Published online May 18, 2021. doi: 10.5312/wjo.v12.i5.320
Peer-review started: January 19, 2021
First decision: February 15, 2021
Revised: February 18, 2021
Accepted: April 22, 2021
Article in press: April 22, 2021
Published online: May 18, 2021
Processing time: 113 Days and 10.2 Hours
Endoscopic fasciotomy of the forearm for chronic exertional compartment syndrome (CECS) has gained popularity recently.
To systematically review the literature of endoscopic fasciotomy for CECS of the forearm, aiming to assess the outcomes and complications of the different endoscopic fasciotomy techniques described in the literature.
On January 18, 2021, PubMed and EMBASE were searched by 3 reviewers independently, and all relevant studies published up to that date were considered based on predetermined inclusion/exclusion criteria. The subject headings “endoscopic fasciotomy” and “compartment syndrome” and their related key terms were used. The Preferred Reporting Item for Systematic Reviews and Meta-Analyses statement was used to screen the articles.
A total of seven studies including 183 patients (355 forearms) were included. The mean age of the patients was 31.2 years (range: 15-42 years). The postoperative follow-up duration ranged from 6 wk to 4.9 years. All patients were able to return to sport activities between postoperative weeks 1 to 8. Recurrence of the compartment syndrome occurred in three patients, giving a rate of 1.6% per patient and 0.8% per forearm. The overall complication rate was 8.7% per patient, and 4.5% per forearm. The most common reported complication was hematoma (7 forearms; 2.0%).
Endoscopic fasciotomy for CECS of the forearm has favorable short- and mid-term outcomes with very low recurrence and complication rates. This, however, needs to be confirmed in larger, long-term follow-up, prospective, comparative studies between open, mini-open and endoscopic fasciotomy techniques.
Core Tip: Endoscopic fasciotomy of the forearm for chronic exertional compartment syndrome (CECS) has gained popularity recently. This study reviewed the literature of endoscopic fasciotomy for CECS of the forearm, summarizing the outcomes and complications of the different endoscopic fasciotomy techniques described.
- Citation: Marwan Y, Addar A, Algarni N, Algarni N, Burman M, Martineau PA. Endoscopic fasciotomy for chronic exertional compartment syndrome of the forearm: Systematic review of outcomes and complications. World J Orthop 2021; 12(5): 320-328
- URL: https://www.wjgnet.com/2218-5836/full/v12/i5/320.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i5.320
Chronic exertional compartment syndrome (CECS) is a condition where there is an exercise-induced increase in pressure within fascial compartments after muscle hyperemia and expansion, resulting in poor tissue perfusion followed by ischemic pain, functional loss, and possible neurologic compromise[1,2]. The symptoms of this condition are exercise-induced, and typically resolve when the activity ceases leaving no permanent damage to the tissue[1,2]. During exercise, the intramuscular pressure elevates to a point that the tissues within the affected compartment become swollen, tight, and painful, preventing further activities[1-3]. While the leg is the most involved, CECS can affect the shoulder, arm, forearm, hand, gluteus, thigh, and foot[1].
In the forearm, CECS is seen in people who perform activities and sports that require prolonged, repetitive and forceful gripping, such as cyclists, arm wrestlers, rowers, rock climbers and weightlifters[2-5]. Patients with CECS present with predictable and reproducible atraumatic exercise-induced pain, cramping and tightness that is typically localized to the affected compartment[1-3]. They may also complain of transient numbness, tingling, or weakness (e.g., loss of grip strength) in the distributions of nerves within the involved compartment, which usually resolve with rest[1-3]. In severe cases of CECS, these symptoms can significantly affect the quality of life, and can be dangerous occasionally (e.g., motocross riders may be unable to hold the handlebar grips while riding)[2,3].
Although the diagnosis of CECS can be made based on history and physical examination, few diagnostic tests can help confirm it[1-3,6-11]. Dynamic intra
The treatment of CECS can be nonsurgical or surgical[1-3]. Nonsurgical treatment in the form of activity modification, physical therapy and pain control can be successful in up to 80% of the cases[3,13]. Patients who have no improvement in symptoms after at least 3 mo despite nonoperative treatment are usually indicated for surgical management in the form of forearm fasciotomy[1-3]. Regardless of the surgical technique used to perform the fasciotomy, the rate of resolution of symptoms and return to sports activities reaches 90%[1-3].
Recently, endoscopic fasciotomy of the forearm for CECS has gained popularity[10,11,14-16]. Authors suggest that this surgical technique result in reduced time to return to competitive sports and decreased surgical scarring and complications[1-3]. Endoscopic fasciotomy techniques have evolved because the expansile muscle bellies which result in the compartment syndrome when swollen lie in the proximal third of the forearm, thus, fasciotomies distal to this region might not be required[2]. In this study, we aim to systematically review the literature of endoscopic fasciotomy for CECS of the forearm. We intend to assess the outcomes and complications of the different endoscopic fasciotomy techniques described in the literature. We hypothesize that overall outcomes are favorable in regards of return to sports and functional outcomes, as well as rate of recurrence and complications is low.
PubMed and EMBASE databases were searched independently by three authors (Marwan Y, Addar A, Algarni N) for relevant articles on January 18, 2021. The search was limited to English language only. The subject headings “endoscopic fasciotomy” and “compartment syndrome” and their related key terms were used. The articles were screened based on the Preferred Reporting Item for Systematic Reviews and Meta-Analyses statement.
The following inclusion criteria were used in our systematic review: (1) Clinical studies; (2) All level of evidence; (3) Endoscopic fasciotomy done for CECS of the forearm; (4) All endoscopic fasciotomy techniques; and (5) No restriction to date of publication. Studies were excluded if they met any of the following criteria: (1) Non-English articles; (2) Open fasciotomy; (3) Endoscopic fasciotomy of other anatomic regions (e.g., leg and foot); (4) Articles published in abstract form only; (5) Review articles; (6) Technique articles; and (7) Cadaveric studies.
Independent screening of the titles and abstracts of the included studies were carried out by the same three authors (Marwan Y, Addar A, Algarni N). Articles were included in the full-text review stage if any of the three authors believed it should, and more were excluded during this stage. The data was then retrieved from the included studies and entered/organized in Microsoft Excel 2013 (Microsoft, Redmond, WA, United States) independently by the same three authors. The information was categorized into basic background/clinical data (e.g., title, authors, year of publication, country of publication, sample size, gender, age, sports, risk factor and preoperative assessment), surgical technique (e.g., equipment, incision and other surgical details) and postoperative outcomes and complications (e.g., follow-up duration, recurrence, complications, return to sports, pain and functional scores). The primary outcome of this review was the recurrence rate, while return to sports, pain improvement, functional scores improvement and complications were the secondary outcomes. Meta-analysis was not done due to the heterogeneity of the included studies; however, a qualitative assessment of the data was done.
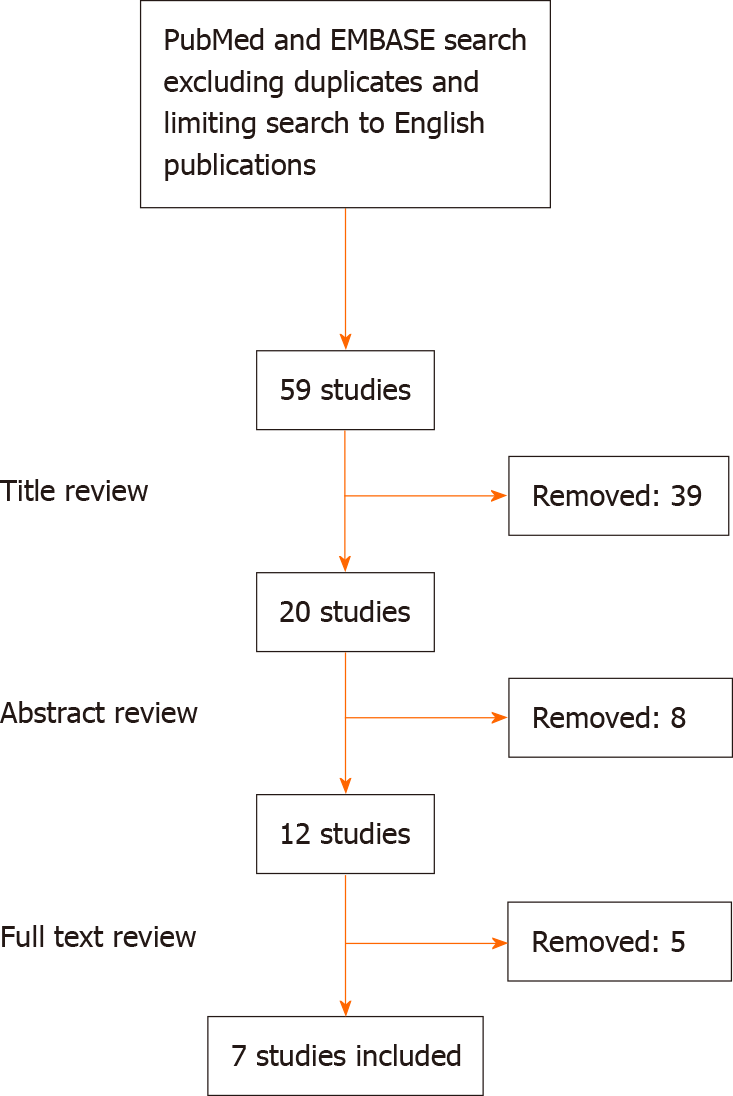
The initial search revealed a total of 59 article (Figure 1). A total of 39, 8 and 5 articles were excluded after title, abstract and full-text review, respectively. Therefore, seven articles were included for final analysis[10,11,14-18]. These articles were published from Asia, Europe and the United States. Additional screening of the references of the seven articles did not reveal more relevant studies that meet our inclusion criteria. The three reviewers (Marwan Y, Addar A, Algarni N) had no disagreements throughout the stages of the systematic review.
Table 1 summarizes the background information and clinical features of the included studies and patients. A hundred and eighty-three patients (355 forearms) underwent endoscopic fasciotomy for CECS of the forearm, of whom 178 (97.3%) were males. The mean age of the patients was 31.2 years (range: 15-42 years). Only four (2.2%) patients were not motorcycle/motocross riders/racers. To help in establishing the diagnosis of CECS, six out of the seven studies used compartment pressure measurements (29 patients; 15.8%), while MRI was used in two studies (155 patients; 84.7%). The visual analogue scale (VAS) score was used to assess the severity of pain in three out of the seven studies (159 patients; 86.9%); however, scale range differed among these studies (one used a scale of 1 to 10, while two used a scale of 0 to 10). On the other hand, the Disabilities of the Arm, Shoulder and Hand (DASH) score was used in a single study (3 patients; 1.6%), and the quick DASH score was used in another study (21 patients; 11.5%).
| Ref. | Sample size | Gender | Age (mean and range) | Sport/risk factor | Diagnostic investigations | Preoperative VAS score (mean and range) | Preoperative DASH score (mean and range) | Preoperative quick DASH score (mean and range) |
| Abe and Fujii[10], 2017 | 1 (unilateral) | 1 F | 15 | Tennis; This case involved the mobile wad only | Compartment pressure measurements (at rest, under stress and after stress) US and MRI | -- | -- | -- |
| Hijjawi and Nagle[14], 2010 | 1 (unilateral) | 1 M | 33 | Truck driver | Compartment pressure measurements (at rest and after stress) | -- | -- | -- |
| Jans et al[11], 2015 | 154 (all bilateral) | 151 M; 3 F | 32.7; 16-42 | Motocross racers | MRI after flexor loading (repetitive grip until exhaustion for 15 minutes) | 1.1 ± 0.3 at rest and 7.4 ± 1.5 after stress (used scale of 1 to 10) | -- | -- |
| Miller et al[17], 2017 | 2 (1 bilateral) | 2 M | 24.5; 23-26 | Motocross racers | Compartment pressure measurements (at rest and after stress) | 9.5; 9-10 (used scale of 0 to 10) | -- | -- |
| Pegoli et al[15], 2016 | 3 (1 bilateral) | 3 M | 25.3 | Motorcycle drivers | Compartment pressure measurements (at rest, under stress and after stress) | 4.5; 3-6 (used scale of 0 to 10) | 21.71%; 18.42-25.00% | -- |
| Ruyer et al[16], 2020 | 21 (15 bilateral) | 21 M | 28; 14-42 | Motorcycle road racing (n = 20), off-road motorcycle racing or enduro (n = 11), quad racing (n = 4) and mountain biking and water skiing (n = 1) | Compartment pressure measurements (pre- and post-stress) | -- | -- | 23 ± 10%; 7-45% |
| Seiler et al[18], 2011 | 1 (bilateral) | 1 F | 19 | Swimmer | Compartment pressure measurements (after stress) | -- | -- | -- |
Table 2 demonstrates the surgical techniques used in the included studies. Each group of surgeons used different set of tools; however, the basic setup consisted of an endoscope and a cutting instrument like blade or electrocautery. Skin incision ranged from one to three, based on surgeon preference, surgical set used and the involved compartment. Interestingly, the largest series of patients underwent fasciotomy of the superficial flexor compartment only without consideration of releasing other compartments of the forearm[11]. A single case had compartment syndrome of the mobile wad only, therefore, release of the brachioradialis fascia was done only[10].
| Ref. | Sample size | Surgical technique | ||
| Special tools | Incisions | Other surgical notes | ||
| Abe and Fujii[10], 2017 | 1 (unilateral) | 2.3 mm endoscope with 30° angle | 1 cm single incision, 2 cm proximal to the point of tenderness | Release of brachioradialis fascia (case involved mobile wad only) |
| Hijjawi and Nagle[14], 2010 | 1 (unilateral) | 4.5 mm 30° endoscope and probe blade from Chow dual-port endoscopic carpal tunnel set | 2 incision: 2 cm transverseincision was made at the junction of the middle and distal thirds of the forearm in line with the flexor-pronator muscles; another 2 cm incision made 4 cm distal to the elbow crease | -- |
| Jans et al[11], 2015 | 154 (all bilateral) | The single-use Vasoview 7 Endoscopic Vessel Harvesting System (Maquet–Getinge Group, Rastatt, Germany) | Single 3 cm volar incision between flexor carpi radialis tendon and palmaris longus tendon made 4 cm proximal to the wrist | Decompression of the superficial flexor compartment done up to 3 cm distal to cubital fold |
| Miller et al[17], 2017 | 2 (1 bilateral) | EndoRelease (Integra LifeSciences Corporation,Plainsboro, New Jersey) system | Single incision over the subcutaneous border of the ulna midway between olecranon and ulnar styloid | -- |
| Pegoli et al[15], 2016 | 3 (1 bilateral) | STORZ endoscopy set | Single 2 cm volar incision: Line drawn between medial epicondyle to wrist flexion crease ulnar to palmaris longus tendon, then divided into 4 parts. Incision is made between first and second quarters proximally | Fasciotomy between flexor carpi radialis/palmaris longus tendons laterally and flexor carpi ulnaris medially |
| Ruyer et al[16], 2020 | 21 (15 bilateral) | SmartRelease® (previously Agee®) endoscopic system (Micro- Aire Surgical Instruments, VA, United States) | Incision based on the involved compartments: Line drawn between medial epicondyle to middle of wrist flexion crease anteriorly, and between lateral epicondyle and Lister’s tubercle posteriorly. 2 or 3 small incisions are made along the lines to fit the 6 cm long endoscopic knife | -- |
| Seiler et al[18], 2011 | 1 (bilateral) | 0° endoscope and electrocautery forceps | 3 incisions: dorsal incision just proximal to extensor retinaculum along a line between lateral epicondyle and Lister’s tubercle; volar incision made along a line between palmaris longus tendon and biceps tendon, proximal incision made 1 cm distal to the midline of the antecubital fossa, and distal incision at the wrist crease just ulnar to palmaris longus tendon | -- |
The outcomes and complications of endoscopic fasciotomy for CECS of the forearm are demonstrated in Table 3. The follow-up duration of the 183 patients ranged from 6 wk to 4.9 years. In two studies (5 patients; 2.7%), the mean VAS score at final follow-up ranged from 0.0 to 0.75 out of 10. Another study (154 patients; 84.1%) reported a final follow-up mean VAS score of 1.0 out of 10 at rest and 1.7 out of 10 following stress. In addition, the postoperative DASH score ranged from 2.15% to 5.39% in two studies (4 patients; 2.2%), and the mean quick DASH score was 1% in a single study (21 patients; 11.5%). All patients were able to return to sport activities, and this was between postoperative week 1 to 8. Recurrence of the compartment syndrome occurred in three patients, giving a rate of 1.6% per patient and 0.8% per forearm. The overall complication rate was 8.7% per patient, and 4.5% per forearm. The most common reported complication was hematoma (7 forearms; 2.0%).
| Ref. | Sample size | Follow-up duration | Postoperative VAS score (mean and range) | Postoperative DASH score (mean and range) | Postoperative quick DASH score (mean and range) | Return to sports | Other outcomes | Recurrence | Complications | |
| Abe and Fujii[10], 2017 | 1 (unilateral) | 7 mo | -- | -- | -- | Returned 2 mo postoperatively | Pain free at 4 mo postoperatively | None | None | |
| Hijjawi and Nagle[14], 2010 | 1 (unilateral) | 6 mo | -- | -- | -- | -- | Pain free at final follow-up | None | None | |
| Jans et al[11], 2015 | 154 (all bilateral) | 6 wk | 1.0 ± 0.2 at rest and 1.7 ± 0.9 after stress (used scale of 1 to 10) | -- | -- | All returned 6 wk postoperatively | -- | 1 recurrence 8 mo postoperatively | 5 hematomas requiring drainage | |
| Miller et al[17], 2017 | 2 (1 bilateral) | 1 mo (only specified for 1 case) | 0.0 | -- | -- | Both returned 1 wk postoperatively | Improved grip strength and wrist ROM | None | 1 case had small seroma resolved with compressive wrapping at 2 wk postoperatively | |
| Pegoli et al[15], 2016 | 3 (1 bilateral) | 45.80 mo (34-55) | 0.75; 0-2 (used scale of 0 to 10) | 5.39%; 2.15-10.05% | -- | All returned 3 wk postoperatively | -- | None | None | |
| Ruyer et al[16], 2020 | 21 (15 bilateral) | 4.9 ± 2.7 yr (range: 1.0-10.2)3 patients lost follow-up | -- | -- | 1 ± 2%; 0-9% | Returned at 4.3 ± 1.8 wk (range: 3-8 wk) postoperatively | 14 were very satisfied with the procedure, 3 were satisfied, and 1 was moderately satisfied. | 2 recurrence due to fibrous scar tissues requiring revision fasciotomy; revision was open for one of them | 2 superficial vascular injury, 1 superficial sensory nerve injury, 2 hematomas (1 requiring drainage), 3 transient hypoesthesia (recovered at 3 mo postoperatively). 2 lateral epicondylalgia | |
| Seiler et al[18], 2011 | 1 (bilateral) | 9 mo | -- | 5.0% | -- | Returned 3 wk postoperatively; full level at 6 wk postoperatively | Pain free at final follow-up | None | None | |
The current systematic review has explored the outcomes and complications of endoscopic fasciotomy for CECS in 355 forearms of 183 patients. Regardless of the technique/equipment used to perform the endoscopic fasciotomy, the outcomes were excellent. The recurrence and complication rates were less than 1% and less than 5% per forearm, respectively. No serious complications were reported. Additionally, no patients were unable to return to their preoperative level of sports activities, and return to sports was between 1 wk to 8 wk postoperatively. Resolution of pain and improvement in functional scores were also excellent.
Surgical treatment for CECS has high success rate, regardless of the surgical technique used[1-3]. Compared to patients who undergo surgical intervention for CECS of the forearm, authors have shown that all patients who underwent nonoperative management continued to struggle and were no longer able to perform sports and activities at the same level of their pre-morbid condition[1,19]. Surgical intervention is, therefore, recommended for those who wish to continue to practice high level of sports activities.
Wide open fasciotomy of the forearm is thought to be the best surgical intervention for CECS, allowing full release of the fascia, better visualization of neurovascular structures, and peripheral nerve decompression if needed; thus, may have lower rate of complications[1-3,20,21]. Based on the available literature on open forearm fasciotomy for CECS and our current systematic review of endoscopic fasciotomy, this is not necessarily true. The rate of patients with full resolution of CECS symptoms following open or mini-open fasciotomy of the forearm ranged between around 85% to 98%[2,9,20-23], while the rate after endoscopic fasciotomy was around 99% [2,10,11, 14-18]. Moreover, complication rate of open and mini-open fasciotomy ranged between around 14% to 21%[2,9,20-23], while the rate following endoscopic fasciotomy was less than 10%[2,10,11,14-18]. Although these differences have not been proven with high-quality, comparative, prospective studies, endoscopic fasciotomy may provide superior outcomes compared to open fasciotomy.
Although this study provides valuable information, several limitations exist. The studies found in the literature and included in the current systematic review are either case series or case reports. Despite the lack of high-quality, high-level of evidence studies, valuable information has been extracted which should help guide future research about endoscopic forearm fasciotomy. Also, as most of the available studies were case reports, cases with unsatisfactory outcomes might have been underreported. Another limitation is that the short period of postoperative follow-up for some of the included studies. A long-term follow-up is needed specially to determine recurrence of the CECS after resuming sports for a longer period post endoscopic fasciotomy. In addition, poor documentation of relevant functional outcomes was noted in the available studies.
Endoscopic fasciotomy for CECS of the forearm has favorable short- and mid-term outcomes with very low recurrence and complication rates. This, however, needs to be confirmed in larger, long-term follow-up, prospective, comparative studies between open, mini-open and endoscopic fasciotomy techniques.
Chronic exertional compartment syndrome (CECS) of the forearm can limit the quality of life and sport activities. Endoscopic forearm fasciotomy has been described to manage this condition.
The literature of endoscopic forearm fasciotomy for CECS has not been analyzed in detail.
To systematically review the literature if endoscopic fasciotomy for the management of CECS of the forearm.
PubMed and EMBASE were searched, and all relevant studies were considered for analysis based on predetermined inclusion/exclusion criteria. The subject headings “endoscopic fasciotomy” and “compartment syndrome” and their related key terms were used.
A total of seven studies including 183 patients (355 forearms) were included. All patients were able to return to sport activities between postoperative week 1 to 8. Recurrence of the compartment syndrome occurred in three patients. The overall complication rate was 8.7% per patient, and 4.5% per forearm.
Outcome of endoscopic fasciotomy for CECS of the forearm are favorable, with low recurrence and complication rates.
Future larger, long-term follow-up, prospective, comparative studies between open, mini-open and endoscopic fasciotomy techniques are needed.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Canada
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mayr J S-Editor: Liu M L-Editor: A P-Editor: Li X
| 1. | Fraipont MJ, Adamson GJ. Chronic exertional compartment syndrome. J Am Acad Orthop Surg. 2003;11:268-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 78] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Liu B, Barrazueta G, Ruchelsman DE. Chronic Exertional Compartment Syndrome in Athletes. J Hand Surg Am. 2017;42:917-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Humpherys J, Lum Z, Cohen J. Diagnosis and Treatment of Chronic Exertional Compartment Syndrome of the Forearm in Motocross Riders. JBJS Rev. 2018;6:e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Bird CB, McCoy JW Jr. Weight-lifting as a cause of compartment syndrome in the forearm. A case report. J Bone Joint Surg Am. 1983;65:406. [PubMed] |
| 5. | Goubier JN, Saillant G. Chronic compartment syndrome of the forearm in competitive motor cyclists: a report of two cases. Br J Sports Med. 2003;37:452-3; discussion 453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Boody AR, Wongworawat MD. Accuracy in the measurement of compartment pressures: a comparison of three commonly used devices. J Bone Joint Surg Am. 2005;87:2415-2422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 53] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med. 1990;18:35-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 304] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 8. | Whitesides TE, Heckman MM. Acute Compartment Syndrome: Update on Diagnosis and Treatment. J Am Acad Orthop Surg. 1996;4:209-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 173] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 9. | Brown JS, Wheeler PC, Boyd KT, Barnes MR, Allen MJ. Chronic exertional compartment syndrome of the forearm: a case series of 12 patients treated with fasciotomy. J Hand Surg Eur Vol. 2011;36:413-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Abe Y, Fujii K. Chronic Compartment Syndrome of the Mobile Wad: A Case Report. J Hand Surg Asian Pac Vol. 2017;22:516-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Jans C, Peersman G, Peersman B, Van Den Langenbergh T, Valk J, Richart T. Endoscopic decompression for chronic compartment syndrome of the forearm in motocross racers. Knee Surg Sports Traumatol Arthrosc. 2015;23:2522-2527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Kumar PR, Jenkins JP, Hodgson SP. Bilateral chronic exertional compartment syndrome of the dorsal part of the forearm: the role of magnetic resonance imaging in diagnosis: a case report. J Bone Joint Surg Am. 2003;85:1557-1559. [PubMed] |
| 13. | Hutchinson MR, Ireland ML. Common compartment syndromes in athletes. Treatment and rehabilitation. Sports Med. 1994;17:200-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Hijjawi J, Nagle DJ. Endoscopic-assisted Fascial Decompression for Forearm Exertional Compartment Syndrome: A Case Report and Review of the Literature. Hand (N Y). 2010;5:427-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Pegoli L, Pozzi A, Pivato G. Endoscopic Single Approach Forearm Fasciotomy for Chronic Exertional Compartment Syndrome: Long Term Follow-up. J Hand Surg Asian Pac Vol. 2016;21:8-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Ruyer J, Rutka V, Garret J, Rizzo C, Guigal V. Endoscopic fasciotomy for chronic exertional compartment syndrome of the forearm: Clinical results of a new technique using an endoscopic carpal tunnel release device. Hand Surg Rehabil. 2020;39:154-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Miller EA, Cobb AL, Cobb TK. Endoscopic Fascia Release for Forearm Chronic Exertional Compartment Syndrome: Case Report and Surgical Technique. Hand (N Y). 2017;12:NP58-NP61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Seiler JG 3rd, Hammond KE, Payne SH, Ivy R. Bilateral exertional compartment syndrome of the forearm: evaluation and endoscopic treatment in an elite swimmer. J Surg Orthop Adv. 2011;20:126-131. [PubMed] |
| 19. | García Mata S, Hidalgo Ovejero A, Martinez Grande M. Bilateral, chronic exertional compartment syndrome of the forearm in two brothers. Clin J Sport Med. 1999;9:91-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Zandi H, Bell S. Results of compartment decompression in chronic forearm compartment syndrome: six case presentations. Br J Sports Med. 2005;39:e35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Barrera-Ochoa S, Haddad S, Correa-Vázquez E, Font Segura J, Gil E, Lluch A, Soldado F, Mir-Bullo X. Surgical Decompression of Exertional Compartment Syndrome of the Forearm in Professional Motorcycling Racers: Comparative Long-term Results of Wide-Open Versus Mini-Open Fasciotomy. Clin J Sport Med. 2016;26:108-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Croutzet P, Chassat R, Masmejean EH. Mini-invasive surgery for chronic exertional compartment syndrome of the forearm: a new technique. Tech Hand Up Extrem Surg. 2009;13:137-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Harrison JW, Thomas P, Aster A, Wilkes G, Hayton MJ. Chronic exertional compartment syndrome of the forearm in elite rowers: a technique for mini-open fasciotomy and a report of six cases. Hand (N Y). 2013;8:450-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |