Published online Dec 18, 2021. doi: 10.5312/wjo.v12.i12.991
Peer-review started: April 23, 2021
First decision: June 16, 2021
Revised: June 28, 2021
Accepted: December 8, 2021
Article in press: December 8, 2021
Published online: December 18, 2021
Processing time: 234 Days and 10.3 Hours
Rotator cuff (RC) tears are one of the most frequent pathologies within the shoulder girdle. Hand dominance and older age are associated with RC tears. Two different surgical procedures, the mini-open (MO) and all-arthroscopic (AA) approach, represented the standard of treatment.
To compare the clinical and biomechanical outcomes of two surgical techniques (AA vs MO procedure) performed to address the painful shoulder syndrome with partial or total supraspinatus tendon tear.
Eighty-eight participants, 50 following RC repair with AA and 38 with MO approach, were recruited in the present cross-sectional case-control study (ORTHO-SHOULDER, Prot. 0054602). All patients underwent postoperative clinical evaluation for pain (Visual analogic scale), impairment, and disability (disability of the arm, shoulder, and hand) and limitation in daily activity (Constant-Murley score). Patients’ shoulder mobility was also assessed in our Laboratory of Functional Movement through a wearable inertial sensor and surface electromyography to monitor kinematics and muscle activity during the movement on the frontal (abduction/adduction) and sagittal (flexion-extension) planes.
No statistically significant differences between the two procedures were observed in either main clinical score or range of motion. A significant increase in velocity during the movement execution and a higher contribution of upper trapezius muscles were found in the AA group compared with MO patients.
In terms of clinical scores, our findings were in line with previous results. However, the use of technology-based assessment of shoulder mobility has revealed significant differences between the two techniques in terms of mean velocity and pattern of muscle activation.
Core Tip: Wearable technologies could be useful in clinical practice since they could provide clinical information during the performance of a motor task. The present work represents a preliminary attempt in making use of novel wearable technologies in common clinical practice.
- Citation: Solarino G, Bortone I, Vicenti G, Bizzoca D, Coviello M, Maccagnano G, Moretti B, D'Angelo F. Role of biomechanical assessment in rotator cuff tear repair: Arthroscopic vs mini-open approach. World J Orthop 2021; 12(12): 991-1000
- URL: https://www.wjgnet.com/2218-5836/full/v12/i12/991.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i12.991
An important group of the population suffers from shoulder pain due to acute or chronic tendon injuries. It is becoming a considerable cause of work disability. Rotator cuff tendinopathy and tears (RCTs) are the most common lesions. After the supraspinatus tendon, the most common injured structure of the rotator cuff (RC) complex, the biceps tendon is the second most commonly injured structure, as it is an element of compensation of the abnormal forces. Biceps’ tears predispose the patient’s rotator cuff to subsequent instability and further subscapularis tendon tears. Multi-tendon shoulder injuries, moreover, complicate the process of diagnosis, treatment, and rehabilitation[1,2]. The overall prevalence of RC abnormalities, regardless of symptoms, ranged from 9.7% in patients younger than or equal to 20 years and increased to 62% in patients aged 80 years and older (P < 0.001)[3]. Many RCTs also cause restriction of shoulder function. Surgical repair of the RC is a cost-effective solution for all populations and reduces the societal burden of the disease. The choice of surgery varies from surgeon-to-surgeon with arthroscopy more common at the present time. Mini-open (MO) technique has represented the gold standard for years, with a 90% success rate[4], since it guaranteed stronger suture fixation and a shorter learning curve[5]. However, the development of dedicated surgical instruments and improvement of the surgical technique have allowed surgeons to perform all-arthroscopic (AA) techniques in rotator cuff repair surgery[6]. The ideal repair of the RC tear must have the potential to withstand physiological loads while allowing simultaneous healing to occur. Currently, no significant superiority of one procedure has been demonstrated over the other[3,7,8], although RCTs in evaluating short- and long-term outcomes of both approaches are limited[9]. Recently, Liu and colleagues performed a RCT in 50 patients who had undergone AA repair and 50 patients who had undergone MO repair with a minimum 1-year follow-up. They concluded that the AA procedure has better recovery at short-term follow-ups, while both techniques are equivalent regarding long-term outcomes[10].
Motion analysis techniques can provide a more thorough description of 3-dimensional kinematics and offer a noninvasive, dynamic, quantitative alternative to radiographic methods. Motion analysis has been widely used to assess the motor abilities of people with neurological and musculoskeletal impairments[11]. To our knowledge, there is limited study regarding what biomechanical effect RTC tears have on different motion tasks and muscle activities after surgical treatment of RC tears. In 2007, Pearsall et al[12] prospectively evaluated patients who underwent a "mini-open" repair vs a completely arthroscopic technique for small to large size rotator cuff tears. They found no statistical difference in outcome between the two groups, indicating that either procedure was efficacious. In 2017, Fritz et al[13] applied a quantitative, validated upper extremity model to assess the kinematics and muscle activity of the shoulder following repair of the supraspinatus RC tendon compared to that in healthy shoulders in different activities of daily living (ADLs). They found that the RC repair group participants could accomplish the ADLs within the same time frame and through thoracolumbar joint kinematics, similar to those in the healthy shoulder group participants.
Wearable sensors are acquiring more and more influence in the diagnostic and rehabilitation field to assess the motor abilities of aging populations[14]. In a recent systematic literature review, Carnevale et al[15] analyzed the wearable systems for monitoring shoulder kinematics and their applicability in clinical settings and rehabilitation. However, to date, no studies have been carried out with wearable technologies in the assessment of quantitative functional recovery of RC tear healing. The present paper aims at comparing the clinical and biomechanical outcomes of two surgical techniques (AA vs MO procedure) to address the painful shoulder syndrome with partial or total supraspinatus tendon tear.
A total of 88 participants, 50 following RC repair with AA and 38 with MO, were recruited for this study. Each participant provided written informed consent to participate in the study approved by the Local Ethical Committee (ORTHO-SHOULDER, n. 6480, Prot. n. 0054602).
Inclusion criteria were: (1) Aged between 40-years-old and 70-years-old; (2) absence of shoulder pathology in the contralateral side; and (3) surgical procedure between January 2018 and October 2019. Exclusion criteria were: (1) Neurological impairments; (2) other pathological conditions that limited shoulder stability; and (3) previous surgical procedures on the ipsilateral side.
The surgeries were performed by single senior shoulder surgeons experienced in both the AA and MO repair techniques. In the case of arthroscopic surgery, the patient is positioned in lateral decubitus with the affected upper limb maintained by dedicated support. The arthroscope was placed in the subacromial space through a standard posterior portal; lateral and posterolateral accessory portals were subsequently established. The tear was adequately mobilized and repaired by attaching the supraspinatus to the prepared greater tuberosity using the single-row repair technique with a suture anchor. The procedure usually starts with the evaluation of the shoulder using the SCOI 15 points exam. The number of anchors and sutures used depended on the tear size and pattern. In the case of mini-open surgery, the patient is positioned in a beach chair position. The approach begins with a 5-cm lateral incision at the anterior border of the acromion. The fibers of the deltoid muscle are split by blunt dissection, and maximal visualization was established using a soft tissue retractor. It is very important not to damage the axillary nerve running close to the distal edge of the incision and to minimize detachment of deltoid muscle fibers from the lateral part of the acromion. A partial bursectomy is performed using dissection scissors. The rest of the procedure is basically the same for both techniques[10]. Both groups used the same rehabilitation protocol.
Each participant underwent concurrent, synchronized motion and electromyography (EMG) analysis. Postoperative outcome measurements were collected by two medical doctors and a bioengineer.
The primary outcome measures were the Constant-Murley score (CMS), the visual analogue scale (VAS) and, the disability of the arm, shoulder, and hand (DASH) score[16,17]. Secondary outcome measures were the biomechanical parameters in terms of the Range of Motion (ROM), quality of movement (velocity and acceleration), and muscle activation.
Kinematics and EMG data of patients were collected in our Laboratory of Functional Movement through the “Shoulder mobility” protocol. Tasks were explained clearly. The beginning and the end were signaled orally by the researcher to all participants. They were told to perform the movements to the highest position they could reach their preferred speed. They were placed standing in a neutral position to perform shoulder abduction in the coronal plane and shoulder flexion in the sagittal plane. They were told to perform both tasks with the elbow extended, the wrist in a neutral position, and the palm of the hand toward the midline at the beginning and end of the movement. They performed two series of five repetitions of both tasks, with a break of about 3 min between each series.
Upper arm active movements were detected with a wireless inertial sensor (BTS G-Sensor, BTS SpA, Milano, Italy), positioned on the arm aligned with the humerus at the level of the lateral epicondyle. The sensor, which communicates with the receiving unit (personal computer) via a Bluetooth link, was used for kinematic information, and BTS EMG-Analyzer software was used for data recording, processing, reporting, and storage. The same software also integrated data from four surface EMG [sEMG, BTS FREEEMG 1000 (BTS SpA, Milano, Italy)] attached to selected muscles according to SENIAM recommendations[18]. Muscle activity was assessed in the injured upper limb muscles (Biceps Brachialis Caput Longus, Upper Trapezius, Deltoid Anterior, Infraspinatus). To detect signals, adhesive Ag/AgCl electrodes (Kendall™ ECG Electrodes H124SG) with an effective diameter of 10 mm and an inter-electrode distance of 20 mm (center to center) were used. Proprietary algorithms fuse sensor data at 200 Hz. After positioning electrodes, patients were instructed to execute the two movements at their natural pace with the inertial sensor synchronized with EMG to identify the different cycles and phases of respectively abduction/adduction and flexion/extension.
ROM (°), acceleration (m/s2), and velocity (v, m/s) were extracted for each cycle in both forward and return direction from the inertial sensor, in the same way muscle activity has been quantified as root mean square (RMS, uV) and percentage of activation with respect to the peak dynamic value of the cycle (%) for each cycle in both directions.
SPSS v23.0 was used for all statistical computations. A P value of ≤ 0.05 was considered statistically significant. Descriptive statistics (mean ± SD) were calculated for age, height, weight, and body mass index (BMI). Standard procedures were used to calculate means and SDs. The Kolmogorov–Smirnov test showed a normal distribution of the data (P > 0.05). Independent t-tests have been used to compare the two surgical treatments (arthroscopic vs mini-open), while the mixed ANOVA test has been performed to understand if there is an interaction between the two treatments (between factor, arthroscopic vs mini-open) on the response of different muscles (within factor) for the selected body plane.
The Pearson χ2 test was used for between-group comparisons. The Fisher exact test was used for group comparisons when appropriate. Correlation between clinical and self-reported outcomes and biomechanical variables was calculated by Pearson’s correlation (r) and P value.
Socio-demographic characteristics of the study sample were shown in Table 1. Eighty-eight patients were finally enrolled in the study [female = 37 (42.1%), mean age = 59.3-years-old] with mean follow-up of 13 mo. Fifty-one patients presented a RC injury on the right side. Fifty patients underwent arthroscopic repair [female = 20 (40%), mean age = 58.5-years-old] and 38 underwent repair with a mini-open incision [female = 14 (36.8%), mean age = 60.3-years-old]. At the time of the examination, almost all the patients reported low pain scores and good health status. No differences emerged between groups in terms of demographic features (age, gender, BMI, and affected side).
| Characteristics | mean ± SD |
| Age (yr) | 59.27 ± 8.94 |
| BMI (kg/m2) | 28.06 ± 4.58 |
| Gender (Female), n (%) | 37 (42.05) |
| Affected Side (Right), n (%) | 51 (57.95) |
| Surgical treatment, n (%) | |
| AA | 50 (56.8) |
| MO | 38 (43.2) |
| Follow up (mo) | 13.62 ± 5.08 |
| VAS | 3.16 ± 2.7 |
| CMS | 69.5 ± 14.41 |
| DASH | 23.01 ± 21.07 |
| SF-12, n (%) | |
| Physical | 43.31 (9.53) |
| Mental | 46.53 (11.88) |
Table 2 summarized the main results in terms of comparisons of clinical, self-reported, and biomechanical outcomes between the two surgical procedures. Clinical scores (CMS, DASH, and VAS) did not differ significantly between groups as either self-reported health status (P > 0.05).
| AA (n = 50) | MO (n = 38) | P value | |
| Clinical score | |||
| VAS | 3 (2.62) | 3.37 (2.97) | 0.78 |
| CONSTANT | 65 (10.32) | 75.12 (17.38) | 0.14 |
| DASH | 24.12 (20.59) | 21.63 (23) | 0.81 |
| Self-reported health measures | |||
| SF-12PH | 43.17 (9.41) | 43.5 (10.34) | 0.94 |
| SF-12ME | 48.86 (9.86) | 43.63 (14.16) | 0.37 |
| Biomechanical tests | |||
| ROMABD | 110.88 (21.9) | 120.76 (27.91) | 0.41 |
| RMSABD,F,TRAP | 125.78 (77.49) | 54.52 (58.25) | 0.051 |
| RMSABD,R,TRAP | 59.5 (30.42) | 28.34 (26.39) | 0.041 |
| PERCABD,BBCL | 8.23 (2.64) | 19.23 (12.15) | 0.041 |
| PERCABD,TRAP | 35.99 (14.39) | 19.57 (15.97) | 0.041 |
| ROMFLEX | 127.95 (25.55) | 141.75 (33.51) | 0.34 |
| VELFLEX,F | 73.97 (31.74) | 46.26 (16.04) | 0.031 |
| VELFLEX,R | 88.65 (30.9) | 56.13 (23.72) | 0.031 |
| RMSFLEX,F,TRAP | 91.19 (49.57) | 41.35 (45.43) | 0.041 |
| RMSFLEX,R,TRAP | 47.15 (24.04) | 22.99 (19.58) | 0.041 |
| PERCFLEX,DLTA | 43.18 (6.9) | 58.65 (9.6) | < 0.011 |
| PERCFLEX,TRAP | 29.97 (11.21) | 14.2 (9.04) | < 0.011 |
A strong inverse correlation has been found among the two clinical scores of shoulder abilities (r = -0.63, P < 0.01): lower level of pain and improved ability to carry out the normal daily activities of the patient (increasing CMS scores) were associated with a lower level of shoulder impairment (decreasing DASH scores). Furthermore, only the DASH score was positively related to pain level (VAS, r = 0.68) and both physical and mental components of SF-12, indicating that lower levels of shoulder impairment were associated with lower pain and better health status.
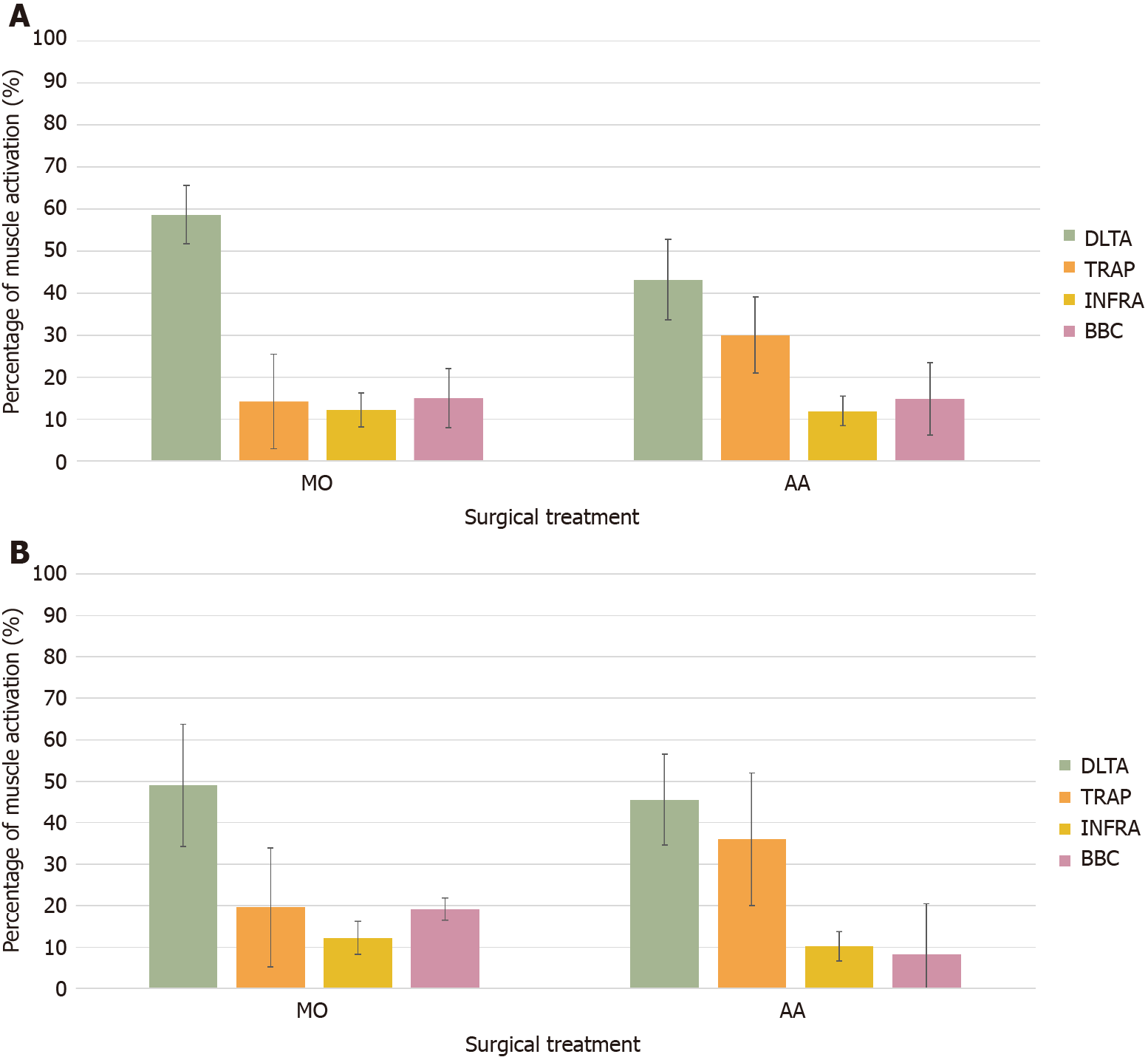
Significant differences emerged in terms of mean activation of the upper trapezius muscle in both abduction and flexion movements. In the AA group, the trapezius muscle was more active than the MO group during both the forward and return phase of both abduction and flexion movements, thus indicating a significant contribution of this muscle in joint mobility and stability.
However, no significant differences were found between groups in the post-operative range of motion either in sagittal (abduction, P = 0.41) or frontal planes (flexion-extension, P = 0.34). Moreover, we observed a significant difference between groups in the average velocity required to complete the flexion movement either in the forward or return phase. Patients who were treated with the MO surgery reported significantly lower velocity in the execution of the movement than patients in the AA group. A possible explanation may be found in the different contributions of observed muscles’ recruitment during the movement: in the AA group, the deltoid anterior and upper trapezius showed a high percentage of mean activation, while in the MO group, the deltoid anterior contributed more than fifty percent of the overall activation.
An overview of the mean contribution of each recorded muscle during the movement is shown in Figure 1. The results of mixed ANOVA revealed that significant interactions were present between the adopted surgical procedure and the contribution of muscles (%) in both abduction (F1.618 = 3.707, P = 0.05) and flexion (F2.035 = 8.732, P < 0.01) movements. In the abduction movement, the activation of the deltoid anterior was significantly higher than other muscles while the contribution of upper trapezius and infraspinatus muscles did not show any difference between each other. Similar results were found in the flexion movement, where the percentage activation of the deltoid anterior was significantly higher than other contributions.
Rotator cuff tears are the most common shoulder injury. Treatment options include nonoperative management, arthroscopic debridement with a biceps tenotomy, or tenodesis, partial repair, complete repair, muscle-tendon transfer, superior capsular reconstruction, patch augmentation, and reverse total shoulder arthroplasty[19]. The treatment can be performed with two different approaches: Mini-open (MO) or all-arthroscopic (AA) technique. The ideal repair of the RC tear should withstand the physiological loads while allowing simultaneous tendon healing to occur. Recently, Liu et al[10] performed an RCT in 50 patients who had undergone AA repair and 50 patients who had undergone MO repair with a minimum 1-year follow-up. They concluded that the AA procedure has better recovery at short-term follow-ups, while both techniques are equivalent regarding long-term outcomes. Although there is still an open debate on the superiority of surgical treatment over the other[20,21], few attempts have been made in promoting the use of motion capture technologies to analyze kinematics and muscle activity of shoulder mobility in the postoperative phase, especially with the advancing in wearable devices.
The present cross-sectional study enrolled a sample of patients who had undergone AA/MO repair with a minimum 1-year follow-up. Patients were then evaluated using both clinical and biomechanical tests to assess whether there were relevant effects of the surgical treatment on the selected outcomes.
Our findings reported no statistically significant difference in terms of clinical scores and joint excursions after RC repair, in line with what emerged from previous studies[10,12,21]. However, significant differences emerged in terms of other kinematic factors and muscle activation. Patients treated with the MO surgery reported significantly lower velocities in the execution of the movement compared with the AA group. The upper trapezius muscle in the AA group showed higher mean activation (RMS) than the MO group during both the forward and return phases of both abduction and flexion movements. Furthermore, in the AA group, deltoid anterior and upper trapezius showed a higher percentage of mean activation, while in the MO group deltoid anterior contributed more than fifty percent of the overall activation.
While different normalization processes and range of movement prevent direct comparison with the current study, previous EMG research during coronal plane abduction indicates that high contraction intensities throughout the abduction movement in healthy subjects were seen for glenohumeral and scapulothoracic prime movers such as anterior and middle deltoid, supraspinatus, serratus anterior, rhomboids, and upper, middle, and lower trapezius[22].
Rehabilitation probably plays a role in the increased ROM and muscular strength, due to the position and kinematics of the scapula. They can influence patient symptoms. Consequently, motivation and cooperation during the rehabilitation process can influence the results[23].
Previous investigations on the role of shoulder muscles in flexion and abduction movements have been carried out mostly in healthy subjects[24,25] showing that deltoids were the largest muscle contributor to humeral elevation during flexion tasks, while trapezius and serratus anterior combined to do more work than deltoids for every task including flexion.
Wearable technologies could support clinical practice since they provide clinical information during the performance of a motor task, and their adoption should grow in shoulder evaluation and therapy. The present work represents a preliminary attempt at promoting novel wearable technologies in clinical practice. We compared the postoperative effects of two surgical treatments through clinical scores, standardized protocol, and wearable sensors. Our findings were almost in line with previous investigations regarding clinical scores. However, our analysis highlighted a different response in muscle activation during the shoulder movement in both flexion/extension and abduction/adduction. A significant interaction effect emerged for mean activation of deltoid anterior and upper trapezius with surgical procedure, thus indicating that the adopted treatment influenced the functional recovery of the joint. Further studies with larger samples are needed to confirm our findings and open new scenarios in surgical planning and rehabilitation of shoulder instability.
Rotator cuff (RC) tears are one of the most frequent pathologies within the shoulder girdle. Hand dominance and older age are associated with RC tears. Two different surgical procedures, the mini-open (MO) and all-arthroscopic (AA) approach represented the standard of treatment.
To understand if AA and MO procedures provide comparable clinical results in the repairment of RC tears.
The present paper aims at comparing the clinical and biomechanical outcomes of two surgical techniques (AA vs MO procedure) to address the painful shoulder syndrome with partial or total supraspinatus tendon tear.
Eighty-eight participants, 50 following RC repair with AA and 38 with MO approach, were recruited in the present cross-sectional case-control study. All the patients underwent postoperative clinical evaluation for pain, impairment, and disability and limitation in daily activity.
No statistically significant differences between the two procedures were observed in either main clinical score or range of motion. A significant increase in velocity during the movement execution and a higher contribution of upper trapezius muscles were found in the AA group compared with MO patients.
In terms of clinical scores, our findings were in line with previous results. However, the use of technology-based assessment of shoulder mobility has revealed significant differences between the two techniques in terms of mean velocity and scheme of muscle activation.
Further studies with larger samples are needed to confirm such findings and open new scenarios in the surgical planning and the rehabilitation of shoulder instability.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zabrzyński J S-Editor: Wang JL L-Editor: Filipodia P-Editor: Wang JL
| 1. | Sayampanathan AA, Andrew TH. Systematic review on risk factors of rotator cuff tears. J Orthop Surg (Hong Kong). 2017;25:2309499016684318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Zabrzyński J, Huri G, Gagat M, Łapaj Ł, Yataganbaba A, Szwedowski D, Askin M, Paczesny Ł. The Impact of Smoking on Clinical Results Following the Rotator Cuff and Biceps Tendon Complex Arthroscopic Surgery. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Sambandam SN, Khanna V, Gul A, Mounasamy V. Rotator cuff tears: An evidence based approach. World J Orthop. 2015;6:902-918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 102] [Cited by in RCA: 128] [Article Influence: 12.8] [Reference Citation Analysis (6)] |
| 4. | Shinners TJ, Noordsij PG, Orwin JF. Arthroscopically assisted mini-open rotator cuff repair. Arthroscopy. 2002;18:21-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Verma NN, Dunn W, Adler RS, Cordasco FA, Allen A, MacGillivray J, Craig E, Warren RF, Altchek DW. All-arthroscopic versus mini-open rotator cuff repair: a retrospective review with minimum 2-year follow-up. Arthroscopy. 2006;22:587-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 118] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 6. | Kang L, Henn RF, Tashjian RZ, Green A. Early outcome of arthroscopic rotator cuff repair: a matched comparison with mini-open rotator cuff repair. Arthroscopy. 2007;23:573-582, 582.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Lindley K, Jones GL. Outcomes of arthroscopic versus open rotator cuff repair: a systematic review of the literature. Am J Orthop (Belle Mead NJ). 2010;39:592-600. [PubMed] |
| 8. | Liem D, Bartl C, Lichtenberg S, Magosch P, Habermeyer P. Clinical outcome and tendon integrity of arthroscopic versus mini-open supraspinatus tendon repair: a magnetic resonance imaging-controlled matched-pair analysis. Arthroscopy. 2007;23:514-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Kolk A, de Witte PB, Henseler JF, van Zwet EW, van Arkel ER, van der Zwaal P, Nelissen RG, de Groot JH. Three-dimensional shoulder kinematics normalize after rotator cuff repair. J Shoulder Elbow Surg. 2016;25:881-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 10. | Liu J, Fan L, Zhu Y, Yu H, Xu T, Li G. Comparison of clinical outcomes in all-arthroscopic versus mini-open repair of rotator cuff tears: A randomized clinical trial. Medicine (Baltimore). 2017;96:e6322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Bortone I, Castellana F, Lampignano L, Zupo R, Moretti B, Giannelli G, Panza F, Sardone R. Activity Energy Expenditure Predicts Clinical Average Levels of Physical Activity in Older Population: Results from Salus in Apulia Study. Sensors (Basel). 2020;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Pearsall AW 4th, Ibrahim KA, Madanagopal SG. The results of arthroscopic versus mini-open repair for rotator cuff tears at mid-term follow-up. J Orthop Surg Res. 2007;2:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Fritz JM, Inawat RR, Slavens BA, McGuire JR, Ziegler DW, Tarima SS, Grindel SI, Harris GF. Assessment of Kinematics and Electromyography Following Arthroscopic Single-Tendon Rotator Cuff Repair. PM R. 2017;9:464-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Zarowin J, Warnick E, Mangan J, Nicholson K, Goyal DKC, Galetta MS, Fang T, Schroeder GD, Kepler CK, Vaccaro AR. Is Wearable Technology Part of the Future of Orthopedic Health Care? Clin Spine Surg. 2020;33:99-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Carnevale A, Longo UG, Schena E, Massaroni C, Lo Presti D, Berton A, Candela V, Denaro V. Wearable systems for shoulder kinematics assessment: a systematic review. BMC Musculoskelet Disord. 2019;20:546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 16. | Longo UG, Vasta S, Maffulli N, Denaro V. Scoring systems for the functional assessment of patients with rotator cuff pathology. Sports Med Arthrosc Rev. 2011;19:310-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 17. | Longo UG, Saris D, Poolman RW, Berton A, Denaro V. Instruments to assess patients with rotator cuff pathology: a systematic review of measurement properties. Knee Surg Sports Traumatol Arthrosc. 2012;20:1961-1970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Hermens HJ, Freriks B, Merletti R, Stegemen D, Blok J, Rau G, Disselhorst-Klug C, Hagg G. European Recommendations for Surface Electromyography. Results of the SENIAM (Surface EMG for Noninvasive Assessment of Muscles) Project. Enschede: Roessingh Research and Development Ltd, 1999. |
| 19. | Checketts JX, Scott J, Gordon J, Jones J, Horn J, Farabough M, Whitener J, Boose M, Vassar M. An Evaluation of the Rotator Cuff Repair Research Pipeline. Orthop J Sports Med. 2018;6:2325967118805731. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Oliva F, Piccirilli E, Bossa M, Via AG, Colombo A, Chillemi C, Gasparre G, Pellicciari L, Franceschetti E, Rugiero C, Scialdoni A, Vittadini F, Brancaccio P, Creta D, Buono AD, Garofalo R, Franceschi F, Frizziero A, Mahmoud A, Merolla G, Nicoletti S, Spoliti M, Osti L, Padulo J, Portinaro N, Tajana G, Castagna A, Foti C, Masiero S, Porcellini G, Tarantino U, Maffulli N. I.S.Mu.L.T - Rotator Cuff Tears Guidelines. Muscles Ligaments Tendons J. 2015;5:227-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 21. | Jancuska J, Matthews J, Miller T, Kluczynski MA, Bisson LJ. A Systematic Summary of Systematic Reviews on the Topic of the Rotator Cuff. Orthop J Sports Med. 2018;6:2325967118797891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | Wickham J, Pizzari T, Stansfeld K, Burnside A, Watson L. Quantifying 'normal' shoulder muscle activity during abduction. J Electromyogr Kinesiol. 2010;20:212-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 23. | Zabrzyński J, Huri G, Gryckiewicz S, Çetik RM, Szwedowski D, Łapaj Ł, Gagat M, Paczesny Ł. Biceps Tenodesis versus Tenotomy with Fast Rehabilitation Protocol-A Functional Perspective in Chronic Tendinopathy. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Vicenti G, Moretti L, Carrozzo M, Pesce V, Solarino G, Moretti B. Evaluation of long-term postoperative outcomes between mini-open and arthroscopic repair for isolated supraspinatus tears: a retrospective analysis. Musculoskelet Surg. 2018;102:21-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Seth A, Dong M, Matias R, Delp S. Muscle Contributions to Upper-Extremity Movement and Work From a Musculoskeletal Model of the Human Shoulder. Front Neurorobot. 2019;13:90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |