Published online Apr 18, 2021. doi: 10.5312/wjo.v12.i4.223
Peer-review started: December 15, 2020
First decision: December 31, 2020
Revised: January 17, 2021
Accepted: March 10, 2021
Article in press: March 10, 2021
Published online: April 18, 2021
Processing time: 118 Days and 10.4 Hours
Previous studies have shown that non-surgical management can be an effective treatment strategy for many patients with rotator cuff tears. Despite the prevalence of rotator cuff disease, few studies have examined the patient and tear related factors that predict outcomes of nonsurgical management in this cohort of patients.
To identify factors that are associated with changes in patient reported outcomes over time in individuals with full-thickness rotator cuff tears treated without surgery.
A cohort of 59 patients who underwent non-surgical management of full thickness rotator cuff tears with a minimum of 1-year follow-up were identified from our institutional registry. Patient demographics, comorbidities and tear characteristics were collected at initial presentation. Outcome measures were collected at baseline and at each clinical follow-up, which included Western Ontario Rotator Cuff (WORC) index, American Shoulder and Elbow Surgeons score, Visual Analog Scale for pain and Single Assessment Numerical Evaluation. Multi- and univariate regression analyses were used to determine the impact of each patient and tear related variable on final WORC scores and change in WORC scores throughout the study.
In this non-surgical cohort, all patient-reported outcome measures significantly improved compared to baseline at 1 and 2-year follow-up. There was no significant difference in outcomes between 1 and 2 years. The average improvement surpassed the published minimal clinically important differences values for WORC, American Shoulder and Elbow Surgeons, Visual Analog Scale pain and Single Assessment Numerical Evaluation scores. Regression analysis identified female gender (β = - 19.88, P = 0.003), smoking (β = -29.98, P = 0.014) and significant subscapularis fatty infiltration (β = -15.35, P = 0.024) as predictors of less favorable WORC scores at 1 year, and female gender (β = -19.09, P = 0.015) alone as a predictor of lower WORC scores at 2 years. Patients with symptom duration greater than 1 year at presentation reported less improvement in WORC scores at 1-year follow-up (β = -14.63, P = 0.052) and patients with traumatic tears reported greater improvements in WORC scores at 2-year follow-up (β = 17.37, P = 0.031).
Patients with full thickness rotator cuff tears can achieve and maintain clinically meaningful benefit from non-surgical management through 2-year follow-up. Female patients, smokers, and those with significant subscapularis fatty infiltration tend to have lower overall WORC scores at 1-year follow-up, and females also have lower WORC scores at 2-year follow-up. Patients presenting with symptoms greater than 1 year had less clinical improvement at 1-year follow-up, and those with traumatic tears had greater clinical improvement at 2-year follow-up.
Core Tip: This clinical study examines the factors, both patient and tear-related, that predict patient reported outcome measures in a cohort of 59 patients with symptomatic, full-thickness rotator cuff tears who are treated non-surgically. All patients included in this study presented with magnetic resonance imaging scans which were used to measure several important characteristics including tear size, associated fatty infiltration and the supraspinatus tangent sign. Linear regression analyses were performed to determine which factors independently predicted patient reported outcome measures.
- Citation: Bush C, Gagnier JJ, Carpenter J, Bedi A, Miller B. Predictors of clinical outcomes after non-operative management of symptomatic full-thickness rotator cuff tears. World J Orthop 2021; 12(4): 223-233
- URL: https://www.wjgnet.com/2218-5836/full/v12/i4/223.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i4.223
Rotator cuff disease represents the most common etiology of shoulder dysfunction in the aging population, with an estimated 4.5 million physician office visits annually in the United States dedicated to its treatment[1,2]. The prevalence of rotator cuff disease increases with age, with over 60% of patients over the age of 80 exhibiting evidence of rotator cuff pathology[3]. Despite its prevalence, the ideal management of full-thickness rotator cuff tears has yet to be clearly defined. There have been several randomized controlled trials comparing surgical and non-surgical management of rotator cuff tears with conflicting results supporting both treatment options[4-6]. Although non-surgical management does not lead to rotator cuff healing, it has been shown to be an effective treatment option in many patients, leading to improvements in function and patient-reported outcomes[7-11].
Despite the generally positive outcomes, few studies have investigated the factors that predict outcomes after non-surgical management of rotator cuff tears. The Multicenter Orthopaedic Outcomes Network (MOON) shoulder group identified patient expectations related to physical therapy, smoking status and activity level to be predictive of outcomes in their prospective cohort of patients with full thickness rotator cuff tears[12]. Boorman et al[13] found that only the rotator cuff quality-of-life index predicted treatment failure in their non-surgical cohort. Both of these studies defined treatment failure as patients who decided to undergo surgical intervention.
The objective of this study was to identify patient characteristics at initial presentation that might be predictive of patient-reported outcomes after non-surgical management of full thickness rotator cuff tears.
This study was approved by our institutional review board. Patients who presented to our institution between 2009 and 2015 with full thickness rotator cuff tears were prospectively enrolled into our research registry. The inclusion criteria for this registry included patients at least 18 years old who were diagnosed with a full thickness rotator cuff tear proven by magnetic resonance imaging (MRI) or ultrasound. Exclusion criteria included patients with isolated subscapularis tears, those with a history of prior ipsilateral shoulder surgery, fracture, dislocation, infection, inflammatory joint disease, or those who had already undergone more than 4 wk of formal non-operative treatment modalities.
Baseline demographic data were obtained, including factors pertinent to rotator cuff pathology [age, sex, body mass index (BMI), smoking, diabetes]. Patients documented whether their symptoms were related to an injury (traumatic vs atraumatic) and how long their symptoms had been present. For the purpose of our analysis, symptom duration was categorized as less than 1 year and greater than 1 year.
Treatment allocation was determined by shared decision making between the surgeon and patient after a thorough clinical exam and discussion of the risks and benefits of operative and non-operative management. No specific criteria were formally utilized to determine the treatment arm, as each decision was individualized for the specific patient. A previous study by Kweon et al[14] analyzed this same patient registry and found that there were some patient factors which predicted allocation to surgical management, including younger age, lower BMI and duration of symptoms less than 1 year. Other relevant factors including sex, tear size, functional comorbidity score or any patient reported outcome measure were no predictive of treatment allocation in this same study. Patients who chose to pursue non-operative management in this registry were enrolled in formal physical therapy with a standardized rotator cuff rehabilitation protocol. This therapy involved shoulder stretching, rotator cuff resistance band strengthening and scapular stabilizing exercises. These patients were also treated with anti-inflammatory medications and occasional steroid injections as needed for pain control.
We identified 151 patients in the registry who underwent non-operative management with a minimum of 1-year follow-up. Fifty-nine of these patients had adequate pre-treatment imaging studies to evaluate rotator cuff muscle grading. Forty-three of the patients were followed for 2 years and the remaining 16 patients had 1 year of follow-up. Of note, there were a total of 316 patients in the registry treated for rotator cuff tears during this study period, signifying that 47.8% (151/316) of the total patients were treated non-operatively.
Upon enrollment into the registry, patients completed a demographic questionnaire as well as several patient-reported outcome measures including the Western Ontario Rotator Cuff (WORC) index[15], American Shoulder and Elbow Surgeons (ASES) score[16], Single Assessment Numerical Evaluation (SANE)[17] and Visual Analog Scale for pain[18]. The WORC index was used as the primary outcome measure for this study as it was developed and validated specifically for patients with rotator cuff tears[19]. The normalized version of the WORC index (WORCnorm) was utilized for this study, which converts the scores to a 0-100 point scale, with 100 representing the highest possible score. Outcome measures were collected at 6 and 12 mo, then at annual intervals. For the purpose of our study, the patients’ last documented outcome measures (either 1 or 2 years) were used as their final outcome.
All patients included in this study underwent an MRI with at least a 1.5T magnet. These MRI studies all included a T1 sagittal oblique sequence which was used to evaluate the rotator cuff musculature. The maximal anterior-posterior and medial-lateral dimensions of the rotator cuff tear were multiplied to obtain the cuff tear index (CTI)[20]. Of note, CTI was originally described using arthroscopic measurement techniques, but MRI based measurements were substituted in this non-surgical cohort. Fatty infiltration was graded on a scale of 0 to 4 as originally described in a computed tomography study by Goutallier et al[21]. Sagittal oblique T1 sequences were used to calculate the grade of fatty infiltration, as described in a subsequent MRI based study by Fuchs et al[22]. For the purpose of analysis, fatty infiltration was grouped by grades 0 and 1 vs grade 2 and higher. The supraspinatus tangent sign was also measured on this sequence, in accordance with the methods proposed by Zanetti et al[23]. MRI analysis was performed independently by two orthopaedic surgery sports medicine fellows, and any discrepancies between graders were resolved by an additional assessment performed by the senior author. Both inter-rater and intra-rater reliability were also assessed for this dataset and published previously by Naimark et al[24].
Descriptive and inferential statistics were analyzed using Statistic Package for Social Science v22.0 (IBM) and STATA/MP 14.2. Differences in patient reported outcome measures at each time point were obtained using univariate analysis of variance post-hoc testing using Tukey’s test was utilized to check for significant differences between specific time points. P values less than 0.05 were considered significant. Baseline demographic data are presented as the mean ± SD or a percentage within groups. An a priori power and sample size analysis using a moderate effect size estimate was calculated and produced a requirement of 21 patients for a power of 0.80 at 95%CI.
Linear regression analyses were conducted for all continuous dependent variable, change in the WORC score and total normalized WORC scores at 1 and 2-year follow-up. Predictor variables included gender, age, BMI, smoking status, diabetes, CTI, traumatic or atraumatic tears, duration of symptoms greater than or less than 1 year, tangent sign, infraspinatus fatty infiltration, and subscapularis fatty infiltration. Multivariable models were completed, then an elimination analysis was performed, removing the least significant variable each time before running the analysis again. This elimination analysis was continued until only statistically significant variables remained. P values less than 0.1 were considered significant.
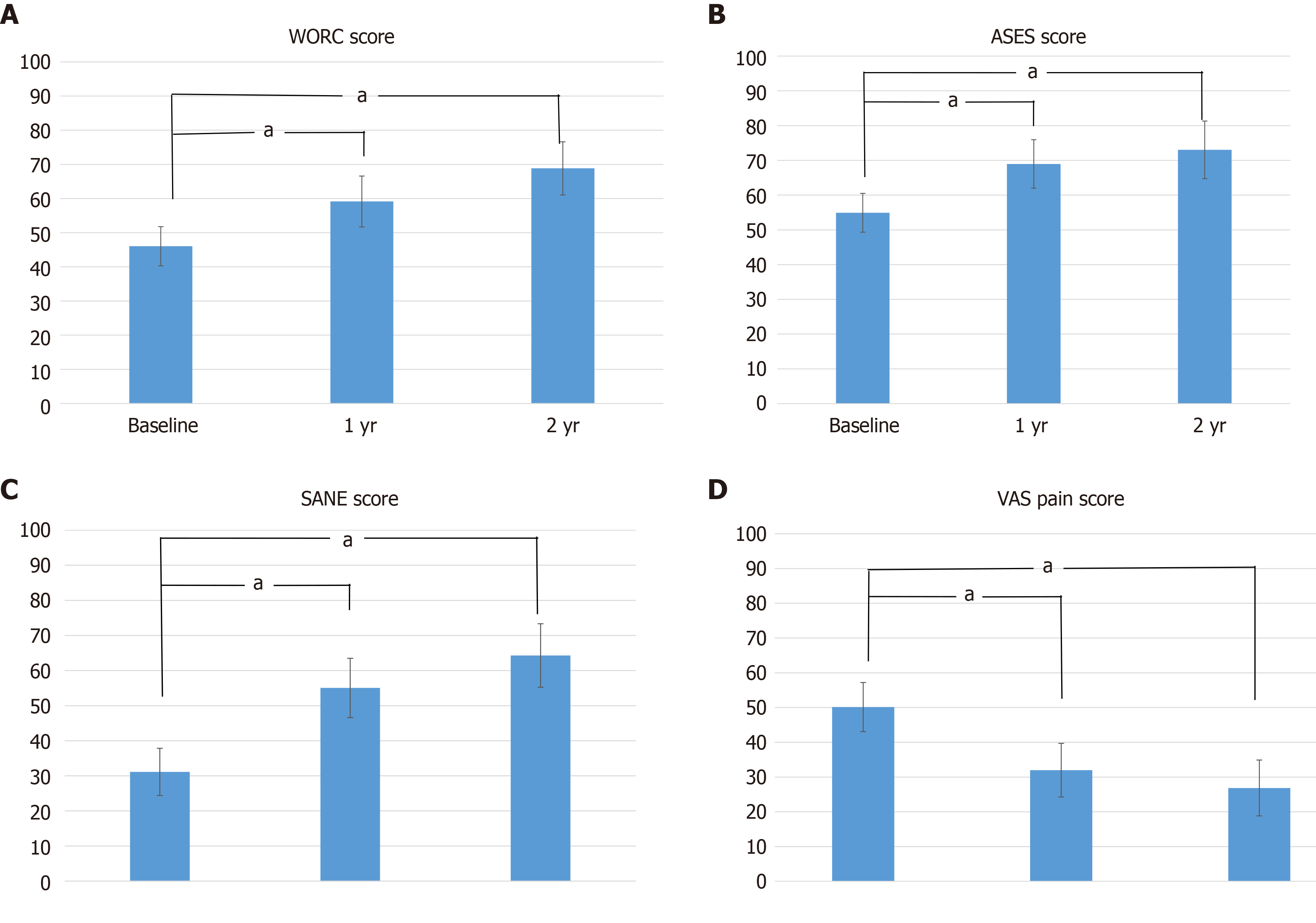
Fifty-nine patients met the inclusion criteria for this study. The baseline characteristics of these patients are displayed in Table 1. All patient-reported outcome measures improved over the course of the study compared to baseline values, as shown in Table 2. Statistically significant improvements were noted between baseline and 1 year and between baseline and 2-year outcomes. There was not a statistically significant improvement in any patient reported outcome between 1 and 2 years (Figure 1).
| Baseline characteristics | |
| Age | 63.85 ± 8.48 |
| Male, n (%) | 37 (62.71) |
| BMI | 29.63 ± 5.58 |
| CTI | 4.77 ± 4.47 |
| Diabetes, n (%) | 5 (8.47) |
| Smoking, n (%) | 4 (6.78) |
| Traumatic, n (%) | 40 (67.8) |
| Duration > 1 yr, n (%) | 17 (28.81) |
| Tangent sign, n (%) | 21 (35.59) |
| Supra FI ≥ 2, n (%) | 27 (45.76) |
| Infra FI ≥ 2, n (%) | 21 (35.59) |
| Subscap FI ≥ 2, n (%) | 20 (33.9) |
| ASES baseline | 54.91 ± 20.85 |
| SANE baseline | 31.13 ± 25.39 |
| WORCnorm baseline | 46.05 ± 21.61 |
| VAS pain baseline | 50.13 ± 26.39 |
| Baseline | Final follow-up | Change | |
| WORCnorm | 46.05 ± 21.61 | 63.58 ± 25.6 | 17.53 ± 6.87 |
| ASES | 54.91 ± 20.85 | 70.1 ± 25.03 | 15.19 ± 6.77 |
| SANE | 31.13 ± 25.39 | 59.4 ± 29.45 | 28.27 ± 7.41 |
| VAS pain | 50.13 ± 26.39 | 29.17 ± 26.68 | -20.96 ± 7.28 |
Multivariable linear regression models using final WORC scores at 1 and 2 years as the clinical outcome measure are shown in Table 3. At 1-year follow-up, female gender, smoking and advanced subscapularis fatty infiltration were found to be predictive of worse WORC scores. These factors predicted fairly substantial decreases of nearly 20, 29 and 15 points respectively. At 2-year follow-up, only female gender remained predictive of worse scores, with a similar decrease of 19 points on the normalized WORC score.
| β | P value | 95%CI | |
| 1 yr | |||
| Female gender | -19.88 | 0.003 | -32.82 to -6.95 |
| Smoking | -28.98 | 0.014 | -51.9 to -6.05 |
| Subscap FI ≥ 2 | -15.35 | 0.024 | -28.62 to -2.07 |
| 2 yr | |||
| Female gender | -19.09 | 0.015 | -34.26 to -3.92 |
In addition to analyzing final WORC scores, multivariable analyses were also performed using the overall change in WORC scores at 1 and 2 years compared to baseline values. These results are shown in Table 4. At 1-year follow-up, patients with chronic symptoms (> 1 year) were predicted to have significantly less improvement in WORC scores by nearly 15 points. At 2-year follow-up, patients with traumatic tears were predicted to have over a 19-point greater increase in WORC scores. Age was also found to be a significant predictor of worse WORC scores at 2-year follow-up, although not likely clinically significant with a β value of less than 1 point. The mean improvements in WORC score at 2-year follow-up for patients with traumatic vs atraumatic and acute vs chronic tears are shown in Table 5.
| β | P value | 95%CI | |
| 1 yr | |||
| Duration > 1 yr | -14.63 | 0.052 | -29.4 to 0.13 |
| 2 yr | |||
| Age | -0.82 | 0.08 | -1.75 to 0.10 |
| Traumatic | 19.06 | 0.017 | 3.65 to 34.48 |
| Mean | SD | 95%CI | |
| Traumatic | 26.82 | 27.3 | 16.39 to 37.25 |
| Atraumatic | 9.45 | 19.06 | -0.49 to 19.38 |
| Duration < 1 yr | 24.61 | 24.72 | 16.04 to 33.18 |
| Duration > 1 yr | 5.71 | 24.84 | -11.01 to 22.44 |
Few studies have examined the factors associated with positive patient-reported outcomes after non-surgical management of full thickness rotator cuff tears. In this study, we demonstrated that clinical outcome measures in a selected population of patients were significantly improved at 1 year. These results were durable at 2 years, with no statistically significant change between the 1 and 2-year follow-up. The average improvements in WORC, ASES, SANE and Visual Analog Scale pain scores all surpassed their published minimal clinically important differences (MCID) at final follow-up[25-27].
These results are consistent with previously published literature regarding non-surgical management of rotator cuff tears. Patients treated non-operatively in the MOON shoulder cohort were noted to have improvements of 22.5, 29.2 and 23.7 points in the WORC, ASES and SANE scores respectively, at 12-wk follow-up[10]. These are comparable to our cohort’s improvements of 17.5, 15.2 and 28.3 points on these same scales respectively.
Based on our multivariable regression analyses, female gender, smoking and significant subscapularis fatty infiltration were found to be predictors of worse clinical outcomes at 1-year follow-up in our primary outcome measure, the normalized WORC score. These variables were not only statistically significant, but also clinically significant with magnitude of change with β values ranging between 15 and 30 points (WORC MCID = 11.7). At 2-year follow-up only female gender remained a significant predictor of WORC scores, suggesting smoking status and subscapularis fatty infiltration may not be as clinically important for determining long-term prognosis.
Female gender has been shown in several other studies to negatively affect pain and clinical outcomes scores after rotator cuff repair surgery, however to our knowledge the same has not been shown in non-surgical cohorts[28-30]. This result may be further explained by the lower baseline WORC scores in females vs males in our cohort (35.5 vs 52.7), as the subsequent regression analyses evaluating change in WORC scores did not find female gender to be a predictor of less improvement throughout the study.
Smoking has also been shown in several studies to be a risk factor for worse clinical outcomes and decreased healing rates after rotator cuff repair[31-33]. In contrast, a study by Dunn et al[12] found that non-smokers were actually more likely to fail non-operative management of rotator cuff tears, however treatment success was defined as avoidance of surgical intervention rather than patient reported outcome measures. There may have been some selection bias introduced into this study outcome as well, as surgeons may have been more willing to offer surgery to non-smokers.
Although patients with isolated full thickness subscapularis tears were excluded from this study, over 1/3 of the patients in our cohort (20/59) did exhibit grade 2 or higher fatty infiltration in the subscapularis, indicating an anterosuperior variant rotator cuff tear. These tears have been associated with worse clinical outcomes in surgical cohorts in previous studies, especially when associated with higher grades of subscapularis fatty infiltration[34,35]. The results of our study mirror these results, with increased grades of subscapularis fatty infiltration portending worse WORC scores at 1-year follow-up.
In addition to the aforementioned factors that were predictive of final WORC scores in our study, we also analyzed the factors that impacted the amount of improvement patients achieved during the study period. We feel that both of these outcomes are worth examining, as they answer different clinical questions. Some patients may be more interested in the degree to which they will improve with a specific intervention rather than the final outcome they will achieve, and vice versa.
With this idea in mind, we performed additional regression analyses using the change in WORC score from baseline at 1 and 2-year follow-up as the clinical outcome measure. We found that patients presenting with symptom duration greater than 1 year achieved significantly less improvement at 1-year follow-up, and those with a traumatic onset of pain achieved significantly greater improvement at 2-year follow-up. Specifically, those with a traumatic onset of shoulder pain improved over 17 points more at 2-year follow-up than those with an atraumatic onset of pain, and those with symptoms less than 1 year at the onset of the study improved nearly 19-points more than those with symptoms greater than 1 year. Considering the MCID for normalized WORC scores has been published at 11.7 points, these variables predicted a fairly impactful magnitude of change.
The considerable effect of tear chronicity on improvement with non-surgical management may be explained by the idea that patients with long-standing symptoms have already gained some positive effects from some form of self-directed rehab, or simply by performing their day-to-day activities. These patients with chronic tears may have also developed some irreversible changes within their rotator cuff musculature, or within the glenohumeral joint itself due to altered mechanics. It is possible that these secondary changes may predispose them to worse outcomes with non-surgical management.
The explanation of the predictive impact of traumatic tears on the magnitude of improvement in this study is less clear. It may be theorized that patients with degenerative rotator cuff tears have a more diffuse underlying problem within the remainder of their intact cuff tendons, vs those who suffered acute traumatic tears. It may also be possible that there is an inherent difference in the population of patients who suffer a traumatic vs atraumatic tear, which may impact their ability to successfully rehab their ailing shoulders. Furthermore, there may be some overlap between tear mechanism and symptom duration at presentation. Specifically, those patients who sustain traumatic tears may be more likely to present for care acutely than those with an insidious onset of symptoms. An additional consideration is that while patients self-reported a traumatic onset of pain, many of these patients could have had pre-existing rotator cuff tears prior to these traumatic events. Their initial magnitude of symptom improvement may be related to resolution of pain related to temporary contusions or sprains related to these traumatic events. No pre-injury imaging studies exist in these patients to determine whether they truly suffered a traumatic rotator cuff tear, or simply trauma in the setting of an existing tear. These concepts warrant further investigation.
Several factors that have been identified as important predictors of outcomes in surgically managed rotator cuff tears, such as tear size, tangent sign, fatty infiltration in the posterosuperior cuff muscles, and diabetes, did not have an apparent impact on the outcomes of our non-surgical cohort[24,36,37]. Many of these factors may be related to tissue healing capacity, which presumably would be less critical in those patients being treated non-surgically. Other studies evaluating outcomes with non-operative management have also found these patient and tear related factors to be unrelated to clinical outcomes[12,13].
Our study was not without limitations. Although the data was collected prospectively, this study was retrospective in nature. Also, treatment allocation into this non-surgical cohort was not randomized. Patients had the ability to choose between surgical and non-surgical management, which could introduce some selection bias into the study. Outcomes of this cohort may not be entirely generalizable to all patients presenting with full thickness rotator cuff tears. The cohort included in this study was also smaller than other similar studies which included multiple centers, such as the MOON group studies[10,12]. Also, although many variables were included in the regression analyses as potential predictors of patient outcomes, other potentially significant factors may have been neglected, such as workers compensation status, tear retraction, or concomitant biceps tendon pathology. Also, standardized physical exam findings were not available for review, and could have impacted patient outcomes. Although fatty infiltration of the various rotator cuff muscles was used as a surrogate of tear location (i.e., anterosuperior vs posterosuperior), the specific location and tendons involved in each rotator cuff tear were not specifically categorized, which may have affected the interpretation of these tear subtypes. Other limitations include the lack if information regarding patient compliance with physical therapy and the lack of any follow up imaging studies to assess progression of tear size or fatty infiltration. These morphologic characteristics may be important when considering the long-term outcomes in these patients.
This study demonstrated that non-operative management of full thickness rotator cuff tears results in clinically meaningful and statistically significant improvements in patient reported outcome measures at 2-year follow-up. Female gender, smoking and advanced subscapularis fatty infiltration were predictive of lower WORC scores at 1-year follow-up; only female gender was predictive of lower WORC scores at 2-year follow-up. Patients with symptom duration greater than 1 year at presentation were found to have less improvement in WORC scores at 1-year follow-up, and those with traumatic tears demonstrated significantly greater improvements at 2-year follow-up. These outcome measures and patient related factors can be used to counsel patients with rotator cuff tears who are contemplating their treatment options.
Rotator cuff tears are extremely prevalent in the general population, and many patients with rotator cuff tears can be treated successfully without surgical intervention. Little data exists in the literature regarding patient and pathology related factors which predict the outcomes after nonsurgical management.
By evaluating the patient reported outcomes in a cohort of patients who underwent nonsurgical management for full-thickness rotator cuff tears, we hope to uncover important factors which may refine treatment indications for this subset of patients.
The objectives of this study were to evaluate the outcomes of nonsurgical management in patient with full thickness rotator cuff tears, and to identify patient and tear related characteristics which may predict outcomes. These findings could have a significant impact on the treatment of patients with rotator cuff tears in the future.
Patients in our institutional registry who underwent nonsurgical management for full thickness rotator cuff tears were identified. Pre-treatment magnetic resonance imaging scans were evaluated for tear size and related muscle atrophy and fatty infiltration. Patient reported outcomes were evaluated at 1 and 2 years after treatment began and regression analyses were performed in order to identify any predictors of patient reported outcomes in this cohort.
Patient reported outcome measures improved significantly at 1 and 2 year follow up after nonsurgical management. Patients who presented with chronic symptoms showed less improvement in patient reported outcome scores, and those with traumatic tears were noted to make greater improvements over the course of the study.
Patients with full thickness rotator cuff tears can achieve significant clinical improvement with nonsurgical management. Several factors may affect the amount of improvement they achieve, including the duration of their symptoms at presentation and the mechanism of their pain at the onset of symptoms. Additional factors likely exist that may impact patient outcomes in the setting of rotator cuff pathology.
Future studies should consider additional factors that may be relevant in predicting outcomes in patients with rotator cuff tears including pertinent physical exam findings and concomitant shoulder pathology such as biceps tendon involvement. Prospective comparative studies of surgical and nonsurgical management will also help clarify the ideal surgical and non-surgical indications in this cohort of patients.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen PC, Grassi FA S-Editor: Zhang L L-Editor: A P-Editor: Xing YX
| 1. | Chakravarty K, Webley M. Shoulder joint movement and its relationship to disability in the elderly. J Rheumatol. 1993;20:1359-1361. [PubMed] |
| 2. | Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res. 2007;455:52-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 253] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 3. | Teunis T, Lubberts B, Reilly BT, Ring D. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg. 2014;23:1913-1921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 383] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 4. | Kukkonen J, Joukainen A, Lehtinen J, Mattila KT, Tuominen EK, Kauko T, Äärimaa V. Treatment of Nontraumatic Rotator Cuff Tears: A Randomized Controlled Trial with Two Years of Clinical and Imaging Follow-up. J Bone Joint Surg Am. 2015;97:1729-1737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 153] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 5. | Lambers Heerspink FO, van Raay JJ, Koorevaar RC, van Eerden PJ, Westerbeek RE, van 't Riet E, van den Akker-Scheek I, Diercks RL. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. J Shoulder Elbow Surg. 2015;24:1274-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 117] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 6. | Moosmayer S, Lund G, Seljom U, Svege I, Hennig T, Tariq R, Smith HJ. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: A randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br. 2010;92:83-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 111] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 7. | Agout C, Berhouet J, Spiry C, Bonnevialle N, Joudet T, Favard L; French Arthroscopic Society. Functional outcomes after non-operative treatment of irreparable massive rotator cuff tears: Prospective multicenter study in 68 patients. Orthop Traumatol Surg Res. 2018;104:S189-S192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Boorman RS, More KD, Hollinshead RM, Wiley JP, Mohtadi NG, Lo IKY, Brett KR. What happens to patients when we do not repair their cuff tears? J Shoulder Elbow Surg. 2018;27:444-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 9. | Khatri C, Ahmed I, Parsons H, Smith NA, Lawrence TM, Modi CS, Drew SJ, Bhabra G, Parsons NR, Underwood M, Metcalfe AJ. The Natural History of Full-Thickness Rotator Cuff Tears in Randomized Controlled Trials: A Systematic Review and Meta-analysis. Am J Sports Med. 2019;47:1734-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 10. | Kuhn JE, Dunn WR, Sanders R, An Q, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW; MOON Shoulder Group. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013;22:1371-1379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 238] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 11. | Zingg PO, Jost B, Sukthankar A, Buhler M, Pfirrmann CW, Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am. 2007;89:1928-1934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 130] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 12. | Dunn WR, Kuhn JE, Sanders R, An Q, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Harrell F, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW; MOON Shoulder Group. 2013 Neer Award: predictors of failure of nonoperative treatment of chronic, symptomatic, full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2016;25:1303-1311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 97] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 13. | Boorman RS, More KD, Hollinshead RM, Wiley JP, Brett K, Mohtadi NG, Nelson AA, Lo IK, Bryant D. The rotator cuff quality-of-life index predicts the outcome of nonoperative treatment of patients with a chronic rotator cuff tear. J Bone Joint Surg Am. 2014;96:1883-1888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Kweon C, Gagnier JJ, Robbins CB, Bedi A, Carpenter JE, Miller BS. Surgical Versus Nonsurgical Management of Rotator Cuff Tears: Predictors of Treatment Allocation. Am J Sports Med. 2015;43:2368-2372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: The Western Ontario Rotator Cuff Index. Clin J Sport Med. 2003;13:84-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 344] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 16. | Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, Iannotti JP, Mow VC, Sidles JA, Zuckerman JD. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1180] [Cited by in RCA: 1266] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 17. | Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27:214-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 468] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 18. | Huskisson EC. Measurement of pain. Lancet. 1974;2:1127-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2733] [Cited by in RCA: 2718] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 19. | de Witte PB, Henseler JF, Nagels J, Vliet Vlieland TP, Nelissen RG. The Western Ontario rotator cuff index in rotator cuff disease patients: a comprehensive reliability and responsiveness validation study. Am J Sports Med. 2012;40:1611-1619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 69] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 20. | Tauro JC. Arthroscopic repair of large rotator cuff tears using the interval slide technique. Arthroscopy. 2004;20:13-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 47] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty infiltration of disrupted rotator cuff muscles. Rev Rhum Engl Ed. 1995;62:415-422. [PubMed] |
| 22. | Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography vs magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 968] [Cited by in RCA: 1037] [Article Influence: 39.9] [Reference Citation Analysis (0)] |
| 23. | Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998;33:163-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 358] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 24. | Naimark M, Trinh T, Robbins C, Rodoni B, Carpenter J, Bedi A, Miller B. Effect of Muscle Quality on Operative and Nonoperative Treatment of Rotator Cuff Tears. Orthop J Sports Med. 2019;7:2325967119863010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Cvetanovich GL, Gowd AK, Liu JN, Nwachukwu BU, Cabarcas BC, Cole BJ, Forsythe B, Romeo AA, Verma NN. Establishing clinically significant outcome after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2019;28:939-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 229] [Article Influence: 38.2] [Reference Citation Analysis (0)] |
| 26. | Kirkley A, Griffin S, Dainty K. Scoring systems for the functional assessment of the shoulder. Arthroscopy. 2003;19:1109-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 366] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 27. | Tashjian RZ, Hung M, Keener JD, Bowen RC, McAllister J, Chen W, Ebersole G, Granger EK, Chamberlain AM. Determining the minimal clinically important difference for the American Shoulder and Elbow Surgeons score, Simple Shoulder Test, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:144-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 303] [Article Influence: 37.9] [Reference Citation Analysis (0)] |
| 28. | Cho CH, Ye HU, Jung JW, Lee YK. Gender Affects Early Postoperative Outcomes of Rotator Cuff Repair. Clin Orthop Surg. 2015;7:234-240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 29. | Daniels SD, Stewart CM, Garvey KD, Brook EM, Higgins LD, Matzkin EG. Sex-Based Differences in Patient-Reported Outcomes After Arthroscopic Rotator Cuff Repair. Orthop J Sports Med. 2019;7:2325967119881959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 30. | Razmjou H, Davis AM, Jaglal SB, Holtby R, Richards RR. Disability and satisfaction after rotator cuff decompression or repair: a sex and gender analysis. BMC Musculoskelet Disord. 2011;12:66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 31. | Mallon WJ, Misamore G, Snead DS, Denton P. The impact of preoperative smoking habits on the results of rotator cuff repair. J Shoulder Elbow Surg. 2004;13:129-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 143] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 32. | Naimark M, Robbins CB, Gagnier JJ, Landfair G, Carpenter J, Bedi A, Miller BS. Impact of smoking on patient outcomes after arthroscopic rotator cuff repair. BMJ Open Sport Exerc Med. 2018;4:e000416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 33. | Neyton L, Godenèche A, Nové-Josserand L, Carrillon Y, Cléchet J, Hardy MB. Arthroscopic suture-bridge repair for small to medium size supraspinatus tear: healing rate and retear pattern. Arthroscopy. 2013;29:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 102] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 34. | Maqdes A, Abarca J, Moraiti C, Boughebri O, Dib C, Leclère FM, Kany J, Elkolti K, Garret J, Katz D, Valenti P. Does preoperative subscapularis fatty muscle infiltration really matter in anterosuperior rotator cuff tears repair outcomes? Orthop Traumatol Surg Res. 2014;100:485-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Millett PJ, Horan MP, Maland KE, Hawkins RJ. Long-term survivorship and outcomes after surgical repair of full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2011;20:591-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 36. | Cho NS, Rhee YG. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg. 2009;1:96-104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 133] [Cited by in RCA: 164] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 37. | Clement ND, Hallett A, MacDonald D, Howie C, McBirnie J. Does diabetes affect outcome after arthroscopic repair of the rotator cuff? J Bone Joint Surg Br. 2010;92:1112-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 73] [Article Influence: 4.9] [Reference Citation Analysis (0)] |