Published online Apr 18, 2021. doi: 10.5312/wjo.v12.i4.207
Peer-review started: January 2, 2021
First decision: January 18, 2021
Revised: January 27, 2021
Accepted: March 8, 2021
Article in press: March 8, 2021
Published online: April 18, 2021
Processing time: 100 Days and 4.2 Hours
Fracture of an ossification of the Achilles tendon (OAT) is a rare entity, and its etiology, pathology, and treatment remain unclear. We reviewed and scrutinized 18 cases (16 articles) of the fracture of an OAT. The most common etiologies of the ossifications include previous surgery and trauma. The fractures often occur without any trigger or with minimal trigger. The long, > 5 cm, ossification in the body of the Achilles tendon may have a higher risk of fracture. The OAT itself is often asymptomatic; however, its fracture causes severe local pain, swelling, and weakness of plantar flexion, which forces patients to undergo aggressive treatments. Regarding the treatments of the fractures, nonoperative treatment by immobilizing ankle joint could be an option for elderly patients. However, because it often cannot produce satisfactory results in younger patients, surgical treatment is typically recommended. Excision of the fractured mass and repairing the tendon is applicable if the remnant is enough. If there is a defect after the excision, reconstruction with autologous grafts or adjacent tendon transfer is performed. Gastrocnemius fascia turndown flap, hamstring tendon and tensor fascia lata are used as autologous grafts, whereas peroneus brevis and flexor hallucis longus tendons are used for the tendon transfer. If the fracture of an OAT is treated properly, the functional result will be satisfactory.
Core Tip: This review paper aims to provide an overview of the fracture of an ossification of the Achilles tendon. This fracture is distinct in that it occurs with minimal or no triggers. Nonoperative treatments may offer acceptable results for the elderly; however, surgeries should be recommended in younger patients. Following excision of the fractured mass, repairing the tendon is only applicable if the remnant is enough. If there is a defect after the excision, reconstruction with auto
- Citation: Ishikura H, Fukui N, Iwasawa M, Ohashi S, Tanaka T, Tanaka S. Fracture of ossified Achilles tendons: A review of cases. World J Orthop 2021; 12(4): 207-213
- URL: https://www.wjgnet.com/2218-5836/full/v12/i4/207.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i4.207
Ossification of the Achilles tendon (OAT) is a rare entity. Among them, fracture of an OAT (FOAT) is exceptionally rare. Therefore, perspectives of the etiology, pathology, and the treatment of the FOAT have not yet been unified. This review aims to summarize and evaluate the current literature on the FOAT and describe current concept of etiology, pathology, and treatment of this condition.
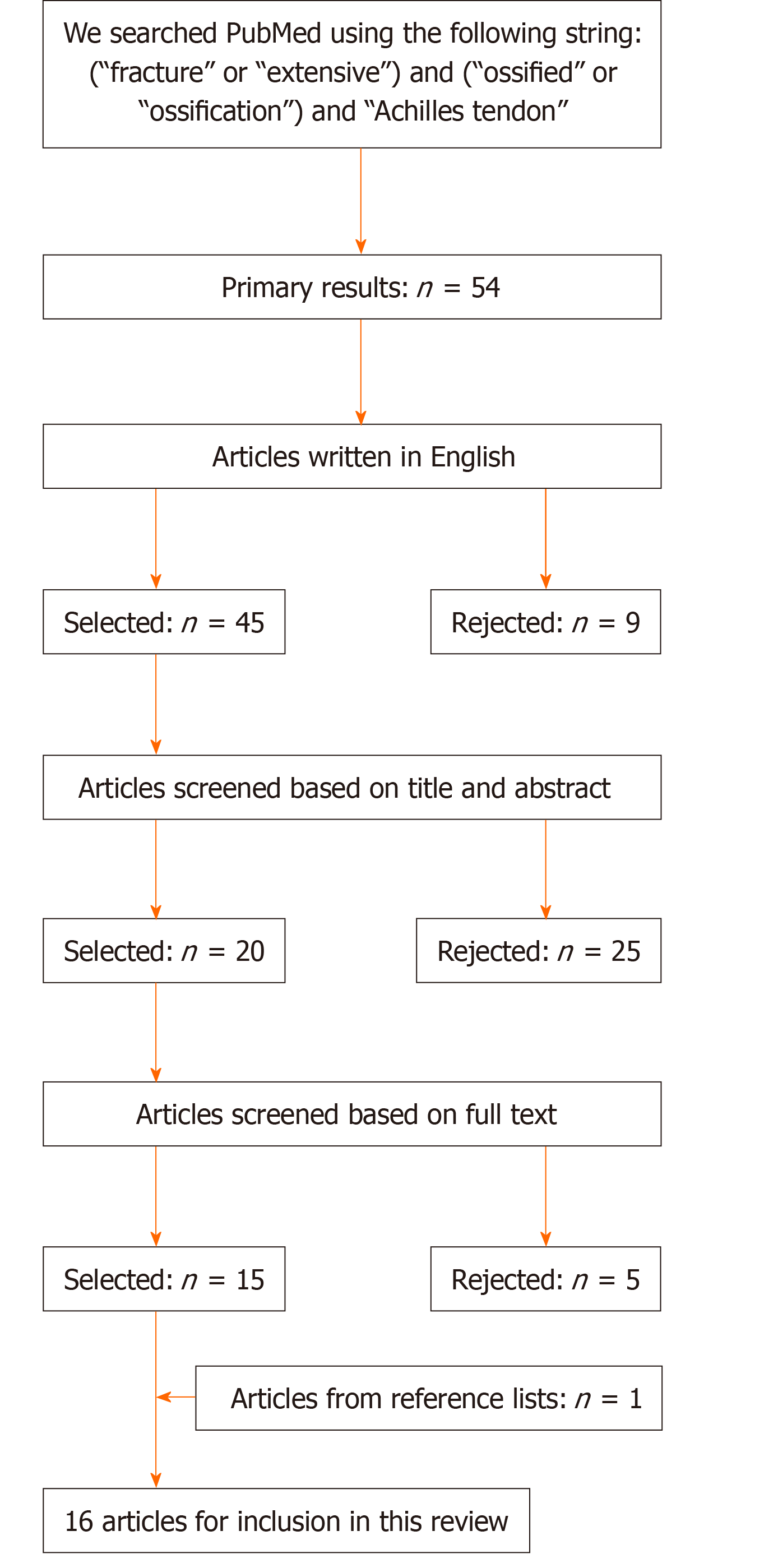
Systematic searches of PubMed were performed in August 2020 to identify studies relating to FOAT. The outline of the search strategy is shown in Figure 1. First, we identified 54 relevant articles by using the specified terms shown in Figure 1. Second, we excluded the articles which were not written in English. Third, articles were screened based on their title and abstract. Fourth, articles were further screened based on the full text and those that described the FOAT cases were selected. Finally, we scrutinized the reference lists of the included 15 articles and added one proper article. As a result, we identified 16 articles. All of them were case reports and included cases of 18 fractures in 16 patients (two patients had the fracture on both sides[1,2]). We show the summary of all the 16 articles in Table 1.
| Ref. | Patient | Size | Cause of ossification | Onset of fracture | Treatment | Histology | Follow-up period | Result | |||
| Age | Sex | Previous trauma | Previous surgery | Other factors | |||||||
| Lotke[1] (1970) | 61 | F | NA | - | + | - | Standing at the sink | Surgery (excision and repairing the tendon) | Mature bone with fibrosis of the marrow space | 15 mo | Good |
| 66 | F | NA | - | + | - | Unspecified | Surgery (excision and repairing the tendon) | Mature bone with fibrosis of the marrow space | 12 mo | Good | |
| Weseley et al[11] (1976) | 58 | M | NA | - | + | - | None (spontaneous occurrence) | Nonoperative (immobilization for 6 wk)→Surgery (excision and transferring peroneus brevis) | Mature bone | 3.5 mo | Nonoperative: poor; surgery: good |
| Brotherton and Ball[14] (1979) | 71 | M | 12.5 cm | + | - | - | Walking uneven ground | Surgery (reduction and holding with a figure of eight wire) | Partly woven and partly lamellar bone, forming a cancellous structure | 4 mo | NA |
| Fink and Corn[8] (1982) | 42 | F | 8 cm | - | - | Hypertension, hypothyroidism, obesity | Stumbling on level ground | Surgery (excision and reconstruction with gastrocnemius fascia flap) | NA | 4 mo | Good |
| Kernohan and Hall[17] (1984) | 64 | M | 20 cm | - | - | Manual worker | NA | Surgery (Achilles tendon graft interposition) | NA | 5 mo | Good |
| Suso et al[16] (1988) | 20 | M | 10 cm | - | - | Long-distance runner | Long-distance run | Surgery (excision and direct repair) | Bony trabeculae, separated by fibrous tissue areas | 3 mo | Good |
| Resnik and Foster[10] (1990) | 36 | M | NA | - | + | - | Stepping in a hole | Nonoperative (immobilization for 6 wk)→Surgery (excision and reconstruction with tensor fascia lata graft) | NA | NA | Nonoperative: poor; surgery: good |
| Friedman[13] (1991) | 41 | F | NA | + | - | - | Twisting the ankle | Surgery (excision, unspecified) | NA | NA | Good |
| Goyal and Vadhva[3] (1997) | 84 | M | 6 cm | - | + | - | Crossing a road | Nonoperative (immobilization for 12 wk) | NA | 12 mo | Good |
| Aksoy and Surat[6] (1998) | 44 | M | 7 cm | + | - | - | Climbing upstairs | Surgery (excision and reconstruction with proximal Achilles tendon flap) | NA | 24 mo | Good |
| Parton et al[5] (1998) | 84 | M | NA | - | + | - | Hurrying across a crossing | Nonoperative (immobilization for 8 wk) | NA | 3 mo | Good |
| Haddad et al[15] (1999) | 67 | F | NA | - | - | Hypertension, obesity | Tripping in the garden | Nonoperative (immobilization for 6 wk) | NA | 6 mo | Good |
| Mády and Vajda[2] (2000) | 57 | M | 5 cm (bilateral) | - | - | History of treatment for clubfeet by serial plaster casts | None (spontaneous occurrence) | Surgery (interosseous polydioxanone suture which was reinforced by a local tendon flap) | Mature osseous tissue | 84 mo | Good |
| Battaglia and Chandler[12] (2006) | 55 | M | NA | + | - | Hypertension, dyslipidemia | Strained while pruning a tree | Nonoperative (immobilization for 12 wk)→Surgery (excision and transferring flexor hallucis longus) | Osseous composition | 6 mo | Nonoperative: poor; surgery: good |
| Ishikura et al[9] (2015) | 50 | F | 14 cm | + | - | - | Climbing upstairs | Surgery (excision and reconstruction with hamstring tendon graft and gastrocnemius fascia flap) | Lamellar bone, which is covered by a number of osteoblasts in some areas | 12 mo | Good |
| Gendera et al[18] (2020) | 70 | M | 12 cm | - | + | - | None (spontaneous occurrence) | Surgery (excision and reconstruction with fascia lata graft) | Broad trabeculae of lamellar bone tissue with vital osteocytes | 12 mo | Good |
Past studies revealed that OAT occurred more frequently in men than in women[1,3,4]. Although the exact mechanism of ossification is unclear, the most commonly known etiologies are previous trauma and surgery[4]. In addition, infectious, metabolic, and systemic diseases such as syphilis, gastrocnemius abscess, osteomyelitis of the calcaneum, gout, diabetes, Wilson’s disease, ochronosis, diffuse idiopathic skeletal hyperostosis, Reiter’s syndrome, and ankylosing spondylitis may also cause ossification[3,5-9].
Only a small number of patients with OAT experience the FOAT. We show the summary of all the FOAT cases in Table 1. Etiologies of FOAT are similar to those of OAT. Among the 16 patients with the FOAT, 10 were men and 6 were women. Six patients had a history of previous surgery and 5 had a history of previous trauma. Among the 6 cases, who had experienced previous surgeries, the most common underlying cause was talipes equinovarus (5 cases)[1-3,5,10], followed by poliomyelitis (1 case)[11]. Achilles tendon rupture[12], ankle dislocation[9], distal tibial fracture[13], deep laceration of the calf[6] and soft tissue injury of the calf[14] were described as the details of the previous trauma.
As for the patients who had no previous trauma or surgery, an obese person[15], a long-distance runner[16] and a manual worker[17] were included in the cases examined. The repetitive stresses from the overweight or overload might have led to the OAT. In that sense, repetitive stresses through obesity or an overactive state might be included in the concept of “previous trauma.”
The mean period between the previous trauma or surgery and the occurrence of FOAT was 44.3 ± 20.8 years (n = 10, 15-78 years). This implies it takes a considerable amount of time for the ossification to grow big enough to fracture.
According to the previous reports about the OAT, a variety of sizes have been reported[4]. However, as for the FOAT, the length is 5 cm or more in all the mentioned cases[2,3,6,8,9,14,16-18].
OAT can occur in the body of the tendon or at its insertion into the calcaneus[1,4,6,14]. In the cases reviewed, the site of ossification could be detected by plain radiographs in 15 cases. The ossifications were located within the body of the tendon in 13 cases. In the remaining 2 cases, the ossification was present at the insertion of the calcaneus[12,15].
Considering these tendencies, ossifications in the body of the Achilles tendon that are > 5 cm long may have a higher risk of fracture. However, additional studies are needed to confirm this hypothesis.
In general, rupture of an unaffected Achilles tendon occurs in sports with abrupt repetitive jumping and sprinting activities[19]. By contrast, FOAT occurs without any trigger or with minimal trigger such as climbing upstairs and crossing a road[2,3,6,9,11,18]. This fact probably reflects the fragility of the OAT. This fragility may be attributable to its histological structure described in the “Histology of FOAT” section.
Although an OAT is usually asymptomatic[10,12], it can sometimes cause pain if the inflammation exists around the ossified area[4]. Meanwhile, once the ossified mass fractures, it causes symptoms including severe local pain, swelling, and weakness of plantar flexion[10,12]. Therefore, if the patients with an OAT suddenly experience pain, a fracture should be suspected[14].
As for the physical examination, it should be noted that Thompson calf squeeze test is sometimes negative despite the presence of the fracture[12,17]. It is probably because of the retained continuity of Achilles tendon component around the fractured ossification. Therefore, plain radiographs should be used to obtain precise diagnosis. Magnetic resonance imaging is also used to evaluate the hemorrhage, edema, and soft tissue condition around the fracture site[5,9].
According to previous reports, FOAT is treated either nonoperatively or surgically. In elderly patients, the nonoperative treatments are one of the options, because it can bring satisfactory results in some cases[3,5,15]. However, in 3 cases of younger patients, it has not produced the desired functional outcome. Resnik and Foster[10] reported a case of a 36-year-old man who underwent nonoperative treatment for FOAT but experienced persistent pain and swelling even after the treatment. He eventually underwent surgical excision of the bony mass and tendon reconstruction. Weseley et al[11] and Battaglia and Chandler[12] reported similar cases of male patients in their 50s who experienced failure of the nonoperative treatment modality and, subsequently, underwent the surgical treatment. Given these results, only limited outcomes should be expected from nonoperative treatment modalities, particularly in younger patients.
The surgical procedures for the treatment of the FOAT include internal fixation[2,14] and excision of the fractured mass, followed by the reconstruction with autografts[6,8-10,18] or adjacent tendon transfer[11,12]. Although internal fixation of the fractured mass reportedly offers the prospect of bone union[2,14], the applicable cases should be limited because this treatment does not eradicate the risk of non-union and refracture. Meanwhile, when the fractured mass was excised, diverse procedures have been conducted to cover the defect. If the ossification does not involve all layers of the Achilles tendon, direct repair of the tendon could be applicable[1,16]. However, if the ossification has infiltrated almost all layers of the tendon and there is a defect after excision, various kinds of grafts including gastrocnemius fascia turndown flap, hamstring tendon and tensor fascia lata grafts have been used to cover the defect[6,8-10,18]. For the adjacent tendon transfer, the peroneus brevis and flexor hallucis longus tendons have been used[11,12].
These procedures of reconstruction are also performed to treat chronic Achilles tendon ruptures[20-23].
Ossification, not calcification, typically accounts for a great majority of patients with Achilles tendon mineralization[4]. This tendency is consistent with our FOAT cases. All the patients whose histological appearances were available in this study showed bone tissues instead of calcification[1,2,9,11,12,14,16,18]. Lamellar bone, or combination of lamellar bone and woven bone was reported. In one of the cases examined here, histological sections stained with hematoxylin and eosin revealed that the tendon tissue underwent cartilaginous metaplasia and was gradually replaced by lamellar bone, which is surrounded by a number of osteoblasts[9]. These histological findings suggest the occurrence of endochondral ossification, which is consistent with the observation of heterotopic ossifications in other studies[24,25]. In that sense, histology of FOAT is quite similar to that of the heterotopic ossification. However, in our FOAT cases, the bone structures are often separated by fibrous tissues[1,16]. Such a mixed structure may be responsible for its fragility and this might be the distinct feature of FOAT. Given this histological finding, leaving the ossified mass in the FOAT patients may entail the risk of refracture. Therefore, the fundamentals of treating FOAT should include excision of the ossified mass as much as possible, followed by repairing or reconstructing the tendons. Past studies also reported the cases describing the combination of endochondral and intermembranous ossification[26,27]. However, the exact mechanism of the ossification in the FOAT patients were not suggested in many cases. Further studies are needed to accumulate the histological findings and elicit the exact mechanism of the ossification and its fracture.
This review provides an overview of the FOAT. Many of the affected patients had a history of previous surgery or trauma. This fracture is distinct in that it occurs without any triggers or with minimal triggers. Nonoperative treatments offer only limited effects and surgeries are often performed. When the fractured mass was excised, repairing the tendon is applicable if the remnant is enough. If there is a defect after the excision, reconstruction with autografts or adjacent tendon transfer is performed. Treated properly, the functional result will be satisfactory.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Buckley R S-Editor: Gao CC L-Editor: A P-Editor: Xing YX
| 1. | Lotke PA. Ossification of the Achilles tendon. Report of seven cases. J Bone Joint Surg Am. 1970;52:157-160. [PubMed] |
| 2. | Mády F, Vajda A. Bilateral ossification in the Achilles tendon: a case report. Foot Ankle Int. 2000;21:1015-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Goyal S, Vadhva M. Fracture of ossified Achilles tendon. Arch Orthop Trauma Surg. 1997;116:312-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Richards PJ, Braid JC, Carmont MR, Maffulli N. Achilles tendon ossification: pathology, imaging and aetiology. Disabil Rehabil. 2008;30:1651-1665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Parton MJ, Walter DF, Ritchie DA, Luke LC. Case report: Fracture of an ossified Achilles tendon - MR appearances. Clin Radiol. 1998;53:538-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Aksoy MC, Surat A. Fracture of the ossified Achilles tendon. Acta Orthop Belg. 1998;64:418-421. [PubMed] |
| 7. | Yu JS, Witte D, Resnick D, Pogue W. Ossification of the Achilles tendon: imaging abnormalities in 12 patients. Skeletal Radiol. 1994;23:127-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Fink RJ, Corn RC. Fracture of an ossified Achilles tendon. Clin Orthop Relat Res. 1982: 148-150. [PubMed] |
| 9. | Ishikura H, Fukui N, Takamure H, Ohashi S, Iwasawa M, Takagi K, Horita A, Saito I, Mori T. Successful treatment of a fracture of a huge Achilles tendon ossification with autologous hamstring tendon graft and gastrocnemius fascia flap: a case report. BMC Musculoskelet Disord. 2015;16:365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Resnik CS, Foster WC. Achilles tendon ossification and fracture. Can Assoc Radiol J. 1990;41:153-154. [PubMed] |
| 11. | Weseley MS, Barenfeld PA, Eisenstein AL. Fracture of an ossific mass in the Achilles tendon. Bull Hosp Joint Dis. 1976;37:159-163. [PubMed] |
| 12. | Battaglia TC, Chandler JT. Ossific tendonitis of the achilles with tendon fracture. Orthopedics. 2006;29:453-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Friedman L. Achilles tendon ossification and fracture. S Afr Med J. 1991;79:170. [PubMed] |
| 14. | Brotherton BJ, Ball J. Fracture of an ossified Achilles tendon. Injury. 1979;10:245-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Haddad FS, Ting P, Goddard NJ. Successful non-operative management of an Achilles fracture. J R Soc Med. 1999;92:85-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Suso S, Peidro L, Ramon R. Fracture of an ossification of the tendo calcaneus. Acta Orthop Belg. 1988;54:391-393. [PubMed] |
| 17. | Kernohan J, Hall AJ. Treatment of a fractured ossified Achilles tendon. J R Coll Surg Edinb. 1984;29:263. [PubMed] |
| 18. | Gendera HAM, Lambers-Heerspink FO, Bruls VE, Drees MMW. Extensive Achilles tendon ossification: Repair using a fascia lata graft. Foot (Edinb). 2020;43:101663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Egger AC, Berkowitz MJ. Achilles tendon injuries. Curr Rev Musculoskelet Med. 2017;10:72-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 113] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 20. | Zhang X, Ruan F, Wu Y, Lu H. Chronic bilateral asynchronous achilles tendon rupture treated using modified whole flexor hallucis longus transfer reconstruction: A case report. Medicine (Baltimore). 2020;99:e21742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Jiang XJ, Shen JJ, Huang JF, Tong PJ. Reconstruction of Myerson type III chronic Achilles tendon ruptures using semitendinosus tendon and gracilis tendon autograft. J Orthop Surg (Hong Kong). 2019;27:2309499019832717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Song YJ, Chen G, Jia SH, Xu WB, Hua YH. Good outcomes at mid-term following the reconstruction of chronic Achilles tendon rupture with semitendinosus allograft. Knee Surg Sports Traumatol Arthrosc. 2020;28:1619-1624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Wegrzyn J, Luciani JF, Philippot R, Brunet-Guedj E, Moyen B, Besse JL. Chronic Achilles tendon rupture reconstruction using a modified flexor hallucis longus transfer. Int Orthop. 2010;34:1187-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 93] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Postacchini F, Di Castro A. Subtotal ossification of the Achilles tendon. Case report. Ital J Orthop Traumatol. 1983;9:529-532. [PubMed] |
| 25. | Zhang Q, Zhou D, Wang H, Tan J. Heterotopic ossification of tendon and ligament. J Cell Mol Med. 2020;24:5428-5437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 26. | Hatori M, Kita A, Hashimoto Y, Watanabe N, Sakurai M. Ossification of the Achilles tendon: a case report. Foot Ankle Int. 1994;15:44-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Hatori M, Matsuda M, Kokubun S. Ossification of Achilles tendon--report of three cases. Arch Orthop Trauma Surg. 2002;122:414-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |