Published online May 18, 2021. doi: 10.5312/wjo.v12.i5.338
Peer-review started: March 5, 2021
First decision: March 31, 2021
Revised: April 12, 2021
Accepted: April 23, 2021
Article in press: April 23, 2021
Published online: May 18, 2021
Processing time: 68 Days and 5.6 Hours
Recently, medical three-dimensional printing technology (3DPT) has demonstrated potential benefits for the treatment of cubitus varus deformity (CVD) by improving accuracy of the osteotomy through the use of an osteotomy guide, with or without a patient-mated plate. Here, we present an interesting CVD case, involving a patient who was treated with corrective biplanar chevron osteotomy using an innovative customized osteotomy guide and a newly designed patient-matched monoblock crosslink plate created with 3DPT.
A 32-year-old female presented with a significant CVD from childhood injury. A computer simulation was processed using images from computerized tomography scans of both upper extremities. The biplanar chevron osteotomy was designed to create identical anatomy between the mirror image of the contralateral distal humerus and the osteotomized distal humerus. Next, the customized osteotomy guide and patient-matched monoblock crosslink plate were designed and printed. A simulation osteotomy was created for the real-sized bone model, and the operation was performed using the posterior paratricipital approach with k-wire positioning from the customized osteotomy guide as a predrilled hole for screw fixation to achieve immediate control of the reduction after osteotomy. Our method allowed for successful treatment of the CVD case, significantly improving the patient’s radiographic and clinical outcomes, with satisfactory result.
3DPT-created patient-matched osteotomy guide and instrumentation provides accurate control during CVD correction.
Core Tip: To the best of our knowledge, this case report introduces a new insight for the clinical application of three-dimensional printing technology in the treatment of cubitus varus deformity. Successful outcome of cubitus varus deformity correction is dependent upon precise preoperative planning and the accuracy of osteotomy and fixation. The treatment procedure itself can be performed safely, with high chance of alignment correction by means of three-dimensional printing technology to generate a well-designed customized osteotomy guide and patient-matched plate.
- Citation: Sri-utenchai N, Pengrung N, Srikong K, Puncreobutr C, Lohwongwatana B, Sa-ngasoongsong P. Three-dimensional printing technology for patient-matched instrument in treatment of cubitus varus deformity: A case report. World J Orthop 2021; 12(5): 338-345
- URL: https://www.wjgnet.com/2218-5836/full/v12/i5/338.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i5.338
Cubitus varus deformity (CVD) is the most common late complication after supracondylar fracture of distal humerus in children[1] and, if left un-intervened, results in multiplanar deformity (varus, hyperextension, and rotation)[2]. The current standard treatment for CVD is corrective supracondylar osteotomy of the humerus, using a plethora of surgical correction techniques[3]. However, previous studies have shown that the conventional corrective osteotomy can result in poor functional outcomes-such as, unsatisfactory correction and residual deformity, and lateral condyle prominence with poor cosmetic appearance[4].
Recently, three-dimensional printing technology (3DPT) has been developing and is one the most exciting and fastest growing fields of healthcare due to its excellent accuracy from using preoperative computed tomography (CT) evaluation and advanced computer software, enabling of personalized treatment, having a wide range of potential uses including in the clinical application of orthopaedic surgery[5]. Regards the treatment of cubitus varus deformity, previous studies showed that 3DPT is beneficial for preoperative planning[6], design of individualized surgical guide[7-9], preparation of the prebent plate with real-sized plastic bone model[10], and patient-matched plate[11,12]. However, through our knowledge, the application of 3DPT in the cubitus varus deformity is still limited to design of osteotomy guide for the simple technique as lateral closed wedged osteotomy and mostly fixation with conventional implants.
This study aimed to present a novel surgical technique based on 3DPT applied to a 32-year-old female with CVD via corrective biplanar chevron osteotomy using a 3DPT-generated customized osteotomy guide and patient-matched monoblock crosslink plate.
A 32-year-old female presented to our clinic with deformity of the left elbow that was progressively worsening.
At 7 years of age, the patient had suffered an injury to the left elbow, which had been treated by a nonoperative method. Since then, the patient experienced a progressive gunstock deformity of the left elbow, but without pain, numbness, or weakness in the left upper extremity.
The patient had previous good health.
The patient reported that no family member had suffered from this symptom before.
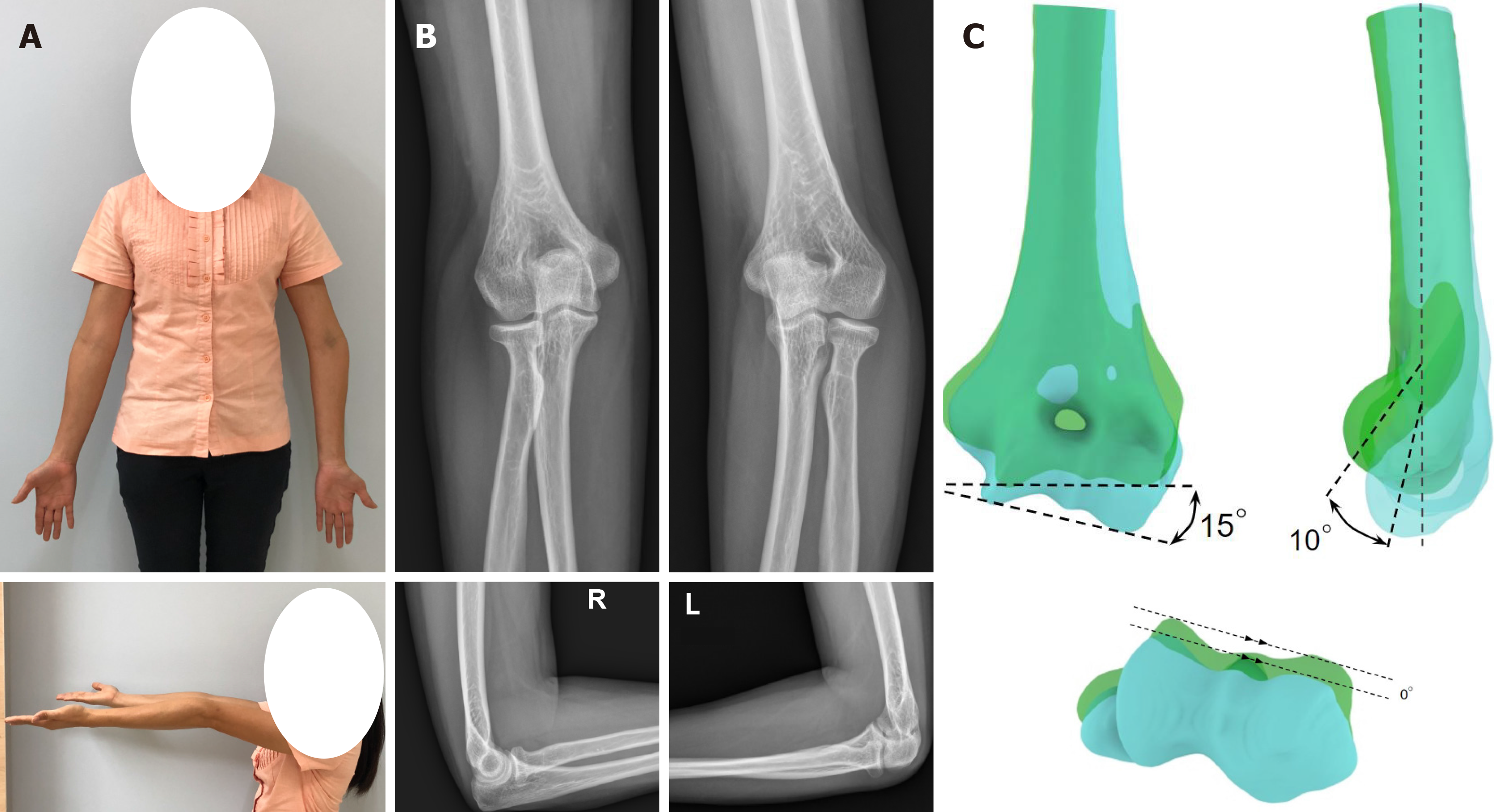
Physical examination showed a 20º varus deformity, with elbow range of motion (ROM) as flexion of 125º, extension of -10º, supination of 85º, and pronation of 80º (Figure 1A). There was no muscle atrophy of the left hand, and the distal neurovascular status of the left upper extremity was intact.
All laboratory tests yielded results within normal range.
Cubitus varus and recurvatum deformity of the distal humerus.
After detailed discussion regarding the treatment option of corrective biplanar chevron osteotomy, an approach was formulated that would involve the use of a 3DPT-generated customized osteotomy guide and an innovative patient-matched monoblock crosslink titanium plate. The customized osteotomy guide was specifically designed to ensure the position of k-wire fixation at the same position of the screw holes on the patient-matched plate. Through these aspects, this specific design was expected to assist the surgeon with bone reduction after osteotomy via application of the plate through the k-wire position, which featured a predrilled hole for screw insertion. Moreover, we also designed the plate configuration as a monoblock crosslink plate, by placing the plate on the medial and posterolateral side of the distal humerus with the built-in metal crosslink between both sides. This plate design was expected to aid in the reduction osteotomy, according to its features of easier and better intraoperative plate position adjustment compared to the conventional dual plating technique. We also intended the crosslink to provide improved biomechanical properties of the plate and stability after fixation, as compared to separate dual plates, as reported for spinal surgery[13]. Therefore, use of the innovative plate design, with its described advantages, and the 3DPT technology for its customized generation would benefit the complex osteotomy operation by reducing operative time related to the bone reduction step and improving accuracy of the osteotomy itself.
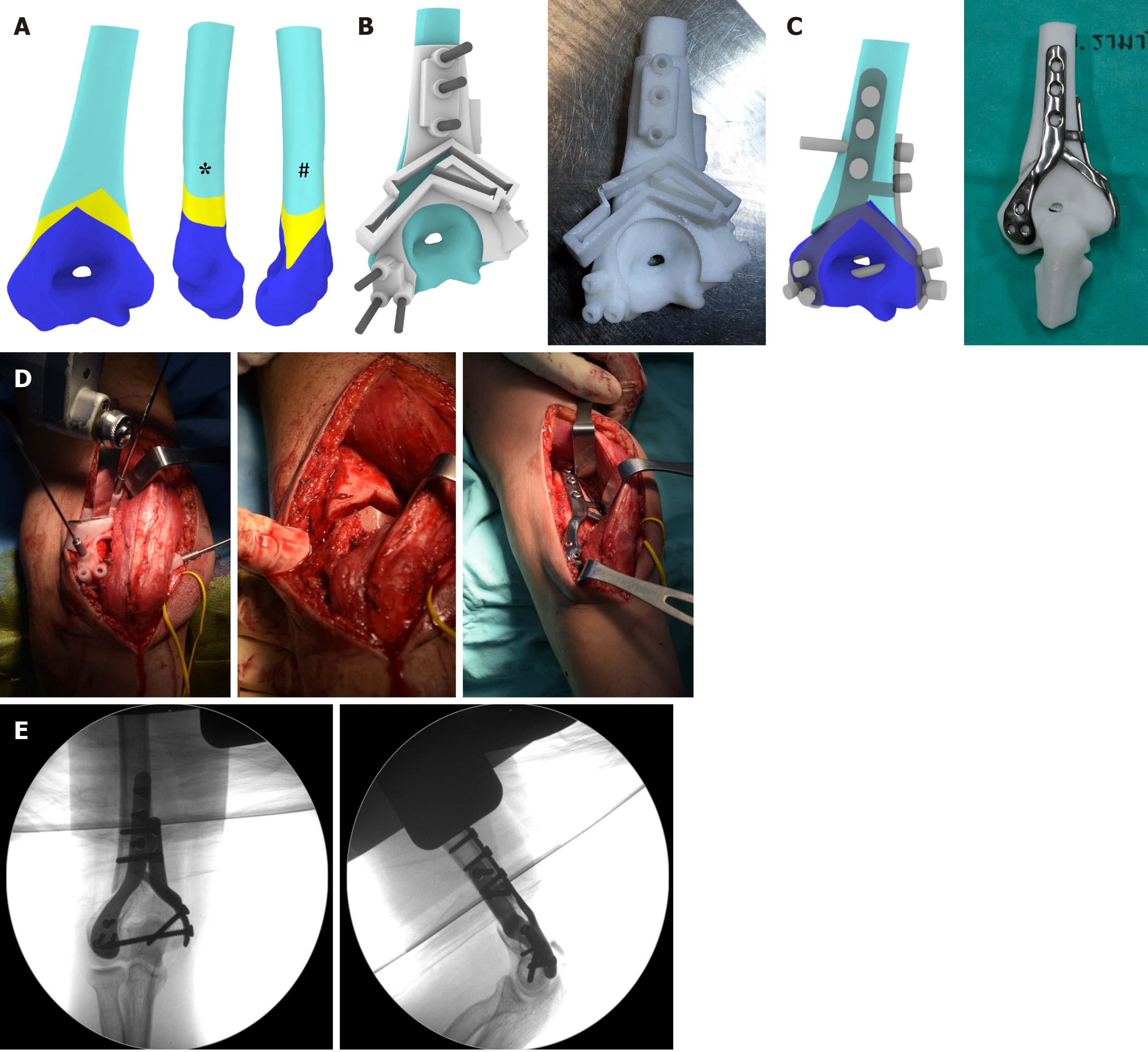
A simulation of the deformity correction was first performed through 3D reconstruction and image processing of DICOM files, taken from CT scans, via Avizo software (Thermo Fisher Scientific, Waltham, MA, United States). A corrective biplanar chevron osteotomy was planned, as illustrated in Figure 2A, to divide the affected bone into three separated fragments. The distal fragment of bone was then reduced to match the mirrored image of the contralateral bone. The designs of the customized osteotomy guide and the patient-matched monoblock crosslink plate were then developed based on the patient’s anatomical bone geometry and the surgeon’s requirements using ANSYS software (Ansys Inc., Canonsburg, PA, United States).
The osteotomy guide was designed to fit over the distal surfaces (posterior, lateral, and medial supracondylar ridge) of the defected bone, excepting the area over the olecranon fossa (Figure 2B). The cutting slots and drilling sleeves were designed to match the cutting planes and the plate’s screw holes, respectively. The patient-specific plate with the monoblock crosslink was designed to fit over the corrected humerus bone, with an overall thickness of 2 mm (Figure 2C). The structural strength of the plate was also confirmed by finite element analysis.
Upon the surgeon’s approval of the design, the patient-specific implant was 3D-printed by selective laser melting using medical grade Ti-6Al-4V alloy (Meticuly Co., Ltd., Bangkok, Thailand). The processing parameters set for the SLM machine (Mlab 200R, Concept Laser GmbH, Germany) were 180 W of laser power and 1250 mm/s of scanning rate. This process was operated under 99.999% Ar atmosphere. Subsequent post-processing techniques, including surface polishing and sterilization, were performed according to routine standards. For osteotomy guides and bone models, fused filament fabrication was used for the 3D printing of biocompatible high-impact polystyrene. The entire fabrication process was certified by the ISO13485 standard for the design, manufacturing, and sterilization of medical devices. Finally, the customized osteotomy guide was printed, and a trial osteotomy was simulated on the real-sized plastic bone model (Figure 2C). The dimensions of the customized osteotomy guide and the patient-specific plate were given in Supplementary Figures 1 and 2.
After administration of combined general anesthesia and an ultrasound-guided supraclavicular nerve block, the patient was placed in the right lateral decubitus position. The operation was performed using a standard posterior paratricipital surgical approach, with a 20-cm posterior midline incision. The triceps muscle was exposed and elevated from the posterior surface of the distal humerus, and then the ulnar nerve was identified. The customized osteotomy guide was placed and fixed with multiple K-wires. After complete osteotomy, the guide and bone blocks were removed, and the plate was inserted under the triceps using the screw fixation based on the predrilled screw holes (Figure 2D).
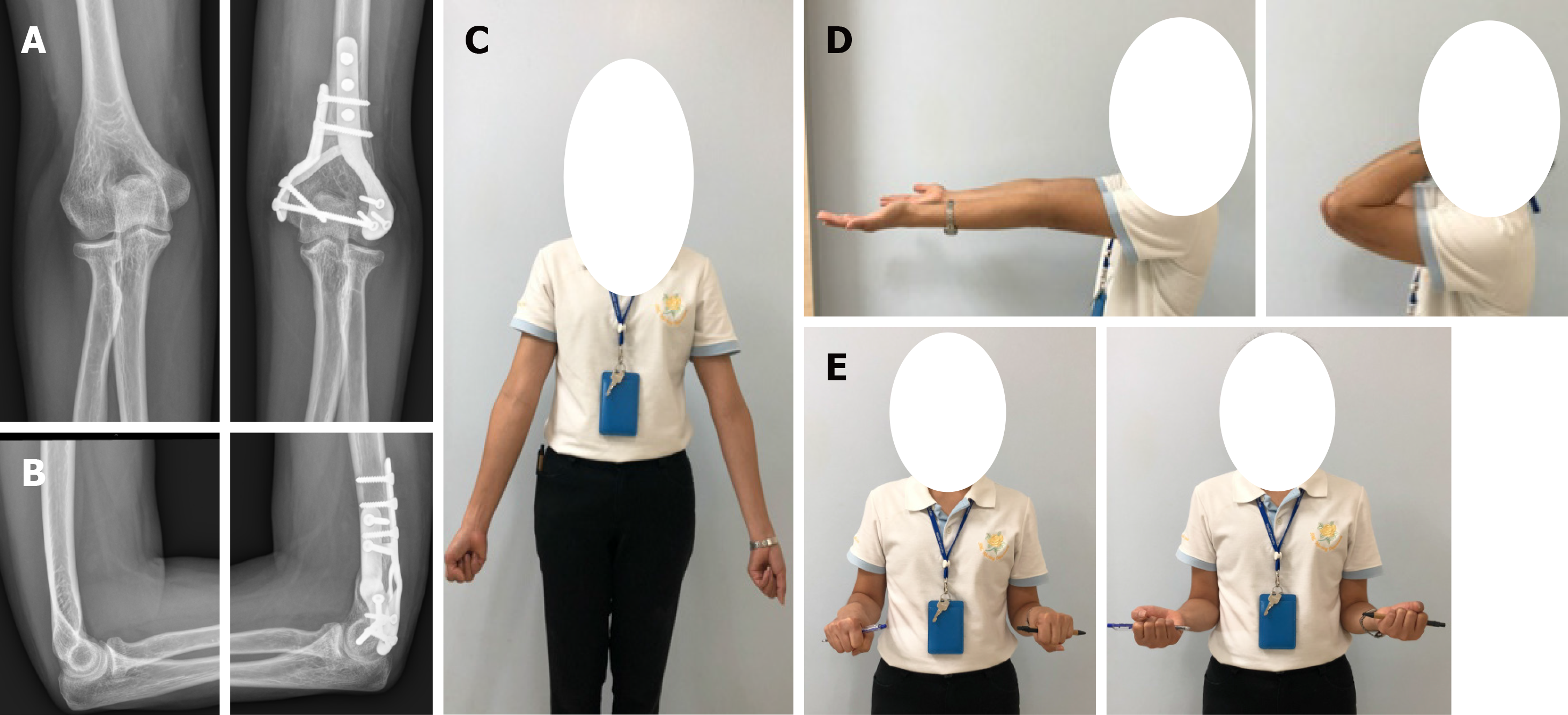
The intraoperative flexion/extension ROM was 135º/0º. The intraoperative fluoroscopic images were checked to confirm the post-reduction alignment (Figure 2E) before wound closure (without nerve transposition). The total operative time was 116 min. The initial postoperative radiographs showed good alignment and adequate fixation stability in both antero-posterior and lateral views.
After surgery, the patient was immobilized with an arm sling for 6 wk and was allowed to perform active assisted-ROM exercises of the wrist, elbow, and shoulder joints, as tolerated. During admission, she reported only minimal pain on motion, with mild paresthesia affecting the ulnar side of the left hand. She was discharged from the hospital 3 d postoperative and was scheduled for follow-up visits at the orthopedic clinic.
At first follow-up, the clinical examination showed nearly normal alignment of the left elbow (compared to the right side). Normal sensation had completely returned by 6 wk postoperative, and the flexion/extension and pronation/supination ROMs of the left elbow were 130º/0º and 90º/90º respectively. The osteotomy healed uneventfully by 3 mo postoperative. The postoperative radiographs demonstrated improved humerus-elbow-wrist angle, from 15º varus to 7º valgus (compared to 8º valgus on the right side) (Figure 3). At the last follow-up visit, at 18 mo postoperative, the patient reported being highly satisfied with the clinical outcome and did not report feeling any pain, swelling, or implant irritation. Therefore, we did not advise removal of the implant in this case.
Medical 3DPT has recently fueled new hope for an effective treatment of CVD. Especially promising is that the technology enables highly accurate control of the plane and the angle of osteotomy, resulting in higher overall operating accuracy and lower risk of complications.
Regarding the development of a customized osteotomy guide for the CVD, Murase et al[14] first reported performing a 3D corrective osteotomy on 22 patients with malunited fractures of the upper extremities (including 4 cases with CVD) by using custom-made osteotomy template and reduction guide on the bone surface of lateral side of distal humerus metaphysis and fix with k-wire. Then the closed wedged osteotomy was performed by cutting through a slit on the template and using the reduction guide to align the bone. Since then, many researchers have worked towards developing an individualized navigation template for lateral closed-wedge osteotomy to treat CVD, and showed the advantages of this technique as to determine the osteotomy angle, osteotomy plane, and rotational angle[8,11,12,15]. In this study, we innovatively designed a customized osteotomy guide to place on the posterior surface of our patient’s distal humerus, to address the need for a posterior slit for the biplanar chevron osteotomy. Although this design might be larger than the previously mentioned lateral-side template, our customized osteotomy guide provided predrilled holes for medial plate placement, resulting in easier placement of the 3D patient-matched plate in the later steps of the procedure. Moreover, performing the osteotomy through a posterior slit would better minimize the risk of ulnar nerve injury that is faced by osteotomy performed through a lateral slit.
Concerning the development of the patient-matched plate for the cubitus varus deformity, there were only two studies by Omori et al[11] in the cadaveric study and Oka et al[12] in the prospective multicenter study. In these studies, both patient-matched plate designs were made from titanium and placing on the lateral side of distal humerus. Although there was no control group in the prospective study by Oka et al[12], they showed that the patient-matched implants resulted in highly accurate correction with an average residual maximal deformity angle of 3.3o and average 3D correction error of < 1.0o and < 1 mm, with high patient satisfaction and no serious complication[12].
Our study has some limitations that must be considered when interpreting our results. First, the present study was based on a single case, without control group patients for comparison. Nonetheless, we believe our method is reliable; our method also showed high accuracy, like the other methods used in previous studies. Second, due to the osteotomy and implant design, our method requires a posterior paratricipital approach, to provide for a medial and lateral soft tissue window and elevation of the triceps muscle. However, this posterior approach allows the surgeon to explore and protect the ulnar nerve, making the overall procedure safer for patients with the type of severe and complex anatomy present with CVD. Moreover, the surgical scar on the posterior side resulting from this approach will be more cosmetically acceptable for patients, especially for younger individuals. Lastly, as with previous studies using the 3DPT technology, our method requires patients to be exposed to radiation from the CT scans required for both upper extremities. Additionally, the materials used for patient-specific plate in this study was designed as Ti-6Al-4V alloy as same as the previous studies. Although Ti-6Al-4V alloy is a well-established biomaterial for orthopaedic implant with high biocompatibility and corrosion resistance as same as commercially titanium implants, it can release a very low concentration of potentially toxic metal ions as aluminum and vanadium ions that had been linked to some health problems such as Alzheimer’s disease, neuropathy and osteomalacia with chronic exposure[16]. Therefore, implant removal after fracture healing or long-term follow up for side effect monitoring are necessary.
This study showed that using of 3DPT is an alternative and noteworthy option for achieving satisfactory outcome in the treatment of CVD. We believed that our method to generate a customized osteotomy guide and patient-matched monoblock crosslink plate provides a new insight for accurate control of the deformity correction by improving the accuracy of osteotomy and stability of fixation, and therefore, avoiding a prolonged operative time and unnecessary blood loss, and decreasing the risk of postoperative complications.
The authors wish to thank Biomedical Engineering Research Center, Chulalongkorn University and Faculty of Medicine Ramathibodi Hospital, Mahidol University for all of the kind help and permission to carry out this study.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee T S-Editor: Zhang H L-Editor: A P-Editor: Xing YX
| 1. | Tellisi N, Abusetta G, Day M, Hamid A, Ashammakhi N, Wahab KH. Management of Gartland's type III supracondylar fractures of the humerus in children: the role audit and practice guidelines. Injury. 2004;35:1167-1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Takeyasu Y, Murase T, Miyake J, Oka K, Arimitsu S, Moritomo H, Sugamoto K, Yoshikawa H. Three-dimensional analysis of cubitus varus deformity after supracondylar fractures of the humerus. J Shoulder Elbow Surg. 2011;20:440-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Verka PS, Kejariwal U, Singh B. Management of Cubitus Varus Deformity in Children by Closed Dome Osteotomy. J Clin Diagn Res. 2017;11:RC08-RC12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Kim HT, Lee JS, Yoo CI. Management of cubitus varus and valgus. J Bone Joint Surg Am. 2005;87:771-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Aimar A, Palermo A, Innocenti B. The Role of 3D Printing in Medical Applications: A State of the Art. J Healthc Eng. 2019;2019:5340616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 167] [Cited by in RCA: 265] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 6. | Bovid KM, Kohler EJ, Habeck JM, Gustafson PA. Utilization of a 3D-printed model for preoperative planning and operative osteotomy of a pediatric cubitus varus deformity. JSES Open Access. 2019;3:219-224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Murase T, Takeyasu Y, Oka K, Kataoka T, Tanaka H, Yoshikawa H. Three-Dimensional Corrective Osteotomy for Cubitus Varus Deformity with Use of Custom-Made Surgical Guides. JBJS Essent Surg Tech. 2014;4:e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Vlachopoulos L, Schweizer A, Meyer DC, Gerber C, Fürnstahl P. Three-dimensional corrective osteotomies of complex malunited humeral fractures using patient-specific guides. J Shoulder Elbow Surg. 2016;25:2040-2047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Zhang YZ, Lu S, Chen B, Zhao JM, Liu R, Pei GX. Application of computer-aided design osteotomy template for treatment of cubitus varus deformity in teenagers: a pilot study. J Shoulder Elbow Surg. 2011;20:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Kataoka T, Oka K, Miyake J, Omori S, Tanaka H, Murase T. 3-Dimensional prebent plate fixation in corrective osteotomy of malunited upper extremity fractures using a real-sized plastic bone model prepared by preoperative computer simulation. J Hand Surg Am. 2013;38:909-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Omori S, Murase T, Kataoka T, Kawanishi Y, Oura K, Miyake J, Tanaka H, Yoshikawa H. Three-dimensional corrective osteotomy using a patient-specific osteotomy guide and bone plate based on a computer simulation system: accuracy analysis in a cadaver study. Int J Med Robot. 2014;10:196-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Oka K, Tanaka H, Okada K, Sahara W, Myoui A, Yamada T, Yamamoto M, Kurimoto S, Hirata H, Murase T. Three-Dimensional Corrective Osteotomy for Malunited Fractures of the Upper Extremity Using Patient-Matched Instruments: A Prospective, Multicenter, Open-Label, Single-Arm Trial. J Bone Joint Surg Am. 2019;101:710-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Brodke DS, Bachus KN, Mohr RA, Nguyen BK. Segmental pedicle screw fixation or cross-links in multilevel lumbar constructs. a biomechanical analysis. Spine J. 2001;1:373-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 67] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Murase T, Oka K, Moritomo H, Goto A, Yoshikawa H, Sugamoto K. Three-dimensional corrective osteotomy of malunited fractures of the upper extremity with use of a computer simulation system. J Bone Joint Surg Am. 2008;90:2375-2389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 191] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 15. | Zhang YW, Xiao X, Gao WC, Xiao Y, Zhang SL, Ni WY, Deng L. Efficacy evaluation of three-dimensional printing assisted osteotomy guide plate in accurate osteotomy of adolescent cubitus varus deformity. J Orthop Surg Res. 2019;14:353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Sansone V, Pagani D, Melato M. The effects on bone cells of metal ions released from orthopaedic implants. A review. Clin Cases Miner Bone Metab. 2013;10:34-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 103] [Article Influence: 8.6] [Reference Citation Analysis (0)] |