Published online May 18, 2021. doi: 10.5312/wjo.v12.i5.301
Peer-review started: January 9, 2021
First decision: January 18, 2021
Revised: January 28, 2021
Accepted: March 8, 2021
Article in press: March 8, 2021
Published online: May 18, 2021
Processing time: 123 Days and 3.7 Hours
The critical shoulder angle (CSA) is a radiographic measurement that provides an assessment of both glenoid inclination and acromial length. Higher values may correlate with the presence of rotator cuff tears. However, it is difficult to obtain a high-quality true anteroposterior (AP) radiograph of the shoulder, with any excess scapular version or flexion/extension resulting in deviation from the true CSA value. Three-dimensional (3D) bony reconstructions of computed tomography (CT) shoulder scans may be able to be rotated to obtain a similar view to that of true AP radiographs.
To compare CSA measurements performed on 3D bony CT reconstructions, with those on corresponding true AP radiographs.
CT shoulder scans were matched with true AP radiographs that were classified as either Suter-Henninger type A or C quality. 3D bony reconstructions were segmented from the CT scans, and rotated to replicate an ideal true AP view. Two observers performed CSA measurements using both CT and radiographic images. Measurements were repeated after a one week interval. Reliability was assessed using intraclass correlation coefficients (ICCs) and Bland-Altman plots [bias, limits of agreement (LOA)].
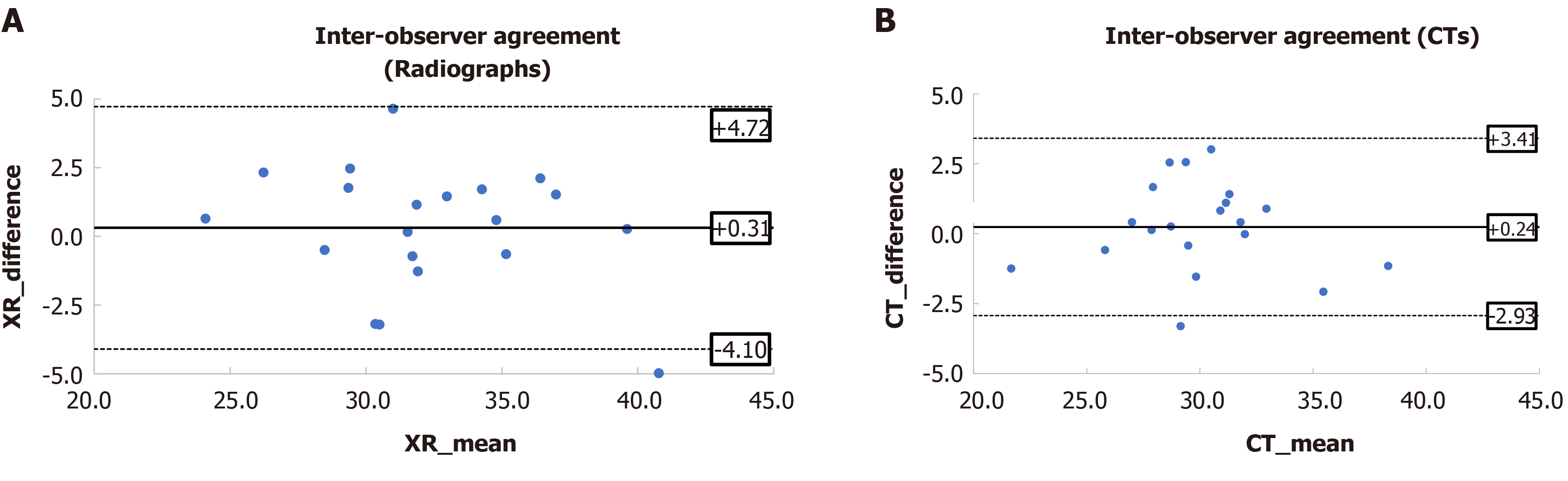
Twenty CT shoulder scans were matched. The mean CSA values were 32.55° (± 4.26°) with radiographs and 29.82° (± 3.49°) with the CT-based method [mean difference 2.73° (± 2.86°); P < 0.001; bias +2.73°; LOA -2.17° to +7.63°]. There was a strong correlation between the two methods (r = 0.748; P < 0.001). Intra-observer reliability was similar, but the best intra-observer values were achieved by the most experienced observer using the CT-based method [ICC: 0.983 (0.958-0.993); bias +0.03°, LOA -1.28° to +1.34°]. Inter-observer reliability was better with the CT-based method [ICC: 0.897 (0.758-0.958), bias +0.24°, LOA -2.93° to +3.41°].
The described CT-based method may be a suitable alternative for critical shoulder angle measurement, as it overcomes the difficulty in obtaining a true AP radiographic view.
Core Tip: The critical shoulder angle (CSA) is a radiographic measure which correlates with the presence of rotator cuff tears. However, it is difficult to obtain high-quality true anteroposterior radiographs that are suitable for CSA measurements. Three-dimensional bony reconstructions may be produced from computed tomography shoulder scans and be rotated to replicate a more ideal true anteroposterior view, and hence obtain a more accurate CSA measurement. This retrospective study demonstrated its improved intra-observer and inter-observer reliability, compared to the standard radiographic method.
- Citation: Mah D, Chamoli U, Smith GC. Usefulness of computed tomography based three-dimensional reconstructions to assess the critical shoulder angle. World J Orthop 2021; 12(5): 301-309
- URL: https://www.wjgnet.com/2218-5836/full/v12/i5/301.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i5.301
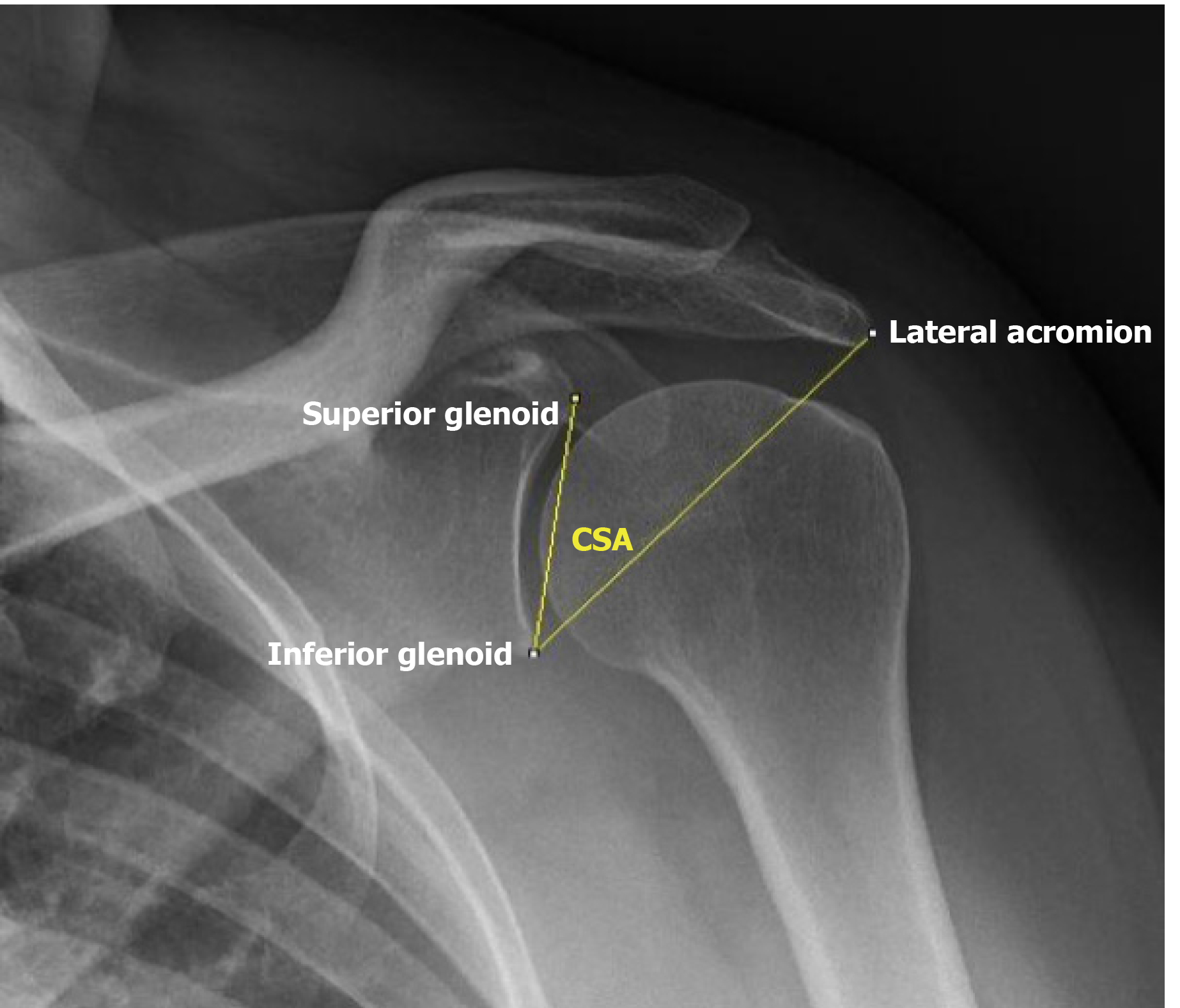
The critical shoulder angle (CSA) is a radiographic measurement that provides an assessment of both glenoid inclination and acromial length[1]. It is defined as the angle between a line joining the superior and inferior bony margins of the glenoid fossa, and the line joining the inferior margin of the glenoid fossa and the most inferolateral aspect of the acromion on a true anteroposterior radiograph of the shoulder (Figure 1)[2]. CSA values greater than 35° and less than 30° are associated with degenerative rotator cuff (RC) tears and primary glenohumeral osteoarthritis (GHOA), respectively[2]. If reduced, this may lower the risk of non-healing or re-tear after RC repair. Thus, this radiological measure may be useful in clinical practice for the preoperative evaluation of RC tears, particularly in the consideration of lateral acromioplasty as an adjunct to RC repair[3].
However, the precision and reliability of the CSA measurement is dependent on the quality of the true anteroposterior (AP) radiograph which should show “visible joint space and only minimal overlap between the posterior and anterior rim of the glenoid”[2,4]. Suter et al[5] demonstrated that any excess scapular ante-/retro-version (+5°/-8°) or flexion/extension (+15°/-26°) results in > 2° deviation of the measured CSA compared with the true value. They consequently defined the Suter-Henninger (SH) criteria, which classifies the radiographic image according to the degree of overlap of the anterior and posterior glenoid rims (Types A-D) and the location of the coracoid process relative to the superior glenoid (Types 1-3)[5].
Unfortunately, it is difficult to gain a high-quality true AP radiograph. A previous study reported the rate of acquisition of SH Type A1 radiographs to be 57%[6]. The use of cross-sectional imaging offers a potential alternative to plain radiographs, as it may eliminate the need for the accurate patient and imaging gantry positioning required to achieve SH Type A or C radiographs. Computed tomography (CT) has shown promising reproducibility in CSA measurements[7]. The use of three-dimensional (3D) bony CT reconstructions of scapulae may offer an alternative, which theoretically can be rotated to a similar view to that of true AP radiographs. The present study aimed to evaluate CSA measurements performed on 3D bony reconstructions of shoulder CT scans, and to correlate the results with conventional measurements of the CSA using true AP radiographs.
This study was approved by the University of New South Wales Human Research Ethics Committee (HC180427). In the absence of pre-existing data on using a 2D angle measurement on 3D reconstructions of CT scans, it was not possible to conduct an a priori power calculation. Previous studies that compared imaging modalities for CSA measurements used sample sizes of 30-60[7,8]. To maximise the sample size, we used all the imaging data available over a 5-year period from the private clinical practice of the senior author (Smith GCS).
A retrospective review of the private medical records from the clinical practice of GS was performed for patients who had non-arthrographic CT shoulder scans performed between June 2013 and June 2018. The earliest CT scan was used if multiple scans of the same patient were available in the database. Identified patients were then similarly searched for radiographic series of the same shoulder side with a true AP view. Prior to the study commencement, two of the authors (Mah D, Smith GCS) trained together using five illustrative cases to establish a routine method of measurement, as described below. In total, there were 96 shoulders (93 patients) with paired imaging identified.
The quality of the AP radiographs was assessed according to the SH criteria by the senior author (Smith GCS). Only SH Type A and C radiographs were included. The CSA was measured radiographically with image processing software ImageJ (ver. 1.51, United States National Institutes of Health, Bethesda, MD, United States) according to the technique described initially by Moor et al[2] (Figure 1). Identifiable osteophytes were not included in angular measurements in patients with GHOA. Of the 96 consecutive shoulders with paired imaging identified, only 20 (21%) had radiographs that were of sufficient quality for inclusion (SH Type A: n = 18; SH Type C: n = 2).
The median age of patients at the time of their CT shoulder scan was 56 years (range: 17-77 years). There were 12 males and 8 females. The median time between CT and radiographic imaging was 113.5 d (range: 0-534 d). The clinical diagnoses were: glenohumeral instability (n = 8), primary GHOA (n = 6), proximal humeral fracture (n = 4), secondary GHOA due to avascular necrosis (n = 1), and humeral tumour (n = 1).
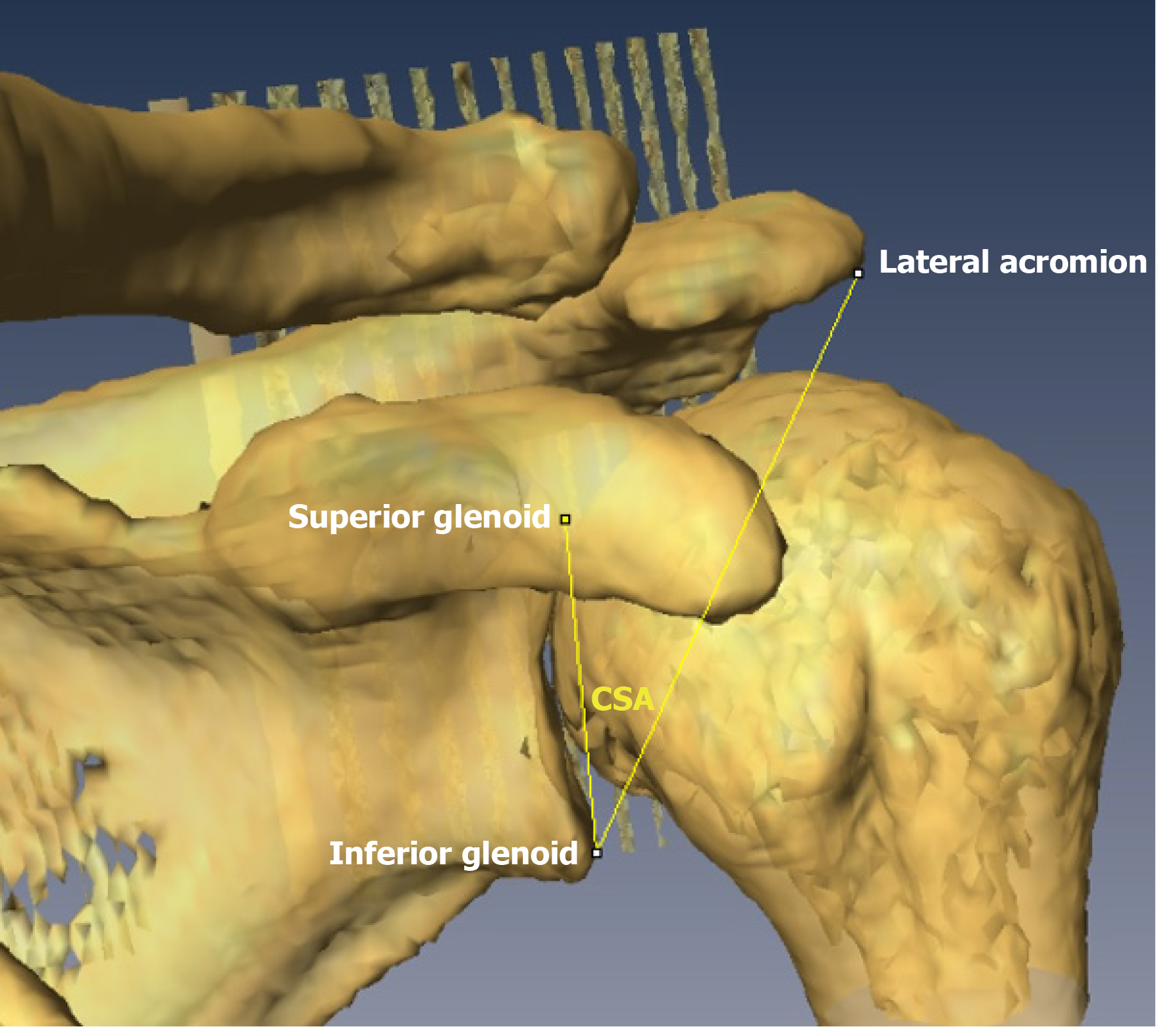
The Digital Imaging and Communications in Medicine files of the remaining paired CT scans were imported into the image processing and 3D reconstruction software Amira (ver. 5.4, Visage Imaging, San Diego, CA, United States). Scapulae were semi-automatically segmented from the CT image data and semi-transparent 3D reconstructions of the bone surfaces were generated. The 3D reconstructions of the scapulae were then rotated, such that the glenoid was orthogonal to the plane of view with minimal overlap of the anterior and posterior margins of the glenoid, and with the midpoint of the coracoid process intersecting the upper margin of the glenoid. This process replicated the view of an ideal SH Type A1 radiographic image. Once the desired position was obtained, a snapshot was taken, and the CSA was measured on the snapshot using ImageJ (Figure 2).
The CSA measurement methods described above were performed by two observers: an experienced shoulder surgeon (Observer 1; Smith GCS) and a final-year medical student (Observer 2; Mah D). All measurements were repeated by both investigators after a one-week interval to assess intra-observer reliability.
Statistical analyses were performed using the statistical software SPSS (ver. 25, IBM Corporation, Armonk, NY, United States). Data were tested for normality using the Kolmogorov-Smirnov test. As the data were normally distributed, the distribution of variables was expressed using mean and standard deviation values. Age and gender group differences were evaluated using independent-samples t-tests. Inter-method comparison was performed using paired-samples t-tests, Pearson correlation coefficients and Bland-Altman plots[9]. Hypothesis tests were conducted at a significance level of 0.05.
The inter-observer and intra-observer reliability of each CSA measurement method was evaluated using two-way mixed consistency single-measures intraclass correlation coefficients (ICCs). The ICCs were classified according to the method described by Koo and Li[10], where values < 0.50, 0.50-0.75, 0.75-0.90, and > 0.90 indicated “poor”, “moderate”, “good”, and “excellent” reliabilities, respectively[10]. The reliabilities were further assessed using bias and limits of agreement (LOA) on Bland-Altman plots.
Table 1 displays the mean CSA values obtained by each method and observer, as well as the absolute difference and Pearson correlation between them. Additionally, there were no statistically significant differences in measured CSA values between age groups (≤ 55 years and > 55 years; P = 0.550) and gender groups (male/female; P = 0.698).
| Observer 1 (Smith GCS) | Observer 2 (Mah D) | Combined | |
| Means (SD) | |||
| Radiographs | 32.42° (4.58°) | 32.88° (3.96°) | 32.55° (4.26°) |
| CT-based method | 29.86° (3.61°) | 29.79° (3.41°) | 29.82° (3.49°) |
| Inter-method | |||
| Difference (LOA) | 12.46° (-3.05° to +7.24°) | 12.99° (-3.15° to +7.97°) | 12.73° (-2.17° to +7.63°) |
| Pearson’s r | 10.769 | 10.725 | 10.748 |
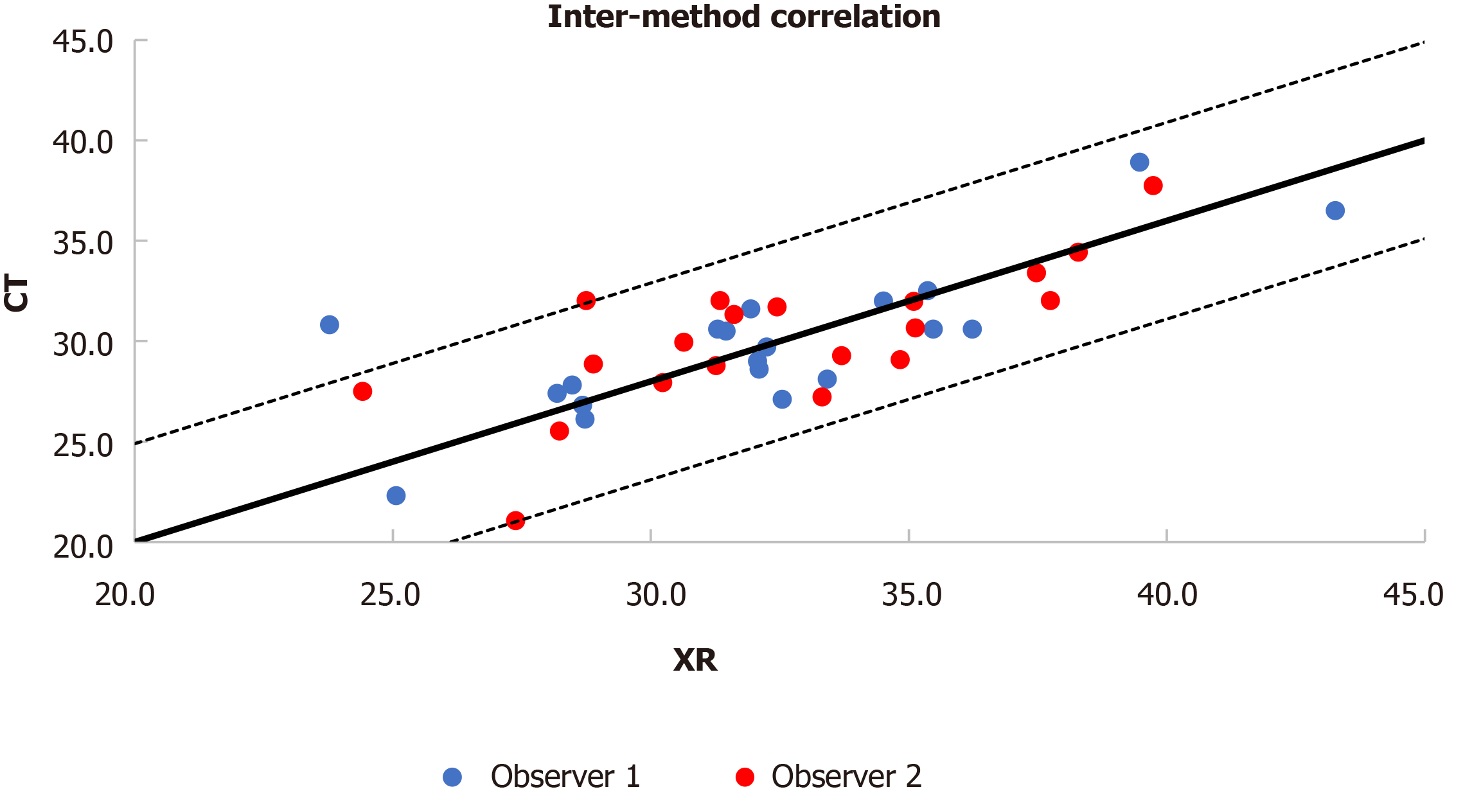
There was a positive inter-method correlation between the CSA values obtained using the CT-based method and the conventional radiographic method (Pearson’s r = 0.748; P < 0.001; Figure 3). The bias between the two methods was +2.73° (LOA: –2.17° to +7.63°).
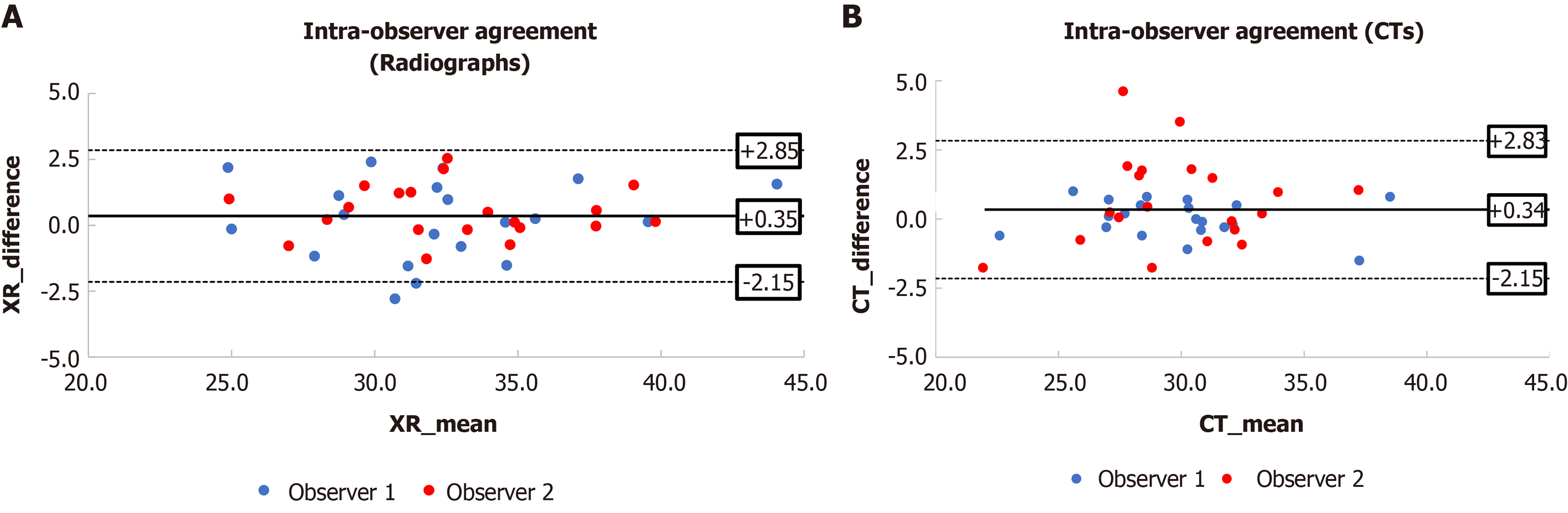
The intra-observer ICC values of the CSA measured using the conventional radiographic method were “excellent” for both observers [Observer 1: ICC: 0.946 (0.870-0.978); Observer 2: ICC: 0.970 (0.925-0.988)]. The bias within observers was +0.35° (LOA: –2.15° to +2.85°; Figure 4A). Similar LOAs were observed for Observer 1 (bias +0.20°; LOA: –2.78° to +3.18°) and Observer 2 (bias +0.50°; LOA: –1.43° to +2.43°).
The intra-observer ICC values of the CSA measured using the CT-based method were “excellent” for Observer 1 [ICC: 0.983 (0.958-0.993)] and “good” for Observer 2 [ICC: 0.887 (0.738-0.954)]. The bias within observers was +0.34° (LOA: -2.15° to +2.83°; Figure 4B). A wider LOA was observed in Observer 2 (bias +0.66°; LOA: -2.54° to +3.85°), compared to Observer 1 (bias +0.03°; LOA: –1.28° to +1.34°).
The inter-observer reliability of CSAs measured using the conventional radiographic method was “good” [ICC: 0.864 (0.688-0.944)]. The bias between the two observers was +0.31° (LOA: -4.10° to +4.72°; Figure 5A).
The inter-observer reliability of CSAs measured using the CT-based method was also “good” [ICC: 0.897 (0.758-0.958)]. The bias between the two observers was +0.24° (LOA: -2.93° to +3.41°; Figure 5B). This achieved slightly better inter-observer reliability than the radiographic method.
The most important finding of this study is its support of the potential use of 3D bony reconstructions of CT shoulder scans to perform CSA measurements. Whilst radiographs have the advantage of being cheap, low-radiation and accessible (and hence are the primary investigation for a variety of shoulder conditions), a recent meta-analysis demonstrated that radiographic quality is a source of heterogeneity in studies that investigate the link between CSA and RC tears and primary GHOA[11]. Poor radiographic quality was found to contribute to differences in the measured CSA found in both symptomatic RC tear patients and primary GHOA patients. In our study, only 21% of the shoulders with paired imaging had true AP radiographs of SH Type A or C, thus highlighting the difficulty in obtaining such high-quality radiographs in routine clinical practice. While fluoroscopy may be able to assist, it is associated with increased radiation exposure and is not available in most locations outside the operating theatre.
Instead of radiographs, a true AP view of the shoulder can theoretically always be obtained using 3D bony reconstructions from CT scan data. Low-dose CT imaging may reduce the radiation dose by 50%, without compromising the diagnostic performance[12]. In our study, there was a strong positive correlation between CSA values obtained using the CT-based method and the conventional radiographic method. Previous authors have suggested that a 2° difference in the measured CSA is clinically unimportant and that LOA values of -2° to +2° for intra- and inter-observer reliability for the measurement of CSA are excellent[2]. Both the intra- and inter-observer reliabilities of each method were slightly worse than, but approximate to this range. The CT-based method demonstrated superiority in terms of inter-observer reliability over the radiographic method. It also yielded statistically significant lower CSA values compared to the conventional radiographic method, which was present regardless of the observer’s clinical experience. This may reflect the ability to always create a SH A1 image, eliminating measurement inaccuracy due to scapular version and flexion/extension[5].
A systematic review concluded that a high CSA is associated with RC re-tear rates and worse clinical outcomes after RC repair[13]. After first being trialled in cadaveric studies, several authors have also described the use of an arthroscopic lateral acromioplasty with the aim of reducing the CSA[14,15]. While it is not currently widely used in the investigation of RC tears, the use of CT would have the additional advantage of allowing accurate preoperative planning of a lateral acromioplasty, with the aim of reducing the CSA to the normal range (30°-35°). This could improve the efficacy of lateral acromioplasty, and reduce the potential compromise of the deltoid origin.
The present study also highlights particular drawbacks with using the CT-based method. Firstly, the intra-observer reliability of the CT-based method was compromised to some degree when the less clinically experienced observer (Mah D) utilised the 3D reconstruction. This suggests a difficulty with obtaining an orthogonal plane of view, likely due to less familiarity with scapular anatomy. This effect was more pronounced at CSA < 30°, suggesting that the presence of osteophytes may affect the reliability of the CT-based method when performed by a less clinically experienced observer. Secondly, although the present study used an image processing software (Amira) that does allow free rotation of the 3D reconstructions in any plane, not all picture archiving and communication system software currently allow the free rotation of images in different planes. This may affect the ability to generate an SH Type A or C view.
Subtraction of the humerus was not undertaken, due to technical difficulties that would also not be able to be practically resolved in a clinical setting. When the 3D reconstructions were rotated to create an overlap of the coracoid process and superior glenoid (and hence a SH Type A1 view), this often obscured the upper margin of the glenoid during CSA measurement which may have affected the measured value and the intra-observer and inter-observer reliabilities to an extent, even with semi-transparent images. However, due to the concave shape of the glenoid, measurement error would tend to have generated an erroneously high CSA using the CT-based method, whereas a lower value was found in this study. Nevertheless, we believe that segmentation and subtraction of the humerus, and the ability to render the resultant image of the scapula radiolucent such that the upper border of the glenoid can be visualised through the coracoid process, would further improve the accuracy of the CT-based method in measuring the CSA.
A limitation of the present study is the small sample size of CT shoulder scans that were appropriately matched with true AP radiographs classified as SH Type A or C. This is a reflection of the difficulty in obtaining high-quality true AP radiographs in clinical settings. Additionally, none of the CT shoulder scans in our analysed population were ordered for RC tear indication, and therefore, the number of patients with a CSA of more than 35° was relatively low. However, the aim of this study was to evaluate the CSA measurement method using 3D reconstructions of CT scans of the shoulder. We do not believe that the outcomes would have been affected by including subjects with a higher CSA.
In conclusion, the use of 3D bony reconstructions from CT scan data may offer a viable alternative to plain radiographs in the measurement of the CSA. The CT-based method is potentially advantageous for measurement of the CSA on 3D reconstructions and presurgical planning for acromioplasty, given the challenges associated with obtaining true AP radiographs.
The critical shoulder angle (CSA) is a radiological measure that assesses both glenoid inclination and acromial length, with higher values being associated with rotator cuff (RC) tears.
It is difficult to obtain a high-quality true anteroposterior (AP) radiograph of the shoulder, with any excess scapular version or flexion/extension resulting in deviation from the true CSA value. This may be overcome by using three-dimensional (3D) bony reconstructions from computed tomography (CT) shoulder scans, which can be rotated to replicate an ideal true AP view.
This study aimed to evaluate CSA measurements performed on 3D bony reconstructions of shoulder CT scans.
CSA measurements were performed on 3D bony reconstructions of shoulder CT scans and corresponding true AP radiographs. Measurements were performed by two observers, on two separate occasions.
There was a strong positive correlation between the two methods. Better intra-observer and inter-observer reliability was seen when using the 3D bony CT reconstructions to measure the CSA.
The use of 3D bony reconstructions from CT shoulder scans may offer a viable alternative to plain radiographs in the measurement of the CSA.
Future research should consider the use of 3D CT bony reconstructions in the preoperative evaluation of RC tears, particularly in the consideration of lateral acromioplasty as an adjunct to RC repair.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Australia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bian Q S-Editor: Zhang L L-Editor: Webster JR P-Editor: Xing YX
| 1. | Gerber C, Snedeker JG, Baumgartner D, Viehöfer AF. Supraspinatus tendon load during abduction is dependent on the size of the critical shoulder angle: A biomechanical analysis. J Orthop Res. 2014;32:952-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 172] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 2. | Moor BK, Bouaicha S, Rothenfluh DA, Sukthankar A, Gerber C. Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint? Bone Joint J. 2013;95-B:935-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 330] [Cited by in RCA: 392] [Article Influence: 32.7] [Reference Citation Analysis (0)] |
| 3. | Katthagen JC, Millett PJ. Editorial Commentary: Lateral Acromioplasty Is Clinically Safe and Has the Potential to Reduce the Risk for Rotator Cuff Re-tears. Arthroscopy. 2018;34:781-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Cherchi L, Ciornohac JF, Godet J, Clavert P, Kempf JF. Critical shoulder angle: Measurement reproducibility and correlation with rotator cuff tendon tears. Orthop Traumatol Surg Res. 2016;102:559-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 69] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 5. | Suter T, Gerber Popp A, Zhang Y, Zhang C, Tashjian RZ, Henninger HB. The influence of radiographic viewing perspective and demographics on the critical shoulder angle. J Shoulder Elbow Surg. 2015;24:e149-e158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 119] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 6. | Chalmers PN, Salazar D, Steger-May K, Chamberlain AM, Yamaguchi K, Keener JD. Does the Critical Shoulder Angle Correlate With Rotator Cuff Tear Progression? Clin Orthop Relat Res. 2017;475:1608-1617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 90] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 7. | Bouaicha S, Ehrmann C, Slankamenac K, Regan WD, Moor BK. Comparison of the critical shoulder angle in radiographs and computed tomography. Skeletal Radiol. 2014;43:1053-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Spiegl UJ, Horan MP, Smith SW, Ho CP, Millett PJ. The critical shoulder angle is associated with rotator cuff tears and shoulder osteoarthritis and is better assessed with radiographs over MRI. Knee Surg Sports Traumatol Arthrosc. 2016;24:2244-2251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 119] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 9. | Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32742] [Cited by in RCA: 32710] [Article Influence: 838.7] [Reference Citation Analysis (3)] |
| 10. | Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15:155-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9979] [Cited by in RCA: 15802] [Article Influence: 1755.8] [Reference Citation Analysis (0)] |
| 11. | Smith GCS, Liu V, Lam PH. The Critical Shoulder Angle Shows a Reciprocal Change in Magnitude When Evaluating Symptomatic Full-Thickness Rotator Cuff Tears Versus Primary Glenohumeral Osteoarthritis as Compared With Control Subjects: A Systematic Review and Meta-analysis. Arthroscopy. 2020;36:566-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Yi JW, Park HJ, Lee SY, Rho MH, Hong HP, Choi YJ, Kim MS. Radiation dose reduction in multidetector CT in fracture evaluation. Br J Radiol. 2017;90:20170240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Sheean AJ, Sa D, Woolnough T, Cognetti DJ, Kay J, Burkhart SS. Does an Increased Critical Shoulder Angle Affect Re-tear Rates and Clinical Outcomes Following Primary Rotator Cuff Repair? Arthroscopy. 2019;35:2938-2947.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Marchetti DC, Katthagen JC, Mikula JD, Montgomery SR, Tahal DS, Dahl KD, Turnbull TL, Millett PJ. Impact of Arthroscopic Lateral Acromioplasty on the Mechanical and Structural Integrity of the Lateral Deltoid Origin: A Cadaveric Study. Arthroscopy. 2017;33:511-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Katthagen JC, Marchetti DC, Tahal DS, Turnbull TL, Millett PJ. The Effects of Arthroscopic Lateral Acromioplasty on the Critical Shoulder Angle and the Anterolateral Deltoid Origin: An Anatomic Cadaveric Study. Arthroscopy. 2016;32:569-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 83] [Article Influence: 9.2] [Reference Citation Analysis (0)] |