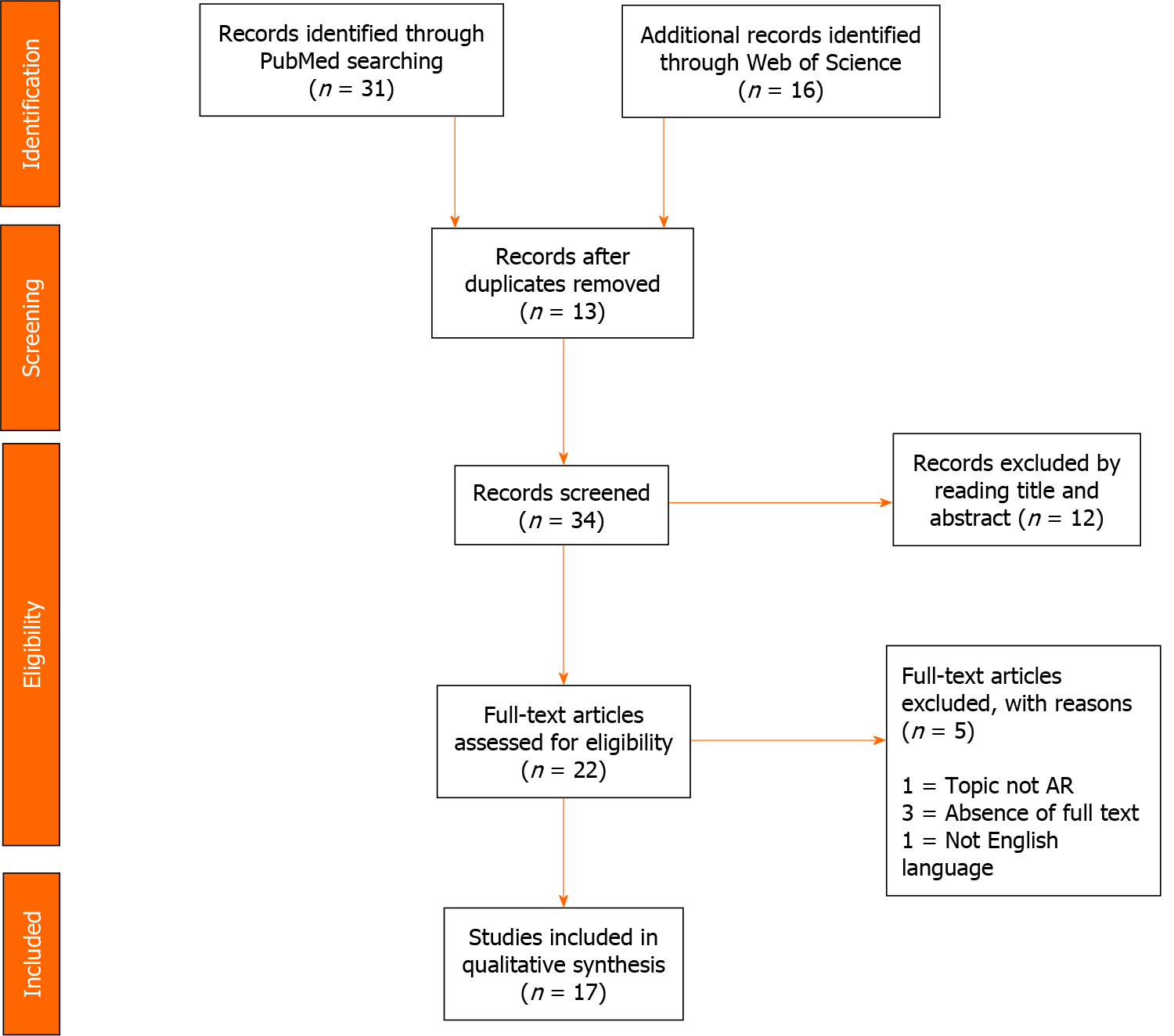
Following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, a systematic review of studies published in the past 5 years and included the PubMed and Science Direct databases was performed on May 6, 2020. The research string used was (pediatric OR children OR Juvenile NOT adult) AND (flexible NOT rigid) AND (flat foot OR pes planus) AND (calcaneo-Stop OR arthroereisis OR subtalar extra-articular screw OR SESA OR subtalar arthroereisis OR endosinotarsal). The risk of bias assessment was performed using the Dutch checklist form for prognosis.
A total of 47 articles were found. Ultimately, after reading the full text and checking reference lists, we selected 17 articles that met the inclusion and exclusion criteria. A total of 1864 FFFs were identified. Eight studies concerned the subtalar AR (47.1%) and nine concerning CS (52.9%). The average age of patients at start of treatment was 11.8 years, the average follow-up of the studies was 71.9 mo (range 29.1-130). Globally, complications occurred in 153 of the 1864 FFF treated, with a rate of 8.2%.
Both AR procedures are valid surgical techniques for treating FFF. Surgeon experience, implant cost, and cosmetic correction are the most common considerations included in the orthopedic device decision-making process. In obese patients, the subtalar AR is not recommended. In adolescents who need to improve sports performance, the CS screw had better results compared with other implants.
Core Tip: Arthroereisis (AR) procedures are widely performed corrective surgeries for juvenile flexible flatfoot. The AR procedures include impact blocking devices and self-locking implants. Impact blocking devices include subtalar extra-articular calcaneo-stop (CS) screws that have a stem and a head and interfere with the talus. Self-locking implants (subtalar AR) are inserted in the sinus tarsi along its main axis. Surgeon experience, implant cost, and, cosmetic correction are the most common criteria included in the orthopedic decision-making process. Both AR procedures improved clinical and radiological parameters. Considering the complications, calcaneo-stop screws had a slightly better rate than subtalar AR.
- Citation: Vescio A, Testa G, Amico M, Lizzio C, Sapienza M, Pavone P, Pavone V. Arthroereisis in juvenile flexible flatfoot: Which device should we implant? A systematic review of literature published in the last 5 years. World J Orthop 2021; 12(6): 433-444
- URL: https://www.wjgnet.com/2218-5836/full/v12/i6/433.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i6.433
Flexible flatfoot (FFF) is a very common condition in children[1] characterized by loss of the medial arch and increases of both heel valgus and plantar pressure[1]. FFF is typically an asymptomatic condition, but pain may occur in the lower leg or medial level of the foot at the insertion point of the posterior tibial on the scaphoid, especially after intense exercise or long walks[2]. In some cases, early and easy fatigue can occur and are consider important symptoms[3]. Surgical treatment is indicated in symp
The first author to introduce the term “arthroereisis” was Lelièvre[5] in the early 70s to illustrate a temporary staple across the subtalar joint. In 1979, the Buruturan[6] impact blocking screw, which was inserted into the calcaneus using the sinus tarsi as the entry point, is the first description of a calcaneo-stop (CS) procedure. In 1992, Viladot[7] reported the success rate achieved by the first non-osseous sinus tarsi implant. The aim of implants is to correct the FFF deformity with preservation of foot function and limitation of excessive anterior displacement of the talus upon the calcaneus[8]. Moreover, some authors[9,10] have hypothesized that CS could play a role in the activation of mechanoreceptors in the sinus tarsi, although it has not yet been supported by experimental evidence. Subtalar implants are classified by type as impact blocking devices, which include subtalar AR; and self-locking implants, which include CS screws[11]. Impact blocking devices have a stem that is fixed in the sinus tarsi vertically just anteriorly to the posterior subtalar surface and a head, that interferes with the talar lateral process, limiting its internal rotation. Self-locking implants are inserted in the sinus tarsi along its main axis, supporting the talar neck, avoiding contact between talar lateral process and sinus tarsi floor, and reducing talar adduction and plantar flexion.
The aim of the study was to review the literature of the last 5 years regarding the surgical treatment of juvenile FFF with a focus on the AR procedures and to report the principal subtalar AR and CS procedure findings concerning clinical and radiological outcomes and complication rate in general population, young athletes and obese population according to the device.
A systematic review of studies published in the last 5 years. Clinical outcomes and radiological measurements, Athletes and Obese cohorts’ outcomes, Complications, Materials of subtalar AR and CS were recorded.
A systematic review of studies published in the last 5 years and indexed in PubMed and Science Direct was performed by an author (Vescio A) on May 6, 2020. The research string used was “(pediatric OR children OR Juvenile NOT adult) AND (flexible NOT rigid) AND (flat foot OR pes planus) AND (calcaneo-stop OR arthroereisis OR SESA OR subtalar arthroereisis OR s OR subtalar extra-articular screw)”.
Eligible studies for this systematic review included FFF treatment and AR. The titles and abstracts were screened, using the following inclusion criteria: treatment consisted of AR with or without additional soft tissue procedures, operative treatment, or cast application, and a minimum average follow-up of 6 mo in patients between 7 and 17 years of age. Studies of patients with secondary, including syndromic and neurological FFF, nonoperative treatment or lateral column lengthening (LCL), or medializing calcaneal osteotomy duplicate publications, articles dealing with other topics, those with poor scientific methodology or without an accessible abstract were excluded. Reference lists were also hand-searched for further relevant studies. Systematic reviews, Meta-analyses, abstracts, case reports, conference presentations, editorials, and expert opinions were excluded.
Two subtalar implant types were considered, impact blocking devices and self-locking implants[13]. The risk of bias assessment was performed independently by two authors (Vescio A and Amico M) using the Dutch checklist form for prognosis recommended by the Cochrane Collaboration[13]. Conflicts about data were resolved by consultation with a senior surgeon (Pavone V). Table 1 presents a risk of bias summary including checklist items with low risk (+), high risk (-), or unclear risk (?). The forms were compared and discussed for final consensus (Table 2).
| Ref. | Patients (mean age) | AR type | Assessment | Results | Complications | Limits |
| Ruiz-Picazo et al[8], 2019 | 16 (32 FFF), 9 yr (range: 7-11 yr). | Subtalar device. Titanium self-locking device. | OxAFQ-C pre- and postoperatively. | Postoperative results were positive, with statistical significance for the “school and play”, “emotional”, and “footwear” domains of the OxAFQ-C scale (P < 0.05) and no differences in the “physical” domain. | 4 (25%). 2 extrusion of the implant and 2 overcorrections. | Retrospective nature, no control group, sample size. lack of objectively measurable parameters. |
| Pavone et al[16], 2019 | 105 (174 FFF) (12.6 ± 1.3 yr), mean follow-up 67.5 ± 16.4 mo. | Calcaneo-stop. | BMI-for-age AOFAS, FADI, FADI Sport, and SF-36 at 1 and 3 yr. Variation of the angles measured on X-ray images. | AOFAS, FADI, FADI Sport, and SF-36 scores and radiological assessments improved significantly postoperatively (P = 0.001) and remained stable over time (1 yr: P < 0.001; 5 yr: P < 0.001) in all groups of patients. An increased persistence of pain and/or discomfort in obese patients than in normal weight patients (P = 0.02). | 20 (11.5%) patients. 1 screw loosening (0.6%); 14 transient pain and discomfort at the level of the surgical incision (8%), 2 contractures of the lateral peroneal muscles (1.15%); 3 superficial infections (1.7%). | Retrospective nature, no control group, sample size. lack of objectively measurable parameters. |
| Pavone et al[1], 2018 | 68 (136 FFF) 12.7 yr (9-15 yr), mean follow-up 57.6 mo. | Calcaneo-stop. | AOFAS, Yoo Score, FADI, FADI Sport, OxAFQ-C scores at 1 and 3 yr. variation of the angles measured on X-ray images. | AOFAS (F 2, 201 = 287.51; P < 0.0001), Yoo Score (F 2, 201= 2627.00; P < 0.0001), OxAFQ-C (F2201 = 210.60; P < 0.0001), FADI (F 2, 201 = 372.62; P < 0.0001) and FADI Sport (F 2, 201= 189.32; P < 0.0001). Radiological assessments improved (P < 0.0001). | 17 (12.5%); 5 pain at surgical scar (3.7%), 4 local symptoms at the incision (2.9%), 3 screw loosening (1.2%) and 4 superficial Infections (2.9%); 1 screw breakage (0.73). | Retrospective study. No control group. Mid-term follow-up. Lack of objectively measurable parameters. |
| Memeo et al[26], 2019 | 202 FFF, 13.6 yr (8-16 yr). Median follow-up was 130 mo (35-150 mo). | Calcaneo-stop. | Clinical evaluation, pain, and variation of the angles measured on X-ray images. | 92% Percutaneous lengthening of the Achilles tendon. Improvement of clinical outcome, restoration of the medial arch and the hind foot valgus in orthostasis. | 32 (15.8%): 23 (11.4%) incomplete correction; 9 (4.5%) screw breakages. | Retrospective study. No control group. Short-term follow-up. Lack of objectively measurable parameters. |
| Memeo et al[26], 2019 | 200 FFF, 12.8 yr (8 to 16 yr). Median follow-up 130 mo (35-150 mo). | Subtalar AR bioabsorbable device. | Clinical evaluation, pain, and variation of the angles measured on X-ray images. | 71% Percutaneous lengthening of the Achilles tendon. Improvement of clinical outcome, restoration of the medial arch and the hind foot valgus in orthostasis. | 25 (12.5%): 20 (10%) inflammatory process involving soft tissues around tarsal sinus; 5 (2.5%) device. removals and substitutes. | Retrospective study. No control group. Mid-term follow-up. Lack of objectively measurable parameters. |
| Megremis et al[18], 2019 | 14 (28 FFF), 10.71 ± 1.58 yr (range 8-14 yr). Mean follow-up duration of 35.14 ± 9.82 mo (19-60 mo). | Subtalar AR. | AOFAS pre- and postoperatively. | The mean postoperative AOFAS score was 88.851 (range 83-97) points (P < 0.0001). | No complication. | Retrospective study. No control group. Short-term follow-up. Lack of objectively measurable parameters. |
| Martinelli et al[14], 2018 | 49 (98 FFF) 10.7 yr (7-14 yr), mean follow-up 4.9 yr. | Subtalar AR. | CHQCF; OxAFQ pre- and postoperatively. Number of sessions per week. | The mean OxAFQ scores within the ‘Emotional’ (P < 0.05) and ‘footwear’ item (P < 0.05) (children), and in the ‘school and play’ (P < 0.05) and ‘footwear’ item for the parent scale. 44 (89%) parents were satisfied with the surgical procedure. | Three residual pain; 1 residual deformity, and one sport limitation. 3 subtalar implants removed because of pain at the sinus tarsi. | Retrospective nature; as some of the anthropological measures were not obtained before surgery. |
| Kubo et al[20], 2020 | Group A (5-8 yr): 6 (11 FFF) MA 7.4 ± 1.2 yr; Group B (9-12 yr): 33 (63 FFF) MA: 11.2 ± 1.0 yr; Group C (13-15 yr): 11 (21 FFF). MA 13.6 ± 0.7 yr. | Calcaneo-stop. | CP; lat. TCA; a.p. TCA, kite angle; NCI; Meary angle. Bony maturation. | Improvement of radiological assessment in each group (P < 0.05). Best deformity correction when surgery was conducted between 9 and 12 yr, with significant improvement in all measured parameters without secondary deterioration during FU. | No complications. | Retrospective study; no clinical scores. |
| Indino et al[28], 2020 | 56 (112 FFF), 9-14 yr (MA 15.5 ± 1.2 yr), mean follow-up 40.1 ± 23.6 mo. | Subtalar AR. | AOFAS, SEFAS, SF-12. | AOFAS 97.3 ± 4.5, SEFAS 47.2 ± 1.5, SF-12.MCS 51.1 ± 8.8, SF-12.PCS 55.6 ± 9.1, Clinical scores were not correlated with the foot radiographic parameters at follow-up period. | No complications. | No preoperative clinical or functional scores. |
| Hsieh et al[15], 2019 | 102 (204 FFF) MA 9.1 ± 0.2 yr). | Subtalar AR. | CP; lat. TCA; a.p. TCA, kite angle; NCI; Meary angle. | 22 cases of bilateral extrusion in the overweight group (39%) vs 13 cases bilateral extrusion in the low body weight group (23%) (P = 0.0004). The inter-observer correlation was 0.95. Improvement of radiological assessment at 3 mo postoperative follow-up (P < 0.05). | 19%. | Retrospective nature, no control group, sample size. lack of objectively measurable parameters. No BMI loss evaluation surgical outcomes. |
| Hagen et al[32], 2019 | 7 (13 FFF), MA 12.43 ± 1.27 yr. | Calcaneo-stop. | Pedobarographic measurements before surgery, 3, 14, 28 d after. | The ground force increased significantly in lateral foot areas (P < 0.001) and decreased in medial areas (P < 0.001). | 1 minor soreness. | Sample size, short follow-up. |
| Hagen et al[31], 2020 | 14 (27 FFF), MA 12.4 ± 1.4 yr. | Calcaneo-stop. | Heel angle, rearfoot angle, leg axis angle, step length, and walking speed, pre- and postoperatively. | Heel valgus (F 1, 24 = 110.465, P < 0.001); Dynamic heel angles vs static heel angles (F 1, 24 = 38.498, P < 0.001). Correlation between heel angle and rearfoot angle (static: r = 0.647, P < 0.001; dynamic: r = 0.640, P = 0.001). Dynamic rearfoot angle vs static rearfoot angle (F 1, 24 = 166.55, P < 0.001). | No complications. | Small size. No clinical assessment. |
| Giannini et al[21], 2017 | 44 (88 FFF). MA 11.7 yr (8-14 yr). | Bioabsorbable Calcaneo-stop. | Patient satisfaction; Meary angle; talocalcaneal angle. | 33 excellent, 9 good outcome, and 2 poor clinical. Meary’s, talocalcaneal angle had improved (P < 0.001). | 2 breakages. | Retrospective nature, no control group, sample size. lack of objectively measurable parameters. |
| Faldini et al[24], 2018 | 173 (283 FFF), MA 11.2 yr. MF 49.5 mo. | Bioabsorbable Calcaneo-stop. | FFI, SEFAS. | FFI score 4; SEFAS score 47.2, well into the normal range. No statistically significant differences between males and females (P value > 0.05). | 3 implant breakages, 1 persistent pain secondary to a local inflammatory response. | No radiological assessment. No control group. |
| Caravaggi et al[33], 2018 | 13 (26 FFF), MA 11.3 ± 1.6 yr, MF 1 yr (12.5 ± 3.7 mo). | Endo-orthotic implant and Calcaneo-stop. | A 10-point VAS, Kinematic and kinetic analysis during normal walking, radiological parameters. | All radiological parameters and VAS were significantly improved at 1-yr follow-up (P < 0.001). No significant differences were detected in spatiotemporal and ground-reaction-force parameters between pre-op evaluation and control in either implant groups. | No complications. | Multisegment foot protocol. Small size. No clinical assessment. |
| Bernasconi et al[27], 2020 | 31 (62 FFF), MA 10.5 ± 1.6 yr, MF 62 ± 15 mo. | Subtalar AR. | ROM; AOFAS; VAS-FA, radiological parameters. | Improvement clinical score and radiological parameters except talonavicular coverage angle (P = 0.49) and calcaneo-fifth metatarsal angle (P = 0.53). Improvement of dorso-plantar view. No loss of correction was found after removal of the implant. | 17 (24%) sinus tarsi syndromes. | Retrospective nature, no control group, sample size. lack of objectively measurable parameters. |
| Elmarghany et al[38], 2020 | 42 (84 FFF); MA 9.92 ± 2.2 yr; range (7-15 yr). MF 29.1 mo. | Calcaneo-stop. | AOFAS; radiological parameters. | Improvement clinical score and radiological parameters (P value < 0.000). | 3 minor complications, 1 (0.02%) under correction. 1 sunken screw. 1 synovits around screw. | Retrospective nature, No control group, sample size. lack of objectively measurable parameters. |
| Ref. | Dutch checklist form for prognosis | ||||
| No participant selection took place | Groups are comparable regarding age | Validated measuring system used | Independent (blind) determination of outcomes | Clear description of groups available | |
| Ruiz-Picazo et al[8], 2019 | + | - | + | ? | + |
| Pavone et al[16], 2019 | + | + | + | - | + |
| Pavone et al[1], 2018 | + | + | + | - | + |
| Memeo et al[26], 2019 | + | + | + | ? | + |
| Megremis et al[18], 2019 | + | - | + | - | + |
| Martinelli et al[14], 2018 | + | ? | + | ? | + |
| Kubo et al[20], 2020 | + | + | + | ? | + |
| Indino et al[28], 2020 | + | - | + | ? | + |
| Hsieh et al[15], 2019 | + | + | + | - | + |
| Hagen et al[32], 2019 | + | + | + | ? | + |
| Hagen et al[31], 2020 | + | + | + | ? | + |
| Giannini et al[21], 2017 | + | + | + | ? | + |
| Faldini et al[24], 2018 | + | + | + | - | + |
| Caravaggi et al[33], 2018 | + | + | + | - | + |
| Bernasconi et al[27], 2020 | + | + | + | ? | + |
| Elmarghany et al[38], 2020 | + | + | + | - | + |
For each included article, a standard data entry form was used to extract the number of patients, number of feet treated, affected side, sex, patient age when treated, type of procedure with or without additional surgeries, number of successes and failures, period of the study, and implant materials. We considered improvement of the medial arch, hindfoot valgus, radiological evaluation, pedobarographic measurements, and functional outcome as indicators of treatment success. The assessment included: (1) The American Orthopedic Foot and Ankle Society (AOFAS) Ankle–Hindfoot score; (2) The Oxford Ankle Foot Questionnaire for Children; (3) The Foot and Ankle Disability Index (FADI); (4) FADI Sport scores; (5) The Foot Function Index Questionnaire; (6) The self-reported Foot and Ankle Score; and (7) Visual Analogue Score. Major and minor complications included screw device loosening, transient pain and discomfort at the level of the surgical incision, contracture of the lateral peroneal muscles, and superficial infection.
A total of 47 articles were retrieved, 34 duplicate publications were excluded, and after the first screening following the previously described selection criteria, 22 were eligible for full-text evaluation. After full-text evaluation, and reference list checking, we selected 17 articles for inclusion (Table 1). The Preferred Reporting Items for Systematic Reviews and Meta-Anal (PRISMA)[12] flowchart of selection and screening is shown in Figure 1. A total of 1864 FFFs were treated In the 17 studies. Eight (762 FFFs) evaluated subtalar AR (47.1%) and nine (1102 FFFs) evaluated CS devices (52.9%). At start of treatment, the average age of patients was 11.8 years, the average follow-up was 71.9 mo (range 29.1-130), and complications occurred in 153 of the 1864 FFF treated, a rate of 8.2% (Table 1).
Eight studies evaluated subtalar AR in a total of 762 FFFs. The average age of patients at the start of treatment was 11.6 years (range 7 to 16 years) and the average follow-up of the studies was 68.9 mo. Every study reported statistically significant differences between pre- and postoperative assessments of pain, clinical scores, or parent and patient satisfaction (P values of 0.001 to 0.05). Radiological measurements showed improvement in every trial (P values of 0.001 to 0.05).
Nine articles evaluated CS in a total of 1102 FFFs. The average age of patients at the start of treatment was 12.0 years (range 7 to 17 years) and the average follow-up of the studies was 70.9 mo. As with subtalar AR Every study reported statistically significant differences between pre- and postoperative assessments of pain, clinical scores, or parent and patient satisfaction (P values of 0.001 to 0.05). Radiological measurements showed improvement in every trial (P values of 0.001 to 0.05). The clinical and radiological characteristics are summarized in Table 1.
Two articles investigated sport activities in FFF patients. In Martinelli et al[14]’s, 49 patients (98 FFFs) underwent to clinical and radiological evaluation after subtalar AR implant. Despite improvements in the emotional, school and play, and footwear (P < 0.05) items of the OxAFQ, the authors did not find any increase sport ability (P > 0.05). On the other hand, Pavone et al[1]. evaluated 68 CS-treated FFFs and reported improvement of sport activity levels, with patients recovering sports activity within 3 mo of surgery and without limitation in the execution of preferred activities (FADI Sport pre- vs postoperative scores P < 0.005).
Two studies included obese patients. Hsieh et al[15] evaluated 102 (204 FFFs) subtalar AR-treated patients. The study outcome was radiological assessment at 3 mo postoperative follow-up. Significatively differences in implant bilateral extrusion (39% vs 23%) were seen in overweight and normal weight patients, respectively, P = 0.0004). Obese patients treated with CS procedure reported a persistence of foot pain (AOFAS pain domain P < 0.05) at 1 year after the surgery compared with normal weight and overweight subjects[16].
Complications occurred in 74 of the 762 FFFs treated with subtalar AR 9.7% and 79 of 1102 FFFs treated with CS (7.2%). The complications in subtalar AR patients included tarsi pain in 40 patients, and under- or overcorrection in four patients. The complications in CS patients included incomplete correction of the deformity in 24 and transient pain or discomfort at the incision site in 20 patients.
Fourteen studies evaluated nonabsorbable implants, seven were CS studies, and seven were subtalar AR studies. Four investigated bioabsorbable implants, three CS screws and one subtalar AR).
AR procedures were found to simple, reliable, and minimally invasive interventions for the treatment of pediatric FFF, allowing the alignment of the talus and calcaneus and restoring a proper foot arch. Both implants improved clinical and radiological outcomes. Despite pain persistence for 1 year following CS treatment, subtalar self-locking is not recommended for obese patients. At the same time, an increase of sport activities was reported after CS implants but no differences were noted after subtalar implant procedures. Complications were reported in 153 of the 1864 FFFs that were treated. To the best of our knowledge, this is the first article investigating the outcomes of AR-treated patients reported in the past 5 years and analyzing CS procedures for impact blocking devices and subtalar AR self-locking implant results separately, including the technique-associated complications in specific populations.
The juvenile and adult surgical indications were not completely defined, and a common consensus was not present among orthopedic surgeons. The principal intervention parameters were age, symptoms including pain while walking or stan
Every study included in this systematic review reported significative improvements of clinical and radiological assessments. Unfortunately, few articles[24,29,30], comparing the self-locking and impact blocking devices, were published in the last 5 years. The articles did not clearly report the exact indication for the implant choice or if the procedures were all performed by the same surgeon. Nevertheless, subtalar AR and CS techniques were found to be similar. Hagen et al[31,32] described an increased ground force in lateral foot areas, a decrease in medial areas, and a correlation between heel angle and rearfoot angle. On the other hand, in Caravaggi et al[33] did not find significant differences in spatiotemporal and ground-reaction-force between preope
The findings related to the return to sport activities after AR implant differed. Patients who underwent CS had improved levels of sport activities without any notable limitation in physical activity[16]. No enhancement of sport activities was found in a subtalar AR study[14]. Pavone et al[16] hypothesized better body aware
Obesity has long been considered a contraindication to AR implant because of excessive stress on the implant[20]. Two studies aimed to investigate the functional and radiological outcomes in overweight and obese patients. Pavone et al[16] reported improvement of clinical and radiological assessments following treatment with CS procedures, even in heavy subjects, despite the persistence of pain for 1 year, compared to nonobese children. The discomfort could be related to the overload of foot structures[16], increased foot pressure with higher peak pressure, and peak force under the midfoot and metatarsal regions[25] during walking and inactivity, which delay the resolution of symptoms in obese children. On the other hand, Hsieh et al[15] noted that subtalar self-blocking implants in overweight patients had an increased possibility of implant extrusion, especially while walking.
Furthermore, a high percentage of satisfaction (78.5% vs 96.4%)[34] with AR procedures, lower risk and complication rates were reported when compared with other procedures. Suh et al[34] reported complication rates of 3.5% to 45% of minor complications in more than 50% of LCL studies. They also reported a 30% rate difference in complications between silicone, polyethylene, staple, titanium, bio
As sinus tarsi pain is the most common complication (54.0%) associated with subtalar self-locking devices[35], with a total of 40 cases (5.2%). It has hypothesized that extrusion and over- or under correction occur because of the difficulty of finding the correct dimension of the implant. Under correction can result from a small device that cannot fully correct excessive subtalar joint eversion, and allow a few degrees of remaining eversion. On the other hand, if the chosen implant size is too large, the subtalar joint motion could be limited, thus resulting in pain or extrusion caused by weight bearing activities. The most frequent complication of CS procedures was the incomplete correction of the deformity (24 cases, 2.2%), transient pain, or discomfort at the incision site (20 patients, 1.8%).
Regarding surgery, no consensus is present about the indications for bioabsorbable, nonabsorbable, or a combination of implant materials[17]. Fourteen studies evaluated nonabsorbable implants (seven CS and 7 subtalar AR studies) and four (three CS[20,24,25], and one subtalar AR[26]) evaluated bioabsorbable implants. Both AR categories were found to result in improvement of clinical and radiological outcome measure
Surgeon experience, implant costs, and cosmetic correction are the most common considerations in the orthopedic decision-making process. The CS procedure is less expensive surgery, compared with any of the other implants[16,17]. Moreover, Ortiz et al[19] noted that, in selected patients, tarsal canal implants produced better cosmetic corrections compared with the CS technique.
Few high-quality studies AR studies have been published. To the best of our knowledge, two systematic reviews and one meta-analysis were previously published. Baryeh et al[36] reported partially conclusive data supporting the subtalar AR as an adjunct treatment, but the analysis was limited to adult acquired flatfoot. Suh et al[34] performed a comparison between AR and the LCL procedures and concluded that LCL achieved more radiographic corrections and more improvements in the AOFAS score than the AR. Complications were more common in the LCL group than in the AR group, and the reoperation rates in the two groups were similar. As reported in a recent European Pediatric Orthopedic Society flatfoot survey[3], the procedure indications are different. At the same time, the survey included dated findings regarding AR complications and first AR devices. A meta-analysis by Hsieh et al[37] in 2020 did not find a superiority between subtalar AR and CS procedures according to the clinical score, but endosinotarsal devices showed a better improvement in Meary’s angle than exosinotarsal screws. Despite the remarkable conclusion, some concerns were present, for example, the authors chose the AOFAS score for the clinical assessment and Meary’s angle for the radiological evaluation. Neither measurement is specific for juvenile FFF, moreover in the few studies included in the meta-analysis, the assessments were not the primary study outcomes and were supplemented with other measurements. In addition differences in study design made group comparability difficult in some cases.
The strength of this study is the reporting of the most important evidence published in the last 5 years. Major limitations include great heterogeneity of the outcome assessments and the lack of high-profile studies. We extensively searched and identified all relevant investigations of FFF treated with AR devices. Therefore, risk of bias assessment had moderate overall risk of influencing our analysis. Statistical analysis was not performed. Variations in clinical and radiological scores were reported in the selected studies. Often more than one measurement was performed in order to evaluate different disease features. Moreover, no FFF-specific scores or X-ray lines were developed, and randomized clinical trials are missing and few were case-control studies. In our opinion, the analysis of partial or not high-quality study data could be misleading.
In conclusion, despite both AR procedures being valid surgical techniques for the treatment of FFF, surgeon experience, implant cost, and cosmetic correction are the most common considerations in the orthopedic decision-making process and AR choice. In obese patients, subtalar ARs are not recommended. In adolescents who need to improve sports performance, CS screws had a slightly lower rate of complications than subtalar self-locking implants.
Flexible flatfoot (FFF) is a common disorder during childhood. When symptoms of early and easy fatigue during walking or pain are present, treatment is mandatory. Arthoereisis (AR) is frequently used for surgical management. Two device types were described, subtalar AR and calcaneo-stop (CS).
No common consensus or AR among orthopedic surgeons is present.
The aim of the study was to report the clinical and radiological outcomes after subtalar AR and CS procedures, including the results in obese and athlete populations, and the technique-related complications. Moreover, the intent was to include the more recent findings of the material devices.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used to perform a systematic review of English-language articles published of the last 5 years.
Seventeen articles were included in the study after the initial screening and the risk of bias assessment. A total of 1864 FFFs were identified. Eight studies evaluated subtalar AR and nine evaluated CS (52.9%). At the start of treatment, the average age of patients was 11.8 years and the average study follow-up was 71.9 mo.
Both AR procedures are valid surgical techniques for FFF treatment, surgeon experience, implant cost, and cosmetic correction were the most common considerations in the orthopedic decision-making process and AR choice. In obese patients, the subtalar AR is not recommended. In adolescents who need to improve sports performance, the CS screw had better results compared with other implants. In adolescents who need to improve sports performance, CS screws had a slightly lower rate of complications than subtalar self-locking implants.
High-quality randomized clinical trials are needed.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Mazzotti A, Trisolino G S-Editor: Gao CC L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Pavone V, Vescio A, Di Silvestri CA, Andreacchio A, Sessa G, Testa G. Outcomes of the calcaneo-stop procedure for the treatment of juvenile flatfoot in young athletes. J Child Orthop. 2018;12:582-589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Vulcano E, Maccario C, Myerson MS. How to approach the pediatric flatfoot. World J Orthop. 2016;7:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (2)] |
| 3. | Pavone V, Testa G, Vescio A, Wirth T, Andreacchio A, Accadbled F, Canavese F. Diagnosis and treatment of flexible flatfoot: results of 2019 flexible flatfoot survey from the European Paediatric Orthopedic Society. J Pediatr Orthop B. 2020;Publish Ahead of Print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Chambers EF. An operation for the correction of flexible flat feet of adolescents. West J Surg Obstet Gynecol. 1946;54:77-86. [PubMed] |
| 5. | LeLièvre J. Current concepts and correction in the valgus foot. Clin Orthop Relat Res. 1970;70:43-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | De Pellegrin M. [Subtalar screw-arthroereisis for correction of flat foot in children]. Orthopade. 2005;34:941-953, quiz 954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Viladot A. Surgical treatment of the child's flatfoot. Clin Orthop Relat Res. 1992;34-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Ruiz-Picazo D, Jiménez-Ortega P, Doñate-Pérez F, Gaspar-Aparicio N, García-Martín V, Ramírez-Villaescusa J, Losa-Palacios S. Radiographic and Functional Results following Subtalar Arthroereisis in Pediatric Flexible Flatfoot. Adv Orthop. 2019;2019:5061934. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Roth S, Sestan B, Tudor A, Ostojic Z, Sasso A, Durbesic A. Minimally invasive calcaneo-stop method for idiopathic, flexible pes planovalgus in children. Foot Ankle Int. 2007;28:991-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Usuelli FG, Montrasio UA. The calcaneo-stop procedure. Foot Ankle Clin. 2012;17:183-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Bernasconi A, Lintz F, Sadile F. The role of arthroereisis of the subtalar joint for flatfoot in children and adults. EFORT Open Rev. 2017;2:438-446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 12. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47187] [Article Influence: 2949.2] [Reference Citation Analysis (0)] |
| 13. | Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 6.0. [July 2019]. In: The Cochrane Collaboration [Internet]. Available from: https://training.cochrane.org/handbook/archive/v6. |
| 14. | Martinelli N, Bianchi A, Martinkevich P, Sartorelli E, Romeo G, Bonifacini C, Malerba F. Return to sport activities after subtalar arthroereisis for correction of pediatric flexible flatfoot. J Pediatr Orthop B. 2018;27:82-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Hsieh CH, Lee CC, Tseng TH, Wu KW, Chang JF, Wang TM. Body Weight Effects on Extra-Osseous Subtalar Arthroereisis. J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Pavone V, Vescio A, Canavese F, Costa D, Sessa G, Testa G. Effects of body weight on the clinical and radiological outcomes of children with flexible flatfeet managed with the 'calcaneo-stop' procedure. J Pediatr Orthop B. 2019;28:228-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Highlander P, Sung W, Weil L Jr. Subtalar arthroereisis. Clin Podiatr Med Surg. 2011;28:745-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Megremis P, Megremis O. Arthroereisis for Symptomatic Flexible Flatfoot Deformity in Young Children: Radiological Assessment and Short-Term Follow-Up. J Foot Ankle Surg. 2019;58:904-915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Ortiz CA, Wagner E, Wagner P. Arthroereisis: What Have We Learned? Foot Ankle Clin. 2018;23:415-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Kubo H, Lipp C, Hufeland M, Ruppert M, Westhoff B, Krauspe R, Pilge H. Outcome after subtalar screw arthroereisis in children with flexible flatfoot depends on time of treatment: Midterm results of 95 cases. J Orthop Sci. 2020;25:497-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Giannini S, Cadossi M, Mazzotti A, Persiani V, Tedesco G, Romagnoli M, Faldini C. Bioabsorbable Calcaneo-Stop Implant for the Treatment of Flexible Flatfoot: A Retrospective Cohort Study at a Minimum Follow-Up of 4 Years. J Foot Ankle Surg. 2017;56:776-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 22. | Yan SH, Zhang K, Tan GQ, Yang J, Liu ZC. Effects of obesity on dynamic plantar pressure distribution in Chinese prepubescent children during walking. Gait Posture. 2013;37:37-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Cousins SD, Morrison SC, Drechsler WI. Foot loading patterns in normal weight, overweight and obese children aged 7 to 11 years. J Foot Ankle Res. 2013;6:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Faldini C, Mazzotti A, Panciera A, Perna F, Stefanini N, Giannini S. Bioabsorbable implants for subtalar arthroereisis in pediatric flatfoot. Musculoskelet Surg. 2018;102:11-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Faldini C, Mazzotti A, Panciera A, Persiani V, Pardo F, Perna F, Giannini S. Patient-perceived outcomes after subtalar arthroereisis with bioabsorbable implants for flexible flatfoot in growing age: a 4-year follow-up study. Eur J Orthop Surg Traumatol. 2018;28:707-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Memeo A, Verdoni F, Rossi L, Ferrari E, Panuccio E, Pedretti L. Flexible Juvenile Flat Foot Surgical Correction: A Comparison Between Two Techniques After Ten Years' Experience. J Foot Ankle Surg. 2019;58:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 27. | Bernasconi A, Iervolino C, D'Alterio R, Lintz F, Patel S, Sadile F. Midterm assessment of subtalar arthroereisis for correction of flexible flatfeet in children. Orthop Traumatol Surg Res. 2020;106:185-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Indino C, Villafañe JH, D'Ambrosi R, Manzi L, Maccario C, Berjano P, Usuelli FG. Effectiveness of subtalar arthroereisis with endorthesis for pediatric flexible flat foot: a retrospective cross-sectional study with final follow up at skeletal maturity. Foot Ankle Surg. 2020;26:98-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 29. | Baker JR, Klein EE, Weil L Jr, Weil LS Sr, Knight JM. Retrospective analysis of the survivability of absorbable vs nonabsorbable subtalar joint arthroereisis implants. Foot Ankle Spec. 2013;6:36-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Shah NS, Needleman RL, Bokhari O, Buzas D. 2013 Subtalar Arthroereisis Survey: The Current Practice Patterns of Members of the AOFAS. Foot Ankle Spec. 2015;8:180-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 31. | Hagen L, Pape JP, Kostakev M, Peterlein CD. Pedobarographic changes during first month after subtalar extra-articular screw arthroereisis (SESA) operation of juvenile flexible flatfoot. Arch Orthop Trauma Surg. 2020;140:313-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 32. | Hagen L, Kostakev M, Pape JP, Peterlein CD. Are there benefits of a 2D gait analysis in the evaluation of the subtalar extra-articular screw arthroereisis? Clin Biomech (Bristol, Avon). 2019;63:73-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | Caravaggi P, Lullini G, Berti L, Giannini S, Leardini A. Functional evaluation of bilateral subtalar arthroereisis for the correction of flexible flatfoot in children: 1-year follow-up. Gait Posture. 2018;64:152-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 34. | Suh DH, Park JH, Lee SH, Kim HJ, Park YH, Jang WY, Baek JH, Sung HJ, Choi GW. Lateral column lengthening vs subtalar arthroereisis for paediatric flatfeet: a systematic review. Int Orthop. 2019;43:1179-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 35. | Tan JHI, Tan SHS, Lim AKS, Hui JH. The outcomes of subtalar arthroereisis in pes planus: a systemic review and meta-analysis. Arch Orthop Trauma Surg. 2021;141:761-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 36. | Baryeh KW, Ismail H, Sobti A, Harb Z. Outcomes Following the Use of Subtalar Arthroereisis in the Correction of Adult Acquired Flatfoot: A Systematic Review. Foot Ankle Spec. 2021;1938640020987775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 37. | Hsieh CH, Lee CC, Tseng TH, Wu KW, Chang JF, Wang TM. Endosinotarsal device exerts a better postoperative correction in Meary's angle than exosinotarsal screw from a meta-analysis in pediatric flatfoot. Sci Rep. 2020;10:13532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 38. | Elmarghany M, Abd El-Ghaffar TM, Elgeushy A, Elzahed E, Hasanin Y, Knörr J. Is subtalar extra articular screw arthroereisis (SESA) reducing pain and restoring medial longitudinal arch in children with flexible flat foot? J Orthop. 2020;20:147-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |