Published online May 18, 2021. doi: 10.5312/wjo.v12.i5.329
Peer-review started: January 12, 2021
First decision: January 24, 2021
Revised: January 29, 2021
Accepted: March 18, 2021
Article in press: March 18, 2021
Published online: May 18, 2021
Processing time: 119 Days and 18.2 Hours
Talar fractures are exceedingly rare in childhood. There are very few studies on the clinical aspects, the long-term outcomes and the appropriate treatment of these fractures in pediatric patients. The mechanism of trauma consists of the application of a sudden dorsiflexion force on a fully plantar-flexed foot. Traumatic mechanism, symptoms and imaging of injuries of the talar head are similar to transitional fractures that are normally described at the distal epiphysis of the tibia: the so-called transitional fracture is defined as an epiphyseal injury when the growth plate has already started to close.
A thirteen-year-old girl reported a high-energy trauma to her right foot, due to falling from her horse. X-rays at the Emergency Department were negative. Because of persistent pain, the patient was assessed by an orthopedic surgeon after two weeks and computed tomography scans revealed a misdiagnosed displaced shear-type fracture of the talar head. Hence, surgical open reduction and fixation with two headless screws was performed. The girl was assessed regularly, and plain films at follow-up revealed complete healing of the fracture. Within six months after surgery, the patient returned to pre-injury sport activities reporting no complications.
Injuries of the talar head in childhood should be considered as transitional fractures. Open reduction with internal fixation aims to reduce malalignment and osteoarthritis. Computed tomography scans are recommended in these cases.
Core Tip: Fractures of the talar head in childhood must be judged as transitional fractures. These injuries, typically occurring at the distal tibia, are defined as an epiphyseal injury when the growth plate has already started to close. This crucial aspect should be considered by orthopedic surgeons: surgical treatment is preferred in order to reduce malalignment and osteoarthritis.
- Citation: Monestier L, Riva G, Faoro L, Surace MF. Rare shear-type fracture of the talar head in a thirteen-year-old child — Is this a transitional fracture: A case report and review of the literature. World J Orthop 2021; 12(5): 329-337
- URL: https://www.wjgnet.com/2218-5836/full/v12/i5/329.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i5.329
Talar fractures are exceedingly rare in childhood, with an estimated incidence of 0.01%-0.08% among all pediatric fractures[1-6]. This rarity is due to skeletal immaturity making the bone more resistant to bending and torsional forces without subsequent fracture[2,4,5,7-9].
In the talus, the neck is usually involved, followed by the body and the head: the latter is protected by ligaments and capsule of the talar-navicular joint[4,10]. Talar fractures are often related to high-energy trauma (high-altitude fall, sport injuries, car accidents)[8,11,12]. The mechanism of trauma generally consists of the application of a sudden dorsiflexion force on a fully plantar-flexed foot: compressive forces through the talar head result in compression of the talar head against the anterior tibial edge[11]. Participation in high-impact sports may increase the incidence of talus fractures in children[12].
Despite the improvements in surgical procedures, complications of these fractures are extremely frequent: osteonecrosis, post-traumatic osteoarthritis and foot deformity are the most common[3,8,11,13]. In the past, fracture displacement and delayed surgery were considered the main risk factors; thus, immediate open reduction with internal fixation (ORIF) was recommended[14,15]. However, the most recent literature has shown that there is no significant correlation between time of surgery and development of osteonecrosis or osteoar
Relatively little is known about talar injuries in childhood, as there are only a small number of studies in the literature. Due to their rarity, there are very few studies on the clinical aspects, the long-term outcomes, and the appropriate treatment in pediatric patients[18].
Here we report the rare case of a shear-type fracture of the talar head in a female adolescent, initially misdiagnosed in the emergency room.
A 13-year-old female came to the Emergency Department (ASST Settelaghi-Fondazione Macchi, Varese, VA, Italy) with a possible dislocation of the right ankle after a fall from her horse.
At clinical examination, an antero-medial tenderness of the foot, local pain and inability to bear weight on right foot were observed.
Laboratory examinations were normal.
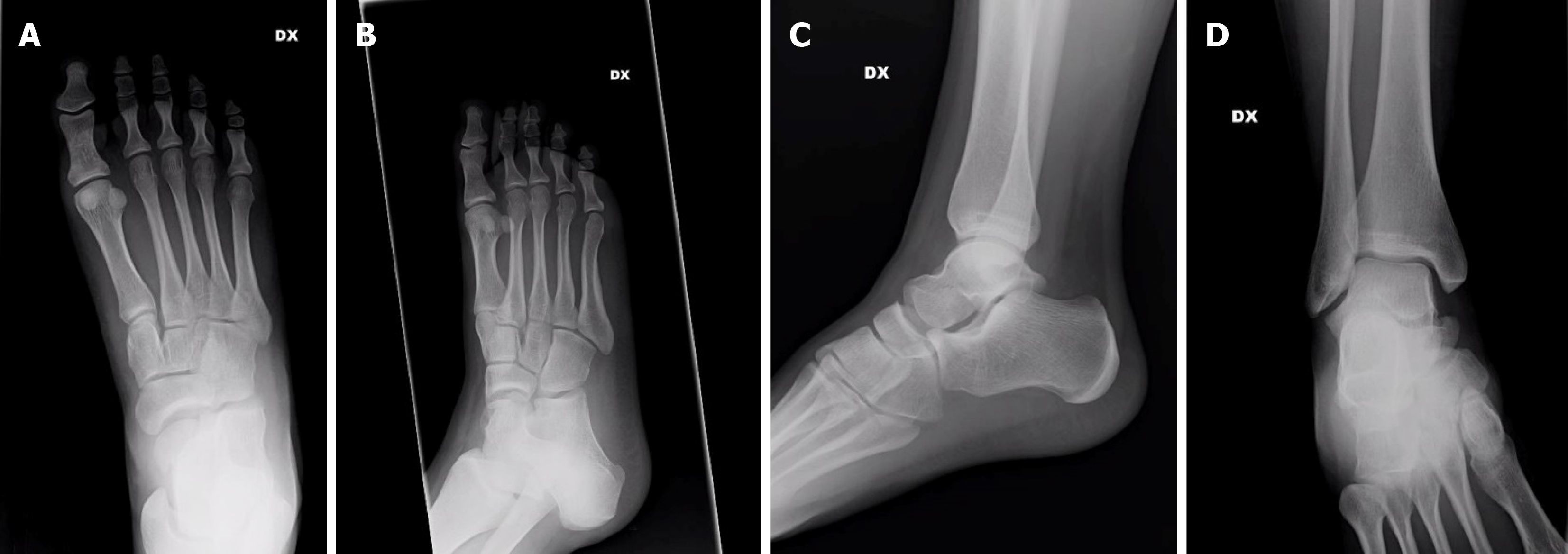
A trauma X-ray series was performed, with no evidence of fractures (Figure 1).
Shear-type fracture of the talar head.
The patient was released from the hospital without evaluation by an orthopedic surgeon and was prescribed rest, no weight-bearing for a week, non-steroidal anti-inflammatory drugs and ice.
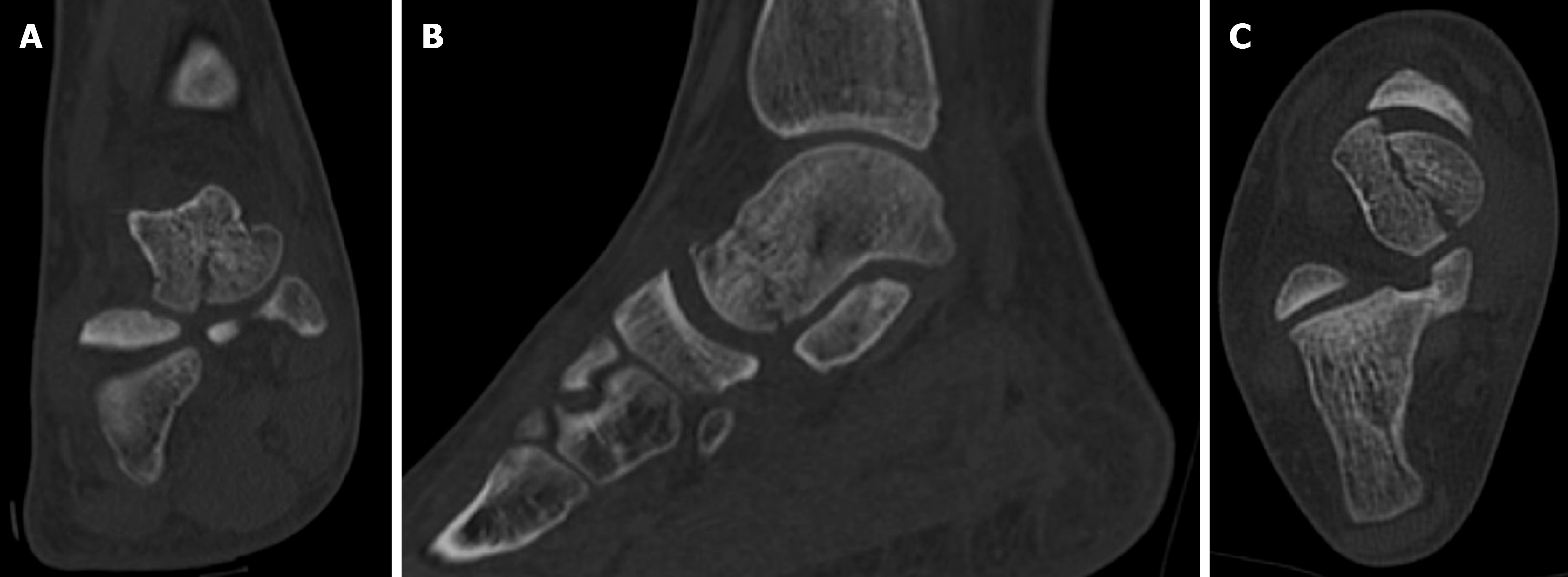
As local pain and inability to weight-bear was protracted with no further trauma, the patient came to our Trauma Unit after fifteen days. Pain at palpation and minimal swelling were found in her right foot. Hence, the orthopedic surgeon requested a computed tomography (CT) scan which revealed a displaced shear-type fracture of the talar head (Figure 2). This fracture was described as type-2, as defined by Canale et al[19].
It was decided to perform ORIF due to displacement and involvement of the articular surface. Surgery was performed two days later (seventeen day after trauma).
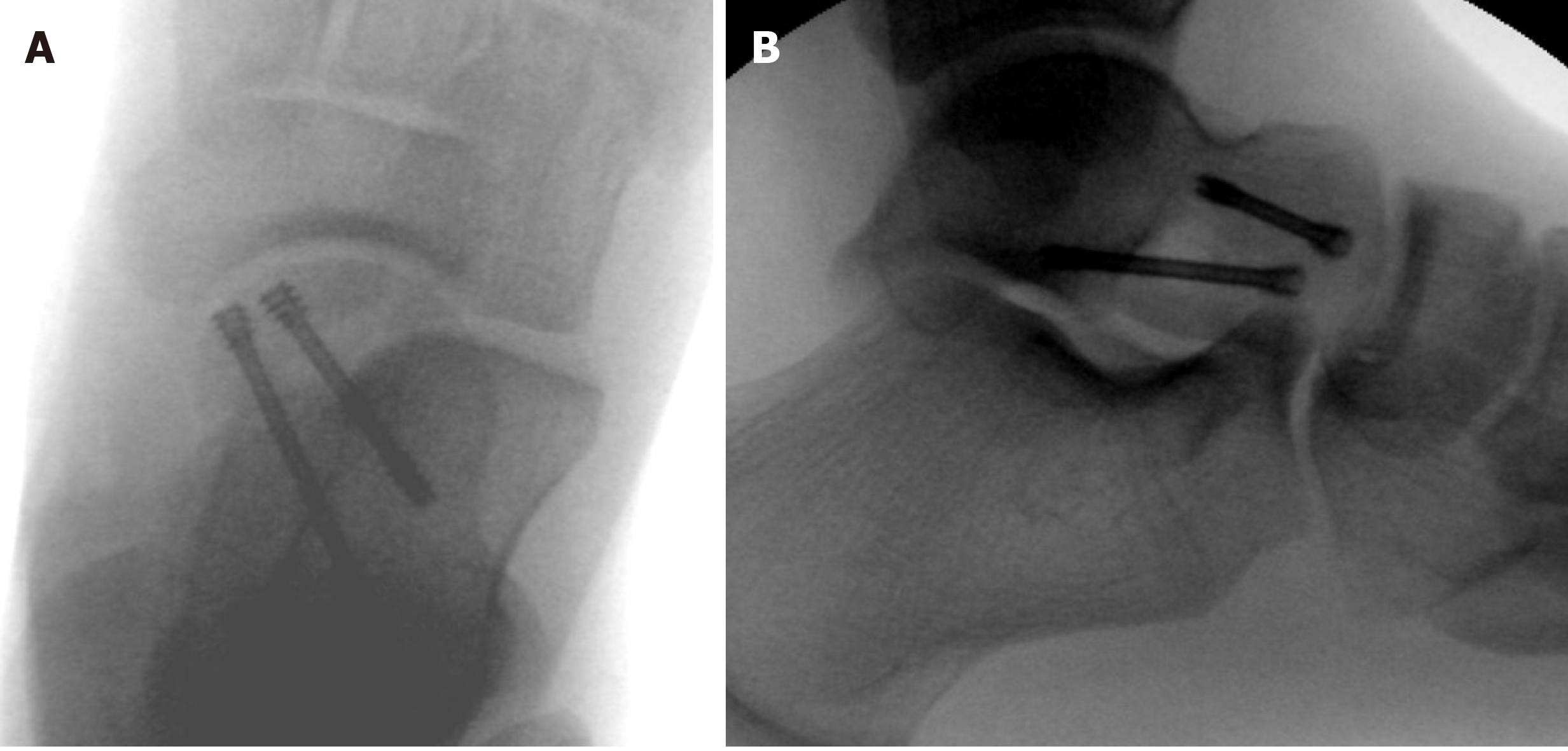
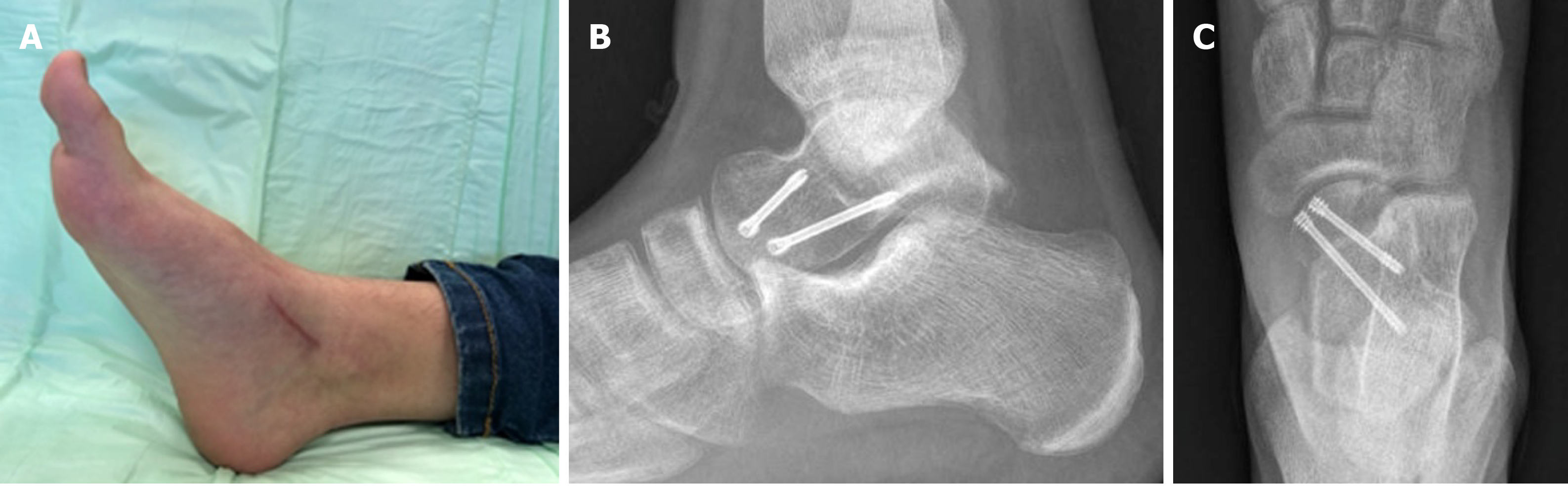
Open reduction was performed through an anteromedial approach and the fracture was fixed using two divergent BSS headless screws (Medartis AG, Basel, Switzerland), favoring compression and avoiding rotation of the fragment (Figure 3).
Postoperatively, the ankle was protected by a below-knee cast and no weight-bearing was allowed. Enoxaparin was prescribed for thromboprophylaxis. Pulsed electromagnetic field therapy was indicated for 4-6 h per day (IGEA Clinical Biophysics, Carpi, Italy).
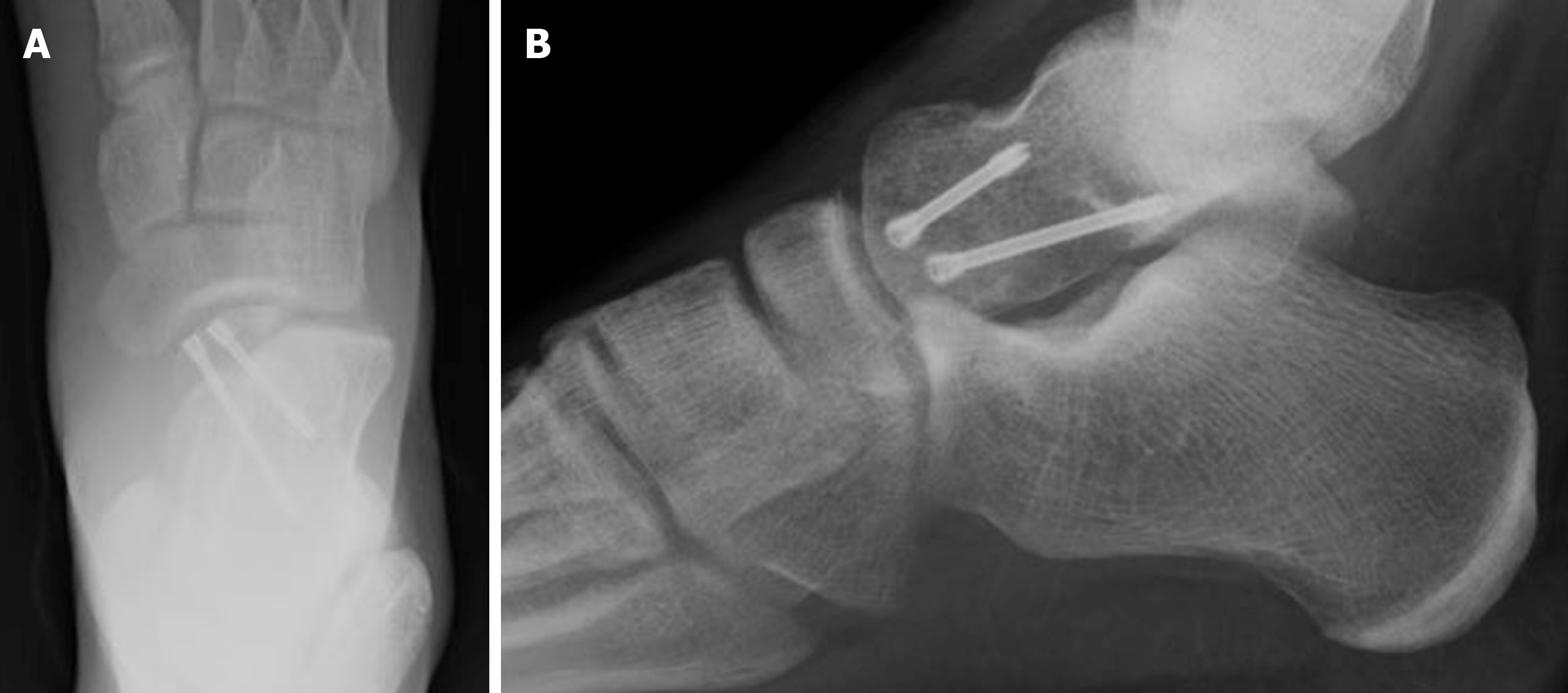
At one-month follow-up, we found no local edema or wound complications, and the patient had minimal pain [(numeric rating scale) NRS = 2]. Plain films revealed initial healing of the fracture (Figure 4). The cast was substituted with a removable air-cushioned ankle orthosis (Bauerfiend© AirLoc) to avoid foot pronation and supination. We believe it was crucial to protect the cartilaginous surface of the talar head. Weight-bearing was not permitted. A rehabilitation protocol was begun with active/passive dorsiflexion and plantarflexion. At six weeks, foot pronation and supination exercises were introduced, as weight off proprioception and exercises in the pool.
At two months follow-up, range of motion was restored without pain (NRS = 0), 50% partial weight-bearing was indicated for two weeks, and then complete weight-bearing as tolerated. A rehabilitation protocol was deployed (Figure 5). Running and atraumatic sport activities were reintroduced at three months.
At six months, the young patient practiced every sport, and specifically horse riding, without any complications (NRS = 0). Range of motion was completely restored, and the patient showed no postoperative foot deformities or neurovascular deficits. Plain films revealed healing of the fracture with no osteonecrosis or osteoarthritis (Figure 6).
Talar fractures are exceedingly rare in childhood with an estimated incidence of 0.01%-0.08%[1-6]. This rarity is due to skeletal immaturity making the bone more resistant to forces without subsequent fracture [2,4,5,7-9].
When comparing children (< 12 years) and adolescents (> 12 years), Ebler reported a higher incidence of talar fractures in the latter, probably due to skeletal development: in younger children, the immature portion of the talus shows more resistance to bending or compressive forces[11]. The severity of these fractures has been demonstrated to be greater in older patients[6,12].
Talar fractures are often related to high-energy trauma (high-altitude falls, sport injuries, car accidents). First described by Anderson in 1919, the mechanism of trauma generally consists of the application of a sudden dorsiflexion resulting in compression of the talar head against the anterior edge of the tibia[18]. This theory was successively confirmed[8,11,12].
The rarity of these fractures in childhood and the difficulty in their diagnosis on plain films often result in misdiagnosis. Our patient was diagnosed after two weeks only because a CT scan was requested due to protracted pain and inability to walk. Hence, we emphasize the importance not only of a careful clinical assessment of the foot and ankle at the Emergency Department, but also of a meticulous examination of the medical history of the patient and of the trauma mechanism. In the case of a pediatric patient with high energy trauma, despite no recognizable fractures on plain films, CT or magnetic resonance imaging (MRI) scans are strongly suggested.
CT scanning has several advantages over MRI: CT is useful for precisely analyzing the degree of injury, specifically articular involvement, and to plan accurate surgical treatment[20]. CT permits rapid acquisition of scans, optimal visual resolution and three dimensional-acquired images. Moreover, sedation and anesthesia are not required. Conversely, MRI eliminates the exposure to radiation in pediatric patients. This issue should not be underestimated as compared to adults, children show more sensitivity of tissues to ionizing radiation and their longer lifetime allows the development of several tumors. For this reason, in the last decades several studies evaluated the effects of exposure to radiation in children, introducing the notion of “as low as reasonably achievable” dose[21-25]. The use of low-dose CT or ultra-low-dose CT, digital acquisition of images and more accurate protective devices have significantly reduced the exposure of pediatric patients to ionizing radiation: with regard to fractures, ultra-low-dose CT has been demonstrated to expose patients to lower doses than plain films[24]. Hence, we strongly believe that a CT scan at the Emergency Department is necessary in the case of high energy trauma involving children. Our statement regarding the necessity of CT scans in pediatric ankle fractures is supported by the literature[26-29].
With regard to the pediatric population, ossification of the talus and the mechanism pattern, an important question emerges: could these injuries be transitional fractures?
Talus development is based on endochondral ossification. The ossific nuclei of the talus compares to the neck during the 26th-28th gestational week. In newborns, up to 24% of the talus consists of bony tissue[30,31]. Frisch described two periosteal collars: the first forms the roof of the sinus tarsi; the second is situated at the top of the ossification center and is covered by a layer of fibrocartilage-like tissue, a layer of dense connective tissue and the synovial membrane of the tibiotalar joint[30]. Complete talar maturity occurs during adolescence (12-22 years). However, because the talus has no epiphysis, it is difficult to determine the maturity of the talus; hence, its development is usually defined by the closure of metatarsals (14-21 years)[32].
The so-called transitional fracture is defined as an epiphyseal injury when the growth plate has already started to close (Figure 7 shows closure of the distal tibial physis). The most involved site is the distal tibia: transitional fracture occurs because of the combination of relative weakness of not yet mineralized epiphyseal areas and the great resistance of mature bone, stabilized by tibiotalar ligaments. The distal epiphysis of the tibia is prone to fracture as it shows a uniform and eccentric closure pattern of the growth plate[33].
Could the fracture of the talar head/neck edge be considered a transitional fracture? Presumably, yes. The mechanism could be compared to that which occurs at the distal tibia. As described above, the enchondral ossification of the talus concludes in adolescence. The weakness of unfused talar areas on the one hand, the increased stability of the already mineralized parts and the strength of the talonavicular joint on the other hand, tend to facilitate fracture at this site when a torsional or compressive force is applied to the foot.
The treatment is conservative for nondisplaced transitional fractures. The tolerance limit is a fracture displacement greater than 2 mm and/or a joint step[33]. The purpose of surgical treatment is anatomical joint reconstruction. Several authors disputed whether an open reduction or percutaneous closed reduction is required[33-35].
With regard to the distal tibia, Schneidmueller et al[33] suggested ORIF should be performed as capsule incision ensures the evacuation of hemarthrosis reducing intraarticular pressure, and permits a direct view of the fracture. Fixation is performed with cannulated screws[33].
The treatment of a transitional fracture aims to reduce complications, physeal malalignment, growth disturbances and post-traumatic osteoarthritis. However, closure of the physeal plate is not sufficient in adolescents to cause significant growth-related problems and ORIF is indicated mostly to reduce articular malalignment leading to osteoarthritis.
These principles can all be applied to fractures of the talar head.
In the present case, we decided to perform ORIF using two headless screws. A displaced shear-type fracture of the talar head could result in midfoot deformity and osteoarthritis of the talonavicular joint. Open reduction was necessary as we performed surgery on the seventeenth day after the trauma. At follow-up, no signs or symptoms were observed in our young patient.
Talar fractures in pediatric patients must be treated similar to those in adults[5,36]. Nondisplaced fractures of the talus can be treated non-operatively by using cast immobilization, while displaced fractures require operative intervention[5,11]. Godoy-Santos et al[8] and Rammelt et al[20] highlighted the limitations of the talar spontaneous remodeling capacity during growth; thus, these authors indicated ORIF for all displaced fractures[8,20]. If a few attempts of closed reduction appear unsuccessful, open reduction should be performed[8].
Kruppa et al[6] demonstrated worse injuries with high rates of complications (nonunion, osteonecrosis, osteoarthritis, deformities) and disabilities in adolescents: in general, older children and adolescents were more likely to benefit from surgical treatment[6].
The purpose of treatment is to reduce the rate of complications: osteonecrosis, osteoarthritis and foot deformities are the most frequent and dangerous[3,5,8,11-13]. With regard to the talar head specifically, unreduced fractures may result in post-traumatic arthritis and three-dimensional deformities: the foot function can be severely restricted by the medial column displacement and subluxation in the talonavicular joint[8,13]. Hence, immediate ORIF was traditionally considered crucial[14,15]. Nonetheless, the most recent literature has shown that there is no significant correlation between time of surgery and development of osteonecrosis or osteoarthritis[16,17].
Talar head fractures represent severe injuries, including in the pediatric population. Open reduction and internal fixation are necessary in the case of displacement. Injuries of the talar head in children and adolescents should be considered as transitional fractures; hence, the treatment aims to reduce malalignment and osteoarthritis. Due to the frequent misdiagnosis of these fractures, CT scans are recommended in children describing high energy trauma.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rabbi Q S-Editor: Zhang L L-Editor: Webster JR P-Editor: Xing YX
| 1. | Beaty JH, Kasser JR. Rockwood and Green’s Fractures in Children. Lippincott Williams & Wilkins, 2006: 1136-1138. |
| 2. | Letts RM, Gibeault D. Fractures of the neck of the talus in children. Foot Ankle. 1980;1:74-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Jensen I, Wester JU, Rasmussen F, Lindequist S, Schantz K. Prognosis of fracture of the talus in children. 21 (7-34)-year follow-up of 14 cases. Acta Orthop Scand. 1994;65:398-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 33] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Thermann H, Schratt HE, Hüfner T, Tscherne H. [Fractures of the pediatric foot]. Unfallchirurg. 1998;101:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Yazdi H, Ramezan Shirazi M. An unusual presentation of talus fracture in a child: a case report. Foot Ankle Surg. 2010;16:e57-e60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Kruppa C, Snoap T, Sietsema DL, Schildhauer TA, Dudda M, Jones CB. Is the Midterm Progress of Pediatric and Adolescent Talus Fractures Stratified by Age? J Foot Ankle Surg. 2018;57:471-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Sferopoulos NK. Talus fractures in children. ARC J Res Sport Med. 2017;2:21-26. |
| 8. | Godoy-Santos AL, Albuquerque DM, Diniz-Fernandes T, Rammelt S. Fracture of the talar neck associated with a compression fracture of the calcaneocuboid joint in a 5-year-old child: a case report. Arch Orthop Trauma Surg. 2013;133:1267-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Mayr J, Peicha G, Grechenig W, Hammerl R, Weiglein A, Sorantin E. Fractures and dislocations of the foot in children. Clin Podiatr Med Surg. 2006;23:167-189, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Bykov Y. Fractures of the talus. Clin Podiatr Med Surg. 2014;31:509-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Eberl R, Singer G, Schalamon J, Hausbrandt P, Hoellwarth ME. Fractures of the talus--differences between children and adolescents. J Trauma. 2010;68:126-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Smith JT, Curtis TA, Spencer S, Kasser JR, Mahan ST. Complications of talus fractures in children. J Pediatr Orthop. 2010;30:779-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Zwipp H, Ranft T. [Malunited juvenile fractures in the foot region]. Orthopade. 1991;20:374-380. [PubMed] |
| 14. | Kızılay YO, Aytan O. Low-Energy Hawkins Type III Talar Neck Fracture-Dislocation With Neurovascular and Tendon Entrapment in a Pediatric Patient. J Foot Ankle Surg. 2017;56:1288-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | García-Rey E, Sanz-Hospital FJ, Galdrán FJ, Cano-Egea JM, Alcázar LFL. Talar neck fractures: results and complications by type. Foot Ankle Surg. 2002;8:203-208. [DOI] [Full Text] |
| 16. | Schulze W, Richter J, Russe O, Ingelfinger P, Muhr G. Surgical treatment of talus fractures: a retrospective study of 80 cases followed for 1-15 years. Acta Orthop Scand. 2002;73:344-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Vallier HA, Nork SE, Barei DP, Benirschke SK, Sangeorzan BJ. Talar neck fractures: results and outcomes. J Bone Joint Surg Am. 2004;86:1616-1624. [PubMed] |
| 18. | Anderson HG. Medical and Surgical Aspects of Aviation. 1919, Henry Frowde Oxford University Press. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 19. | Canale ST, Kelly FB Jr. Fractures of the neck of the talus. Long-term evaluation of seventy-one cases. J Bone Joint Surg Am. 1978;60:143-156. [PubMed] |
| 20. | Rammelt S, Schneiders W, Fitze G, Zwipp H. [Foot and ankle fractures in children]. Orthopade. 2013;42:45-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Kern M, Tucker A, Rogers K, Kruse RW. CT Utilization for Pediatric Orthopedic Trauma. Del Med J. 2015;87:366-369. [PubMed] |
| 22. | Frush DP. Justification and optimization of CT in children: how are we performing? Pediatr Radiol. 2011;41 Suppl 2:467-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Almohiy H. Paediatric computed tomography radiation dose: A review of the global dilemma. World J Radiol. 2014;6:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (2)] |
| 24. | Moritz JD, Hoffmann B, Sehr DH, Eggerking J, Keil K, Caliebe A, Dischinger J, Heller M, Bolte H. [Pediatric fracture diagnosis--ultra-low-dose CT with an effective dose equal to that of radiographs]. Rofo. 2012;184:1026-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Goske MJ, Strauss KJ, Westra SJ, Frush DP. The Image Gently ALARA CT summit on new CT technologies for children. Pediatr Radiol. 2014;44 Suppl 3:403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Nenopoulos A, Beslikas T, Gigis I, Sayegh F, Christoforidis I, Hatzokos I. The role of CT in diagnosis and treatment of distal tibial fractures with intra-articular involvement in children. Injury. 2015;46:2177-2180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Lemburg SP, Lilienthal E, Heyer CM. Growth plate fractures of the distal tibia: is CT imaging necessary? Arch Orthop Trauma Surg. 2010;130:1411-1417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Olgun ZD, Maestre S. Management of Pediatric Ankle Fractures. Curr Rev Musculoskelet Med. 2018;11:475-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 29. | Eismann EA, Stephan ZA, Mehlman CT, Denning J, Mehlman T, Parikh SN, Tamai J, Zbojniewicz A. Pediatric Triplane Ankle Fractures: Impact of Radiographs and Computed Tomography on Fracture Classification and Treatment Planning. J Bone Joint Surg Am. 2015;97:995-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 30. | Fritsch H, Schmitt O, Eggers R. The ossification centre of the talus. Ann Anat. 1996;178:455-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Howard CB, Benson MK. The ossific nuclei and the cartilage anlage of the talus and calcaneum. J Bone Joint Surg Br. 1992;74:620-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 32. | Herring JA. Growth and Development. In: Herring JA. Tachdjian’s Pediatric Orthopaedics, 4th Edition. Saunders, 2008. |
| 33. | Schneidmueller D, von Rüden C, Friederichs J, Bühren V. [Transitional fractures: Epiphyseal injuries in adolescence]. Unfallchirurg. 2016;119:517-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Spiegel PG, Mast JW, Cooperman DR, Laros GS. Triplane fractures of the distal tibial epiphysis. Clin Orthop Relat Res. 1984;74-89. [PubMed] |
| 35. | Crawford AH. Triplane and Tillaux fractures: is a 2 mm residual gap acceptable? J Pediatr Orthop. 2012;32 Suppl 1:S69-S73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 36. | Draijer F, Havemann D, Bielstein D. [Injury analysis of pediatric talus fractures]. Unfallchirurg. 1995;98:130-132. [PubMed] |